Abstract
Background: In the past decade, targeted therapy with antiangiogenic drugs has become standard of care for most types of metastatic, progressive thyroid cancer. While these drugs were thought initially to be less toxic than traditional chemotherapy, they can have rare but serious and fatal toxicities. Once such toxicity that has been reported in other tumor types is upper airway fistula formation, which can be life-threatening.
Summary: Here, we describe three patients treated with antiangiogenic tyrosine kinase inhibitors at two academic institutions who developed aerodigestive fistula. All three patients had risk factors for fistula formation, which included external beam radiation and/or large tumor with invasion of the tracheal wall.
Conclusions: Fistula formation is a known but rare side effect of antiangiogenic tyrosine kinase inhibitors. Knowledge of the risk factors that may predispose thyroid cancer patients to this serious adverse event is vital prior to prescribing antiangiogenics. Particular caution should be observed when using these drugs in patients undergoing radiation therapy or surgery, or in patients whose tumor is invading vital structures of the neck, as they may be at higher risk of developing this rare complication. In these patients, antiangiogenic tyrosine kinase inhibitors should be used cautiously, patients should be aware of the risk, and physicians should monitor patients for symptoms of fistula.
Introduction
Thyroid cancer is the most common endocrine malignancy and is expected to have an incidence of 62,980 in 2014. It is the fifth most commonly diagnosed cancer in women and the eighth most diagnosed cancer in the United States (1). Ninety-five percent of thyroid cancers are differentiated thyroid cancers (DTC), which include papillary, follicular, and Hürthle cell thyroid cancers, and 85% of patients with DTC are cured with surgery, radioactive iodine (RAI), and thyrotropin (TSH) suppression. Medullary thyroid cancer (MTC) represents up to 3% of thyroid cancers, and although the 10 year survival of patients with MTC is 75%, only 40% of patients with locally advanced or metastatic disease survive to 10 years (2). The excellent prognosis for patients treated with standard therapy for DTC accounts for the relatively low overall mortality rate, and only 1890 deaths are expected from thyroid cancer in 2014 (1–3).
Despite the favorable prognosis of most thyroid cancers, a small percentage of patients develop metastatic disease that is not responsive to RAI. Poor response to conventional chemotherapy has led to the use of antiangiogenic tyrosine kinase inhibitor (TKI) therapy, and average progression-free survival ranges from 9 to 21 months, depending on the TKI used, as compared to 5–6 months with standard chemotherapy (4–12). This class of TKI has now become the standard of care for patients with progressive metastatic disease (13).
Although TKIs were initially believed to be less toxic than conventional chemotherapy, they can have rare serious and even life-threatening side effects. In this article, we present three cases of aerodigestive fistula formation after treatment with an antiangiogenic TKI.
Patients
Patient 1
A 57-year-old male presented to his primary care physician after noticing tightening of his shirt collar around his neck and was found to have a left thyroid mass on exam. Cross-sectional imaging confirmed a large mass on the left side of the thyroid extending into the substernum and tracheal deviation to the right with left neck adenopathy. A biopsy of a left neck lymph node showed atypical cells that had features suggestive of a thyroid neoplasm.
He underwent a total thyroidectomy with left modified neck dissection. Pathology revealed a 9.5 cm Hürthle cell carcinoma with extrathyroidal extension, lymphovascular invasion, and positive surgical margins. Two out of 30 lymph nodes in the left neck were positive for Hürthle cell carcinoma. A whole body 131I scan revealed localized uptake in the neck, and he was given 200 mCi RAI. The patient presented to M. D. Anderson for a second opinion. Review of systems and a physical exam were unremarkable. His thyroglobulin was 2225 ng/mL, and his TSH was 43 mU/L. Cross-sectional imaging was concerning for metastatic disease involving the mediastinum bilaterally and possible right lung nodules. He underwent a left paratracheal neck dissection and superior mediastinal lymphadenectomy for residual disease.
Six months later, progressive disease was found in the mediastinum and lungs associated with a rising thyroglobulin. He was started on 400 mg of sorafenib twice daily off clinical trial. He tolerated therapy, but had a mixed response to treatment. His pulmonary disease stabilized, but the left mediastinal lymphadenopathy progressed.
Thirteen months after sorafenib initiation, he underwent median sternotomy at an outside institution with resection of left and right paratracheal lesions. Sorafenib was stopped one week preoperatively. Three months later, he completed external beam radiation to the mediastinum and thyroid bed with a total dose of 66 Gy in 33 daily fractions over 48 calendar days using 3D conformal radiation therapy technique. He resumed sorafenib one week following radiation. The following year, he underwent left vocal cord laryngoplasty.
Approximately nine months later, he was found to have progressive mediastinal, right hilar, and subcarinal disease with a rising thyroglobulin. He discontinued sorafenib at this time to enroll in a clinical trial with cabozantinib. The patient had experienced recurrent episodes of bronchitis several months prior to the clinical trial. Three months after starting cabozantinib, he had begun to feel that ingested liquids were moving into his lungs. He then had recurrent episodes of cough productive of purulent sputum and was hospitalized for aspiration pneumonia. Cabozantinib was discontinued. An esophagram revealed a 1–2 cm esophageal fistula near the area of his previous surgery and radiation (Fig. 1). Bronchoscopy confirmed the presence of a tracheosophageal fistula a few centimeters above the carina (Fig. 1). The patient underwent placement of an esophageal stent, and no leak was seen on a follow-up barium swallow. He recovered fully from the aspiration pneumonia with antimicrobials and was eventually discharged. Two weeks later, the patient had an episode of severe hemoptysis after coughing violently, collapsed, and died suddenly. At autopsy, he was found to have a 5 mm aortotracheal fistula at his previous radiation site without evidence of cancer at the fistula site.
FIG. 1.
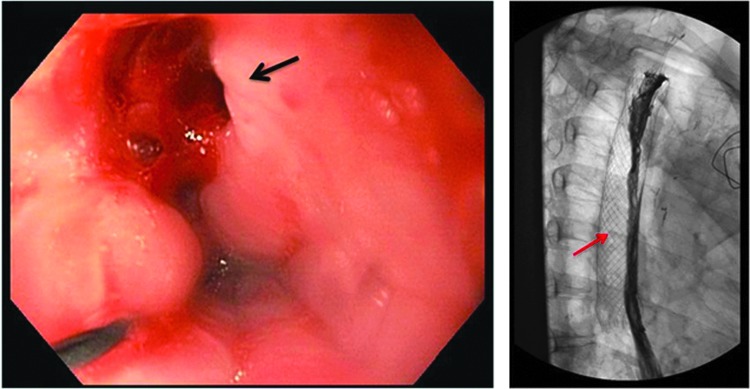
Patient 1: Tracheoesophageal fistula. Left: A fistula was found on endoscopy at 25 cm (black arrow) 26 months after starting sorafenib for Hürthle cell thyroid cancer. Right: Esophagram following stent (red arrow) placement reveals no extraluminal contrast.
Patient 2
A 49-year-old male was found to have a left neck mass on exam after presenting to an outside hospital with a four-week history of hoarseness. Cross-sectional imaging showed a highly fluorodeoxyglucose-avid 7 cm left thyroid nodule and multiple small pulmonary masses. Fine-needle biopsy of the thyroid nodule revealed papillary thyroid cancer. He subsequently underwent partial left thyroid lobectomy, which confirmed a 2.5 cm poorly differentiated papillary thyroid cancer. During surgery, he was noted to have extensive invasion of the surrounding structures, and there was gross disease that was unresectable. Following surgery, he was treated with 66 Gy external beam radiation in 33 daily fractions over 46 calendar days with five weeks of concomitant adriamycin. A magnetic resonance imaging (MRI) and positron emission tomography/computed tomography (PET-CT) scan of the brain obtained the following month showed multiple brain lesions, the largest measuring 2.4 cm, in addition to his persistent neck and lung disease. He denied headache or other neurological complaints. He was started on 2 mg of dexamethasone every other day and received whole brain radiation. He was also found to have multiple bone metastases, including to the right second rib and bilateral hips, and underwent external beam radiation to the left hip. A month later, he elected to have left laryngoplasty with placement of a vocal cord implant.
The patient presented for a second opinion regarding treatment. He denied dysphagia or shortness of breath and had maintained an active lifestyle. Exam was significant for surgical changes of the neck, eschar from radiation therapy, and a palpable thyroid mass. A CT scan of the neck showed a 6 cm heterogeneous, nonenhancing left neck mass with numerous areas of internal necrosis. The tumor was likely invading the left tracheal wall, but there was no evidence of endoluminal involvement. Sunitinib was intitiated at a dose of 37.5 mg daily continuously. Approximately six weeks after starting sunitinib, the patient began to complain of increasing neck pain. A CT scan of the neck, performed two months after starting sunitinib, revealed erosion of the mass into the tracheal wall and a significant decrease in tumor size. It also demonstrated a linear gas collection between the residual neck mass and the left anterior aspect of the trachea that was consistent with a trachea-tumor fistula (Fig. 2). Sunitinib was discontinued. The patient was evaluated by a thoracic surgeon and scheduled for an elective tracheal stent placement. Seven days later, the patient was admitted with respiratory distress and stridor. Approximately 80% of his mid-trachea was found to be occluded by the tumor, and a tracheal stent was placed for airway protection. The patient decided to enroll in hospice care and died one week later.
FIG. 2.
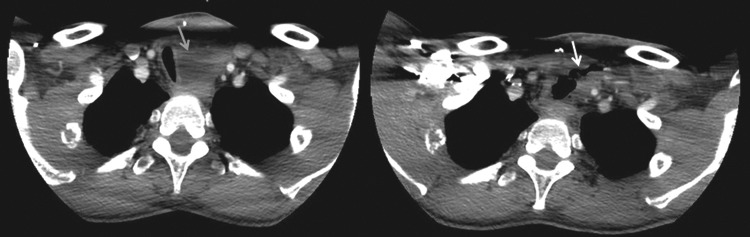
Patient 2: Tracheo-tumor fistula. Left: Computed tomography (CT) scan of the chest obtained prior to starting sunitinib shows tracheal compression due to a left-sided mass (gray arrow). Right: CT chest scan obtained two months after starting sunitinb for papillary thyroid cancer reveals a fistulous tract between the trachea and thyroid mass (white arrow).
Patient 3
A 58-year-old male with no significant past medical history presented to his primary care physician with a year of progressively worsening neck pain, hoarseness, and dysphagia. Imaging showed a left thyroid mass measuring 9 cm with substernal extension. A core biopsy was done and was consistent with medullary thyroid carcinoma. He was referred to our center, and imaging confirmed medullary thyroid cancer with invasion into the esophagus and posterior trachea, and he had associated multicompartmental cervical as well as mediastinal adenopathy. He also had a pancreatic lesion presumed to be metastatic disease. A germline RET mutation was absent.
Due to progressive disease, the patient enrolled in a clinical trial with lenvatinib. He developed fatigue and diarrhea, but otherwise initially tolerated the drug well and had a best response of stable disease with regression. After four months of therapy, he developed progressive dysphagia and anorexia and a percutaneous endoscopic gastrostomy (PEG) tube was placed for nutritional support. CT imaging six months after the start of therapy revealed an increase in size of the neck mass and air within the mass near the esophagus, which prompted concern for fistula formation. An esophagram revealed a fistula between the cervical esophagus and the thyroid mass (Fig. 3). Since the fistula was in the proximal esophagus, stent placement was not an option. Lenvatinib was discontinued.
FIG. 3.

Patient 3: Esophago-tumor fistula. Top: Esophagram, obtained six months after starting lenvatinib for medullary thyroid cancer, demonstrates a large fistulous tract arising from the left side of the lower cervical esophageal wall and extending in the direction of the known left thyroid mass (black arrow). Bottom: CT chest scan revealed a fistula between the left side of the lower cervical esophageal wall and the left thyroid mass (white arrow).
The patient presented to the hospital a month later with left lower neck swelling and purulent drainage from an opening in the skin of his left neck. He was found to have an abscess secondary to his esophageal fistula. He was hospitalized and then discharged on several weeks of antimicrobials. A week after finishing antimicrobial therapy, the patient was again admitted with a 3 cm abscess in his left neck. He was treated with broadened antimicrobial coverage. The patient elected to be admitted to hospice care and died two days later.
Discussion
Antiangiogenic TKIs have become an important part of therapy for progressive and advanced medullary and RAI-resistant differentiated thyroid cancers. Although antiangiogenic TKIs lack many of the toxicities associated with traditional cytotoxic chemotherapy, they are known to have side effects that range from mild fatigue and mucositis to hypertension, stroke, and delayed healing (14–17). As antiangiogenic TKIs are more commonly used, additional side effects, including aerodigestive fistula, are being elucidated. The product labeling for sunitinib and cabozantinib report fistula as a rare adverse event. Cabozantinib carries a black box warning for perforations, fistulas, and bleeding. Tracheal and esophageal (“non-GI”) fistulas were reported in 4% of patients on this drug, and two of the cases were fatal. Lenvatinib is not a commercially available drug.
Here, we present three cases of aerodigestive fistula formation after treatment with antiangiogenic therapy for thyroid cancer. To our knowledge, only one case of antiangiogenic therapy for thyroid cancer resulting in aerodigestive fistula formation has been reported, but no details regarding the patient's history were published (18). Tracheoesophageal fistula has been reported in lung cancer patients after treatment with the VEGF inhibitor bevacizumab plus radiation (19–21). Additionally, a study of 43 head and neck cancer patients treated with bevacizumab and chemoradiotherapy identified five patients who formed an aerodigestive fistula with treatment (22). Bronchial fistula formation after treatment with sunitinib and radiation therapy for a pulmonary renal cell metastasis has also been reported (23). A history of esophagitis, radiation therapy at the fistula formation site, or instrumentation was common to these patients.
Notably, no aerodigestive fistulas were reported in a study by Schwartz et al. that examined outcomes in differentiated thyroid cancer patients who underwent surgery and received postoperative external beam radiation without antiangiogenic therapy (24). This suggests that fistula formation in thyroid cancer patients is exceedingly rare in the setting of modern radiation and surgery alone. Two cases of aerodigestive fistula following surgery and external beam radiation for thyroid cancer were previously reported by Grossman et al. in 1985 (25). One patient who was treated in 1970 with cobalt developed a nonhealing tracheocutaneous fistula after surgical tracheostomy. A second patient was found to have a tracheal cutaneous fistula 25 years after his initial surgery and high-dose surface x-ray radiation given in 1975. In both of these cases, radiation with a significantly higher surface dose compared to modern modalities was used. Risk for these rare complications after surgery and radiation alone is therefore considerably less in contemporary practice.
The three thyroid cancer patients reported here had one or more risk factors for weakening of the aerodigestive tract epithelia, including a history of external beam and invasion of tumor into the esophagus or trachea. In patient 1, the tracheosophageal fistula was also believed to have provided entry for bacteria, which may have incited an inflammatory response and accelerated soft tissue damage that led to the formation of his aortotracheal fistula. It is likely that antiangiogenic TKIs administered to patients with pre-existing risk factors including radiotherapy, surgery, and tumor invasion of vital structures played a role in the development of aerodigestive fistulas by impairing growth of new blood vessels and delaying wound healing, thereby increasing susceptibility to fistula formation.
As antiangiogenic TKIs develop more of a role in thyroid cancer treatment, understanding their side effects and under which conditions they occur is key for the identification of patients at risk for rare but serious complications from these drugs and in order to define interventions that will prevent their associated morbidity and mortality. Particular caution should be observed when using these drugs in patients undergoing radiation therapy, instrumentation of the trachea or esophagus, or in patients whose tumor is invading vital structures of the neck including the esophagus, trachea, and major vasculature, as these patients may be at higher risk of developing fistulas. In these patients, antiangiogenic TKIs and external beam radiation should be used cautiously, and physicians should question patients regarding symptoms of fistula.
Further studies are needed to characterize risk factors better for aerodigestive fistula formation and to define interventions to prevent their occurrence. It is important to continue to study novel nonantiangiogenic treatments for thyroid cancer in order to identify safer alternate therapies for patients at high risk of fistula formation.
Acknowledgment
This study was supported in part through The University of Texas MD Anderson Cancer Center's Cancer Center Support Grant CA16672.
Author Disclosure Statement
M.E.C. received research funding from Exelixis, Eisai, and Roche. There are no other disclosures.
References
- 1.Siegel R, Ma J, Zou Z, Jemal A.2014Cancer Statistics, CA Cancer J Clin 64:9–29 [DOI] [PubMed] [Google Scholar]
- 2.Roman S, Lin R, Sosa JA.2006Prognosis of medullary thyroid carcinoma: demographic, clinical, and pathologic predictors of survival in 1252 cases. Cancer 107:2134–2142 [DOI] [PubMed] [Google Scholar]
- 3.Gilliland FD, Hunt WC, Morris DM, Key CR.1997Prognostic factors for thyroid carcinoma. A population-based study of 15,698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973–1991. Cancer 79:564–573 [DOI] [PubMed] [Google Scholar]
- 4.Cohen EE, Rosen LS, Vokes EE, Kies MS, Forastiere AA, Worden FP, Kane MA, Sherman E, Kim S, Bycott P, Tortorici M, Shalinsky DR, Liau KF, Cohen RB.2008Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II study. J Clin Oncol 26:4708–4713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurzrock R, Sherman SI, Ball DW, Forastiere AA, Cohen RB, Mehra R, Pfister DG, Cohen EE, Janisch L, Nauling F, Hong DS, Ng CS, Ye L, Gagel RF, Frye J, Muller T, Ratain MJ, Salgia R.2011Activity of XL184 (cabozantinib), an oral tyrosine kinase inhibitor, in patients with medullary thyroid cancer. J Clin Oncol 29:2660–2666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sherman SI, Jarzab B, Cabanillas ME, Licitra L, Pacini F, Martins R, Robinson B, Ball DW, McCaffrey J, Shah MH, Bodenner D, Allison R, Newbold K, Elisei R, O'Brien JP, Schlumberger M.2011A phase II trial of the multitargeted kinase inhibitor E7080 in advanced radioiodine (RAI)-refractory differentiated thyroid cancer (DTC). J Clin Oncol 29:5503 [Abstract] [Google Scholar]
- 7.Sherman SI, Wirth LJ, Droz JP, Hofmann M, Bastholt L, Martins RG, Licitra L, Eschenberg MJ, Sun YN, Juan T, Stepan DE, Schlumberger MJ.2008Motesanib diphosphate in progressive differentiated thyroid cancer. N Engl J Med 359:31–42 [DOI] [PubMed] [Google Scholar]
- 8.Bible KC, Suman VJ, Molina JR, Smallridge RC, Maples WJ, Menefee ME, Rubin J, Sideras K, Morris JC, 3rd, McIver B, Burton JK, Webster KP, Bieber C, Traynor AM, Flynn PJ, Goh BC, Tang H, Ivy SP, Erlichman C.Efficacy of pazopanib in progressive, radioiodine-refractory, metastatic differentiated thyroid cancers: results of a phase 2 consortium study. Lancet Oncol 11:962–972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kloos RT, Ringel MD, Knopp MV, Hall NC, King M, Stevens R, Liang J, Wakely PE, Jr, Vasko VV, Saji M, Rittenberry J, Wei L, Arbogast D, Collamore M, Wright JJ, Grever M, Shah MH.2009Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol 27:1675–1684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta-Abramson V, Troxel AB, Nellore A, Puttaswamy K, Redlinger M, Ransone K, Mandel SJ, Flaherty KT, Loevner LA, O'Dwyer PJ, Brose MS.2008Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 26:4714–4719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cabanillas ME, Waguespack SG, Bronstein Y, Williams MD, Feng L, Hernandez M, Lopez A, Sherman SI, Busaidy NL.2010Treatment with tyrosine kinase inhibitors for patients with differentiated thyroid cancer: the M. D. Anderson experience. J Clin Endocrinol Metab 95:2588–2595 [DOI] [PubMed] [Google Scholar]
- 12.Carr LL, Mankoff DA, Goulart BH, Eaton KD, Capell PT, Kell EM, Bauman JE, Martins RG.Phase II study of daily sunitinib in FDG-PET-positive, iodine-refractory differentiated thyroid cancer and metastatic medullary carcinoma of the thyroid with functional imaging correlation. Clin Cancer Res 16:5260–5268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherman SI, Tuttle RM, Ball DW, Byrd D, Clark OH, Daniels GH, Dilawari RA, Doherty GM, Ehya H, Farrar WB, Haddad RI, Kandeel F, Kloos RT, Kopp P, Lamonica DM, Loree TR, Lydiatt WM, McCaffrey J, Olson JA, Parks L, Ridge JA, Shah JP, Sturgeon C, Waguespack SG, Wang TN, Wirth LJ.2009NCCN Practice Guidelines in Oncology: Thyroid Carcinoma. J Natl Compr Canc Netw 12009. [DOI] [PubMed] [Google Scholar]
- 14.Package insert sorafenib (Nexavar). Available at: www.berlex.bayerhealthcare.com/html/products/pi/Nexavar_PI.pdf (accessed September14, 2012)
- 15.Package insert sunitinib (Sutent). Available at: www.pfizeroncology.com/sites/pop/PDFs/uspi_sutent.pdf (accessed September14, 2012)
- 16.Package insert vandetanib (Vandetanib). Available at: www1.astrazeneca-us.com/pi/vandetanib.pdf (accessed September14, 2012)
- 17.Package insert pazopanib (Votrient). Available at: GlaxoSmithKline. www.gsksource.com/gskprm/htdocs/documents/VOTRIENT-PI-MG.PDF (accessed September14, 2012)
- 18.Cohen EE, Needles BM, Cullen KJ, Wong SJ, Wade JL, Ivy SP, Villaflor VM, Seiwert TY, Nichols K, Vokes EE.2008Phase 2 study of sunitinib in refractory thyroid cancer. J Clin Oncol 26:abstr 6025 [Google Scholar]
- 19.Spigel DR, Hainsworth JD, Yardley DA, Raefsky E, Patton J, Peacock N, Farley C, Burris HA, 3rd, Greco FA.2010Tracheoesophageal fistula formation in patients with lung cancer treated with chemoradiation and bevacizumab. J Clin Oncol 28:43–48 [DOI] [PubMed] [Google Scholar]
- 20.Goodgame B, Veeramachaneni N, Patterson A, Govindan R.2008Tracheo-esophageal fistula with bevacizumab after mediastinal radiation. J Thorac Oncol 3:1080–1081 [DOI] [PubMed] [Google Scholar]
- 21.Gore E, Currey A, Choong N.2009Tracheoesophageal fistula associated with bevacizumab 21 months after completion of radiation therapy. J Thorac Oncol 4:1590–1591 [DOI] [PubMed] [Google Scholar]
- 22.Seiwert TY, Haraf DJ, Cohen EE, Stenson K, Witt ME, Dekker A, Kocherginsky M, Weichselbaum RR, Chen HX, Vokes EE.2008Phase I study of bevacizumab added to fluorouracil- and hydroxyurea-based concomitant chemoradiotherapy for poor-prognosis head and neck cancer. J Clin Oncol 26:1732–1741 [DOI] [PubMed] [Google Scholar]
- 23.Basille D, Andrejak M, Bentayeb H, Kanaan M, Fournier C, Lecuyer E, Boutemy M, Garidi R, Douadi Y, Dayen C.2010Bronchial fistula associated with sunitinib in a patient previously treated with radiation therapy. Ann Pharmacother 44:383–386 [DOI] [PubMed] [Google Scholar]
- 24.Schwartz DL, Lobo MJ, Ang KK, Morrison WH, Rosenthal DI, Ahamad A, Evans DB, Clayman G, Sherman SI, Garden AS.2009Postoperative external beam radiotherapy for differentiated thyroid cancer: outcomes and morbidity with conformal treatment. Int J Radiat Oncol Biol Phys 74:1083–1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grossman TW, Wilson JF, Toohill RJ.1985Delayed aerodigestive tract complications following combined therapy for thyroid cancer. Ann Otol Rhinol Laryngol 94:505–508 [DOI] [PubMed] [Google Scholar]


