ABSTRACT
As the United States ages, the patient population in acute care hospitals is increasingly older and more medically complex. Despite evidence of a high burden of disease, high costs, and often poor outcomes of care, there is limited understanding of the presentation, diagnostic strategies, and management of acute illness in older adults. In this paper, we present a strategy for the development of a research agenda at the intersection of hospital and geriatric medicine. This approach is informed by the Patient-Centered Outcomes Research Institute (PCORI) framework for identification and prioritization of research areas, emphasizing input from patients and caregivers. The framework’s four components are: 1) Topic generation, 2) Gap Analysis in Systematic Review, 3) Value of information (VOI) analysis, and 4) Peer Review. An inclusive process for topic generation requiring the systematic engagement of multiple stakeholders, especially patients, is emphasized. In subsequent steps, researchers and stakeholders prioritize research topics in order to identify areas that optimize patient-centeredness, population impact, impact on clinical decision making, ease of implementation, and durability. Finally, next steps for dissemination of the research agenda and evaluation of the impact of the patient-centered research prioritization process are described.
KEY WORDS: geriatrics, hospitals, hospitalists, patient-centered care, research
INTRODUCTION
As the population of the United States ages, the patient population in acute care hospitals has become older and more medically complex. Patients aged 65 years and older constitute 13 % of the population, but account for 37 % of hospital discharges and 43 % of hospital days.1 Older patients spend more time in the hospital with each admission (5.5 days) compared to younger patients (4.3 days).2 Caring for hospitalized older adults represents a major cost to society, accounting for over 43 % of annual spending on inpatient care.3,4 By 2030, the number of older adults will exceed 19 % of the US population and an even higher fraction of health care costs.5
For the older patient, hospitalization marks a period of high risk. One in 20 die during hospitalization and another 20–30 % die within 1 year following discharge.6 Hospitalized older adults are at risk for adverse drug events, nosocomial infections, and falls.7 A third of older patients are discharged more disabled than before admission.8 Despite these risks and associated costs, there is limited understanding of the presentation, diagnostic strategies, and management of acute illness in older patients. Principles of care for acutely ill frail elders have been implemented in model geriatric programs such as ACE (Acute Care for the Elderly), which are associated with modest improvements in selected outcomes such as length of stay and costs, but have limited application because of barriers such as staffing constraints.9 Given demographic trends and limitations of staffing and care delivery, acute care is increasingly skewed toward geriatric medicine in settings with limited access to geriatric medicine specialists and infrequent use of model geriatric programs.
During the same time that the acute care hospital population has become increasingly old and vulnerable, the nature of hospital care has changed. Hospital-based physicians or hospitalists, dedicated to providing acute hospital-based care, now number over 30,000 and work in 80 % of US hospitals.10 The Society for Hospital Medicine (SHM) provides a structure that has been an organizing force for this rapidly emerging specialty, and hospitalist involvement in geriatric care is becoming more prevalent. Between 1997 and 2006, the likelihood that a hospitalist would treat a hospitalized Medicare patient rose 29 % per year.11 Like other inpatient providers, hospitalists—the majority of whom trained in internal medicine—generally lack specialized training in geriatric medicine. Compounding this knowledge gap, a 2006 sample identified fewer than a dozen hospital medicine programs in the country offering specific approaches to address the care needs of hospitalized older adults.12 Anecdotally, hospitalist engagement with established geriatric care models may be growing.
Because of the growth of acute geriatric care and the limited database available to guide acute geriatric care, the authors of this paper—a subcommittee of SHM’s Research Committee—met in April 2012 to develop a process for creating a patient-centered, geriatric, and hospital medicine research agenda. This subcommittee was motivated by a ‘report card’ to SHM from the Association of Specialty Professors (ASP), an organization of specialty internal medicine divisions from the United States and Canada, which supports integrating geriatrics into the internal medical specialties.13 The report cards are routinely issued to national physicians’ organizations rating their organization’s efforts to incorporate geriatric-focused issues into organizational activities. ASP’s 2011 report card for SHM specifically identified the lack of a geriatric research agenda as a significant deficiency.
The subcommittee consists of two geriatrician-hospitalists, and three general internist-hospitalists, all with longstanding involvement with SHM. Four of the five participants are also funded health services researchers, each of whom researches conditions and practices relevant to hospitalized older adults. One is a member of the Patient-Centered Outcomes Research Institute (PCORI) methodology committee. The final member was SHM’s former geriatric interest group chair and liaison to ASP. The subcommittee produced a plan identifying and prioritizing research topics at the growing intersection of geriatric and hospital medicine that are informed by the increasing focus on patient-centeredness in medicine and biomedical research.
Patient-Centered Outcomes Research
Congress and the American public have identified the need for a medical research agenda that addresses questions most relevant to the concerns of patients and lay caregivers.14 PCORI, established by the Affordable Care Act, defined patient-centered outcomes research (PCOR) as “helping people and their [lay] caregivers communicate and make informed health care decisions, allowing their voices to be heard in assessing the value of health care options.”15 We use the term “caregiver” to refer to lay caregivers and the term “providers” to refer to members of the health care team (physicians, nurses, allied health professionals, social work, and direct care providers). Attributes of PCOR are identified in Box 1.
| Box 1: Attributes of Patient-Centered Outcomes Research (PCOR) (http://www.pcori.org/what-we-do/pcor/) |
| 1. Assesses the benefits and harms of preventive, diagnostic, therapeutic, palliative, or health delivery system interventions to inform decision making, highlighting comparisons and outcomes that matter to people; |
| 2. Is inclusive of an individual’s preferences, autonomy and needs, focusing on outcomes that people notice and care about such as survival, function, symptoms, and health related quality of life; |
| 3. Incorporates a wide variety of settings and diversity of participants to address individual differences and barriers to implementation and dissemination; and |
| 4. Investigates (or may investigate) optimizing outcomes while addressing burden to individuals, availability of services, technology, and personnel, and other stakeholder perspectives. |
Box 1 shows that PCOR is not exclusively about shared decision-making; in fact, older adults may prefer to be informed, but not responsible for medical decisions.16 However, a PCOR agenda for the hospitalized older adult population would be oriented to the unique needs of this population. For example, research addressing the benefits and harm of interventions (attribute 1) is needed, since the effectiveness of many common therapies has not been assessed in older patients because of frequent exclusion from therapeutic trials.17 Additionally, this population is vulnerable to harm related to medical care.18 Research inclusive of individuals’ preferences, autonomy, and needs (attribute 2) would incorporate knowledge of common cognitive impairments, functional impairments, and limited life expectancy in older patients. Such factors alter the risk-benefit ratio for common therapeutic interventions and complicate diagnostic evaluations and treatment decisions.8 Additionally, such research would examine outcomes of interest to the older population—such as functional status and quality of life—versus traditional outcomes such as 30-day mortality. Research with diverse participants (attribute 3) would account for atypical presentations of acute medical and surgical illness commonly seen in older adults19,20 and include patients with multimorbidity. Finally, research focusing on optimizing outcomes while addressing burden to individuals (attribute 4) might investigate optimization of systems and models of care that have been shown be beneficial to frail hospitalized older adults.21 A PCOR agenda for hospitalized older adults would result in an expanded clinical knowledge base for providers that is sensitive to the needs, concerns, and expectations of hospitalized older adults and their caregivers.
METHODS
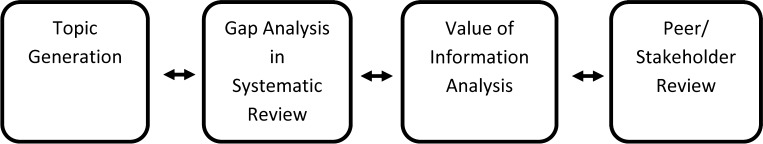
We adapted a framework developed by PCORI (Fig. 1) for identification and prioritization of research areas, focusing on inclusion of input from older patients and caregivers. The framework’s four components are: 1) Topic generation, 2) Gap Analysis in Systematic Review, 3) Value of information (VOI) analysis, and 4) Peer Review. Stakeholders are asked to consider: 1) patient-centeredness, 2) population impact, 3) impact on clinical decision-making (e.g. the research reduces uncertainty in making treatment decisions or provides new information about the balance of benefits versus harms), 4) ease of implementation, and 5) durability of information.22 Each component is discussed in detail below, with an emphasis on the process for topic generation.
Figure 1.
Schematic of the steps involved in research prioritization (adapted from the PCORI Methodology Report).28 The proposed methodology begins with a systematic and inclusive process for topic generation. The systematic engagement of multiple stakeholders, especially patients, is a critical component of topic generation. This is followed by a multistep prioritization beginning with systematic reviews and gap analysis to identify what is known, and what desirable knowledge is not known. The VOI analysis is a methodology used to identify the research questions with the greatest potential to improve population health. Finally, proposals addressing the high value research questions are subjected to peer and stakeholder review to ensure methodological rigor. Although these steps are depicted as linear, in practice, prioritization and reprioritization occur at all stages of the process. The integration of patient viewpoints is included at all stages of research prioritization.
Topic Generation
Traditionally, topic generation is the purview of researchers and funding organizations. One common scenario is to convene thought leaders, usually established researchers in the field, to identify research priorities. In contrast, we propose a multidisciplinary approach that incorporates input from older patients, their caregivers, and providers.
Participants
Topic generation requires forming a stakeholder partnership group that includes multiple stakeholders who are not researchers. Potential participants include representatives from: 1) patient and caregivers, 2) advocacy organizations for the elderly or organizations that address diseases common among hospitalized older patients, 4) post-acute care providers, and 4) third party payers.
Health services and clinical researchers should participate in the steering committee. Provider participation should include practicing hospitalists, primary care physicians who provide inpatient care for geriatric patients, subspecialists representing a selection of relevant subspecialties, and allied health professions (such as nursing, pharmacy, physical and occupational therapies, and social workers).
Strategy for stakeholder involvement: We propose a collaborative and consultative approach to public engagement, drawing heavily from the published work of the James Lind Alliance (JLA)—an initiative promoting patient–clinician partnerships in health research based in the United Kingdom.23 The approach includes five phases: 1) organizations and representatives are identified and invited to join a steering committee; 2) stakeholder organizations generate ideas for research topics, soliciting input from members to identify gaps in scientific knowledge regarding the care of the acutely ill older patient; 3) preparation of a list of potential research questions resulting from the solicitation process; 4) stakeholders prioritize the most important research questions, often in a face-to-face meeting; 5) the prioritized list is disseminated to stakeholders and funding agencies. In this manner, the stakeholders provide their unique perspectives, experiences, knowledge, preferences, and ideas.
Systematic Review and Gap Analysis
After the topic generation process, we propose using the Agency for Health Research and Quality (AHRQ)s Future Research Needs (FRN) process.24 The FRN process begins with systematic literature reviews conducted in high priority areas that are subsequently used as the basis for generating input from patient and provider stakeholders.
Research Prioritization: VOI Analysis
Given the volume of potential research questions generated by the first two steps, it may be necessary to further prioritize research projects for funding. VOI Analysis identifies research priorities by quantifying the expected improvement in population health that the proposed research may yield, thereby providing guidance for decisions about which systematic reviews to charter and/or what studies to fund. VOI analysis quantifies elements such as the difference in health benefits and reduction in uncertainty produced by the research, the likelihood that the findings can be implemented, the durability of the information gained, and the size of the impacted patient population.25 Although some VOI approaches may be too burdensome to apply to some research topics, newer VOI methods and algorithms have been developed that are easier to apply26 and help identify which VOI method may be most appropriate for a potential research topic.25 VOI analysis will need to be conducted by experienced centers and with the funding of federal or private partners.
Peer/Stakeholder Review
The ideal outcome produced by the above activities is a set of questions that can be addressed by new research proposals. The identified research questions should be disseminated to funding agencies, foundations, and/or professional societies who solicit and fund research proposals.
Peer review may be the most common process used for selecting meritorious research projects for funding. However, peer review methodologies have not been standardized and their effectiveness may be limited if relevant stakeholders, such as patients or their advocates, are excluded. A lack of diversity with regard to race and socioeconomic status of reviewers, or conflicts of interests between reviewers and those being reviewed, are additional factors limiting traditional peer review. Therefore, it is anticipated that the proposed peer review processes will incorporate the views of diverse stakeholders, as endorsed by PCORI.27
DISSEMINATION
Dissemination and implementation are complementary because effective dissemination of a research agenda should result in adoption by funding agencies, funded research projects, implementation, and improved health outcomes for older adults. The following components would be important for these efforts:
Research funding: Important sources of funding for established researchers will be from PCORI, the National Institutes of Health, the Agency for Healthcare Research and Quality, and private foundations such as the John A. Hartford Foundation (http://www.jhartfound.org/). Programs that foster early-career researchers include the Grants for Early Medical/Surgical Subspecialists’ Transition to Aging Research (GEMSSTAR) program and its companion, the T. Franklin Williams Scholars program.28, 29 GEMSSTAR is an RO3 mechanism offered by the National Institute on Aging (NIA) for internal medicine and surgical subspecialists (including hospitalists). The T. Franklin Williams Scholars program is one of several mechanisms that provide companion career development awards to GEMSSTAR awardees through organizational partnerships.
Meetings & Publications: Publications and meetings would remain important venues for dissemination of this work.
On-line content and communities: The Portal of Geriatric Online Education (www.pogoe.org) brings together diverse resources for geriatrics providers. It aggregates critically appraised papers in the field, clinical resources such as tools to improve discharge summaries, and educational curricula to better inform clinicians. Additionally, learning communities or geriatric care collaboratives could be important dissemination tools.
Social media: Social Media could be an important mechanism for linking providers and patient and caregiver communities for dissemination of best care practices for hospitalized older adults.
Policy: Changes in policy regarding inpatient geriatric care may include the development of quality or performance measures that provide a mechanism for increasing evidence based and newly developed standards of care. Engagement of the policy and practice communities through already established channels, such as Academy Health or the American Board of Internal Medicine’s Choosing Wisely campaign, could facilitate dissemination efforts.
Healthcare system uptake: Uptake of evidence-based best practices regarding the care of hospitalized older persons would be critical to a dissemination program. Collaboration with health systems during evaluation and dissemination activities would ensure that hospitalized older adults directly benefit from care improvements.
Recognized dissemination frameworks should guide these efforts. We think that RE-AIM (Reach, Efficacy, Adoption, Implementation, and Maintenance) and PARiHS (Promoting Action on Research Implementation in Health Services) are most relevant to implementing evidence-based geriatrics care in the hospital because of their health service focus.
RE-AIM defines program elements that maximize sustainable adoption and provides two significant insights at the intersection of geriatrics and hospital medicine. First, research must include aspects of evaluation that inform a dissemination strategy. This may include formative evaluation that explores the impact of organizational context, perceptions, and the input of stakeholders. Second, research must be relevant to the population of hospitalized older adults and practicing hospitalists across a broad range of inpatient settings.
PARiHS considers research evidence, the local context, and facilitating factors in the implementation of research findings. Similar to the RE-AIM framework, it emphasizes a ongoing evaluation to best inform intervention effectiveness.
EVALUATION
We propose a multi-pronged and multi-year approach to evaluate a hospital medicine-geriatric medicine research initiative to improve outcomes for hospitalized older adults. A comprehensive assessment would include the impact of the research initiative on geriatric and hospital medicine research communities, practicing hospitalists, other physicians with inpatient practices, and geriatric patients and their caregivers. The evaluation would include an assessment of the research impact on efficacy and effectiveness over time. Based on the dissemination components described above, the following areas could be considered as evaluation criteria:
Growth in research funding
Increased content on care of hospitalized older adults at regional and national meetings of clinical practitioners and researchers
Increased publication of articles on care of hospitalized older adults in relevant journals such as the Journal of Hospital Medicine, Journal of General Internal Medicine, and those of related subspecialty societies
Increased focus on acute care of hospitalized older patients by providers, policy makers, and patient safety organizations. Content could be assessed in terms of webpages, publically reported performance measures, and national initiatives
Increased adoption of care models most relevant to hospitalized older adults21
Changes in outcomes of care for traditional metrics such as costs, complication rates, and readmission rates and changes for patient-centered metrics such as functional status, quality of life, and patient care experiences.
LIMITATIONS
The ultimate goal of the proposed research-agenda setting process is improving the health of hospitalized older adults, with patients as the centerpiece of the research process. The research agenda will optimize patient-centeredness, population impact, impact on clinical decision-making, ease of implementation, and durability. Potential limitations to this process include the risk that diverse stakeholders will not participate and their exclusion from the process may skew priorities towards or away from a given research area. Secondly, the process does not strictly define how stakeholders should weigh the criteria to prioritize a set of questions. For example, is patient-centeredness more important than population impact? Third, certain criteria such as durability are more challenging to assess, may not be fully anticipated prior to implementation, and may require years to evaluate. Finally, using a patent-centered approach means that research that may be highly relevant to policy makers, educators, or researchers may not be fully reflected during this prioritization process. These stakeholders, however, will be included in the process, and should be able to shape the discussion that includes their viewpoints.
Fundamentally, this process does not make a determination about the value of additional research in the care of hospitalized older adults relative to the amount of research already conducted in this area and the broader research needs of hospitalized older adults and the population at large. To the extent that care of hospitalized older adults has been addressed by previous research and has not been adequately implemented, the proposed methodology may address this gap by generating prioritized topics in implementation science. Limited resources preclude funding all deserving research topics. Funders will need to identify societal needs and assess this agenda against additional meritorious research topics when determining funding priorities.
CONCLUSIONS
Several forces are shaping the future of acute inpatient care. Changing demographics of the hospitalized patient population, along with a rapid increase in the proportion of multi-morbid hospitalized older adults, an inpatient workforce (hospitalists, generalists and subspecialists) with inadequate geriatrics training, and gaps in evidence-based guidance to inform diagnostic and therapeutic decision-making for acutely ill older patients, are all at play. Finally, there is growing recognition that patients and other stakeholders deserve a greater voice in determining the direction of research. The road map drawn in this paper can be used to address the growing need for a patient-centered research agenda at the intersection of hospital medicine and geriatric medicine. In so doing, we have relied heavily on the framework proposed by PCORI, and outline a process that begins with inclusive topic generation, followed by systematic review and gap analysis, VOI analysis, and peer review. Additionally, we have proposed a dissemination and evaluation strategy. We believe the adoption of this methodology will create a knowledge base that is rigorously derived and most relevant to the care of hospitalized older adults and their families. Its application will ultimately result in improved outcomes for hospitalized older adults.
Acknowledgements
Contributors
Claudia Stahl, Society of Hospital Medicine; Angela Richard, Brian Bandle, and Julie Slater, University of Colorado School of Medicine.
Funders
This work was supported by the American Association of Instructors of Medicine/ Association of Specialty Providers, and the John A. Hartford Foundation. Dr. Wald is supported by a Paul Beeson Career Development Award in Aging (NIA 5 K23 AG034544). Dr. Mattison acknowledges the support of Rx Foundation. This work was also supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (REA 05–129, CDA 07–022). Investigator salary support (to Dr. Leykum) is provided through this funding, and through the South Texas Veterans Health Care System. Dr. Vasilevskis was supported by the National Institute On Aging of the National Institutes of Health (K23AG040157) and the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research, Education and Clinical Center (GRECC).
Prior Presentations
None.
Conflict of Interest Summary
Wald: none; Leykum: none; Mattison: UpToDate (contributor), Practical Reviews in Hospital Medicine (contributor/reviewer); Vasilevskis: none; Meltzer: PCORI Methodology Committee (member).
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institutes of Health or the Department of Veterans Affairs.
REFERENCES
- 1.Hall M, DeFrances C, Williams S, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Hyattsville: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 2.DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. National Center for Health Statistics. VitalHealthStat13(165). 2007. http://www.cdc.gov/nchs/data/series/sr_13/sr13_165.pdf#table1. Accessed December 18, 2013. [PubMed]
- 3.Wier, L.M., (Thomson Reuters), Pfuntner, A. (Thomson Reuters), and Steiner, C. (AHRQ). Hospital Utilization among Oldest Adults, 2008. HCUP Statistical Brief #103. December 2010. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb103.pdf. Accessed December 18, 2013.
- 4.Wier LM (Thomson Reuters), Pfuntner A (Thomson Reuters), Maeda J (Thomson Reuters), Stranges E (Thomson Reuters), Ryan K (Thomson Reuters), Jagadish P (AHRQ), Collins Sharp B (AHRQ), Elixhauser A (AHRQ). HCUP Facts and Figures: Statistics on Hospital-based Care in the United States, 2009. Rockville, MD: Agency for Healthcare Research and Quality, 2011 (http://www.hcup-us.ahrq.gov/reports.jsp). Accessed December 18, 2013.
- 5.Centers for Disease Control and Prevention. [Public health and aging, trends in aging.]. MMWR 2003;52:[101–106]. http://www.cdc.gov/MMWR/preview/mmwrhtml/mm5206a2.htm. Accessed December 19, 2013.
- 6.Covinsky K, Palmer R, Fortinsky R, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 7.Creditor MC. Hazards of Hospitalization of the Elderly. Ann Intern Med. 1993;118(3):219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 8.Landefeld CS. Improving health care for older persons. Ann Intern Med. 2003;139:421–424. doi: 10.7326/0003-4819-139-5_Part_2-200309021-00008. [DOI] [PubMed] [Google Scholar]
- 9.Landefeld CA, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–44. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 10.Society of Hospital Medicine. Text on Hospital Medicine for Use on Websites and Newsletters. http://www.hospitalmedicine.org/AM/Template.cfm?Section = Home&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID = 23498. Accessed December 19, 2013.
- 11.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112. doi: 10.1056/NEJMsa0802381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wald H, Huddleston J, Kramer A. Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs. J Hosp Med. 2006;1(1):29–35. doi: 10.1002/jhm.9. [DOI] [PubMed] [Google Scholar]
- 13.Alliance for Academic Internal Medicine. Association of Specialty Professors. http://www.im.org/About/AllianceSites/ASP/Pages/Default.aspx/. Published 2012. Accessed December 19, 2013.
- 14.Eden J, Wheatley B, McNeil B, Sox H, Eds. Knowing What Works in Health Care: A Roadmap for the Nation. Washington, D.C. The National Academies Press; 2008.
- 15.Patient-Centered Outcomes Research Institute. Patient-Centered Outcomes Research. Patient-Centered Outcomes Research Institute. http://www.pcori.org/research-we-support/pcor/. Published March 5, 2012. Last accessed December 18, 2013.
- 16.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. J Gen Intern Med. 2005;20(6):531–5. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zulman DM, Sussman JB, Chen X, Cigolle CT, Blaum CS, Hayward RA. Examining the evidence: a systematic review of the inclusion of older adults in randomized controlled trials. J Gen Intern Med. 2011;26(7):783–90. doi: 10.1007/s11606-010-1629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Long SJ, Brown KF, Ames D, Vincent C. What is known about adverse events in older medical hospital inpatients? A systematic review of the literature. Int J Qual Health Care. 2013. doi:10.1093/intqhc/mzt056. [DOI] [PubMed]
- 19.Canto JG, Fincher C, Kiefe CI, et al. Atypical presentations among medicare beneficiaries with unstable angina pectoris. Am J Cardiol. 2002;90(3):248–253. doi: 10.1016/S0002-9149(02)02463-3. [DOI] [PubMed] [Google Scholar]
- 20.Storm-Dickerson TL, Horattas MC. What have we learned over the past 20 years about appendicitis in the elderly? Am J Surg. 2003;185:198–201. doi: 10.1016/S0002-9610(02)01390-9. [DOI] [PubMed] [Google Scholar]
- 21.Boult C, Green AF, Boult LB, Pacala JT, Snyder C, Leff B. Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine’s “retooling for an aging America” report. J Am Geriatr Soc. 2009;57(12):2328–37. doi: 10.1111/j.1532-5415.2009.02571.x. [DOI] [PubMed] [Google Scholar]
- 22.PCORI (Patient-Centered Outcomes Research Institute) Methodology Committee. 2013. “The PCORI Methodology Report”. http://www.pcori.org/assets/2013/11/PCORI-Methodology-Report.pdf. Accessed December 19, 2013.
- 23.The James Lind Alliance. JLA Method. http://www.lindalliance.org/JLA_Method.asp. Accessed December 19, 2013.
- 24.Carey T, Sanders GD, Viswanathan M, Trikalinos TA, Kato E, Chang S. Framework for Considering Study Designs for Future Research Needs. Methods Future Research Needs Paper No. 8 (Prepared by the RTI–UNC Evidence-based Practice Center under Contract No. 290–2007–10056-I.) AHRQ Publication No. 12–EHC048-EF. Rockville, MD: Agency for Healthcare Research and Quality. March 2012. http://www.effectivehealthcare.ahrq.gov/search-for-guides-reviews-and-reports/?pageaction = displayProduct&productID = 1001. Accessed December 19, 2013. [PubMed]
- 25.Hoomans T, Seidenfeld J, Basu A, Meltzer D. Systematizing the Use of Value of Information Analysis in Prioritizing Systematic Reviews. (Prepared by the University of Chicago Medical Center through the Blue Cross and Blue Shield Association Technology Evaluation Center Evidence-based Practice Center under Contract No. 290–2007–10058.) AHRQ Publication No. 12–EHC109-EF. Rockville, MD: Agency for Healthcare Research and Quality. August 2012. http://effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports/?productid = 1210&pageaction = displayproduct. Accessed December 19, 2013.
- 26.Meltzer DO, Hoomans T, Chung JW, Basu A. Minimal modeling approaches to value of information analysis for health research. Published online before print June 28, 2011. Med Decis Making. 2011;31(6):E1–E22. doi: 10.1177/0272989X11412975. [DOI] [PubMed] [Google Scholar]
- 27.PCORI (Patient Centered Outcomes Research Institute) Methodology Committee. 2013. The PCORI Methodology Report. http://www.pcori.org/research-we-support/research-methodology-standards/Update. November 19, 2013. Last accessed December 19, 2013.
- 28.NIA GEMSSTAR/ AAIM-ASP T. Franklin Williams Scholars Award http://www.im.org/AcademicAffairs/Aging/Pages/2014NIAGEMSSTAR.aspx. Last accessed December 19, 2013.