Abstract
Purpose
Survivorship care planning should involve discussions between providers and cancer survivors to address survivors' needs and optimize adherence. We examined the frequency and factors associated with oncologists' and primary care physicians' (PCPs) reports of provision of written survivorship care plans (SCPs) and discussion of survivorship care recommendations with survivors.
Methods
A nationally representative sample of 1,130 oncologists and 1,020 PCPs was surveyed about survivorship care practices with survivors. Logistic regression models predicted multilevel factors associated with providing SCPs or discussing recommendations with survivors.
Results
Although a majority of oncologists (64%) reported always/almost always discussing survivorship care recommendations with survivors, fewer also discussed who survivors should see for cancer-related and other follow-up care (32%); fewer still also provided a written SCP to the survivor (< 5%). Survivorship care recommendations and provider responsibility were not regularly discussed by PCPs and survivors (12%). Oncologists who reported detailed training about late and long-term effects of cancer were more likely to provide written SCPs (odds ratio [OR], 1.73; 95% CI, 1.22 to 2.44) and discuss survivorship care planning with survivors (OR, 2.02; 95% CI, 1.51 to 2.70). PCPs who received SCPs from oncologists were 9× more likely (95% CI, 5.74 to 14.82) to report survivorship discussions with survivors.
Conclusion
A minority of both PCPs and oncologists reported consistently discussing and providing SCPs to cancer survivors. Training and knowledge specific to survivorship care and coordinated care between PCPs and oncologists were associated with increased survivorship discussions with survivors. These nationally representative data provide a useful benchmark to assess implementation of new efforts to improve the follow-up care of survivors.
INTRODUCTION
There are approximately 14 million cancer survivors in the United States, and this number is projected to increase substantially with the aging of the population and improvement of survival rates.1,2 Survivors, most of whom will live years after cancer treatment, have unique health care needs,3,4 including prevention or management of chronic and late physical and psychosocial effects of treatment and comorbid conditions. Survivorship care planning has been proposed as a way to meet these needs.4
The Institute of Medicine report “From Cancer Patient to Cancer Survivor: Lost in Transition” recommends that all survivors completing primary treatment receive a survivorship care plan (SCP), including a written treatment summary and an individualized follow-up plan, from their oncology provider.4 Recommendations suggest that survivorship care planning should also include discussions with survivors about care recommendations and delineation of which provider (eg, oncologist, primary care physician [PCP], or other specialist) is responsible for overseeing cancer-related and other medical follow-up.4,5 By 2015, the American College of Surgeons Commission on Cancer will require provision of written SCPs to survivors on treatment completion.6 Other major cancer organizations also promote SCPs.5,7,8 The language surrounding these recommendations, standards, and resources all suggest their intended target is the survivor. Involving survivors in survivorship care planning may promote shared decision making, self-management, and patient engagement, which are associated with positive patient outcomes, including adherence to treatment recommendations.9–11
Because many survivors transition from oncologists to PCPs for a large portion of their post-treatment care,12 optimal communication about survivorship care planning with survivors should also involve the survivor's PCP.13 Cancer survivors look to follow-up care plans to aid in care coordination and reduce conflicting advice.3 PCP-survivor discussions of survivorship care planning may increase the likelihood that survivors receive comprehensive and nonduplicative follow-up care.14,15
Despite recommendations and the presumed utility of SCPs, they have not been universally adopted. Of 53 National Cancer Insitute cancer centers, only 43% report implementing SCPs for some or all of their cancer survivors.3 Many recently diagnosed survivors report not receiving treatment summaries (62%) or written follow-up instructions (42%).16 National estimates of discussions of SCPs with the survivor by practicing oncologists or PCPs are lacking. We used a nationally representative survey of oncologists and PCPs to assess the self-reported frequency of: oncologists' provision of written SCPs to survivors, oncologists' discussion of care recommendations and delineation of provider responsibility for survivorship care with survivors, and PCPs' discussion of care recommendations and provider responsibility with survivors. Additionally, we explored multilevel factors associated with providing SCPs or discussing survivorship care with survivors, including factors related to individual physicians, perception of difficulties providing care to survivors, care coordination with other physicians, and practice environment.
METHODS
Survey and Sample Description
This study used data from the Survey of Physicians' Attitudes Regarding the Care of Cancer Survivors (SPARCCS), a 2009 nationally representative mailed survey completed by 1,130 oncologists and 1,072 PCPs about practices and attitudes regarding post-treatment follow-up care for breast and colon cancer survivors. Approval was obtained from the National Institutes of Health Human Research Protections Program and the US Office of Management and Budget. Most survey items were adapted from previous physician surveys.17–20 For the complete survey, visit http://healthservices.cancer.gov; detailed methods have been published elsewhere.21
Eligible physicians were identified from the American Medical Association (AMA) Physician MasterFile using stratified sampling across specialty, age, sex, census region, metropolitan statistical area, and mail-undeliverable status. We excluded PCPs who reported never having seen a breast or colon cancer survivor in clinical practice (n = 51) or who reported practicing outside primary care (n = 1). The absolute response rate was 57.5%; responders did not significantly differ from nonresponders on any variables examined.21
Measures
Oncologists reported how often they provided survivors with a written SCP summarizing past treatments and recommendations for future care and surveillance. Additionally, to assess discussion of follow-up care with survivors, both PCPs and oncologists responded to three items: one regarding discussion of survivorship care recommendations (“How often do you have a specific discussion with the patient regarding recommendations for future care and surveillance?”) and two regarding delineation of provider responsibilities for survivorship care (“How often do you discuss with your patient which physician will follow them for their cancer?” and “How often do you discuss with your patient which physician will handle any other medical issues?”).22 Responses were dichotomized as always/almost always versus less than always.
Four outcome variables were created: (1) oncologists' provision of written SCPs to survivors; (2) oncologists' discussion of recommendations and delineation of provider responsibility for survivorship care (cancer-related and other medical issues) with survivors; (3) PCPs' discussion of recommendations and provider responsibility with survivors; and (4) oncologists' provision of a written SCP and discussion of recommendations/responsibilities for survivorship care (combination of outcomes one and two). Because of the small number of oncologists who reported both providing a written SCP and discussing recommendations/responsibilities for survivorship care with survivors, we examined prevalence but did not model outcome four. Outcome variables were dichotomized as reporting always/almost always on all questions versus less than almost always for any question.
Physician, Survivor, Care Coordination, and Practice Environment Factors
To comprehensively assess factors associated with survivorship care planning at multiple levels, we included factors chosen a priori representing: (1) physicians; (2) difficulties encountered in care interactions with survivors; (3) follow-up care coordination with other physicians; and (4) practice environment, as suggested by the social ecologic model.23–25
Physician factors.
Physicians indicated their race/ethnicity, specialty, frequency with which they ordered tests or treatments for cancer survivors to protect from malpractice litigation, and training regarding the late and long-term effects of cancer.21 PCPs reported frequency of problems caring for survivors related to inadequate knowledge; this item was not included for oncologists, given the limited distribution of responses. Physician age and sex were obtained from the AMA MasterFile.
Difficulties encountered in care interactions.
Physicians reported the frequency of encountering the following difficulties when caring for breast and colon cancer survivors: “patients refuse or do not adhere to recommended care”; “patients have language barriers that interfere with communication”; “patients are unable to pay (or lack insurance coverage) for follow-up care”; and “patients request more aggressive cancer surveillance or testing than I would recommend.”
Follow-up care coordination factors.
Physicians indicated their preferred model of survivorship care,17,21 categorized according to preferred role: own responsibility, shared responsibility, or someone else has responsibility.26,27 Physicians indicated the extent to which the following problems were encountered while caring for survivors: difficulties transferring patient care responsibilities, uncertainty about which physician is providing survivors' general preventive health care, concerns over missed care, and concerns over duplicate care.28 PCPs also reported the frequency of receipt of written SCPs from survivors' oncologists.22,27
Practice environment factors.
Providers reported the overall number of patients seen per week, number of patients with breast or colon cancer seen, percentage of patients uninsured/insured by Medicaid, number of physicians in their practice, medical records system used, percentage of time spent in patient care, and whether they are paid by salary based on productivity. Metropolitan statistical area was obtained from the AMA MasterFile.
Data Analysis
All analyses were conducted in SUDAAN (version 10.0.1; http://www.rti.org/sudaan/) and incorporated sampling weights to account for complex survey design and nonresponse. Estimates represent the entire population of practicing medical oncologists and PCPs. Because analyses were based on multiple levels of influence as indicated by the social ecological theory, three stepwise multiple logistic regressions were used to model factors associated with: (1) oncologists' provision of written SCPs to survivors; (2) oncologists' discussion of recommendations and provider responsibility for survivorship care with survivors; and (3) PCPs' discussion of recommendations and provider responsibility for survivorship care with survivors. To maximize the amount of variance explained while simultaneously minimizing the number of variables in the model, potential covariates were entered into regression models in four stepwise blocks (representing levels of social ecological influence: physician factors, difficulties encountered in care, care coordination factors, practice environment factors). For each block, the least significant items were iteratively removed until all remaining variables in the block were significant. Significant variables from previous blocks that became nonsignificant when additional blocks were entered were retained in the model. Wald statistics tested the contribution of individual factors in the model building and final model.
RESULTS
Oncologists were slightly younger and more likely to be Asian and male compared with PCPs (Table 1). PCPs reported less training regarding late or long-term effects of cancer treatment, greater preference for shared care or someone else taking responsibility for survivorship care, less use of electronic medical records, and smaller practice sizes. PCPs spent a greater percentage of time on patient care but saw on average 37 patients with breast or colon cancer per year, as opposed to 35 per week seen by oncologists.
Table 1.
Characteristics of Oncologists and PCPs
| Characteristic | PCPs |
Oncologists |
P | ||||
|---|---|---|---|---|---|---|---|
| No. | % | 95% CI | No. | % | 95% CI | ||
| Physician Characteristics | |||||||
| Sex | < .001 | ||||||
| Male | 679 | 64.2 | 61.5 to 66.7 | 837 | 72.9 | 70.4 to 75.2 | |
| Female | 341 | 35.8 | 33.3 to 38.5 | 293 | 27.1 | 24.8 to 29.6 | |
| Race/ethnicity | < .001 | ||||||
| Non-Hispanic white | 710 | 70.7 | 67.7 to 73.5 | 726 | 62.7 | 60.2 to 65.1 | |
| Asian | 174 | 15.1 | 13.2 to 17.3 | 299 | 28.2 | 25.9 to 30.6 | |
| Other | 136 | 14.2 | 11.9 to 16.9 | 105 | 9.1 | 7.7 to 10.7 | |
| Age, years | .003 | ||||||
| Mean | 48.3 | 47.2 | |||||
| SE | 0.3 | 0.2 | |||||
| Specialty | — | ||||||
| General internal medicine | 480 | 37.8 | 36.2 to 39.4 | — | — | — | |
| Family medicine | 458 | 43.4 | 42.0 to 44.9 | — | — | — | |
| Obstetrics-gynecology | 82 | 18.7 | 17.3 to 20.3 | — | — | — | |
| Medical oncology | — | — | — | 553 | 47.8 | 44.6 to 50.9 | |
| Hematology/oncology | — | — | — | 566 | 51.3 | 48.1 to 54.4 | |
| Other (hematology, radiation oncology, surgical oncology) | — | — | — | 11 | 1.0 | 0.6 to 1.7 | |
| Received training regarding late or long-term effects of cancer treatment | < .001 | ||||||
| No | 329 | 34.3 | 31.1 to 37.7 | 83 | 7.1 | 5.9 to 8.5 | |
| Yes, somewhat | 627 | 60.2 | 56.7 to 63.6 | 637 | 56.7 | 53.7 to 59.6 | |
| Yes, in detail | 48 | 4.2 | 3.1 to 5.8 | 406 | 35.9 | 33.1 to 38.8 | |
| Order tests and treatments to protect from malpractice litigation | < .001 | ||||||
| Never or rarely | 473 | 46.5 | 43.3 to 49.6 | 663 | 58.7 | 55.6 to 61.7 | |
| Sometimes, often, or always/almost always | 500 | 48.6 | 45.3 to 51.9 | 445 | 39.4 | 36.5 to 42.4 | |
| Problems caring for cancer survivors related to inadequate knowledge | < .001 | ||||||
| Never or rarely | 545 | 51.1 | 47.4 to 54.8 | 968 | 85.8 | 83.7 to 87.7 | |
| Sometimes, often, or always/almost always | 430 | 44.2 | 40.8 to 47.6 | 116 | 10.0 | 8.3 to 12.1 | |
| Difficulties Encountered in Care Interactions | |||||||
| Patient nonadherence | .086 | ||||||
| Never or rarely | 385 | 39.4 | 36.0 to 42.9 | 413 | 36.2 | 33.0 to 39.6 | |
| Sometimes, often, or always/almost always | 613 | 58.1 | 54.6 to 61.6 | 700 | 62.3 | 58.9 to 65.6 | |
| Language barriers | .011 | ||||||
| Never or rarely | 797 | 77.4 | 74.2 to 80.3 | 826 | 72.7 | 69.8 to 75.5 | |
| Sometimes, often, or always/almost always | 195 | 19.5 | 16.6 to 22.9 | 281 | 25.2 | 22.3 to 28.3 | |
| Patients unable to pay | .741 | ||||||
| Never or rarely | 346 | 34.2 | 31.0 to 37.7 | 379 | 33.7 | 30.6 to 36.9 | |
| Sometimes, often, or always/almost always | 647 | 62.5 | 58.9 to 66.0 | 726 | 63.7 | 60.5 to 66.8 | |
| Patients request more aggressive surveillance | < .001 | ||||||
| Never or rarely | 451 | 44.6 | 41.7 to 47.6 | 283 | 24.3 | 21.9 to 26.9 | |
| Sometimes, often, or always/almost always | 529 | 50.7 | 47.7 to 53.7 | 833 | 74.4 | 71.8 to 76.8 | |
| Follow-Up Care Coordination | |||||||
| Preferred model of survivorship care | < .001 | ||||||
| Shared responsibility | 407 | 37.3 | 34.2 to 40.5 | 182 | 16.0 | 14.1 to 18.1 | |
| My responsibility | 103 | 9.3 | 7.7 to 11.3 | 643 | 56.5 | 53.1 to 59.7 | |
| Someone else's responsibility | 428 | 45.8 | 42.7 to 48.9 | 263 | 23.9 | 21.3 to 26.6 | |
| Difficulties transferring patient care responsibilities | < .001 | ||||||
| Never or rarely | 577 | 58.7 | 55.4 to 61.9 | 405 | 36.4 | 33.4 to 39.5 | |
| Sometimes, often, or always/almost always | 423 | 39.3 | 36.2 to 42.5 | 707 | 62.1 | 59.1 to 65.0 | |
| Uncertainty about who should provide general preventive care | < .001 | ||||||
| Never or rarely | 686 | 65.0 | 61.8 to 68.2 | 637 | 56.4 | 53.4 to 59.4 | |
| Sometimes, often, or always/almost always | 311 | 32.3 | 29.0 to 35.7 | 470 | 41.4 | 38.5 to 44.4 | |
| Concern over missed care | .128 | ||||||
| Never or rarely | 414 | 41.3 | 38.2 to 44.5 | 437 | 39.0 | 36.1 to 42.0 | |
| Sometimes, often, or always/almost always | 555 | 53.7 | 50.6 to 56.8 | 666 | 58.6 | 55.6 to 61.7 | |
| Concern over duplicate care | < .001 | ||||||
| Never or rarely | 502 | 50.8 | 47.4 to 54.1 | 483 | 43.2 | 40.2 to 46.3 | |
| Sometimes, often, or always/almost always | 491 | 46.2 | 42.9 to 49.5 | 628 | 55.0 | 51.9 to 58.1 | |
| Receive SCPs from oncologists | — | ||||||
| Less than always/almost always | 873 | 85.1 | 82.2 to 87.7 | — | — | — | |
| Always/almost always | 133 | 13.4 | 11.0 to 16.1 | — | — | — | |
| Practice Environment | |||||||
| No. of breast and colon cancer survivors seen per year (PCPs) or per week (oncologists) | — | ||||||
| Mean | 37.2 | 47.2 | |||||
| SE | 1.4 | 0.8 | |||||
| Percent of time spent in patient care | < .001 | ||||||
| Mean | 88.7 | 82.1 | |||||
| SE | 0.4 | 0.6 | |||||
| Medical record system used | < .001 | ||||||
| Paper records | 388 | 40.0 | 37.1 to 43.0 | 247 | 21.7 | 19.2 to 24.5 | |
| Partial or transitioning to electronic records | 288 | 27.8 | 24.8 to 31.0 | 498 | 43.6 | 40.8 to 46.4 | |
| Full electronic records | 327 | 30.7 | 27.7 to 33.8 | 375 | 33.4 | 30.7 to 36.3 | |
| Percentage of patients uninsured/insured by Medicaid | .030 | ||||||
| ≤ 10 | 382 | 37.1 | 34.0 to 40.3 | 361 | 31.1 | 28.4 to 33.9 | |
| ≥ 11 | 606 | 60.2 | 56.8 to 63.4 | 699 | 61.8 | 58.6 to 64.8 | |
| No. of physicians in practice | < .001 | ||||||
| 1 | 253 | 24.1 | 21.5 to 26.9 | 122 | 10.1 | 8.4 to 12.1 | |
| 2-5 | 422 | 42.8 | 39.4 to 46.2 | 436 | 39.2 | 36.4 to 42.1 | |
| 6-15 | 223 | 21.9 | 19.1 to 24.9 | 339 | 29.6 | 26.9 to 32.4 | |
| ≥ 16 | 103 | 9.5 | 7.7 to 11.6 | 212 | 19.2 | 17.0 to 21.6 | |
| Salary based on productivity | .341 | ||||||
| Yes | 355 | 33.5 | 30.3 to 36.8 | 387 | 34.0 | 31.2 to 37.0 | |
| No | 635 | 63.7 | 60.4 to 66.9 | 666 | 59.2 | 56.2 to 62.0 | |
| MSA* | .012 | ||||||
| Population ≥ 1 million | 622 | 61.5 | 59.1 to 63.8 | 728 | 65.6 | 63.1 to 67.9 | |
| All others | 398 | 38.5 | 36.2 to 40.9 | 402 | 34.4 | 32.1 to 36.9 | |
Abbreviations: MSA, metropolitan statistical area; PCP, primary care physician; SCP, survivorship care plan.
From American Medical Association MasterFile.
Frequency of Discussion of Survivorship Care and Provision of Written SCPs
Nearly two thirds of oncologists reported always/almost always discussing survivorship care recommendations with survivors (64.0%; 95% CI, 61.3 to 66.7; Fig 1). Approximately half reported always/almost always discussing with survivors which physician would follow them for their cancer care (50.0%; 95% CI, 46.8 to 53.2) or which physician would handle other medical issues (42.2%; 95% CI, 38.9 to 45.6). However, only approximately one third of oncologists reported always/almost always discussing with survivors recommendations for survivorship care and provider responsibility for cancer and other medical follow-up (31.7%; 95% CI, 28.8 to 34.6).
Fig 1.
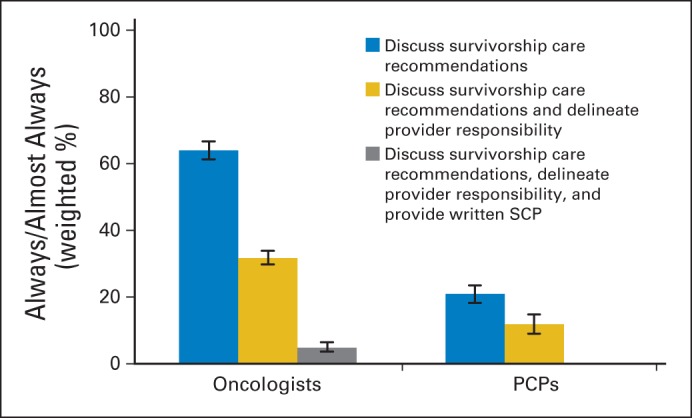
Oncologists and primary care physicians (PCPs) reporting discussion of survivorship care and provision of survivorship care plans (SCPs) to survivors.
Less than 10% of oncologists reported always/almost always providing a written SCP to survivors (9.6%; 95% CI, 8.0 to 11.5). Moreover, less than 5% of oncologists reported always/almost always giving survivors a written document and having discussions of survivorship recommendations and provider responsibility with survivors (4.8%; 95% CI, 3.6 to 6.4).
For PCPs, 21% (95% CI, 18.5 to 23.8) reported always/almost always discussing recommendations for survivorship care with survivors; 34% (95% CI, 31.1 to 37.3) reported always/almost always discussing with survivors which physician would follow them for their cancer; 33% (95% CI, 30.4 to 35.8) reported discussing which physician would handle other medical issues. However, only 12% (95% CI, 10.0 to 14.1) of PCPs reported always/almost always discussing all three items with survivors.
Factors Associated With Oncologists' Provision of SCPs and Discussion of Recommendations and Provider Responsibilities
Oncologists who reported detailed training regarding late and long-term effects of cancer were more likely to report always/almost always providing written SCPs to survivors (odds ratio [OR], 1.73; 95% CI, 1.22 to 2.44; Table 2). Compared with non-Hispanic white oncologists, those of other racial/ethnic groups were more likely to provide written SCPs to survivors (Wald F = 8.80; P < .001). Oncologists who reported that their patients requested more aggressive cancer surveillance or testing than they would recommend were 47% less likely to provide written SCPs to survivors than oncologists who rarely or never experienced this problem (95% CI, 0.33 to 0.84).
Table 2.
Factors Associated With Oncologists Reporting Always/Almost Always Providing Written SCPs to Survivors (n = 108)
| Factor | OR | 95% CI | Wald F | P |
|---|---|---|---|---|
| Race/ethnicity | 8.80 | < .001 | ||
| Non-Hispanic white | Ref | |||
| Asian | 2.75 | 1.64 to 4.60 | < .001 | |
| Other* | 2.69 | 1.35 to 5.35 | .005 | |
| Training regarding late and long-term effects of cancer | 9.90 | .002 | ||
| No or yes, somewhat | Ref | |||
| Yes, in detail | 1.73 | 1.22 to 2.44 | .002 | |
| Patients request more aggressive surveillance | 7.60 | .007 | ||
| Never or rarely | Ref | |||
| Sometimes, often, or always/almost always | 0.53 | 0.33 to 0.84 | .007 |
Abbreviations: OR, odds ratio; SCP, survivorship care plan.
Other includes Hispanic white, non-Hispanic black, and multiple race/ethnicity.
Oncologists who received detailed training about late and long-term effects of cancer were 2× more likely to always/almost always discuss recommendations and provider responsibilities with survivors than oncologists who received some or no training (95% CI, 1.51 to 2.70; Table 3). Oncologists who preferred a shared model of survivorship care (OR, 0.64; 95% CI, 0.41 to 0.98) and those who reported uncertainty about who should provide general preventive care (OR, 0.74; 95% CI, 0.56 to 0.99) were less likely to discuss recommendations and responsibilities for follow-up care with survivors. Asian oncologists were 60% more likely to report always/almost always having these discussions with survivors (95% CI, 1.13 to 2.27).
Table 3.
Factors Associated With Oncologists Reporting Always/Almost Always Discussing Survivorship Care Recommendations and Delineation of Provider Responsibility With Survivors (n = 356)
| Factors | OR | 95% CI | Wald F | P |
|---|---|---|---|---|
| Age | 1.01 | 1.00 to 1.03 | .080 | |
| Race/ethnicity | 3.62 | .030 | ||
| Non-Hispanic white | Ref | |||
| Asian | 1.60 | 1.13 to 2.27 | .008 | |
| Other* | 1.04 | 0.63 to 1.70 | .887 | |
| Sex | 2.86 | .094 | ||
| Male | Ref | |||
| Female | 1.32 | 0.95 to 1.82 | .094 | |
| Training regarding late and long-term effects of cancer | 22.86 | < .001 | ||
| No or yes, somewhat | Ref | |||
| Yes, in detail | 2.02 | 1.51 to 2.70 | < .001 | |
| Preferred model of survivorship care | 2.25 | .110 | ||
| Shared responsibility | 0.64 | 0.41 to 0.98 | .040 | |
| Own responsibility | Ref | |||
| Someone else's responsibility | 0.83 | 0.57 to 1.21 | .322 | |
| Uncertainty about who should provide general preventive care | 4.34 | .040 | ||
| Never or rarely | Ref | |||
| Sometimes, often, or always/almostalways | 0.74 | 0.56 to 0.99 | .040 |
Abbreviation: OR, odds ratio.
Other includes Hispanic white, non-Hispanic black, and multiple race/ethnicity.
Factors Associated With PCPs' Discussion of Recommendations and Provider Responsibilities
PCPs who always/almost always received both a treatment summary and follow-up care plan from survivors' oncologists were more than 9× more likely to have discussions about survivorship care with survivors than those PCPs who did not always receive these documents (95% CI, 5.74 to 14.82; Table 4). PCPs who reported inadequate knowledge or training to manage the problems of survivors were 43% less likely (95% CI, 0.34 to 0.96) to have these discussions with survivors. Female PCPs were twice as likely to have these discussions with survivors than male PCPs (95% CI, 1.26 to 3.27). Older PCPs were more likely to report always/almost always discussing both survivorship care recommendations and responsibilities with survivors (OR, 1.04; 95% CI, 1.01 to 1.06). PCPs who reported a high percentage of time spent in patient care were 42% less likely to have these discussions with survivors compared with those who reported a low percentage of time spent in patient care (95% CI, 0.35 to 0.98). PCPs who saw more than 35 breast or colon cancer survivors per year were 46% less likely to always/almost always have these discussions with survivors than those who saw fewer than 15 survivors per year (95% CI, 0.33 to 0.90).
Table 4.
Factors Associated With PCPs Reporting Always/Almost Always Discussing Recommendations and Delineation of Provider Responsibility With Survivors (n = 122)
| Factor | OR | 95% CI | Wald F | P |
|---|---|---|---|---|
| Age | 1.04 | 1.01 to 1.06 | .006 | |
| Sex | 8.69 | .004 | ||
| Male | Ref | |||
| Female | 2.03 | 1.26 to 3.27 | .004 | |
| Inadequate knowledge or training to manage problems of cancer survivors | 4.57 | .035 | ||
| Never or rarely | Ref | |||
| Sometimes, often, or always/almostalways | 0.57 | 0.34 to 0.96 | .035 | |
| Receive SCP from oncologist | 86.23 | < .001 | ||
| Less than always/almost always | Ref | |||
| Always/almost always | 9.22 | 5.74 to 14.82 | < .001 | |
| No. of patients with breast or colon cancer seen per year | 3.00 | .054 | ||
| 0-14 | Ref | |||
| 15-34 | 0.75 | 0.39 to 1.41 | .363 | |
| ≥ 35 | 0.54 | 0.33 to 0.90 | .017 | |
| Percentage of time spent in patient care* | 4.31 | .040 | ||
| Low | Ref | |||
| High | 0.58 | 0.35 to 0.98 | .040 |
Abbreviations: OR, odds ratio; PCP, primary care physician; SCP, survivorship care plan.
Median split of percentage of time spent on patient care reported by PCPs.
DISCUSSION
To our knowledge, this study represents the first attempt using a nationally representative sample of providers to estimate prevalence and model socioecological predictors of oncologist-reported provision of written SCPs to survivors, as well as oncologist- and PCP-reported discussions with survivors of recommendations and provider responsibilities for survivorship care. Although a majority of oncologists reported always/almost always discussing survivorship care recommendations with survivors, far fewer reported discussing either delineation of provider responsibility for survivorship care or providing written care plans. Moreover, a meager 5% of oncologists reported always/almost always doing all three, despite these activities increasingly becoming the expected standard of care.6 Discussions of survivorship care recommendations and provider responsibility are also not regularly occurring between PCPs and survivors. To achieve patient-centered survivorship care and promote higher-quality care,29 gaps in communicating with and, ideally, engaging survivors in the care planning process must be addressed.
Beyond providing a national benchmark for physicians' communication with survivors about survivorship care, this study suggests factors associated with these behaviors that may serve as targets for intervention. Results across the three models suggest two areas in particular that could increase discussions of survivorship care with survivors: physician training and care coordination. PCPs who reported inadequate knowledge or training to manage survivors' needs and oncologists who lacked detailed training regarding late and long-term effects of cancer were significantly less likely to report discussing survivorship care with survivors. Physicians may benefit from expanded medical education opportunities specifically focused on the needs of cancer survivors or establishment of best practice guidelines to direct care.5,30 If confident in their expertise, physicians may feel more comfortable or motivated to offer a written SCP and discuss survivorship care with survivors.
Regarding care coordination, PCPs who received SCPs from oncologists were more than 9× more likely to report discussions with survivors. This finding is worth emphasis. Prior studies have shown that PCPs often report uncertainty about follow-up care for survivors and rate the transition of care from oncologists as poor.28,31 Unfamiliarity with post-treatment surveillance guidelines may contribute to the lower surveillance rates documented among survivors seen by PCPs relative to oncologists.32–35 However, only 20% of oncologists report consistently providing treatment summaries and follow-up care plans to survivors' PCPs.27 Our study suggests that providing an SCP to the PCP may increase the likelihood of the PCP discussing follow-up care plans with the survivor and could inform the provision of timely and appropriate care. Oncologists' attitudes about models of survivorship care also seemed to be associated with the likelihood of discussing survivorship planning and provision of SCPs. Specifically, those who were uncertain about who should provide general preventative care to survivors and those who preferred nononcologist-led models of survivorship care had less frequent discussions of survivorship care planning with survivors. Models of survivorship care planning that clearly outline the coordination between oncologists and PCPs may also improve communication with survivors.
Demographic and practice characteristics associated with discussing survivorship care with survivors suggest populations in which these interventions may be particularly salient. For example, male PCPs and oncologists were less likely to discuss survivorship care with survivors. This finding is consistent with prior literature showing that female providers typically have longer and more patient-centered communication with patients.36–38 In addition, PCPs who saw a large number of cancer survivors per year and those who spent a larger portion of their time in patient care were less likely to discuss recommendations and responsibilities with survivors. Identifying mechanisms driving this association is a necessary next step toward developing effective interventions for PCPs who see a large number of survivors. Oncologists who reported not providing written SCPs also reported having patients who requested more aggressive follow-up than they would recommend. Future research should investigate if SCPs help survivors understand why specific tests are not necessary and thus have the potential to reduce inappropriate or overuse of these procedures.
Although this study has many strengths, including a nationally representative sample of PCPs and oncologists, there are a number of notable limitations. It is a survey-based self-report of practices concerning breast and colon cancer survivors; however, given the reportedly low percentage of oncologists who reported both providing SCPs and discussing survivorship care, it is unlikely respondents were motivated to provide socially desirable responses. Because of the cross-sectional design, we were unable to differentiate cause and effect of the associations, and the results are mainly limited to hypothesis generation. Furthermore, some significant associations must be interpreted with caution, because they were driven by relatively small groups (eg, only approximately 5% of oncologists reported extensive training in late effects). Our survey included data on training and care coordination; future research should investigate other potential strategies for improving the discussion and provision of survivorship care, such as incorporation of health information technology and coordination among medical teams. It is important for future studies to further elucidate these associations as treatment patterns change.
These data also do not allow us to assess quality, appropriateness, or comprehensibility of the SCPs or discussions, nor can we determine whether conversations were truly patient centered, with shared decision making and addressing of survivor preferences. Care recommendations consistent with patient preferences are associated with better patient engagement in care, adherence to recommendations, and self-management.39,40 An important next step is looking beyond measurement of frequency to assess the quality and content of these documents and discussions and their impact on quality of care, physician behaviors, and survivor health outcomes.
These nationally representative provider-reported data suggest that oncologists rarely reported consistently providing written SCPs to survivors and that oncologists and PCPs often failed to discuss survivorship care recommendations and delineation of provider responsibility for follow-up care with survivors. These data provide a useful benchmark to assess implementation of new mandates affecting the care of cancer survivors. The next step is to develop intervention studies to test the hypothesis that improved care coordination and enhanced physician survivorship training will increase the frequency of survivorship care discussions and downstream consequences, such as survivor adherence to care recommendations, quality of life, and survival.
Glossary Terms
- patient-centered communication (PCC):
communication that helps clinicians provide care according to the patient's values, needs, and preferences and that allows patients to provide input and participate actively in decisions regarding their health and health care. Patient-centered communication has six critical functions: fostering healing relationships, exchanging information, making decisions, responding to emotions, managing uncertainty, and enabling patient self-management.
Footnotes
Listen to the podcast by Dr Cheung at www.jco.org/podcasts
Supported by Contract No. HHSN261200700068C from the National Cancer Institute and by intramural research funds from the American Cancer Society Behavioral Research Center.
The views expressed in this report do not necessarily represent the views of the US Government or the American Cancer Society.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTSOF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Danielle Blanch-Hartigan, Laura P. Forsythe, Catherine M. Alfano, Julia H. Rowland
Financial support: Tenbroeck Smith
Administrative support: Julia H. Rowland
Collection and assembly of data: Tenbroeck Smith, Julia H. Rowland
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103:117–128. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parry C, Kent EE, Mariotto AB, et al. Cancer survivors: A booming population. Cancer Epidemiol Biomarkers Prev. 2011;20:1996–2005. doi: 10.1158/1055-9965.EPI-11-0729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salz T, Oeffinger KC, McCabe MS, et al. Survivorship care plans in research and practice. CA Cancer J Clin. doi: 10.3322/caac.20142. [epub ahead of print on January 12, 2012] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hewitt M, Greenfield S, Stovall E, editors. Washington, DC: National Academies Press; 2006. From Cancer Patient to Cancer Survivor: Lost in Transition. [Google Scholar]
- 5.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Commission on Cancer. Cancer Program Standards 2012: Ensuring Patient-Centered Care (version 1.0) Chicago, IL: American College of Surgeons; 2012. [Google Scholar]
- 7.LIVESTRONG Care Plan. http://www.livestrongcareplan.org/
- 8.National Coalition for Cancer Survivorship: Cancer Survival Toolbox. http://www.canceradvocacy.org/toolbox/
- 9.Greenfield S, Kaplan SH, Ware JE, Jr, et al. Patients' participation in medical care: Effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 10.Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: A STARNet study. Ann Fam Med. 2010;8:410–417. doi: 10.1370/afm.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arora NK. Interacting with cancer patients: The significance of physicians' communication behavior. Soc Sci Med. 2003;57:791–806. doi: 10.1016/s0277-9536(02)00449-5. [DOI] [PubMed] [Google Scholar]
- 12.Pollack LA, Adamache W, Ryerson AB, et al. Care of long-term cancer survivors: Physicians seen by Medicare enrollees surviving longer than 5 years. Cancer. 2009;115:5284–5295. doi: 10.1002/cncr.24624. [DOI] [PubMed] [Google Scholar]
- 13.Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24:5117–5124. doi: 10.1200/JCO.2006.07.0474. [DOI] [PubMed] [Google Scholar]
- 14.Snyder CF, Earle CC, Herbert RJ, et al. Trends in follow-up and preventive care for colorectal cancer survivors. J Gen Intern Med. 2008;23:254–259. doi: 10.1007/s11606-007-0497-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snyder CF, Frick KD, Herbert RJ, et al. Preventive care in prostate cancer patients: Following diagnosis and for five-year survivors. J Cancer Surviv. 2011;5:283–291. doi: 10.1007/s11764-011-0181-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sabatino SA, Thompson TD, Smith JL, et al. Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: Results from a national survey. J Cancer Surviv. 2013;7:32–43. doi: 10.1007/s11764-012-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung WY, Neville BA, Cameron DB, et al. Comparisons of patient and physician expectations for cancer survivorship care. J Clin Oncol. 2009;27:2489–2495. doi: 10.1200/JCO.2008.20.3232. [DOI] [PubMed] [Google Scholar]
- 18.Del Giudice ME, Grunfeld E, Harvey BJ, et al. Primary care physicians' views of routine follow-up care of cancer survivors. J Clin Oncol. 2009;27:3338–3345. doi: 10.1200/JCO.2008.20.4883. [DOI] [PubMed] [Google Scholar]
- 19.Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients' experiences with care for lung cancer and colorectal cancer: Findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28:4154–4161. doi: 10.1200/JCO.2009.27.3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malin JL, Ko C, Ayanian JZ, et al. Understanding cancer patients' experience and outcomes: Development and pilot study of the Cancer Care Outcomes Research and Surveillance patient survey. Support Care Cancer. 2006;14:837–848. doi: 10.1007/s00520-005-0902-8. [DOI] [PubMed] [Google Scholar]
- 21.Potosky AL, Han PK, Rowland J, et al. Differences between primary care physicians' and oncologists' knowledge, attitudes and practices regarding the care of cancer survivors. J Gen Intern Med. 2011;26:1403–1410. doi: 10.1007/s11606-011-1808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganz PA. Survivorship care planning: Implementing the survivorship care plan. In: Hewitt M, Ganz PA, editors. Implementing Cancer Survivorship Care Planning. Washington, DC: National Academies Press; 2007. pp. 5–30. [Google Scholar]
- 23.Taplin S. Understanding and influencing multilevel factors across the cancer continuum. Presented at Multilevel Interventions in Health Care: Building the Foundation for Future Research; March 4-5, 2010; Las Vegas, NV. [Google Scholar]
- 24.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 2008. pp. 465–486. [Google Scholar]
- 25.Glanz K, Rimer BK. Theory at a Glance: A Guide for Health Promotion Practice. Bethesda, MD: National Cancer Institute; 1997. [Google Scholar]
- 26.Forsythe LP, Alfano CM, Leach CR, et al. Who provides psychosocial follow-up care for post-treatment cancer survivors? A survey of medical oncologists and primary care physicians. J Clin Oncol. 2012;30:2897–2905. doi: 10.1200/JCO.2011.39.9832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forsythe LP, Parry C, Alfano CM, et al. Use of survivorship care plans in the United States: Associations with survivorship care. J Natl Cancer Inst. 2013;105:1579–1587. doi: 10.1093/jnci/djt258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nissen MJ, Beran MS, Lee MW, et al. Views of primary care providers on follow-up care of cancer patients. Fam Med. 2007;39:477–482. [PubMed] [Google Scholar]
- 29.Institute of Medicine. Washington DC: National Academies Press; 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. [PubMed] [Google Scholar]
- 30.Birken SA, Mayer DK, Weiner BJ. Survivorship care plans: Prevalence and barriers to use. J Cancer Educ. 2013;28:290–296. doi: 10.1007/s13187-013-0469-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grunfeld E, Mant D, Vessey MP, et al. Specialist and general practice views on routine follow-up of breast cancer patients in general practice. Fam Pract. 1995;12:60–65. doi: 10.1093/fampra/12.1.60. [DOI] [PubMed] [Google Scholar]
- 32.McBean AM, Yu X, Virnig BA. The use of preventive health services among elderly uterine cancer survivors. Am J Obstet Gynecol. 2008;198:86.e81–86.e88. doi: 10.1016/j.ajog.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 33.Earle CC, Burstein HJ, Winer EP, et al. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21:1447–1451. doi: 10.1200/JCO.2003.03.060. [DOI] [PubMed] [Google Scholar]
- 34.Keating NL, Landrum MB, Guadagnoli E, et al. Factors related to underuse of surveillance mammography among breast cancer survivors. J Clin Oncol. 2006;24:85–94. doi: 10.1200/JCO.2005.02.4174. [DOI] [PubMed] [Google Scholar]
- 35.Field TS, Doubeni C, Fox MP, et al. Under utilization of surveillance mammography among older breast cancer survivors. J Gen Intern Med. 2008;23:158–163. doi: 10.1007/s11606-007-0471-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: A meta-analytic review. JAMA. 2002;288:756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 37.Hall JA, Irish JT, Roter DL, et al. Gender in medical encounters: An analysis of physician and patient communication in a primary care setting. Health Psychol. 1994;13:384–392. doi: 10.1037//0278-6133.13.5.384. [DOI] [PubMed] [Google Scholar]
- 38.Hall JA, Roter DL. Medical communication and gender: A summary of research. J Gend Specif Med. 1998;1:39–42. [PubMed] [Google Scholar]
- 39.Dentzer S. Rx for the ‘blockbuster drug’ of patient engagement. Health Aff (Millwood) 2013;32:202. doi: 10.1377/hlthaff.2013.0037. [DOI] [PubMed] [Google Scholar]
- 40.Epstein RM, Street RL. Patient communication in cancer care: Promoting healing and reducing suffering. Bethesda MD: National Cancer Institute; 2007. NIH publication 07-6225. [Google Scholar]


