Abstract
Central hyperthermia is a very rare disease; however, once it happens, it is associated with a poor prognosis and high mortality for patients with severe brainstem strokes. Following a pontine hemorrhage, a 46-years-old female developed prolonged hyperthermia. Work-ups to the fever gave no significant clues for the origin of fever, and hyperthermia did not respond to any empirical antibiotics or antipyretic agents. The patient's body temperature still fluctuated in a range of 37.5℃ to 39.2℃. Considering the lesion of hemorrhage, we suspected central hyperthermia rather than infectious diseases. We started with baclofen administration at a dose of 30 mg/day. The body temperature changed to a range of 36.6℃ to 38.2℃. We raised the dose of baclofen to 60 mg/day. The patient's body temperature finally dropped to a normal range. Central hyperthermia, caused by failures of thermoregulatory pathways in brainstem, following the pontine hemorrhage rarely occurs. Baclofen can be used to treat suspected central hyperthermia in a patient with pontine hemorrhage.
Keywords: Fever, Pons, Hemorrhage, Baclofen
INTRODUCTION
Prolonged central hyperthermia following pontine hemorrhage is a very rare disease, caused by failures of thermoregulatory pathways at the brainstem. Although central hyperthermia has been known for a long time, our knowledge remains limited.
Central hyperthermia is usually associated with a high body temperature that does not respond to common antipyretic treatments [1]. According to some literature, high fever (>39℃) with tachycardia (>110 beat/min) developed within 24 hours from the onset of stroke is correlated with high risks of death [2,3]. Furthermore, if patients survived from the above situation, most survivors remained in a severely disabled state.
In this respect, early diagnosis and treatment of central hyperthermia is critical. However, in most cases, it is difficult to diagnose early because of high mortality rates due to complications, such as sudden cardiac deaths, acute renal failures, rhabdomyolysis, etc., induced by high fevers and the time duration required to perform numerous tests for exclusion of infected sources.
A patient who had hyperthermia for more than a month without specific fever focus was being transferred to our department. We diagnosed her with prolonged central hyperthermia considering injured lesion. She was treated with baclofen and thus, we reported the case and provided relative literature reviews.
CASE REPORT
Following pontine hemorrhage, a 46-years-old female developed prolonged hyperthermia. At the day of admission, she visited our emergency department with symptoms of a sudden headache, weakness on both upper extremities, and mental changes. She did not have specific past histories, such as diabetic mellitus, hypertension, pulmonary tuberculosis, hepatitis B, and so on. There were no preceding infections or fevers at least 1 week prior to the onset of pontine hemorrhage.
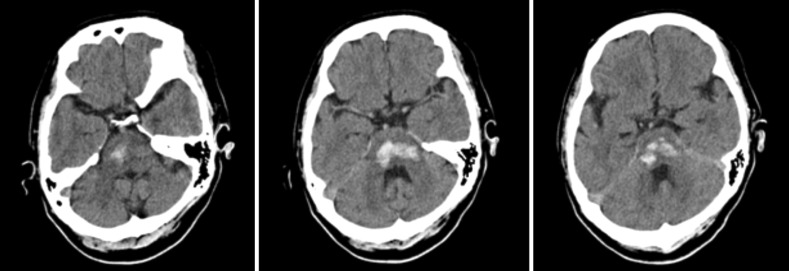
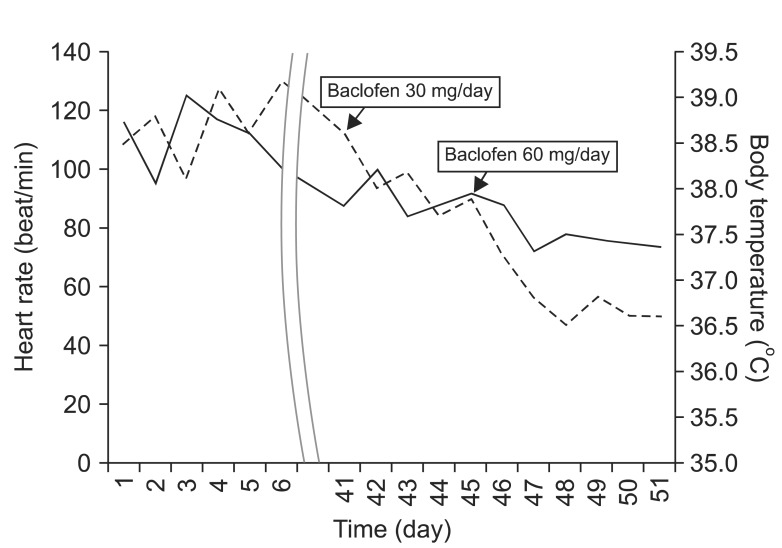
Brain computed tomography (CT) was conducted and hemorrhage was observed throughout lower midbrain to pons (Fig. 1). She took the non-surgical treatment at neurosurgeon department. One day after the admission, fever above 38℃ and intermittent tachycardia (>110 beat/min) developed approximately 1-2 times a day. Whole work-ups to the fever, including laboratory tests (complete blood count, white blood cell differ-count, C-reactive protein, erythrocyte sedimentation rate, electrolyte, urinalysis, urine microscopy, aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transpeptidase, total bilirubin, blood urea nitrogen/creatinine, microbial culture on blood, sputum, urine and cerebrospinal fluid analysis, etc.) and radiologic study (chest X-ray and chest CT to rule out pneumonia, paranasal sinus water's view to rule out sinusitis), showed no significant clues for the origin of fever. Despite the consultation to department of infectious diseases, the origin of fever was still ambiguous and empirical antibiotic treatments were performed, but the fever did not respond to any antibiotics (cefbuperazone+clindamycin, amoxicillin+clavulanate, ceftazidime, meropenem) or antipyretics (acetaminophen, non-steroidal anti inflammatory drugs, aspirin lysinate, etc.). Suspicions of drug fevers, antiepileptic agents (valproic acids) and any non-essential drugs (neurostimulators, such as phenytoin, donepezil, acetyl-L-carnitine, antipyretics, etc.) were then discontinued. But, the body temperature was still fluctuating in a range of 37.5℃ to 39.2℃ and tepid massage was the only way to control the fever. After 40 days from admission, she was transferred to the department of rehabilitation medicine. Intermittent fever over 38℃ and tachycardia (>110 beat/min) was still ongoing. Whole work-up of fever was tested again, and still the results indicated no clues for the origin of fever. Since then, we suspected the possibility of non-infectious diseases so we searched literatures related to fevers of unknown origin in patients diagnosed with intracranial hemorrhages. Assuming the lesion of hemorrhage, central hyperthermia was strongly suspected and there was a case report of central hyperthermia treated by baclofen [4], thus, we started baclofen oral administration at a dose of 30 mg/day after 44 days from admission. Then, the body temperatures tended to subside, however, intermittent fever sustained at a range of 36.6℃ to 38.2℃. To further drop the body temperature, we raised the dose of baclofen to 60 mg/day. Finally, after 47 days from admission, the body temperature dropped to a normal range and was maintained stably (Fig. 2). Until now, she is being administered 60 mg/day of baclofen and her basal body temperature is being maintained within normal limits. She is undergoing comprehensive rehabilitation for the sequelae of pontine hemorrhages without any specific side effects of baclofen.
Fig. 1.
Computed tomography demonstrated hemorrhage in brainstem and middle cerebellar peduncle which are mainly posterior pons and the largest diameter is 29 mm.
Fig. 2.
Fever patterns of prolonged central hyperthermia in a pontine hemorrhage.
DISCUSSION
Central hyperthermia is likely a result of direct pontine destruction or indirect compression. Central hyperthermia is characterized by an unchanged setting of the thermoregulatory center so antipyretics have no effects on central hyperthermia.
Diagnosis of central hyperthermia must meet the following criteria: 1) no preceding infections or fevers at least 1 week prior to stroke onset, 2) high fever (>39℃) developing within 24 hours after onset of stroke, and 3) negative work-ups for fever of infectious origin [2]. But the underlying pathophysiology of this condition is unknown.
Body temperature is strictly controlled in humans at approximately 37℃. Several physiologic mechanisms are involved in temperature homeostasis, all of which are coordinated through the hypothalamus [4]. The central pathway for control of thermoregulatory thermogenesis and innervations of brown adipose tissue (BAT) is complex [5]. BAT is an important effector organ for non-shivering thermogenesis in the defense against cold [4]. Preoptic chiasma/anterior hypothalamic nuclei are accepted as the center for body temperature control. Cooling of this area activates BAT [6], whereas warming suppresses activation of BAT and non-shivering thermogenesis [7]. The efferent signals from the preoptic chiasma/anterior hypothalamic nuclei are the inhibitor of gamma-aminobutyric acids (GABA) to reach ventromedial hypothalamic nucleus [8]. The signal from the ventromedial hypothalamic nucleus reached the raphe nuclei through the lower midbrain and release GABA in this area [9,10]. The thermoregulatory signal is connected to the sympathetic chain. The sympathetic chain controls the BATs for non-shivering thermogenesis.
We hypothesized that baclofen had an effect on central hyperthermia for patients with pontine hemorrhages. Baclofen, a GABA agonist, functioned as inhibitory signals directly acting on the raphe nuclei to suppress BAT activation, which in turn suppresses the body temperatures [4]. Thus, baclofen may control central hyperthermia by replacing neurotransmitters (GABA, glutamate) which were blocked due to the location of hemorrhage.
The present case provided us guidance for understanding thermoregulatory dysfunction in patients with brainstem hemorrhage. In the case of pontine strokes, we should include prolonged central hyperthermia as possible causes of fever and consider the administration of baclofen.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Morales-Ortiz A, Jimenez-Pascual M, Perez-Vicente JA, Monge-Arguiles A, Bautista-Prados J. Fever of central origin during stroke. Rev Neurol. 2001;32:1111–1114. [PubMed] [Google Scholar]
- 2.Sung CY, Lee TH, Chu NS. Central hyperthermia in acute stroke. Eur Neurol. 2009;62:86–92. doi: 10.1159/000222778. [DOI] [PubMed] [Google Scholar]
- 3.Wijdicks EF, St Louis E. Clinical profiles predictive of outcome in pontine hemorrhage. Neurology. 1997;49:1342–1346. doi: 10.1212/wnl.49.5.1342. [DOI] [PubMed] [Google Scholar]
- 4.Huang YS, Hsiao MC, Lee M, Huang YC, Lee JD. Baclofen successfully abolished prolonged central hyperthermia in a patient with basilar artery occlusion. Acta Neurol Taiwan. 2009;18:118–122. [PubMed] [Google Scholar]
- 5.Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev. 2004;84:277–359. doi: 10.1152/physrev.00015.2003. [DOI] [PubMed] [Google Scholar]
- 6.Imai-Matsumura K, Nakayama T. The central efferent mechanism of brown adipose tissue thermogenesis induced by preoptic cooling. Can J Physiol Pharmacol. 1987;65:1299–1303. doi: 10.1139/y87-206. [DOI] [PubMed] [Google Scholar]
- 7.Boulant JA. Role of the preoptic-anterior hypothalamus in thermoregulation and fever. Clin Infect Dis. 2000;31(Suppl 5):S157–S161. doi: 10.1086/317521. [DOI] [PubMed] [Google Scholar]
- 8.Amir S, Schiavetto A. Injection of prostaglandin E2 into the anterior hypothalamic preoptic area activates brown adipose tissue thermogenesis in the rat. Brain Res. 1990;528:138–142. doi: 10.1016/0006-8993(90)90206-q. [DOI] [PubMed] [Google Scholar]
- 9.Shibata M, Iriki M, Arita J, Kiyohara T, Nakashima T, Miyata S, et al. Procaine microinjection into the lower midbrain increases brown fat and body temperatures in anesthetized rats. Brain Res. 1996;716:171–179. doi: 10.1016/0006-8993(96)00040-6. [DOI] [PubMed] [Google Scholar]
- 10.Morrison SF, Sved AF, Passerin AM. GABA-mediated inhibition of raphe pallidus neurons regulates sympathetic outflow to brown adipose tissue. Am J Physiol. 1999;276(2 Pt 2):R290–R297. doi: 10.1152/ajpregu.1999.276.2.R290. [DOI] [PubMed] [Google Scholar]