Abstract
Background/Aims
There is an increased risk for inflammatory bowel disease (IBD) patients to develop infections due to the use of immunomodulators and biologics. Several infections are preventable by immunizations. This study investigated the knowledge and awareness of Korean gastroenterologists regarding the vaccination of patients with IBD.
Methods
A self-reported questionnaire was sent by e-mail to the faculty members of tertiary hospitals. Gastroenterologists were asked ten questions regarding the immunization of patients with IBD. A total of 56 gastroenterologists completed the questionnaire.
Results
A majority of gastroenterologists (>60%) had rarely or never recorded an immunization history from their patients with IBD. Moreover, 50% to 70% of the gastroenterologists did not know that live vaccines should be avoided in immunosuppressed patients. The most commonly mentioned resistance to vaccinations was "the lack of concern and knowledge regarding vaccination." Gastroenterologists more frequently asked about the immunization history of influenza, pneumococcal, hepatitis A, and hepatitis B vaccines and recommended these vaccines more often than others.
Conclusions
Korean gastroenterologists' awareness and knowledge regarding the vaccination of patients with IBD were very poor. Intensive educational programs on immunization guidelines directed toward gastroenterologists who care for patients with IBD are required to ensure that these patients receive the necessary vaccinations.
Keywords: Immunization, Inflammatory bowel disease, Vaccine, Immunosuppression
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic intestinal inflammatory condition with unidentified causes. Although the precise pathogenesis is still unknown, IBD is believed to result from complex interactions between genetic, environmental, bacterial, and immunological factors that induce intestinal inflammation.1 Over the last decade, treatment modalities for patients with IBD have improved dramatically. The increasing use of immune modulators (such as azathioprine and 6-mercaptopurine) and biologics (such as infliximab and adalimumab) has reportedly improved the prognosis of IBD.2,3 However, these medications along with corticosteroids place patients at increased risk of infectious complications, several of which are potentially preventable through vaccination.4 Many case reports of fatal varicella infection,5,6,7,8,9 fulminant hepatitis,10 and pneumococcal infection11,12 in immunosuppressed IBD patients have been reported in the literature. Despite the increased risk of infections, several studies have showed that many patients with IBD are not vaccinated appropriately. For instance, Melmed et al.13 revealed that out of 146 patients who reported current or prior use of immunosuppressive medications, 28% recalled yearly influenza vaccinations and only 9% reported receiving a pneumococcal vaccine. In another study of 2,076 IBD cases, effective vaccination against hepatitis B was demonstrated in only 12% of patients.14 These patients stated that the most common reasons for nonimmunization were a lack of awareness and concern for side effects.13 This suggests that physicians are not adequately educating and recommending vaccinations to their patients. Two recent studies in Western countries demonstrated that a substantial proportion of gastroenterologists lack knowledge of the appropriate immunizations to recommend to the patients with IBD.15,16 Moreover, Korean gastroenterologists are expected to have more indifference and less knowledge regarding vaccinating these patients compared to Western gastroenterologists because IBD in Korea is rarer than in Western countries. However, the incidence and prevalence of Korean IBD are increasing rapidly17 and vaccination of these patients requires greater attention. In this study, we investigated Korean gastroenterologists' knowledge regarding vaccinating patients with IBD and defined the gastroenterologist's role in vaccinations.
MATERIALS AND METHODS
1. Study participants
We sent an electronic questionnaire between January and February 2013 to gastroenterologists who were members of the Korean Association for the Study of Intestinal Diseases. We only included faculty members of tertiary hospitals and adult gastroenterologists. If the electronic questionnaire was not completed within 10 days, a second e-mail reminder was sent followed by a third one 10 days later if still not completed. If there were any unanswered questions, we sent another e-mail asking to complete the questionnaire.
2. Study questionnaire
Physicians were asked ten questions regarding demographic information, current vaccination practices for patients with IBD, and knowledge regarding the appropriate vaccines to administer. Demographic data included sex, years in practice, the dominant type of clinical practice, and the number of IBD cases in their practice (past and present).
Physicians were questioned as to how frequently they asked their patients regarding their immunization history. They were also asked a series of knowledge-based questions regarding the suitable inactivated and live attenuated vaccinations for immunocompetent or immunosuppressed IBD cases. Physicians were then asked whether they actually recommended each vaccine to these patients. For the respondents who thought the vaccine is necessary for patients with IBD, but did not actually vaccinate the patients, the reasons for discrepancy between their thoughts and practice were investigated (Supplementary Table 1). This study was approved by the Institutional Review Board of Kangbuk Samsung Hospital, Seoul, Korea.
3. Statistical analysis
Categorical and ordinal variables were summarized using counts and percentages. The chi-square or Fisher exact test was used to compare characteristics of the responding gastroenterologists. p-values <0.05 were considered statistically significant. The SPSS version 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses.
RESULTS
1. Demographics of the responding gastroenterologists
Questionnaires were mailed to 64 gastroenterologists and 56 (87.5%) returned a completed questionnaire. Table 1 shows the physicians' characteristics. The majority of gastroenterologists were male (75.0%) and 66.1% (37 of 56) of respondents have been in practice for over 5 years. Approximately one-fifth (21.4%) of the 56 gastroenterologists were exclusively lower gastrointestinal (GI) specialists and the others were nonexclusive lower GI specialists. Out of the 56 respondents, 23 (41.1%) cared for more than 200 IBD cases to date and 30 (53/6%) cared for more than 60 follow-up IBD cases each year.
Table 1.
Characteristics of the Responding Gastroenterologists (n=56)
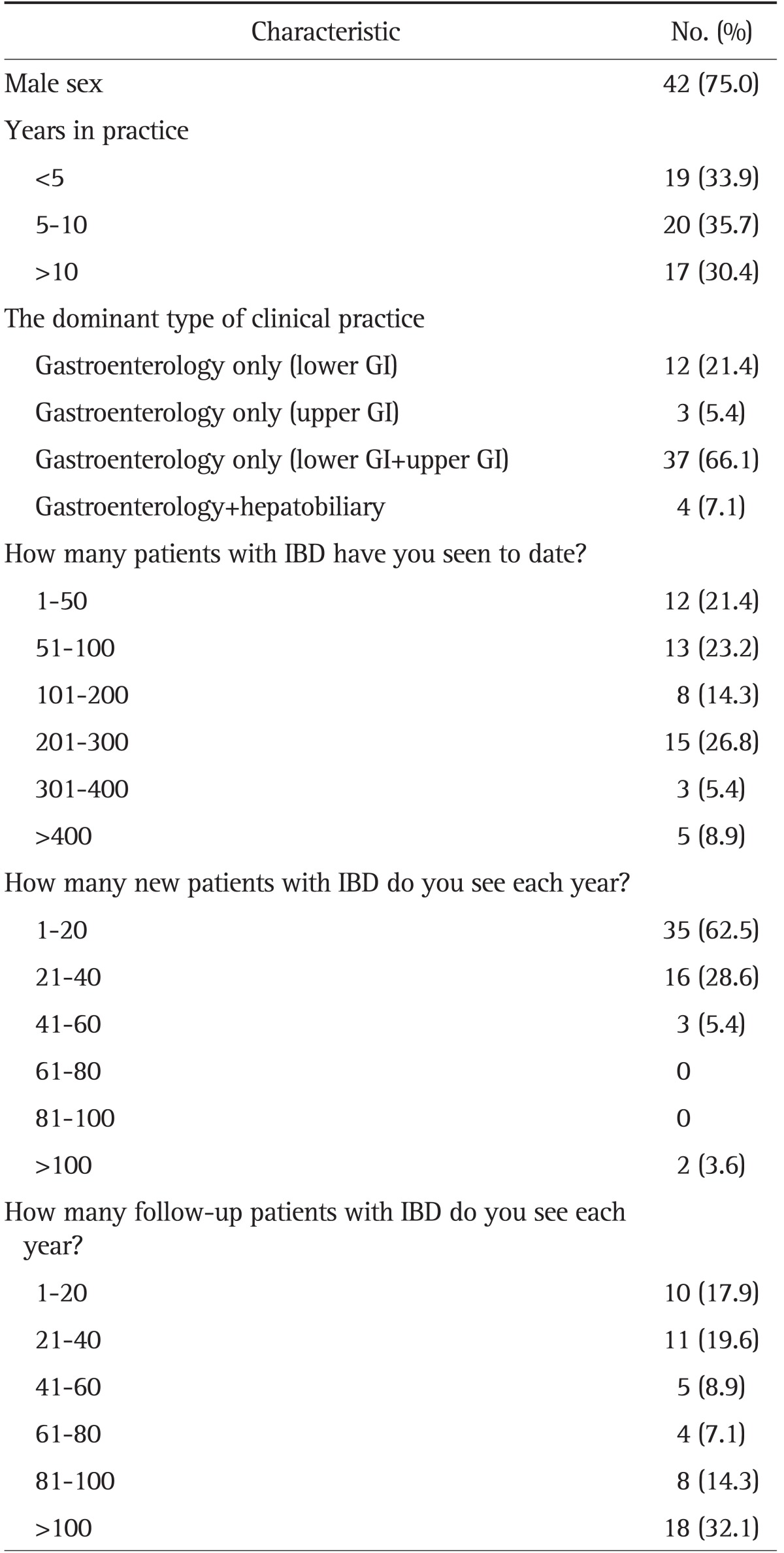
GI, gastrointestinal; IBD, inflammatory bowel disease.
2. Immunization histories and administration of vaccines
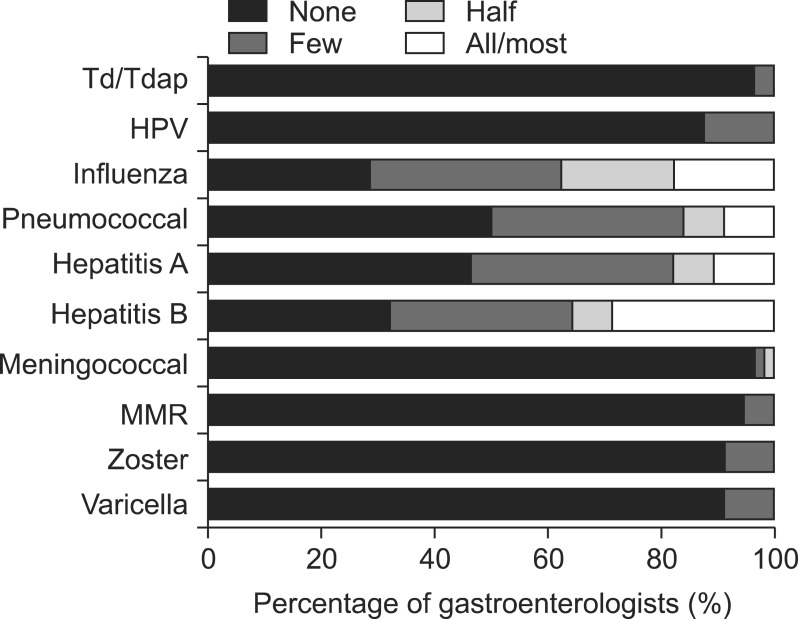
A majority of gastroenterologists have rarely or never taken an immunization history from their patients with IBD. Most physicians (>80%) did not inquire regarding individual immunizations for tetanus, diphteria, pertussis (Td/Tdap), human papillomavirus (HPV), meningococcal, measles, mumps, rubella (MMR), zoster, and varicella. Moreover, only 37.5%, 16.1%, 17.9%, and 35.7% of physicians asked at least half of their patients with IBD whether they had received the influenza, pneumococcal, hepatitis A, and hepatitis B vaccine, respectively (Fig. 1). There were no significant differences in how often they asked their patients regarding immunization histories (all individual immunizations including influenza and pneumococcal vaccines) according to years in practice, dominant type of clinical practice, and number of IBD cases (Table 2).
Fig. 1.
The percentage of gastroenterologists who collect specific immunization histories from their patients with inflammatory bowel disease.
Td/Tdap, tetanus, diphtheria, pertussis; HPV, human papillomavirus; MMR, measles, mumps, rubella.
Table 2.
Frequency of Obtaining Immunization Histories from at Least Half of Their Inflammatory Bowel Disease Patients according to Gastroenterologists' Characteristics
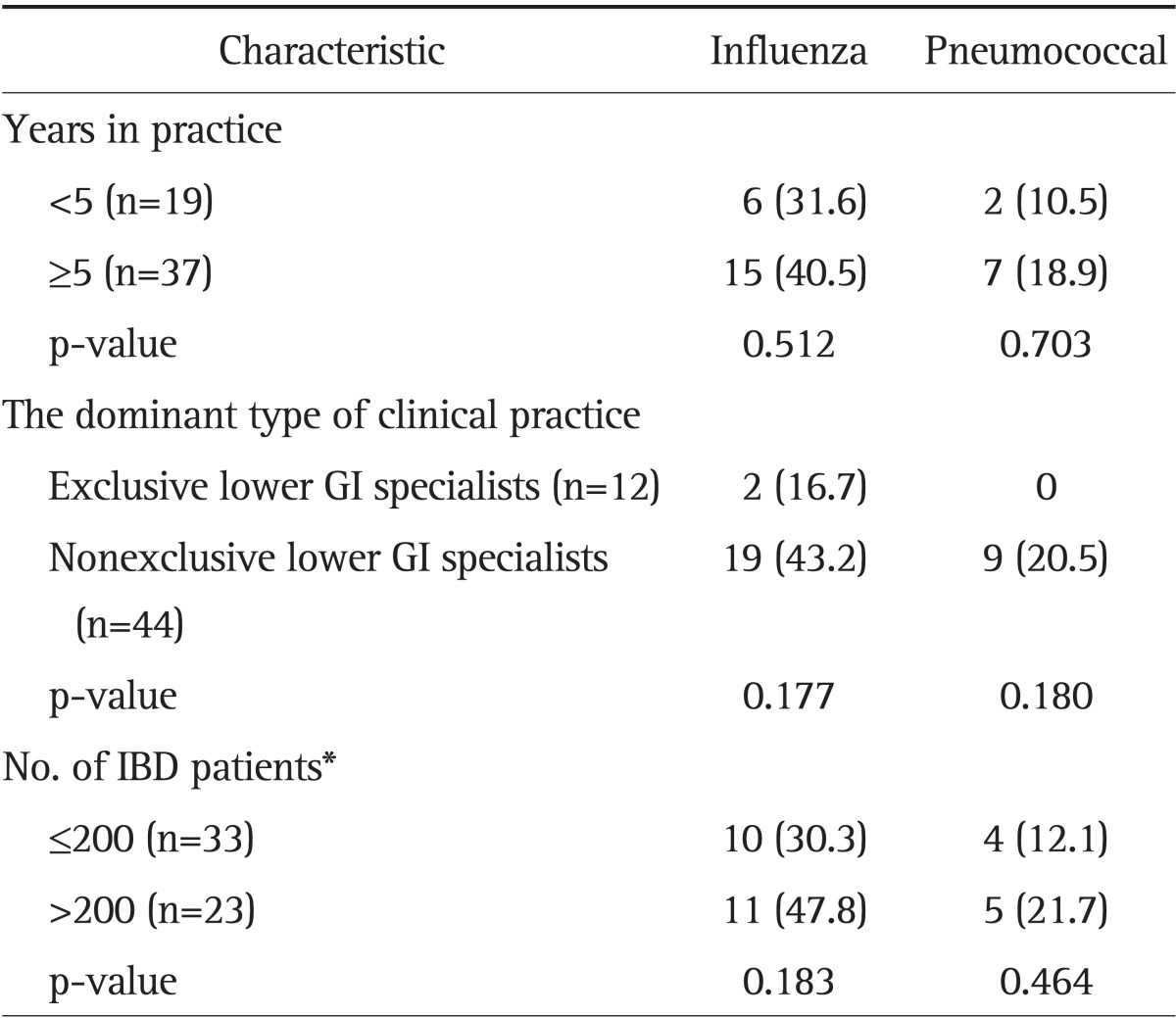
Data are presented as number (%).
GI, gastrointestinal; IBD, inflammatory bowel disease.
*How many patients with IBD have you seen to date?
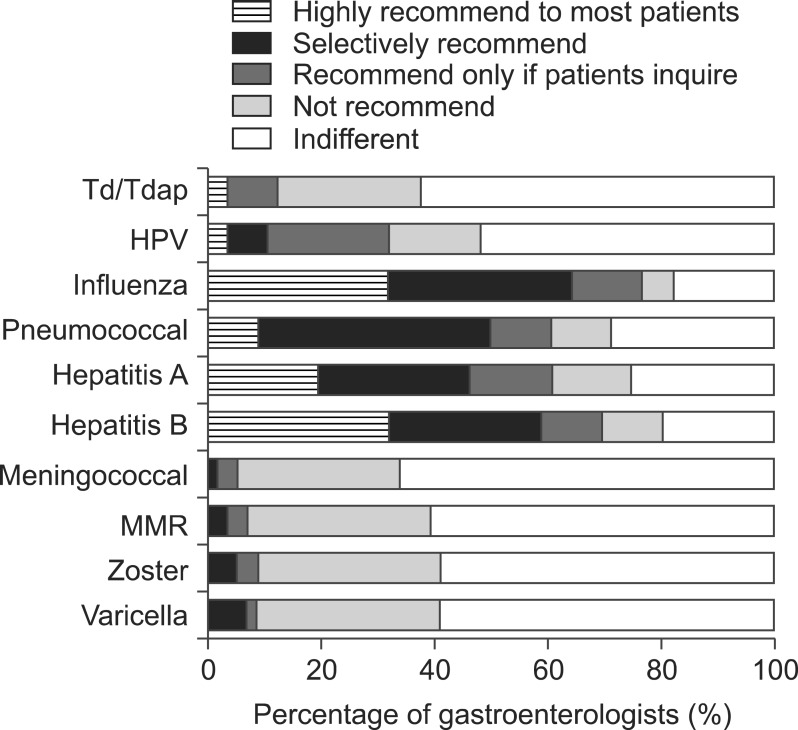
More than half of gastroenterologists were indifferent regarding the vaccine recommendation for Td/Tdap, HPV, meningococcal, MMR, zoster, and varicella. Conversely, 64.3%, 50.0%, 46.4%, and 58.9% of physicians highly or selectively recommended influenza, pneumococcal, hepatitis A, and hepatitis B vaccines, respectively, to their patients with IBD (Fig. 2).
Fig. 2.
The percentage of gastroenterologists who recommend specific immunizations to their patients with inflammatory bowel disease.
Td/Tdap, tetanus, diphtheria, pertussis; HPV, human papillomavirus; MMR, measles, mumps, rubella.
3. Immunizations in immunocompetent and immunosuppressed IBD cases
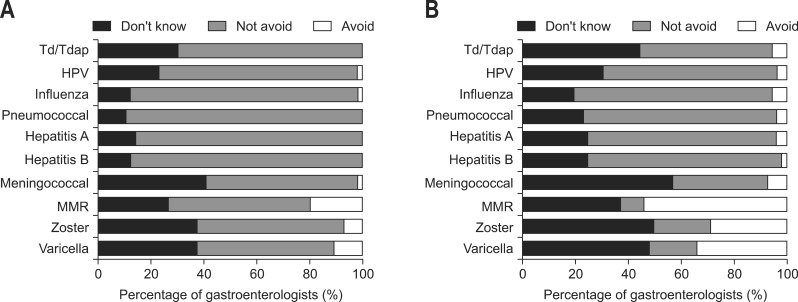
Ten percent to 40% of gastroenterologists did not know which vaccinations should be given to immunocompetent patients with IBD (Fig. 3A). More than half of gastroenterologists responded that they do not know whether or not the three live vaccines (MMR, zoster, and varicella) should be avoided in immunosuppressed IBD or they do not avoid administering the three live vaccines to their immunosuppressed IBD. Only 30% to 50% of gastroenterologists thought that MMR (53.6%), zoster (28.6%), and varicella (33.9%) should be avoided in immunosuppressed IBD (Fig. 3B). There were no significant differences in knowledge regarding the three live vaccines in immunosuppressed IBD according to gastroenterologists' characteristics (Table 3).
Fig. 3.
The percentage of gastroenterologists who would avoid specific immunizations in immunocompetent inflammatory bowel disease (IBD) (A) and immunosuppressed IBD (B) patients.
Td/Tdap, tetanus, diphtheria, pertussis; HPV, human papillomavirus; MMR, measles, mumps, rubella.
Table 3.
Knowledge Regarding the Live Vaccines in Immunosuppressed Patients according to Gastroenterologists' Characteristics
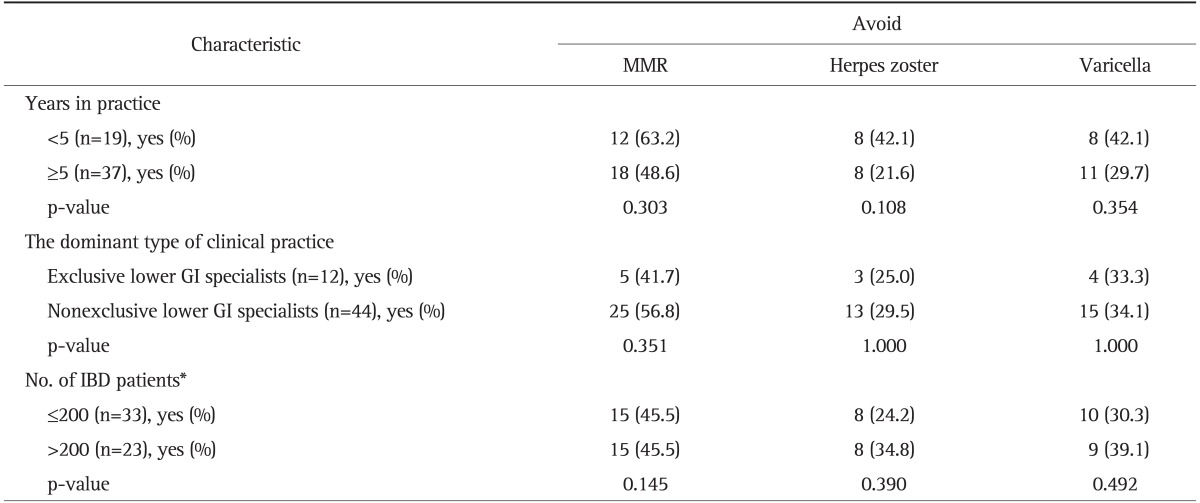
MMR, measles, mumps, rubella; GI, gastrointestinal; IBD, inflammatory bowel disease.
*How many patients with IBD have you seen to date?
Eighty percent (45 of 56) of gastroenterologists thought the vaccines are necessary for IBD, but did not vaccinate their patients. Of these 45 gastroenterologists, 39 specified the reasons for the discrepancy between their thoughts and practice. The most common reasons were as follows: the lack of concern for vaccinations (n=20), insufficient patient exam time in the office (n=9), and the lack of information or knowledge regarding vaccinations (n=7).
DISCUSSION
A recent guideline has indicated that inactivated vaccines are well tolerated in patients with IBD, regardless of their status of immunosuppression.18 These vaccines include the Tdap, HPV, influenza, pneumococcal, hepatitis A and B, and meningococcal vaccines. Conversely, live vaccines such as MMR, zoster, and varicella should be avoided in immunocompromised IBD cases. Specifically, live vaccination is contraindicated if planning to start immunosuppressive or biologic therapy within 4 to 12 weeks or if already on immunosuppressive or biologic therapy.18 We summarized the current guideline about the vaccination in patients with IBD in the Supplementary Table 2 on the basis of the Western guideline.18
As expected, a large portion of Korean gastroenterologists who care for patients with IBD have rarely or never taken an immunization history and were indifferent regarding the recommendation of vaccines. Moreover, more than half of gastroenterologists did not know that live vaccines should be avoided in immunosuppressed IBD. Gastroenterologists may not have known which vaccines are live vaccines, and thus knowledge regarding the live vaccines in immunocompromised patients might have been poor. The lack of knowledge for live vaccines represents insufficient information regarding vaccination. Because gastroenterologists' vaccine awareness and knowledge is poor, patients with IBD are not being appropriately immunized. According to two Western studies, the proportions of patients with IBD who properly received influenza, pneumococcal, and hepatitis B vaccinations were only 28%, 9%, and 12%, respectively.13,14 Similarly, vaccination rates of Koreans with IBD are expected to be very low. Further studies need to investigate the actual vaccination status of Koreans with IBD. Prior studies have emphasized the importance of physician recommendations in patients' decisions to receive vaccines.15,16,19 Therefore, if physicians are unsure of adequate vaccinations to recommend, patients may not receive the necessary vaccinations.
Fortunately, Korean gastroenterologists were more concerned regarding influenza, pneumococcal, hepatitis A, and hepatitis B vaccines compared with the other vaccines. In other words, Korean gastroenterologists asked more frequently regarding immunization history of these four vaccines and they recommended the vaccines more often in IBD cases compared to the other vaccines. We speculate that the gastroenterologists often recommended pneumococcal and influenza vaccination because these two vaccines need to be administered periodically during adulthood. In addition, the hepatitis vaccinations were more frequently recommended compared with other vaccine types possibly because Korea is a hepatitis B endemic area. With regard to other vaccine types, the gastroenterologists may have thought that most patients have received vaccinations as part of the recommended childhood immunizations.
The most commonly mentioned resistances to vaccinations were "the lack of concern and knowledge regarding vaccinations" and "the insufficient patient exam time in the office." Our study clearly demonstrated that educating gastroenterologists is necessary to increase awareness of the importance of vaccinating patients with IBD. Additionally, a practical guide should be provided to clinicians regarding appropriate vaccinations to administer. Because there is no current guideline for Korean patients with IBD, the Western guideline should be followed. However, the suitability of the Western guideline should be verified for Korean patients and an adequate vaccination guideline should be reestablished. In addition, quality indicators for IBD management should include vaccinations. Furthermore, because gastroenterologists felt they had insufficient time to thoroughly exam their patients, systems such as the use of electronic medical record prompts may be effective in increasing vaccination rates.
A few gastroenterologists were concerned that the clinical IBD activity may be affected by vaccination or that patients may not be able to mount an immune response to vaccines. Although there are case reports of ulcerative colitis relapsed by influenza vaccination,20,21 the general expert consensus is that vaccinations in patients with IBD are not associated with a flare in disease activity.18,22,23 Recent studies regarding the immune response to vaccines in IBD showed that although immunomodulators and biological agents may cause slightly diminished immune responses, the majority of immunized patients develop protective antibodies.24,25,26,27 Given that immunosuppressive therapy may lead to an impaired immune response to a vaccine and may place these patients at increased risk for a variety of infections which are preventable by vaccination, newly diagnosed patients with IBD should be thoroughly vaccinated before the initiation of immunosuppressive therapy.
A previous study demonstrated that the knowledge and attitudes of patients as well as provider recommendations may enhance vaccination rates.19 Considering the importance of patient demand for vaccines, the widespread use of direct reminders to patients by means of e-mails, telephone calls or letters may be helpful in improving vaccination rates.
Our study has several limitations. First of all, primary care physicians' knowledge regarding vaccinating patients with IBD was not investigated. However, IBD is a rare disease in Korea compared to Western countries. In Korea, IBD is generally managed by gastroenterologists. And primary care physicians who care for patients with IBD are very scarce. Secondly, pediatric gastroenterologists were not surveyed. The pediatric gastroenterologists are expected to have a higher awareness of the adequate immunizations to administer given the importance of vaccination emphasized during their pediatric training. If we included pediatric gastroenterologists, the results regarding gastroenterologists' knowledge of vaccinations might have improved. Thirdly, there is the limitation caused by questionnaire study, that is, the answers would be exaggerated because of the goal of keeping the questionnaires brief and simple. Gastroenterologists may have felt specific questions did not offer appropriately nuanced choices. For instance, gastroenterologists may have thought that the answers to some questions depended on the various patients' statuses such as patient characteristics, economic capacities, and ongoing treatment plans. This may be one cause of "don't know" answers. Fourth, we did not evaluate the validity and reliability of the questionnaires for vaccination knowledge. Finally, we did not investigate knowledge and awareness regarding immunization among patients with IBD. Opinions toward immunizations in these patients may provide information that contributes to the improvement of vaccination rates.
In conclusion, Korean gastroenterologists show indifference to vaccinations in IBD cases and lack adequate knowledge of established immunization guidelines. Considering that patients with IBD have an increased risk of becoming immunocompromised due to their treatment, gastroenterologists need to realize the importance of immunizations and acquire greater knowledge regarding vaccination recommendations.
Footnotes
No potential conflict of interest relevant to this article was reported.
Supplementary Material
The Content of the Questionnaire Regarding Vaccination Information
Vaccination Recommendations in IBD Patients
References
- 1.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 2.Moum B. Medical treatment: does it influence the natural course of inflammatory bowel disease? Eur J Intern Med. 2000;11:197–203. doi: 10.1016/s0953-6205(00)00091-1. [DOI] [PubMed] [Google Scholar]
- 3.Ramadas AV, Gunesh S, Thomas GA, Williams GT, Hawthorne AB. Natural history of Crohn's disease in a population-based cohort from Cardiff (1986-2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–1206. doi: 10.1136/gut.2009.202101. [DOI] [PubMed] [Google Scholar]
- 4.Domm S, Cinatl J, Mrowietz U. The impact of treatment with tumour necrosis factor-alpha antagonists on the course of chronic viral infections: a review of the literature. Br J Dermatol. 2008;159:1217–1228. doi: 10.1111/j.1365-2133.2008.08851.x. [DOI] [PubMed] [Google Scholar]
- 5.Keene JK, Lowe DK, Grosfeld JL, Fitzgerald JF, Gonzales-Crussi F. Disseminated varicella complicating ulcerative colitis. JAMA. 1978;239:45–46. [PubMed] [Google Scholar]
- 6.Deutsch DE, Olson AD, Kraker S, Dickinson CJ. Overwhelming varicella pneumonia in a patient with Crohn's disease treated with 6-mercaptopurine. J Pediatr Gastroenterol Nutr. 1995;20:351–353. doi: 10.1097/00005176-199504000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Lemyze M, Tavernier JY, Chevalon B, Lamblin C. Severe varicella zoster pneumonia during the course of treatment with azathioprine for Crohn's disease. Rev Mal Respir. 2003;20(5 Pt 1):773–776. [PubMed] [Google Scholar]
- 8.Leung VS, Nguyen MT, Bush TM. Disseminated primary varicella after initiation of infliximab for Crohn's disease. Am J Gastroenterol. 2004;99:2503–2504. doi: 10.1111/j.1572-0241.2004.41389_7.x. [DOI] [PubMed] [Google Scholar]
- 9.Vergara M, Brullet E, Campo R, Calvet X, Blanch L. Fulminant infection caused by varicella herpes zoster in patient with Crohn disease undergoing treatment with azathioprine. Gastroenterol Hepatol. 2001;24:47. doi: 10.1016/s0210-5705(01)70132-x. [DOI] [PubMed] [Google Scholar]
- 10.Esteve M, Saro C, González-Huix F, Suarez F, Forné M, Viver JM. Chronic hepatitis B reactivation following infliximab therapy in Crohn's disease patients: need for primary prophylaxis. Gut. 2004;53:1363–1365. doi: 10.1136/gut.2004.040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ritz MA, Jost R. Severe pneumococcal pneumonia following treatment with infliximab for Crohn's disease. Inflamm Bowel Dis. 2001;7:327. doi: 10.1097/00054725-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Foster KJ, Devitt N, Gallagher PJ, Abbott RM. Overwhelming pneumococcal septicaemia in a patient with ulcerative colitis and splenic atrophy. Gut. 1982;23:630–632. doi: 10.1136/gut.23.7.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melmed GY, Ippoliti AF, Papadakis KA, et al. Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol. 2006;101:1834–1840. doi: 10.1111/j.1572-0241.2006.00646.x. [DOI] [PubMed] [Google Scholar]
- 14.Loras C, Saro C, Gonzalez-Huix F, et al. Prevalence and factors related to hepatitis B and C in inflammatory bowel disease patients in Spain: a nationwide, multicenter study. Am J Gastroenterol. 2009;104:57–63. doi: 10.1038/ajg.2008.4. [DOI] [PubMed] [Google Scholar]
- 15.Wasan SK, Coukos JA, Farraye FA. Vaccinating the inflammatory bowel disease patient: deficiencies in gastroenterologists knowledge. Inflamm Bowel Dis. 2011;17:2536–2540. doi: 10.1002/ibd.21667. [DOI] [PubMed] [Google Scholar]
- 16.Yeung JH, Goodman KJ, Fedorak RN. Inadequate knowledge of immunization guidelines: a missed opportunity for preventing infection in immunocompromised IBD patients. Inflamm Bowel Dis. 2012;18:34–40. doi: 10.1002/ibd.21668. [DOI] [PubMed] [Google Scholar]
- 17.Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008;14:542–549. doi: 10.1002/ibd.20310. [DOI] [PubMed] [Google Scholar]
- 18.Wasan SK, Baker SE, Skolnik PR, Farraye FA. A practical guide to vaccinating the inflammatory bowel disease patient. Am J Gastroenterol. 2010;105:1231–1238. doi: 10.1038/ajg.2009.733. [DOI] [PubMed] [Google Scholar]
- 19.Nichol KL, Mac Donald R, Hauge M. Factors associated with influenza and pneumococcal vaccination behavior among high-risk adults. J Gen Intern Med. 1996;11:673–677. doi: 10.1007/BF02600158. [DOI] [PubMed] [Google Scholar]
- 20.Kwon OS, Park YS, Choi JH, et al. A case of ulcerative colitis relapsed by influenza vaccination. Korean J Gastroenterol. 2007;49:327–330. [PubMed] [Google Scholar]
- 21.Fields SW, Baiocco PJ, Korelitz BI. Influenza vaccinations: should they really be encouraged for IBD patients being treated with immunosuppressives? Inflamm Bowel Dis. 2009;15:649–651. doi: 10.1002/ibd.20731. [DOI] [PubMed] [Google Scholar]
- 22.Melmed GY. Vaccination strategies for patients with inflammatory bowel disease on immunomodulators and biologics. Inflamm Bowel Dis. 2009;15:1410–1416. doi: 10.1002/ibd.20943. [DOI] [PubMed] [Google Scholar]
- 23.Moscandrew M, Mahadevan U, Kane S. General health maintenance in IBD. Inflamm Bowel Dis. 2009;15:1399–1409. doi: 10.1002/ibd.20944. [DOI] [PubMed] [Google Scholar]
- 24.Dotan I, Werner L, Vigodman S, et al. Normal response to vaccines in inflammatory bowel disease patients treated with thiopurines. Inflamm Bowel Dis. 2012;18:261–268. doi: 10.1002/ibd.21688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mamula P, Markowitz JE, Piccoli DA, Klimov A, Cohen L, Baldassano RN. Immune response to influenza vaccine in pediatric patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5:851–856. doi: 10.1016/j.cgh.2007.02.035. [DOI] [PubMed] [Google Scholar]
- 26.Lu Y, Jacobson DL, Ashworth LA, et al. Immune response to influenza vaccine in children with inflammatory bowel disease. Am J Gastroenterol. 2009;104:444–453. doi: 10.1038/ajg.2008.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gelinck LB, van der Bijl AE, Beyer WE, et al. The effect of anti-tumour necrosis factor alpha treatment on the antibody response to influenza vaccination. Ann Rheum Dis. 2008;67:713–716. doi: 10.1136/ard.2007.077552. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Content of the Questionnaire Regarding Vaccination Information
Vaccination Recommendations in IBD Patients