Abstract
Members of the genus Brucella are pathogenic bacteria exceedingly well adapted to their hosts. The bacterium is transmitted by direct contact within the same host species or accidentally to secondary hosts, such as humans. Human brucellosis is strongly linked to the management of domesticated animals and ingestion of their products. Since the domestication of ungulates and dogs in the Fertile Crescent and Asia in 12000 and 33000 ya, respectively, a steady supply of well adapted emergent Brucella pathogens causing zoonotic disease has been provided. Likewise, anthropogenic modification of wild life may have also impacted host susceptibility and Brucella selection. Domestication and human influence on wild life animals are not neutral phenomena. Consequently, Brucella organisms have followed their hosts’ fate and have been selected under conditions that favor high transmission rate. The “arm race” between Brucella and their preferred hosts has been driven by genetic adaptation of the bacterium confronted with the evolving immune defenses of the host. Management conditions, such as clustering, selection, culling, and vaccination of Brucella preferred hosts have profound influences in the outcome of brucellosis and in the selection of Brucella organisms. Countries that have controlled brucellosis systematically used reliable smooth live vaccines, consistent immunization protocols, adequate diagnostic tests, broad vaccination coverage and sustained removal of the infected animals. To ignore and misuse tools and strategies already available for the control of brucellosis may promote the emergence of new Brucella variants. The unrestricted use of low-efficacy vaccines may promote a “false sense of security” and works towards selection of Brucella with higher virulence and transmission potential.
Keywords: brucellosis, Brucella, zoonosis, Brucella-vaccines, domestication
INTRODUCTION
Brucellosis is a vicious disease caused by facultative intracellular extracellular pathogens of the genus Brucella (Moreno and Moriyón, 2002). The bacterium preferentially replicates within phagocytic cells of the reticuloendothelial system, and in the pregnant animal, inside placental trophoblasts. In domesticated animals, brucellosis is mainly manifested by abortion and epididymitis. Under natural conditions, Brucella is horizontally or vertically transmitted. Horizontal transmission occurs through close contact from host to host by means of secretions, sexual intercourse, and more commonly, through liking of aborted fetuses (Figure 1). Although Brucella has been observed to survive for some time in open environments, the bacterium hardly divides and eventually dies (Crawford et al., 1990). Likewise, some vectors have sporadically been implicated in brucellosis transmission (Gudoshnik, 1958; Dawson et al., 2008; Neglia et al., 2013). However, neither of these two last events plays a significant role in the transmission of brucellosis and they are not of epidemiological relevance (Meyer, 1977; Moreno and Moriyón, 2006).
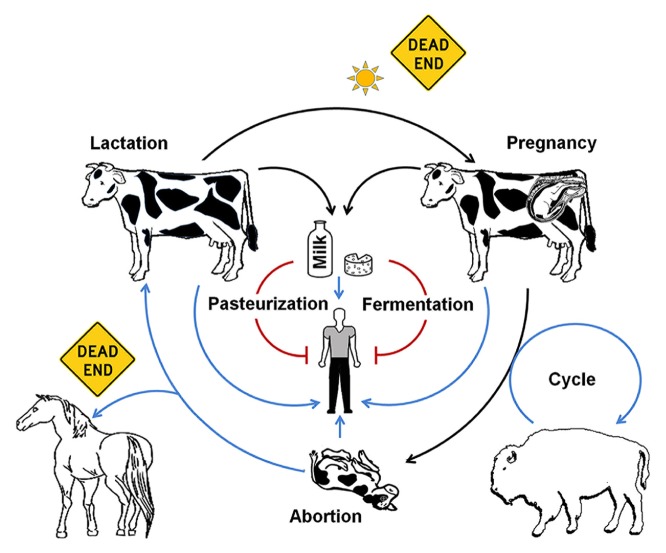
FIGURE 1.
Brucella (B. abortus) life host cycle. After host infection the invading Brucella replicates within cells of the reticuloendothelial system where it remains for a protracted period of time. After pregnancy, the bacterium invades trophoblasts and the mammary gland. In these sites the bacterium extensively replicates inducing abortion and shedding through milk (black arrows). The heavy contaminated placenta and fetus become the main source of infection for humans and other animal hosts (blue arrows). Humans may acquire the bacterium through ingestion of unpasteurized dairy products. Brucella may live up to several weeks, as long as enough organic material is available and the bacterium is protected from the sun’s rays. When exposed to sun’s rays in the open, Brucella organisms steadily die (doted black arrow). Pasteurization or fermentation of dairy products eliminates Brucella organisms and the risk of human contamination (red blunt arrows). Cross contamination of wild life animals (e.g., bison at lower right) may maintain the bacteria cycling within wild herds, and then of epidemiological relevance. Humans and other animals (e.g., horses) are considered dead ends for the bacterium, and therefore there are not of epidemiological relevance.
In humans, the disease is more severe than in domestic animals, displaying a collection of clinical symptoms (Dalrymple-Champneys, 1960; Pedro-Pons et al., 1968; Figure 2). While there are a few reports of vertical and horizontal transmission between humans (Meltzer et al., 2010; Wyatt, 2010), these are rare events. Therefore, brucellosis in humans is strongly linked to the management of infected animals and ingestion of unpasteurized dairy products (Moreno and Moriyón, 2006; Figure 1). In this regard, there is a clear connection of brucellosis with the domestication of even-toed ungulates, milking practices, and fabrication of cheese and other dairy products. It is, therefore, not accidental that lactase persistence – a genetic trait that allows adults to digest lactose from raw milk – has been traced to ungulate domestication places (Sahi, 1994; Enattah et al., 2008; Itan et al., 2010) and in course with the persistence of brucellosis in ancient pastoral people.
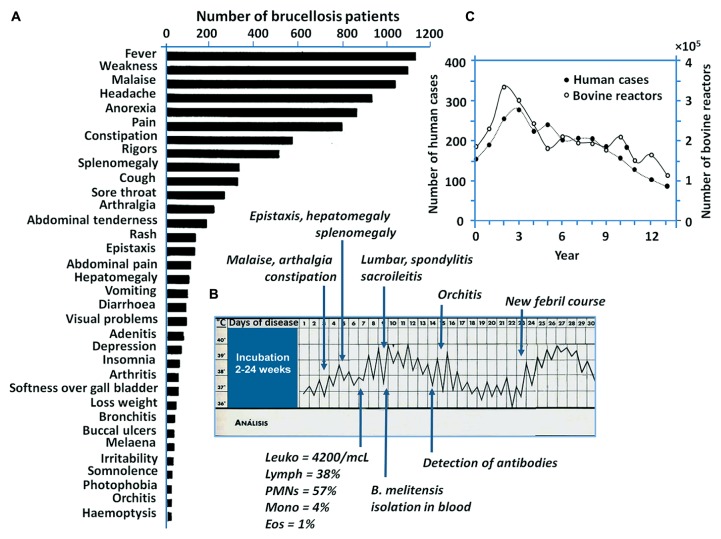
FIGURE 2.
Brucellosis in humans. (A) The bar graphic displays the most frequent 34 signs of brucellosis recorded in 1500 patients with proved disease (adapted from Dalrymple-Champneys, 1960). (B) The clinical chart displays the typical “undulant fever” suffered by one patient with subsequent clinical signs of brucellosis (adapted from Pedro-Pons et al., 1968). (C) Human brucellosis cases and bovines displaying positive Brucella infections in United States during 13 year lapse period (1976–1986; adapted from Nicoletti, 1989). In contrast to the silent course of brucellosis in non-pregnant domestic animals, brucellosis in humans courses with a broad collection of clinical symptoms. Notice that the increase and decrease of human brucellosis cases roughly correlates with the increase or decrease of the infection in cattle.
At no other time in human history have the changes in technology, domestication and environment been more rapid and so extreme. For thousands of years humans have created new ways of living and social actions have emerged to minimize the effects of infectious diseases. However, domestication and clustering of wild life reservoirs with narrower genetic backgrounds have provided a steady supply of emergent pathogenic organisms. In this regard, brucellosis constitutes an utmost example of a how animal pathogens can emerge as public and veterinary health problems. Here I review how humans have fostered the illness we now call brucellosis that has accompanied civilization since ancient times, when the malady was recognized by its main symptoms: abortion and fever.
THE DISCOVERY OF Brucella AND BRUCELLOSIS
The seminal discovery of the causative agent of brucellosis, “Micrococcus melitensis” (later named Brucella melitensis), by the British Surgeon Captain David Bruce, his wife Mary Elizabeth Steele and the Maltese microbiologist doctor Giuseppe Caruana-Scicluna has been eagerly described in many assays (Spink, 1956; Ruiz-Castañeda, 1986; Wyatt, 2000, 2009a). These scientists isolated the bacterium from the liver of diseased soldiers in the Mediterranean island of Malta in 1887, a country that holds prominent megalithic constructions beyond 7000 years old. Following this discovery, the Maltese medical doctor Fioravanti Temistocle Archimede Laurenzo Giuseppe Sammut, better known as “Temi Zammit,” found that the causative agent of Malta fever, Mediterranean fever, Cyprus fever, Neapolitan fever, Gibraltar fever, Crimean fever, Cartagena fever, Rock fever, Barcelonan fever, Corps disease, and undulant fever – just to mention a few names used for this vicious malady – was transmitted from infected goats to humans through contaminated milk (Wyatt, 2005, 2011). Thereafter, Surgeon Captain M. Louis Hughes and Captain James Crawford Kennedy discovered significant details on the zoonotic transmission of brucellosis, including venereal transmission in both humans and animals (Wyatt, 2009b).
Ten years after the isolation of M. melitensis, the Danish scientist Bernhard Bag identified “Bacillus abortus” (later named Brucella abortus) in bovine aborted fetuses (Bang, 1897). Traum (1914) reported the isolation of another organism related to M. melitensis (later assigned as Brucella suis) from aborted pigs in United States. But the final link of these zoonotic bacteria was accomplished in 1918 by the outstanding American microbiologist Alice Catherine Evans (Evans, 1918). Her achievements helped to understand the epidemiology of brucellosis and contributed to the founding of milk pasteurization as preventive measure. Then, in 1920, Louis Meyer and Wilbur Shaw honored David Bruce and proposed to group these pathogenic bacteria within a single genus named Brucella (Meyer and Shaw, 1920).
The events that followed all these inspiring investigations have demonstrated the existence of different Brucella species (Figure 3) that cause brucellosis in domestic animals (cows, sheep, goats, pigs, camels, reindeer, and dogs), wild land animals (bison, elk, hares, muskox, caribou, foxes, and several rodents) and sea mammals (dolphin, whales, seals, and walruses; Godfroid et al., 2011; Guzmán-Verri et al., 2012). Despite of this diversity the only species that are linked to human brucellosis are B. melitensis, B. suis, B. abortus, and to minor extent Brucella canis (Moreno and Moriyón, 2006); this last specie being the causative agent of canine brucellosis (Carmichael and Bruner, 1968). Apart from this group there are other Brucella strains (e.g., B. inopinata) that have been rarely isolated from humans (McDonald et al., 2006; De et al., 2008; Scholz et al., 2010); however, no connection between zoonotic transmission and disease has been established.
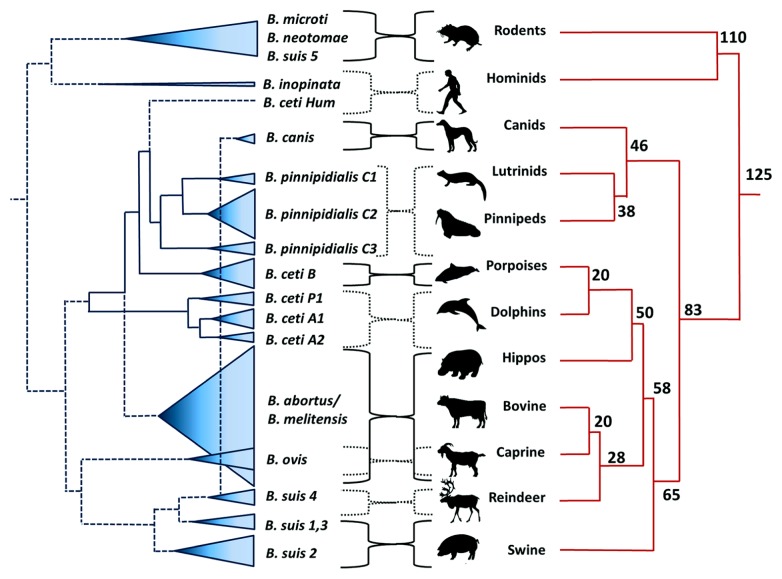
FIGURE 3.
Dispersion of Brucella species confronted to the phylogeny of their preferred host mammal. The dispersion of the various Brucella species is depicted as cones proportional to the number of strains analyzed. The numbers in the mammal phylogenetic tree represent millions of years. B. suis biovar 2 also has affinity for hares (lagomorphos). B. ceti Hum (human type) does not correspond phylogenetically to B. ceti group and this single isolate requires taxonomic definition. The source of the two isolates of B. inopinata is unknown. Notice that phylogenetic relationship between the two clades is not perfect suggesting that carnivore mammals acquire brucellosis (probably by depredation) after the initial dispersion of cetaceans and ungulates from an ancestral mesonychid, close to 65–60 million ya. Phylogenetic dendrogram was adapted from Guzmán-Verri et al. (2012).
Members of the genus Brucella are phyllogenetically related to α-Proteobacteria that live in close association with animal and plant cells (Moreno and Moriyón, 2002). From the genotypic perspective the genus is monophyletic with DNA similarity above 97% (Verger et al., 1985). In spite of this, Brucella species can be distinguished by single-nucleotide polymorphism analysis, host preference and conspicuous differences in virulence (Bosseray et al., 1982; Foster et al., 2012). In addition, there are several straight forward phenotypic differences, being the most obvious the absence of surface O-polysaccharide chain in naturally occurring rough species such as B. canis and Brucella ovis (Moreno and Moriyón, 2006). One interesting feature of the genus is the absence of plasmids and lysogenic phages, a phenomenon that precludes the horizontal transference of genes through classical routes (Moreno, 1998). Based on this, it has been proposed that the extant Brucella species expand clonally within the host environment and that genetic drift depends almost exclusively on mutation and internal genetic rearrangements (Moreno, 1998).
Brucellosis is one of the few diseases in which efficient live bacterial vaccines (e.g., B. abortus S19 and B. melitensis Rev1) have been developed (Cotton et al., 1933; Elberg and Meyer, 1958). Likewise, through history of microbiology very few diseases have more diagnostic tests than brucellosis (Moreno and Moriyón, 2006). As expected, the isolation of the bacterium stands as the gold standard. However, simple techniques, such as the Rose Bengal test, have survived all challenges and are the most wildly used serological assays (Díaz et al., 2011). This is not by chance, since by the combination of immunization with smooth vaccines, Rose Bengal serological diagnosis and culling of the animals, brucellosis has been controlled and eradicated in many countries of the world (Davidson, 1970; Crawford and Hidalgo, 1977; Whittem, 1978; Wise, 1980; Chamberlin, 1985; Crawford et al., 1990).
THE EMERGENCE OF ZOONOTIC BRUCELLOSIS
Through coordinated measures, brucellosis was finally eradicated from the island of Malta 90 years after the discovery of the disease (Wyatt, 2009a). Unfortunately, this has not been the fate of other areas around the Mediterranean Sea, mainly in African, eastern Mediterranean, and Middle East countries, where the disease has been endemic for thousands of years and from which brucellosis was spread around the world (Figure 4).
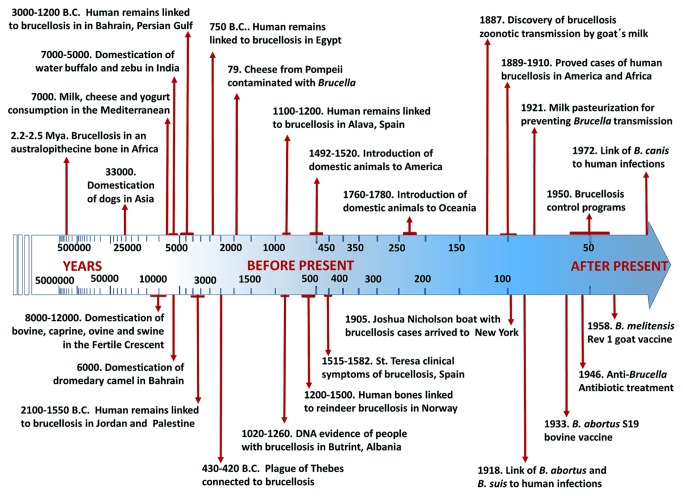
FIGURE 4.
Timeline of events associated with zoonotic brucellosis. The scale increases logarithmically from 5 million years in the past to 50 years estimated as the “present” (in 1950). Dates are designated as indicated in the main text.
ZOONOTIC BRUCELLOSIS IN EURASIA AND MIDDLE EAST
Analogous to the island of Malta, Butrint in Albania keeps valuable World Heritage Sites that give testimony on the existence of pastoral inhabitants for millennia (Ryder, 1981). Pathological studies and DNA analysis performed in human remains from graves dated 1260–1020 ya, revealed the presence of Brucella as the causative agent of the disease that affected these Middle Age inhabitants in the ancient city of Butrint (Mutolo et al., 2012). In addition to Albania, other Balkans countries such as Macedonia and Bosnia and Herzegovina still struggle with animal and human brucellosis; a phenomenon that was boosted by the decline of veterinary and health services in these countries during the political and armed conflicts in the 1990s (Bosilkovski et al., 2010; Puto et al., 2010; Ahmetagic et al., 2012). Human brucellosis outbreaks have also thrived in Balkan neighboring countries such as Greece, Italy, and Turkey (Minas et al., 2007; Mancini et al., 2013). Most likely the disease was endemic in these Mediterranean counties since the beginning of civilization (D’Anastasio et al., 2011). Remains of cheese buried in Pompeii and Herculaneum have been associated with the transmission of brucellosis in Roman imperial times (Capasso, 2002). Likewise, a critical analysis of Thucydides’ history regarding the plague of Athens (2430–2420 ya) suggests the presence brucellosis (Kousoulis et al., 2012). Archeological evidence from 7000 ya in the eastern Mediterranean region of Anatolia demonstrated ancient skills to transport milk and to manufacture yogurt and cheese, all vehicles for brucellosis contagion (Evershed et al., 2008).
Presumptive human brucellosis cases in skeletal remains from the Bronze Age (4100–3550 ya) have been found in Palestine and Jordan (Capasso, 2002; D’Anastasio et al., 2011). It is not coincidental that these places are close to the Fertile Crescent and Taurus Mountains, sites where sheep, goats, cows, and pigs – all known to be preferred Brucella hosts – were domesticated between 12000 and 10000 ya (Nelson, 1998; Naderi et al., 2008; Pariset et al., 2011; Bonfiglio et al., 2012). Brucellosis has been also implicated in Bronze Age sites located in Bahrain, Persian Gulf (Rashidi et al., 2001; D’Anastasio et al., 2011). This archipelago belongs to a region where the dromedary camel – another common Brucella host – was domesticated about 6000 ya (Peters, 1997). In this area, human brucellosis acquired through the ingestion of camel dairy products is still endemic, mainly in semi-nomadic Bedouin populations (Rafai, 2002; Shimol et al., 2012). Analyses of human DNA remains from 5000 to 4500 ya have revealed that late Neolithic Europeans displayed lower frequency of lactase persistence than modern extant populations (Plantinga et al., 2012). This is compatible with evolutionary pressures related to the consumption of raw milk and consequently with higher chances to become infected with Brucella.
Brucellosis is highly prevalent in Asia (Zhang et al., 2010; Denisov et al., 2013; Li et al., 2013). Paleopathological evidence indicates that Lapp people in the Artic area of Northern Eurasia domesticated reindeer (the preferred host for B. suis biovar 4) 3000–2000 ya or even earlier (Røed et al., 2011; van Kolfschoten et al., 2011) and that these inhabitants also suffered from brucellosis (Ortner, 2003; Røed et al., 2011). Bovine and swine were already present in China, Mongolia, and Korea, at least 5000 ya or even before, shortly after their domestication in the Fertile Crescent (Nelson, 1998; Giuffra et al., 2000; Zhang et al., 2013). It seems that water buffalo (Bubalus spp.) was also domesticated in China about 4000 ya (Teasdale and Bradley, 2012). However, milk and derived dairy products are not commonly found in East Asian cuisines, a culinary activity that is compatible by the lactose intolerance distribution in these populations (Itan et al., 2010). Two exceptions are human groups living in the Asian steppes and Mongolia who still consume milk and fermented dairy products; then keeping lactose tolerance and human brucellosis. It is likely that brucellosis was endemic in these areas before imperial times.
ZOONOTIC BRUCELLOSIS IN AFRICA AND INDIAN SUBCONTINENT
Human brucellosis is highly prevalent in India (Mantur and Amarnath, 2008). Bovine Bos indicus zebu breeds were domesticated in the Indus Valley region (today Pakistan) about 7000 ya (Teasdale and Bradley, 2012). An independent domestication of water buffalo was achieved in India about 5000 ya (Kumar et al., 2007). Infected water buffalos shed Brucella in the milk; however, these animals are more resistant to Brucella induced abortion than Bos species (Borriello et al., 2006; Adams and Schutta, 2010). An independent domestication of goats also occurred in the Indus Basin in Pakistan already 9000 ya (Joshi et al., 2004). Considering these events, it is striking that up to 80% of the Indian population is lactose intolerant. It has been determined that the mutation for lactose tolerance was introduced later on to eastward India from the Middle East (Gallego Romero et al., 2012). This suggests that ingestion of dairy products started later in India than in other regions, and with it, zoonotic brucellosis. Another alternative comes from how Indians prepare their milk: they often ferment it in the form of lassi or paneers, processes that break down the lactose and also kills Brucella organisms.
Human brucellosis was described in Mediterranean African countries more than 100 ya (Rafai, 2002). It is likely that brucellosis was present in human settlements in Northern Africa already 3000 ya and highly prevalent in Egypt during biblical times (e.g., OT, Isaiah 37:8–9, and 2 Kings 19:8–9). Studies performed in Egyptian archeological sites dated 750 B.C. have revealed several human hip bones with signs of brucellosis in this region (Hodgkins, 2002). Brucellosis in southern Africa was detected in dairy herds as early 1913 and the first human cases in 1921 (Bevan, 1931). It seems that the introduction of Indian and Eurasian bovine, sheep, and goat breeds into Africa occurred rapidly after their domestication in the Fertile Crescent. Nevertheless, it has been established that different African ethnic groups have distinct lactase gene mutations that arose independently in different locations between 6800 and 2700 ya (Tishkoff et al., 2007). These data fits well with archeological evidence suggesting that pastoral peoples reached eastern Africa in different migration waves, about 4500–3500 ya.
It is feasible that brucellosis existed in indigenous African Artiodactyla species (which include a significant number of potential Brucella hosts) long before the introduction of domesticated herds. A paleopathological study has suggested the presence of Brucella infections in australopithecines, already 2.5–2.3-million ya (D’Anastasio et al., 2009, 2011). As expected, this proposal not only has implications on the origin of the disease in local African fauna but, remarkably, also on the feeding habits of these human ancestors. In spite of this, it seems that Brucella infections in indigenous African mammals remain low (Gomo et al., 2012) and only relevant when wildlife ungulates become in contact with infected domesticated cows, goats, or sheep (Madsen and Anderson, 1995).
INTRODUCTION OF ZOONOTIC BRUCELLOSIS IN THE AMERICAN CONTINENT AND OCEANIA
The only indigenous Brucella specie in the American Continent seems to be Brucella neotomae, first isolated in United States from desert wood rats in 1957 (Stoenner and Lackman, 1957). B. neotomae is confined to these rodents with no other known hosts. The absence of domesticated ungulate reservoirs before European colonization very likely circumvented the presence of zoonotic brucellosis in the New World. This is revealed by the close to 100% lactose intolerance of adult Amerindians and in Inuit people (Alzate et al., 1969; Ellestad-Sayed et al., 1978; Sahi, 1994). Thus, it is unlikely that American inhabitants – who populated the continent between 12000 and 4000 ya – ingested milk from potential Brucella infected wild life ungulates such as bison, muskox, elk, or caribou. Therefore, the various zoonotic Brucella species were likely introduced in America during the last decade of the fifteenth century by the first Spaniards conquerors following the arrival of cattle in the colonies (Bowling, 1942). At that time brucellosis was probably highly endemic in the Iberian Peninsula. This is supported by the discovery of human remains from the late Middle Ages displaying pathological signs of brucellosis (Etxeberria, 1994) and by the description of the disease in Spain. For instance the clinical description of the “lousy fever” suffered by the mystic poet St. Teresa of Jesus – born 20 years after Christopher Columbus opened up the Western Hemisphere to European colonization – is compatible with brucellosis (Senra-Valera, 2006).
As for other infectious diseases, the spreading of brucellosis from the “Old World” to the “New World” very likely was a significant outcome of the conquests. It has been well documented that during his second voyage to the American Continent in 1493, Christopher Columbus introduced a significant number of cattle and pigs (de las Casas, 1951). Very probably by these means the introduction of brucellosis in the continent, including the contamination of indigenous fauna such as bison (Rhyan et al., 2013). Brucellosis was detected in a Yellowstone American buffalo herd already in 1917 (Mohler, 1917). Until the first half of the twentieth century, European cows shared with bison herds the same pasture lands (Bowling, 1942) making likely cross infection (Figure 1). Indeed, brucellosis in North American bison and elk has been related to cross contamination of bacterial strains (including vaccine strains) from infected European bovine breeds (Meagher and Meyer, 1994; Higgins et al., 2012). Furthermore, the same B. abortus biovars (1 and 2) are found in both classes of bovine herds. The disease in the American buffalo is similar to that of domesticated cattle (Rhyan et al., 2001b); though it is believed that bison, like water buffalo, may display some resistance to Brucella induced abortion (Herman, 2013).
The origin of B. suis biovar 4 infecting Canadian and Alaskan caribou and muskox has been traced to imported reindeer from Siberia, early in the twentieth century (Meyer, 1966; Forbes, 1991). Domesticated reindeer should be also considered a potential source of zoonotic disease since brucellosis – caused by B. suis biovar 4 – has been found in Eskimos (Davies and Hanson, 1965; Meyer, 1966; Forbes, 1991). Alternatively, B. suis biovar 4 could have arrived with infected caribou and muskox through the Bering Land Bridge during the last glaciation (Campos et al., 2010; Røed et al., 2011).
Human brucellosis was prevalent in Mexico, USA, and Canada for centuries (Spink, 1956; Wise, 1980; Ruiz-Castañeda, 1986). The first human cases in North America were recognized between 1889 and 1894 (Craig, 1903; Gentry and Ferenbaugh, 1911). With the exception of Mexico, nowadays the presence of human brucellosis has become a rare event in northern hemisphere of the American continent. This was the result of the successful pasteurization of dairy products and the application of control programs based in extensive immunization of herds with smooth Brucella vaccines, diagnostic tests such as Rose Bengal and complement fixation and efficient culling and management of animal flocks during the second half of the twentieth century (Crawford and Hidalgo, 1977; Wise, 1980). In contrast, the absence of coordinated control programs, poor management of animal flocks, and the introduction of vaccines with low efficacy have kept brucellosis highly prevalent in Mexico, Central America, and most South American countries (Moreno, 2002; Vargas, 2002; Lucero et al., 2008; Herrera-López et al., 2010; Godfroid et al., 2011; Aznar et al., 2012; Román et al., 2013; Rubach et al., 2013).
Brucella canis – the last Brucella zoonotic specie described – was discovered in Southern United States in the late 1960s (Carmichael and Bruner, 1968). Dogs were the first animals to be domesticated in the world. The earliest archeological vestiges are from Siberia dated 33000 ya; while in the American continent the oldest known ancient remains date 11000 ya (Leonard et al., 2002; Ovodov et al., 2011). Then, it was expected to find B. canis in dog’s wild relatives. However, there are no reports of B. canis in wolf or coyote packs and these wild canines seem to display some resistance to smooth Brucella species (Davis et al., 1988; Tessaro and Forbes, 2004). Nevertheless, it seems feasible that B. canis evolved in dog’s ancestor after predation of B. suis biovar 4 infected hosts in Asia (e.g., caribou/reindeer), since these two brucellae species are closely related (Figure 3). Moreover, wolves and Artic foxes can become naturally infected with rangiferine brucellosis (Neiland, 1975). As other zoonotic brucellae, B. canis might have penetrated to the American Continent during the European colonization. Alternatively, B. canis could have traveled in infected dogs through the Bering Strait already 12000 ya (Leonard et al., 2002). Presently, canine brucellosis has spread throughout the American Continent (Hollett, 2006; Tuemmers et al., 2013). In any case, the zoonotic potential of B. canis is low and just sporadic human cases have been reported in the world (Lucero et al., 2008).
Human and animal brucellosis were very important diseases in New Zealand and Australia as these countries keep large numbers of sheep and bovines. As expected, lactose intolerance occurrence in indigenous people from Oceania is above 95% (Enattah et al., 2008; Itan et al., 2010), a fact that agrees with the absence of indigenous large mammal animals in this region. It is therefore likely that human brucellosis stared with the arrival of infected domestic livestock to Oceania lands in the eighteenth century, through “The First Fleet” and in the ships commanded by Capitan Cook (Gillen et al., 1989). Before this, the only placental mammals (and potential Brucella hosts) in Australia were bats, some indigenous rats, mice, and the feral dog named “dingo” introduced from Asia 5000 ya (Ardalan et al., 2012). In New Zealand the only placental mammals were bats, kiore rats and the Polynesian dog named kurı-.
Bovine brucellosis was first recorded in New Zealand in 1893 and eradicated 106 years later by an aggressive program that included S19 vaccination, testing, and slaughter of the infected herds (Davidson, 1970). A comparable control program was followed by Australia with a great success (Whittem, 1978; Chamberlin, 1985). The first cases of ram epididymitis caused by Brucella ovis were recorded in New Zealand in 1953 (Buddle, 1956). Since B. ovis is not pathogenic for humans or other species of animals and mainly affects rams, there are no clear historical records regarding this disease before its discovery. In addition, Brucella strains have been isolated in rodents and foxes in Australia (Tiller et al., 2010a; Al Dahouk et al., 2012) and two unconventional Brucella strains (one in Australia and one in New Zealand) have been detected in humans (McDonald et al., 2006; Tiller et al., 2010b). In spite of this, no links with the transmission from animals to humans has been established in these cases. Canine brucellosis has just been recently found in domestic dogs in Australia (Gardner and Reichel, 1997; Hofer et al., 2012) but never reported in dingo or kurı- dogs. Presently, human and animal brucellosis are just sporadic in Australia and New Zealand, remaining feral pigs as the only source of human infections (Eales et al., 2010).
ARTIFICIAL SELECTION OF Brucella
Pathogens and hosts evolve in response to each other and the genetic diversity of both parties represents a pool of possible variants to maintain adaptation via natural selection (Ewald, 2004). Thus, the “arm race” between Brucella and preferred hosts has been driven by genetic adaptation of the bacterium virulent systems confronted with the evolving immune defenses of the host. Domestication, anthropogenic modification of wild life and selection of animals by humans are not neutral phenomena. In each event a concomitant selection of the parasitic microbiota occurs (Pearce-Duvet, 2006). Consequently, it is expected that the prevalent extant Brucella strains have been selected through “narrow funnels” connected to these processes.
Brucella SELECTION THROUGH DOMESTICATION OF ANIMALS
It does not seem by chance that the most virulent Brucella species with higher zoonotic spectrum are those from domesticated animals; while those that display lower pathogenicity and zoonotic potential are those from wild life animals (Figure 5). Reports of human infections from wildlife reservoirs are scarce. Moreover, within the zoonotic brucellae there are some species that are more virulent than others (e.g., B. melitensis > B. suis biovars 1, 3, and 4 ≥ B. abortus > B. canis; Spink, 1956; Bosseray et al., 1982; Ruiz-Castañeda, 1986; Caron et al., 1994). In contrast, Brucella ceti and Brucella pinnipedialis preferentially infecting free living cetaceans and pinnipeds, respectively, have seldom been found in other animal groups and their zoonotic potential and overall virulence for other animal species, including bovine and swine, seem low (Rhyan et al., 2001a; Perrett et al., 2004; Bingham et al., 2008; Guzmán-Verri et al., 2012). Likewise, Brucella species and strains (e.g., B. neotomae, B. microti, and B. suis biovar 5) having preference for wild land mammals are confined to their natural hosts and seldom found in domestic animals or humans (Moreno and Moriyón, 2006; Al Dahouk et al., 2012). Therefore, it is expected that the most prevalent virulent Brucella strains were selected during the domestication of animals.
FIGURE 5.
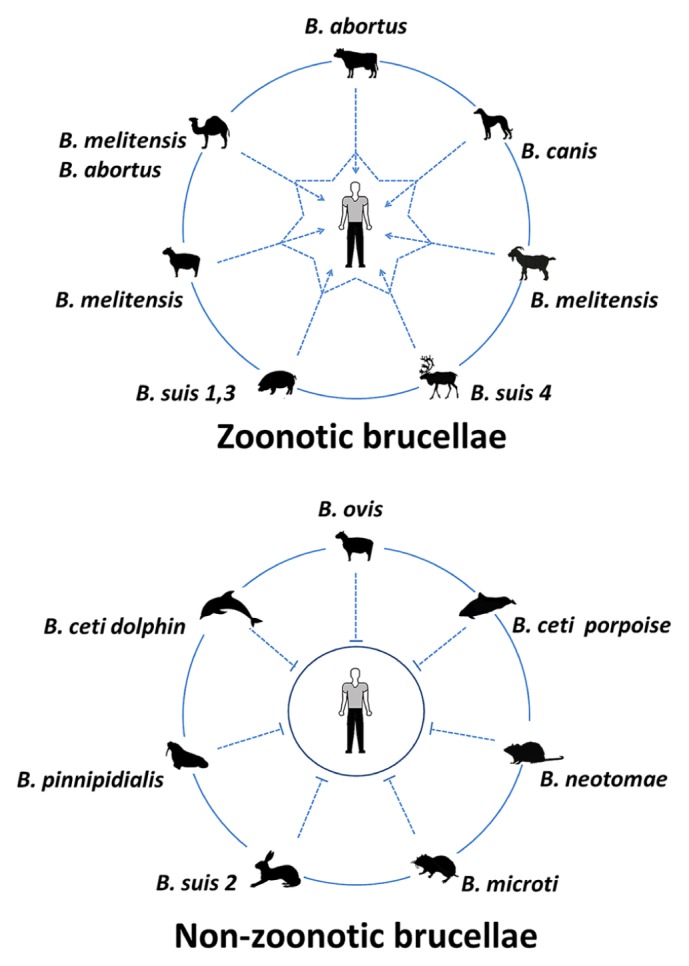
Zoonotic and non-zoonotic Brucella species. The most virulent species with higher zoonotic spectrum are those from domesticated animals; while those displaying lower pathogenicity and zoonotic potential are those from wild life animals. One exception is B. ovis which is a pathogen for rams and does not infect other hosts.
The selection of Brucella towards lower or higher virulence has been demonstrated experimentally. Through mutagenesis of genes coding for the so called virulent determinants or regulatory molecules Brucella may become attenuated (González et al., 2008; Barrio et al., 2009; Wang et al., 2012). Likewise, by means of genetic manipulation or selection through serial passages into animals, Brucella strains can become robust pathogens (Gibby and Gibby, 1965; Jiménez de Bagüés et al., 2010; Grilló et al., 2012; Terwagne et al., 2013).
In addition of displaying host preferences, the various Brucella species and strains also form genetic groups that relate with distinctive geographic origins (Le Flèche et al., 2006; Foster et al., 2012; Garofolo et al., 2013; Jiang et al., 2013; Di et al., 2014). This means that Brucella clones rapidly expand and transmit within domesticated groups of animals. In spite of their high DNA similarity, the various bacterial species and strains are selected and form discrete family clusters. These observations parallel those showing that some Brucella strains may have been removed or minimized from the bacterial pool as consequence of the control programs. Indeed, several B. abortus biotypes described decades ago (Crawford et al., 1990; Meyer, 1990) have not been isolated for more than 40 years; instead, predominant variants remain in bovine herds. Therefore, it is feasible that Brucella selection towards higher transmissibility and replication occurs through successive infections in confined hosts, as proposed for the evolution of other diseases (Ewald, 2004).
One exception is B. ovis (Figure 5). Although this bacterium may have been also subjected to selection processes during the domestication of sheep, it remains non-pathogenic for humans or for other animals (Blasco, 1990). In general, rough brucellae such as B. ovis are less virulent than their smooth counterparts and have narrower ability to infect other hosts (Moreno and Moriyón, 2006; González et al., 2008). It may be that B. ovis was already selected towards a higher affinity for venereal transmission in sheep before domestication of ovine, as suggested before (Moreno, 1992). Moreover, the basal “deep” phylogenetic location of B. ovis in relation to B. abortus, B. melitensis, B. suis, and B. canis clusters (Foster et al., 2012), also suggests earlier adaptation of B. ovis to its host.
HERD SIZE AND POPULATION DENSITY IN THE SELECTION OF Brucella
Other trend that has favored the prevalence and dissemination of brucellosis corresponds to the intensive exploitation of productive animals (Crawford et al., 1990). Humans have taken advantage of the innate social behavior of ungulates and canines and clustered them in small areas. In addition, following anthropocentric purposes, the genetic background of these domestic animals has been narrowed. As in other infectious disease, lower genetic diversity and crowded effect may favor transmission and select for faster replicating organisms with major zoonotic potential (McDaniel et al., 2013). Examples of these were observed in the early days of brucellosis in Malta (Wyatt, 2005, 2009a), and more recently in foodborne outbreaks in Peru (Román et al., 2013) and massive outbreaks in Inner Mongolia, threatening hundreds of thousands of people.
Inner Mongolia, which keeps the largest sheep population (18.2% of the flock), also ranks first in animal and human brucellosis in China (Pu et al., 2009; Mi et al., 2010; Zhang et al., 2010). In 2007, new brucellosis cases were reported in 85 out of 102 districts in Inner Mongolia, with positive prevalence remaining in the other 47 districts. From 1996 to 2010, 78246 human cases were detected with 90% of the new cases reported between 2005 and 2010. This accounts for 40% of the near 200000 cases detected in China for this period. In 2010, this figure reached 47.2%. According to various models, this may be just the “tip of the iceberg” and it is expected that the number of human cases will increase dramatically in the following years (Hou et al., 2013). Moreover, it has been demonstrated that in endemic areas about 20% of the infected individuals remain undiagnosed. Indeed, family members of the patients with brucellosis are under increased risk of acquiring the disease (Tabak et al., 2008). Thus, family screening in endemic areas is recommended.
Novel circumstances for fast transmission of zoonotic brucellosis have also been observed in confined semi-nomadic Bedouins infected from camel’s milk (Shimol et al., 2012; Shemesh and Yagupsky, 2013) and commercial dog kennels. Camels cohabiting with goats and sheep in small areas are becoming a common practice in Middle East and Arab countries. Dog packs seldom exceed more than a dozen individuals. Consequently, in crowded kennels B. canis spreads rapidly inducing massive abortions in bitches, testicular degeneration in males, and becomes a zoonotic risk (Lucero et al., 2008; Gyuranecz et al., 2011; Reynes et al., 2012; Marzetti et al., 2013). Therefore, intensive exploitation and clustering of animals in poor epidemiological control conditions may favor selection for faster Brucella transmission and zoonotic disease.
SELECTION OF Brucella IN WILDLIFE ANIMALS
Distinct Brucella clusters have also been identified in wild life animal populations located in areas separated by natural barriers (Forbes, 1991; Maquart et al., 2009; Guzmán-Verri et al., 2012). As with domesticated species, anthropogenic modification of wild life may also have narrowed the genetic diversity, impact host susceptibility and pathogen transmission. A noteworthy event has been the threatening of the American buffalo which was close to extinction (Hornaday, 1889). Thus, the prevailing bison herds have been founded by a small group of few surviving individuals (Gross and Wang, 2005). This is relevant since North American bison herds remain infected with B. abortus (Rhyan et al., 2001b). The European counterpart of this incident corresponds to the Alpine ibex (Capra ibex). Historically these wild goats were endemic throughout the European Alps. Due to excessive hunting and constrain of their natural habitat, the ibex herds in Central Europe declined to low dangerous numbers. As consequence, the founding of new ibex herds in the Alps come from a pool of few animals, narrowing their genetic diversity (Biebach and Keller, 2009). In certain areas ibex herds are infected with B. melitensis strains displaying also high seroprevalence (Ferroglio et al., 1998; Mick et al., 2014). Therefore, these wild goats may become a source for the reintroduction of B. melitensis in domestic ruminants and humans in Central Europe (Mailles et al., 2012; Hars et al., 2013; Rautureau et al., 2013).
Another example relates to the hunting of marine mammals, linked to the overexploitation of their natural food resources and contamination of the seas. These negative activities have promoted clustering of different Brucella infected marine mammals in reduced areas where food is available, causing excessive competition, undernutrition, stress, and immunosuppression (Ohishi et al., 2008; Van Bressem et al., 2009). As revealed by the increasing brucellosis case reports in some species of cetaceans over others (Maquart et al., 2009; Guzmán-Verri et al., 2012), these unnatural conditions may favor the selection of Brucella organisms with higher transmission rate.
Brucella divergence seems linked to selective forces within the host environment, and consequently, to the evolution of the host (Moreno, 1998). However, this constrain is not absolute and Brucella species living in wild life or in semi-domesticated hosts may still qualify as potentially pathogens for humans and domestic animals (Godfroid et al., 2011). The phenotypes of B. ceti, B. pinnipedialis, B. microti, and B. neotomae correspond to smooth types equipped with all known “virulent” factors (Audic et al., 2009; Guzmán-Verri et al., 2012). Up to now “mysterious” subtle differences with the classical zoonotic Brucella have kept these other wildlife species out from causing disease in humans. But the correlation of the various species in relation to host preference is not perfect and phylogenic patters suggest that Brucella organisms are capable to breakdown the species barrier and “jump” from one mammal order to a very differ one (Figure 3). Eventually, this might favor the persistence of a distinct Brucella clone in a different “preferred” host.
COPING WITH BRUCELLOSIS
In the presence of brucellosis, management becomes highly demanding (Spink, 1956; Ruiz-Castañeda, 1986; Moreno and Moriyón, 2006). Domesticated animals and humans have coexisted for millennia without significant intervention measures to control the disease. It is likely that a large part of the prevalent Brucella zoonotic species was selected in flocks during this long-lasting initial period. In some regions of the world, mainly in low income countries, these weak control actions are still common (Rubach et al., 2013). It is likely that a fraction of the genetic background of both humans and animals has been also shaped during the coexistence with Brucella organisms; mainly nearby to the regions where domestication took place (Pashaei et al., 2009; Asaei et al., 2013; Rasouli et al., 2013).
ERADICATING BRUCELLOSIS
After the discovery of Brucella organisms and their mode of transmission, direct measures toward the control and eradication of the disease were taken in several countries. As stated, killing of the bacterium by milk heating was one of the first procedures that prevented the transmission of brucellosis. A second relevant action was the discovery of diagnostic techniques capable to distinguish infected animals (Alton et al., 1988). Third, was the development of efficient vaccines for protecting bovine, caprine, and ovine herds (Cotton et al., 1933; Elberg and Meyer, 1958). In addition, in some areas systematic slaughtering of the infected animals reduced the density of the bacterium (Ebel et al., 2008). Though, the control of brucellosis by the sole action of culling the infected animals is extremely expensive and not practical under high disease prevalence conditions (Moreno, 2002; Office International des Épizooties, 2013). Following this, massive vaccination in combination with serological diagnoses and culling of the infected animals has become the chief strategy for the control of brucellosis (Office International des Épizooties, 2013). Countries where brucellosis has effectively been controlled have used the following procedures: reliable live vaccines (e.g., S19 and Rev1), adequate immunization protocols (e.g., single dose vaccination, reduced dose), extensive protection coverage (e.g., 100% of the herds at risk), suitable diagnostic tests (e.g., Rose Bengal, RID, Complement fixation, iELISA), sustained removal of the infected animals and restriction in the traffic of animals from infected herds to free herds (e.g., control transhumance herds; Davidson, 1970; Whittem, 1978; Wise, 1980; Moreno and Moriyón, 2006; Ebel et al., 2008). Accordingly, these countries have also narrowed the genetic pool of virulent brucellae and succeeded in eradicating human brucellosis.
THE BASIC REPRODUCTIVE NUMBER AND SELECTION OF VIRULENCE THROUGH VACCINATION
The basic reproductive number, also known as R0, is the average number of secondary infections arising from one infected individual in a completely susceptible animal population (Gandon et al., 2001). That is, for the disease to spread and for an effective animal to animal Brucella transmission it is required that the pathogen’s R0 exceeds 1 (Figure 6). In contrast if R0 < 1, then the disease has the tendency to fade away. Higher the R0 value, higher will be the number of subsequently infected individuals. Concomitantly, larger and denser the population of susceptible individuals higher would be the chances for the pathogen to achieve a steady and successful adaptation in the host. As consequence of a collection of unsuccessful events in many middle and low income countries (Moreno, 2002; Blasco and Moriyón, 2005), the R0 value exceeds 1; thus keeping the disease and the zoonotic potential high (Vargas, 2002; Godfroid et al., 2011; Aznar et al., 2012; Chand and Chhabra, 2013; Denisov et al., 2013; Jiang et al., 2013; Li et al., 2013; Rubach et al., 2013).
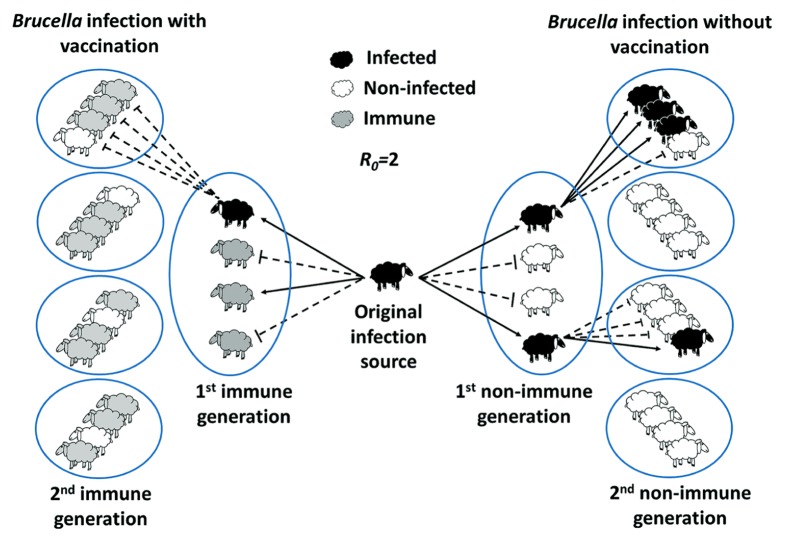
FIGURE 6.
Herd immunity theory and the basic reproductive ratio (R0) in Brucella herd infections. Herd immunity theory proposes that the protective effect of Brucella vaccinated individuals in a given population extends beyond to unvaccinated population. R0 corresponds to the average number of new Brucella infections caused by single infected source. If acquired immunity is present in the herd, the population is no longer entirely susceptible. The greater the proportion of individuals is immune to Brucella, the smaller the probability that a susceptible host will come into contact with an infectious animal. Then, the transmission from one animal to other is likely to be disrupted when an appropriate number of the population (predicted on the basis of R0) are immune to the bacterium. For instance, if R0 = 2 (an estimated R0 for B. melitensis transmission in sheep), then a geometric increase in infections occurs over time (right panel). If 75% of the population is protected by the vaccine (minimal protection rate estimated for Rev1 vaccine), then the bacteria fails to grow in the host animal and be transmitted (left panel). It is predicted that vaccines with lower protection rate require larger coverture and greater actions of culling of the animals. New productive infections are depicted by black solid arrows; unproductive transmission is indicated by dashed blunt arrows.
Yet, brucellosis is a complex disease and significant political and economic interests are often in play (Moreno, 2002; Pappas and Memish, 2007; Lundquist, 2012). Of all the problems in control programs, the introduction of low protection rate vaccines stands as a major drawback (Blasco et al., 1993; Verger et al., 1995; Moriyón et al., 2004; Godfroid et al., 2011). Apart from their failure in controlling brucellosis, there are long-term consequences in the use vaccines with low efficacy. In this direction a variety of evolutionary scenarios are possible (Gandon et al., 2001; Gandon and Day, 2007), including the selection of more virulent Brucella strains.
Effective vaccination limits Brucella infection, restricts shedding, hampers transmission from animal to animal and diminishes the risk of zoonosis (Nicoletti, 1990). In addition, when combined with removal of positive infected animals, efficient vaccination may select for breeds with higher resistance against the disease (Adams and Schutta, 2010). Immunization with efficient vaccines may replace natural infections by inducing competent immunity (Plommet et al., 1987); likewise, culling of the infected animals replaces the natural selection of hosts displaying reproduction impartments, such abortion, placenta retention, and infertility (Fogel and Fogel, 2011). Eventually, these sustained combined strategies establish a R0 < 1 with the concomitant peter out of the disease. Moreover, when R0 < 1 the pathogen evolution rate towards higher virulence may be overcome and virulent field Brucella strains eradicated from domestic flocks (Davidson, 1970; Whittem, 1978; Wise, 1980; Moreno and Moriyón, 2006; Office International des Épizooties, 2013).
In contrast, inefficient vaccines currently used in many countries for the control of bovine, sheep, or caprine brucellosis might work in the opposite direction. Indeed, the protection afforded to non-immune animals by the presence of sufficient numbers of immune individuals, known as “herd immunity” (Figure 6) is threatened if the immune status of the herd is low. That is, inefficient vaccines may promote a fertile niche in weakly immune hosts allowing virulent Brucella to be transmitted though vaccinated animals (Herrera-López et al., 2010, 2011; Arellano-Reynoso et al., 2013). In curse this will increase the number of secondary infections. For example, if the anti-Brucella vaccine fails to generate immunity in a fraction p of those animals vaccinated, then to achieve herd immunity we need to vaccinate a proportion of individuals equivalent to R0 - 1/R0(1 - p) (Figure 7). Hence, if p is too big it may be impossible to eradicate brucellosis as it has been the case in many countries where vaccines of low-efficacy have extensively been used (Blasco et al., 1993; Moreno, 2002; Vargas, 2002; Blasco and Moriyón, 2005; Arellano-Reynoso et al., 2013; Chand and Chhabra, 2013; Denisov et al., 2013; Hou et al., 2013; Jiang et al., 2013; Li et al., 2013; Oseguera-Montiel et al., 2013; Rubach et al., 2013).
FIGURE 7.
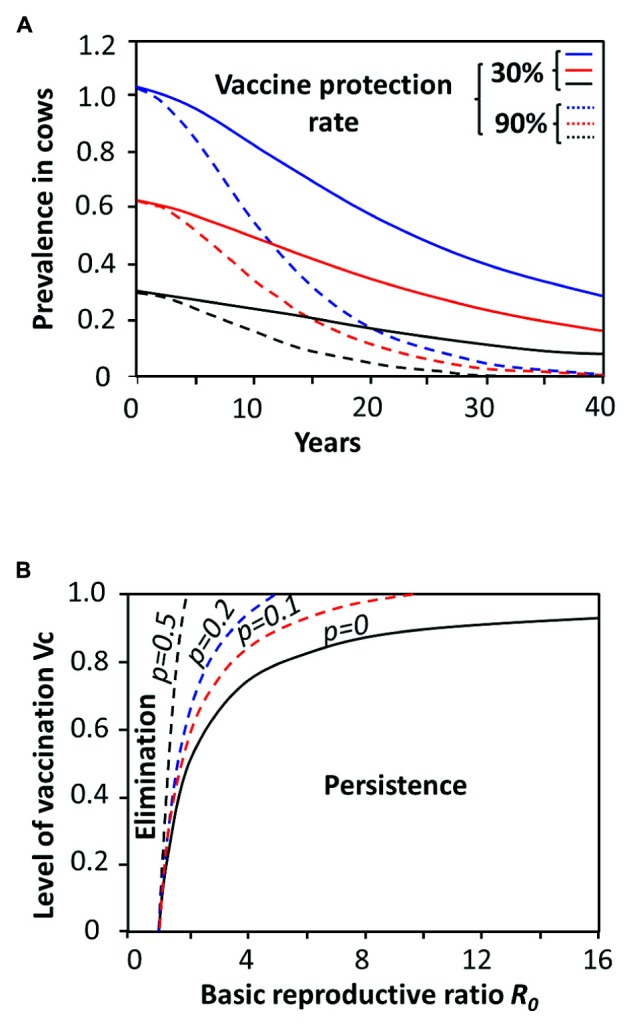
Sceneries for vaccine performances against brucellosis according to various models. (A) Predicted model for bovine brucellosis eradication in Mato Grosso (blue), Rodôni (red), and Goiás (black) Brazilian States with different experimental prevalences using two vaccine protection rates. Protection rate by low-efficacy vaccines or low coverage vaccination are not capable to eradicate brucellosis in four decades (solid lines), independently of the initial prevalence. The critical threshold applies to both: (i) the proportion of the population that needs to be vaccinated, and; (ii) the protective quality of the vaccine (adapted from Amaku et al., 2009). (B) Prediction for the elimination or persistence or of brucellosis according to R0 and the critical level of vaccination Vc. The Vc needed to protect a given population of animals is calculated by Vc = 1 - 1/R0. Those vaccines that fail to generate immunity in a fraction p of the immunized individuals, require higher coverage defined by R0 - 1/R0(1 - p). However, if p is too big it may be impossible to eradicate the Brucella infection. Parameters such as culling of the infected animals and diminishing of the density of the susceptible animals have a significant impact in both (A) and (B) since by reducing the value of p (not shown). The solid black line represents the outcome of an ideal no “leaking” vaccine (adapted from Keeling et al., 2013).
In cases in which the relative fitness of competing pathogens depends on the immune status of their host, low-efficacy vaccines inducing responses below the protective threshold may also prompt pathogen evolution towards higher virulence (Figure 8; Read and Mackinnon, 2008). Selection pressures may work in the same direction observed for non-sterilizing antibiotic treatments, in which the surviving microbes may display a higher resistance edge (Davies and Davies, 2010). Furthermore, anti-Brucella vaccines lacking some fundamental virulent molecular determinants or displaying a large collection of mutations (Wang et al., 2012), give a competitive advantage to virulent strains possessing full set of these factors, as it has been already shown for rough Brucella strains devoid of O-polysaccharide antigen (González et al., 2008; Barrio et al., 2009; Herrera-López et al., 2010).
FIGURE 8.
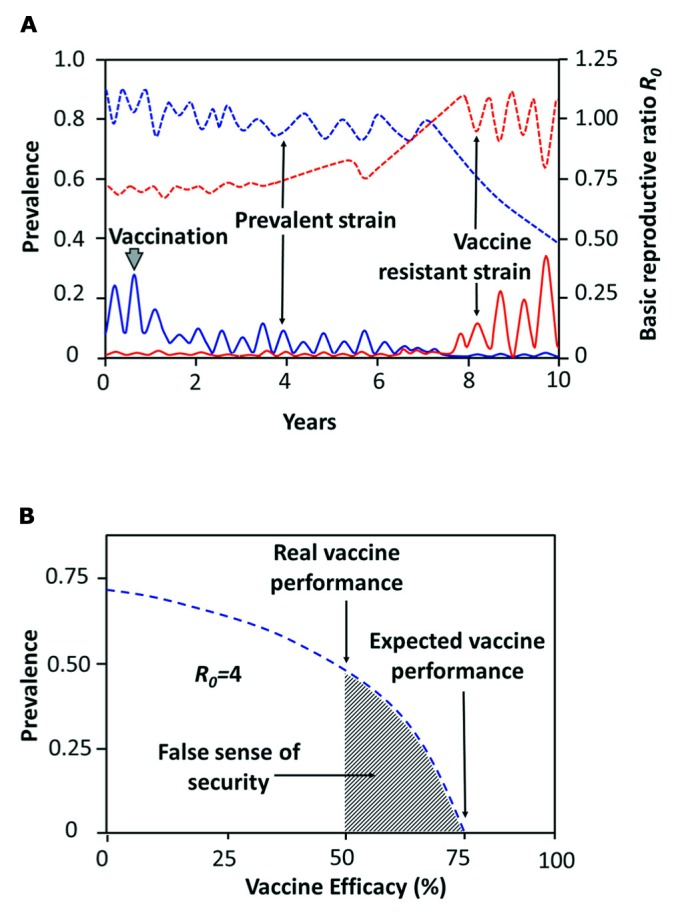
Prediction for emergence of resistant-vaccine Brucella strains and the false sense of security. (A) Immunization with low efficacy vaccines may change the competitive balance between Brucella virulent strains. Before vaccination (6–8 months of age) one prevalent strain is observed (blue line). After vaccination of 100% of the susceptible animals with a low efficacy vaccine that only gives 30–40% protection rate, the vaccine-resistant strain (red line) may eventually emerge with a competitive advantage that is only evident after a large proportion of the population has been vaccinated over the years. The vaccine resistant-strain arises from the Brucella pool, either through mutation of the prevalent strain or by selection of previously existing strains. Only after the R0 of the vaccine-resistant strain has exceeded that of the prevalent strain, then a new brucellosis epidemic event develops. Solid blue and red lines correspond to the prevalence ordinate; dashed lines correspond to the R0 ordinate (adapted from Scherer and McLean, 2002). (B) Reduction in brucellosis prevalence below the critical vaccination threshold (expected vaccine performance) with an anti-Brucella vaccine efficacy of 75% and R0 = 4. In a bovine close homogeneous population a lower value for R0 would be associated with a lower Brucella prevalence. The false sense of security (shadow area) for a given vaccine lays between the expected vaccine performance (e.g., 75%) and the real vaccine performance (e.g., 50%).
ANTI-Brucella VACCINES AND A FALSE SENSE OF SECURITY
In certain contexts vaccination induces a “sense of security” in non-specialized general public. This sense of security is sustained in the trust and faith that people have developed on vaccines that successfully prevented and eradicated diseases. If the vaccine is highly efficient, then the faith and trust is justified and not harm is done. However, this complacency is particularly dangerous when vaccines with low efficacy and short-term protective duration are introduced; then, a “false sense of security” may be generated, mainly when the information is not given properly (Henderson et al., 2011). Generally speaking, the false sense of security lays between the optimal expected efficacy for a given vaccine and the real performance of that vaccine (Figure 8) and it has a direct impact in the assessment of herd immunity. The use of anti-Brucella vaccines displaying low efficacy could generate a false sense of security in the minds of livestock farmers and Veterinary Health authorities, who may believe that herds are fully protected.
Under low threshold immunity conditions the host becomes a favorable environment for the replication and spread of field bacterial strains (Moreno, 2002; Herrera-López et al., 2010, 2011; Arellano-Reynoso et al., 2013; Denisov et al., 2013; Jiang et al., 2013) and a potential niche for Brucella selection. This is particularly relevant when prevalence is high and surveillance is low to begin with and when the favored virulent microbe emerges within a restricted population. These arguments are supported by several mathematical and epidemiological models (Gandon et al., 2001; Scherer and McLean, 2002; Day and Gandon, 2007; Gandon and Day, 2007).
ANTIBIOTICS AND Brucella
In the light of unrestricted use of antibiotics the emergence of antibiotic resistant Brucella clones should not be excluded a priori. However, in contrast to other bacterial pathogens, antibiotics do not seem to play a significant selective role in brucellosis. Due to economical, epidemiological, and public health reasons, treatment with antibiotics has been precluded in productive animals with brucellosis (Guerra and Nicoletti, 1986; Radwan et al., 1993; Office International des Épizooties, 2013). One exception is canine brucellosis. Pets with brucellosis are frequently treated with antibiotics, not always with success (Ledbetter et al., 2009). Antibiotics have also been used in brucellosis research for selecting specific strains displaying antibiotic resistance (Schurig et al., 1991; Adone et al., 2005; Ravanel et al., 2009), This has also important implications in the accidental transmission of Brucella organisms in the laboratory and the potential role of this bacterium as biological weapon (Yagupsky and Baron, 2005). In spite of this, most Brucella clinical isolates remain susceptible to the classical antibiotics used for treatment of brucellosis (Guerra and Nicoletti, 1986; Ayaşlıoğlu et al., 2008; Maves et al., 2011; Abdel-Maksoud et al., 2012). In broad terms, people constitute a dead end for Brucella transmission (Spink, 1956; Ruiz-Castañeda, 1986); therefore, antibiotic treatment of infected humans is not epidemiologically relevant (Figure 1). This phenomenon may relate to the absence of plasmids and lysogenic phages in Brucella organisms, as it has been explained elsewhere (Moreno, 1998). In this sense, the short-term emergence of antibiotic resistant Brucella does seem plausible.
CONCLUDING REMARKS
The capabilities of Brucella to infect and propagate in the preferred hosts follow at least five stages: (i) ability to invade; (ii) power to circumvent the initial defenses; (iii) competence to replicate; (iv) capacity to be transmitted; and (v) endurance to be maintained within the host population (Moreno and Moriyón, 2006; Martirosyan et al., 2011). How, when, and where pathogens cross the boundaries that separate their natural hosts from human populations and provoke an epidemic disease, is not entirely known. Human-to-human Brucella transmission would require that the pathogen’s R0 exceeds 1 (Gandon et al., 2001). Although Brucella animal pathogens have already achieved the first three stages in humans and in occasions the fourth stage (Meltzer et al., 2010), still the disease in humans is terminal and human mediated transmission is not of epidemiological importance (Figure 1). Thus, Brucella has not yet reached the R0 threshold to emerge as permanent pathogen within human populations and contagion remains dependent on animal reservoirs. However, under these circumstances human brucellosis may display a R0 above the threshold that depends on the zoonotic infection rate. For instance, as consequence of high prevalence in domestic animal reservoirs (sheep) in Inner Mongolia, the R0 for human infection corresponds to 1.8 (Hou et al., 2013). Under the prevailing control measures and use of low protective vaccines (Blasco et al., 1993; Verger et al., 1995) it was predicted that human brucellosis will continue to increase for the next decade in China.
Ecological factors and human activities may influence and induce changes in the microbial virulence patterns. But to distinguish Brucella clones displaying higher virulence is not an easy task (Moreno and Moriyón, 2002). Brucella organisms lack classical molecular markers commonly used to trace virulence such as toxins, fimbria, plasmids, capsules, antigenic variation or resistant forms. The so called “virulent factors” are intertwined with the overall Brucella structure and physiology (Moreno and Moriyón, 2002; Barbier et al., 2011) and are found in practically all Brucella species examined, independently of their pathogenicity for humans (Audic et al., 2009, 2011). Moreover, many of the molecular determinants such as cell envelope components, secretion systems, regulatory systems, transporters, and effectors assigned as virulent factors are also found in soil bacteria related to brucellae (Barquero-Calvo et al., 2009). As stated before, Brucella species form a compact genetic cluster and display host preference commensurate with their phylogenetic dispersion (Maquart et al., 2009; Audic et al., 2011; Foster et al., 2012). Therefore, the major scientific challenges that brucellosis research confronts relate to the identification of those discrete genotypic and phenotypic changes that have favored the adaptation to the preferred hosts and those molecular determinants that have made some Brucella species more virulent than others. In addition, efficient vaccines for dogs, pigs, water buffalo, and camels, as well as for some wild life animals, are required (Godfroid et al., 2011).
During the first half of the twentieth century through the early 1980s, efficient live Brucella S19 and Rev 1 vaccines for preventing brucellosis were developed together with robust procedures for testing their safety and efficacy (Cotton et al., 1933; Elberg and Meyer, 1958; Crawford and Hidalgo, 1977; Alton et al., 1988; Moreno and Moriyón, 2006). In addition, various inexpensive and straightforward serological tests as well as good management strategies were successfully implemented (Crawford and Hidalgo, 1977; Alton et al., 1988). Those were the days when brucellosis control programs succeeded in many parts of the world (Crawford and Hidalgo, 1977; Plommet, 1992). Circumstances have changed and the global agenda has been modified towards other interests. Taking into account that ignorance persists and economic profits pursue without other considerations, it is difficult to envision what will happen and how biological and cultural evolution will shape brucellosis and human battlement against this zoonotic disease.
For much of the twentieth century the misuse of antibiotics has taken place with little concern on the evolutionary consequences and selection of antibiotic resistance hypervirulent bacterial strains (Davies and Davies, 2010). It is our contention that we should not repeat that complacency with misuse of poor brucellosis vaccines, dubious immunization protocols, expensive diagnostic tests, and inadequate management procedures.
AUTHOR CONTRIBUTIONS
Edgardo Moreno wrote and revised the manuscript and made the figures.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The author thanks all personal from PIET-UNA and CIET-UCR for their valuable discussions. This work was partially funded by FIDA-2014 UNA, FS-CONARE UNA/UCR.
REFERENCES
- Abdel-Maksoud M., House B., Wasfy M., Abdel-Rahman B., Pimentel G., Roushdy G., et al. (2012). In vitro antibiotic susceptibility testing of Brucella isolates from Egypt between 1999 and 2007 and evidence of probable rifampin resistance. Ann. Clin. Microbiol. Antimicrob. 11 24 10.1186/1476-0711-11-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams G., Schutta C. J. (2010). Natural resistance against brucellosis: a review. Open Vet. Sci. J. 4 61–71 [Google Scholar]
- Adone R., Ciuchini F., Marianelli C., Tarantino M., Pistoia C., Marcon G., et al. (2005). Protective properties of rifampin-resistant rough mutants of Brucella melitensis. Infect. Immun. 73 4198–4204 10.1128/IAI.73.7.4198-4204.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmetagic S., Tihic N., Ahmetagic A., Custovic A., Smriko-Nuhanovic A., Mehinovic N., et al. (2012). Human brucellosis in Tuzla Canton. Med. Arh. 66 309–314 10.5455/medarh.2012.66.309-314 [DOI] [PubMed] [Google Scholar]
- Al Dahouk S., Hofer E., Tomaso H., Vergnaud G., Le Flèche P., Cloeckaert A., et al. (2012). Intraspecies biodiversity of the genetically homologous species Brucella microti. Appl. Environ. Microbiol. 78 1534–1543 10.1128/AEM.06351-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alton G. G., Jones L. M., Angus R. D., Verger J. M. (1988). Techniques for the Brucellosis Laboratory. Paris: Institut National de la Recherche Agronomique (INRA) [Google Scholar]
- Alzate H., González H., Guzmán J. (1969). Lactose intolerance in South American Indians. Am. J. Clin. Nutr. 22 122–123 [DOI] [PubMed] [Google Scholar]
- Amaku M., Dias R. A., Ferreira-Neto J. S., Ferreira F. (2009). Mathematical modeling of bovine brucellosis control by vaccination. Arq. Bras. Med. Vet. Zootec. 61 135–141 10.1590/S0102-09352009000700017 [DOI] [Google Scholar]
- Ardalan A., Oskarsson M., Natanaelsson C., Wilton A. N., Ahmadian A., Savolainen P. (2012). Narrow genetic basis for the Australian dingo confirmed through analysis of paternal ancestry. Genetica 140 65–73 10.1007/s10709-012-9658-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arellano-Reynoso B., Suárez-Güemes F., Estrada F. M., Michel-Gómez-Flores F., Hernández-Castro R., Acosta R. B., et al. (2013). Isolation of a field strain of Brucella abortus from RB51-vaccinated- and brucellosis-seronegative bovine yearlinggs that calved normally. Trop. Anim. Health Prod. 45 695–697 10.1007/s11250-012-0252-8 [DOI] [PubMed] [Google Scholar]
- Asaei S., Rasouli M., Moravej A. (2013). Interleukin-8 but not interleukin-6 variant may affect susceptibility to brucellosis. Iran J. Immunol. 10 158–166 [PubMed] [Google Scholar]
- Audic S., Lescot M., Claverie J. M., Cloeckaert A., Zygmunt M. S. (2011). The genome sequence of Brucella pinnipedialis B2/94 sheds light on the evolutionary history of the genus Brucella. BMC Evol. Biol. 11:200. 10.1186/1471-2148-11-200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audic S., Lescot M., Claverie J.-M., Scholz H. C. (2009). Brucella microti: the genome sequence of an emerging pathogen. BMC Genomics 10:352. 10.1186/1471-2164-10-352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayaşlıoğlu E., Kılıç S., Aydın K., Kılıç D., Kaygusuz S., Ağalar C. (2008). Antimicrobial susceptibility of Brucella melitensis isolates from blood samples. Turk. J. Med. Sci. 38 257–262 [Google Scholar]
- Aznar M. N., Samartino L. E., Humblet M. F., Saegerman C. (2012). Bovine brucellosis in Argentina and bordering countries: update. Transbound. Emerg. Dis. 61 121–133 10.1111/tbed12018 [DOI] [PubMed] [Google Scholar]
- Bang B. (1897). The etiology of epizootic abortion. J. Comp. Pathol. Ther. 10 125–149 10.1016/S0368-1742(97)80014-8 [DOI] [Google Scholar]
- Barbier T., Nicolas C., Letesson J. J. (2011). Brucella adaptation and survival at the crossroad of metabolism and virulence. FEBS. Lett. 585 2929–2934 10.1016/j.febslet.2011.08.011 [DOI] [PubMed] [Google Scholar]
- Barquero-Calvo E., Conde-Alvarez R., Chacón-Díaz C., Quesada-Lobo L., Martirosyan A., Guzmán-Verri C., et al. (2009). The differential interaction of Brucella and Ochrobactrum with innate immunity reveals traits related to the evolution of stealthy pathogens. PLoS ONE 4:e5893. 10.1371/journal.pone.0005893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrio M. B., Grilló M. J., Muñoz P. M., Jacques I., González D., de Miguel M. J., et al. (2009). Rough mutants defective in core and O-polysaccharide synthesis and export induce antibodies reacting in an indirect ELISA with smooth lipopolysaccharide and are less effective than Rev 1 vaccine against Brucella melitensis infection of sheep. Vaccine 27 1741–1749 10.1016/j.vaccine.2009.01.025 [DOI] [PubMed] [Google Scholar]
- Bevan L. E. W. (1931). Notes on a case of Rhodesian undulant fever. Trans. R. Soc. Trop. Med. Hyg. 24 93–95 10.1016/S0035-9203(30)90746-8 [DOI] [Google Scholar]
- Biebach I., Keller L. F. (2009). A strong genetic footprint of the re-introduction history of Alpine ibex (Capra ibex ibex). Mol. Ecol. 18 5046–5058 10.1111/j.1365-294X.2009.04420.x [DOI] [PubMed] [Google Scholar]
- Bingham J., Taylor T. K., Swingler J. E., Meehan G., Middleton D. J., Mackereth G. F., et al. (2008). Infection trials in pigs with a human isolate of Brucella (isolate 02/611 ‘marine mammal type’). N. Z. Vet. J. 56 10–14 10.1080/00480169.2008.36798 [DOI] [PubMed] [Google Scholar]
- Blasco J. M. (1990). “Brucella ovis,” in Animal Brucellosis eds Nielsen K., Duncan J. R. (Boca Raton, FL: CRC Press; ) 351–382 [Google Scholar]
- Blasco J. M., Marín C., Jiménez-de Bagüés M. P., Barberán M. (1993). Efficacy of Brucella suis strain 2 vaccine against Brucella ovis in rams. Vaccine 11 1291–1294 10.1016/0264-410X(93)90097-H [DOI] [PubMed] [Google Scholar]
- Blasco J. M., Moriyón I. (2005). Protection of Brucella abortus RB51 revaccinated cows. Comp. Immunol. Microbiol. Infect. Dis. 28 371–373 10.1016/j.cimid.2005.05.002 [DOI] [PubMed] [Google Scholar]
- Bonfiglio S., Ginja C., De Gaetano A., Achilli A., Olivieri A., Colli L., et al. (2012). Origin and spread of Bos taurus: new clues from mitochondrial genomes belonging to haplogroup T1. PLoS ONE 7:e38601. 10.1371/journal.pone.0038601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borriello G., Capparelli R., Bianco M., Fenizia D., Alfano F., Capuano F., et al. (2006). Genetic resistance to Brucella abortus in the water buffalo (Bubalus bubalis). Infect. Immun. 74 2115–2120 10.1128/IAI.74.4.2115-2120.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosilkovski M., Krteva L., Dimzova M., Vidinic I., Sopova Z., Spasovska K. (2010). Human brucellosis in Macedonia – 10 years of clinical experience in endemic region. Croat. Med. J. 51 327–336 10.3325/cmj.2010.51.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosseray N., Plommet M, De Rycke J. (1982). Evolution de l’infection de la sourispar Brucella abortus, Brucella melitensis et Brucella suis vers l’étatchronique et la guérison. Ann. Rech. Vet. 13 153–161 [PubMed] [Google Scholar]
- Bowling G. A. (1942). The introduction of cattle into colonial North America. J. Dairy Sci. 25 129–154 10.3168/jds.S0022-0302(42)95275-5 [DOI] [Google Scholar]
- Buddle M. B. (1956). Studies on Brucella ovis (nsp.), a cause of genital disease of sheep in New Zealand and Australia. J. Hyg. (Lond.) 54 351–364. 10.1017/S0022172400044612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos P., Willerslev E., Sher A., Orlando L., Axelsson E., Tikhonov A., et al. (2010). Ancient DNA analyses exclude humans as the driving force behind late Pleistocene musk ox (Ovibos moschatus) population dynamics. Proc. Natl. Acad. Sci. U.S.A. 107 5675–5680 10.1073/pnas.0907189107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capasso L. (2002). Bacteria in two-millennia-old cheese, and related epizoonoses in Roman populations. J. Infect. 45 122–127 10.1053/jinf.2002.0996 [DOI] [PubMed] [Google Scholar]
- Carmichael L. E., Bruner D. W. (1968). Characteristics of a newly-recognized species of Brucella responsible for infectious canine abortions. Cornell Vet. 48 579–592 [PubMed] [Google Scholar]
- Caron E., Liautard J. P., Köhler S. (1994). Differentiated U937 cells exhibit increased bactericidal activity upon LPS activation and discriminate between virulent and avirulent Listeria and Brucella species. J. Leukoc. Biol. 56 174–181 [DOI] [PubMed] [Google Scholar]
- Chamberlin W. E. (1985). Early history of bovine brucellosis eradication in Australia. Aust. Vet. J. 62 289–292 10.1111/j.1751-0813.1985.tb14907.x [DOI] [PubMed] [Google Scholar]
- Chand P., Chhabra R. (2013). Herd and individual animal prevalence of bovine brucellosis with associated risk factors on dairy farms in Haryana and Punjab in India. Trop. Anim. Health Prod. 45 1313–1319 10.1007/s11250-013-0362-y [DOI] [PubMed] [Google Scholar]
- Cotton W. E., Buck J. M., Smith H. E. (1933). Efficacy and safety of abortion vaccines prepared from Brucella abortus strains of different degrees of virulence. J. Agric. Res. 46 291–314 [Google Scholar]
- Craig C. F. (1903). Malta fever: its occurrence in the United States Army, with a review of the literature. Am. J. Med. Sci. 125 105–115 10.1097/00000441-190301000-00009 [DOI] [Google Scholar]
- Crawford R. P., Hidalgo R. M. (1977). Bovine Brucellosis. Galveston, TX: Texas A&M University Press [Google Scholar]
- Crawford R. P., Huber J. D., Adams B. S. (1990). “Epidemiology and surveillance,” in Animal Brucellosis eds Nielsen K., Duncan J. R. (Boca Raton, FL: CRC Press; ) 131–151 [Google Scholar]
- Dalrymple-Champneys W. (1960). Clinical Features, Brucella Infection and Undulant Fever in Man. London: Oxford University Press [Google Scholar]
- D’Anastasio R., Staniscia T., Milia M. L., Manzoli L., Capasso L. (2011). Origin, evolution and paleoepidemiology of brucellosis. Epidemiol. Infect. 139 149–156 10.1017/S095026881000097X [DOI] [PubMed] [Google Scholar]
- D’Anastasio R., Zipfel B., Moggi-Cecchi J., Stanyon R., Capasso L. (2009). Possible brucellosis in an early hominin skeleton from Sterkfontein, South Africa. PLoS ONE 4:e6439. 10.1371/journal.pone.0006439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson R. M. (1970). Control of bovine brucelosis in New Zealand. Bull. Off. Int. Epizoot. 73 29–32 [PubMed] [Google Scholar]
- Davies J., Davies D. (2010). Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. 74 417–433 10.1128/MMBR.00016-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies L. E. C., Hanson S. (1965). The Eskimos of the Northwest Passage: a survey of dietary composition and various blood and metabolic measurements. Can. Med. Assoc. J. 92 205–206 [PMC free article] [PubMed] [Google Scholar]
- Davis D. S., Heck F. C., Williams J. D., Simpson T. R., Adams L. G. (1988). Interspecific transmission of Brucella abortus from experimentally infected coyotes (Canis latrans) to parturient cattle. J. Wildl. Dis. 24 533–537 10.7589/0090-3558-24.3.533 [DOI] [PubMed] [Google Scholar]
- Dawson C. E., Perrett L. L., Stubberfield E. J., Stack J. A., Farrelly S. S., Cooley W. A., et al. (2008). Isolation and characterization of Brucella from the lungworms of a harbor porpoise (Phocoena phocoena). J. Wildl. Dis. 44 237–246 10.7589/0090-3558-44.2.237 [DOI] [PubMed] [Google Scholar]
- Day T., Gandon S. (2007). Applying population-genetic models in theoretical evolutionary epidemiology. Ecol. Lett. 10 876–888 10.1111/j.1461-0248.2007.01091.x [DOI] [PubMed] [Google Scholar]
- De B. K., Stauffer L., Koylass M. S., Sharp S. E., Gee J. E., Helsel L. O., et al. (2008). Novel Brucella strain (BO1) associated with a prosthetic breast implant infection. J. Clin. Microbiol. 46 43–49 10.1128/JCM.01494-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de las Casas B. (1951). Historia de las Indias. Buenos Aires: Fondo de Cultura Económica [Google Scholar]
- Denisov A. A., Sclyarov O. D., Salmakov K. M., Shumilov K. V. (2013). The Russian experience in brucellosis veterinary public health. Rev. Sci. Tech. 32 229–237 [DOI] [PubMed] [Google Scholar]
- Di D., Cui B., Wang H., Zhao H., Piao D., Tian L., et al. (2014). Genetic polymorphism characteristics of Brucella canis isolated in China. PLoS ONE 9:e84862. 10.1371/journal.pone.0084862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz R., Casanova A., Ariza J., Moriyón I. (2011). The Rose Bengal test in human brucellosis: a neglected test for the diagnosis of a neglected disease. PLoS Negl. Trop. Dis. 5:e950. 10.1371/journal.pntd.0000950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eales K. M., Norton R. E., Ketheesan N. (2010). Brucellosis in northern Australia. Am. J. Trop. Med. Hyg. 83 876–878 10.4269/ajtmh.2010.10-0237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebel E. D., Williams M. S., Tomlinson S. M. (2008). Estimating herd prevalence of bovine brucellosis in 46 USA states using slaughter surveillance. Prev. Vet. Med. 85 295–316 10.1016/j.prevetmed.2008.02.005 [DOI] [PubMed] [Google Scholar]
- Elberg S. S., Meyer K. F. (1958). Caprine immunization against brucellosis. A summary of experiments on the isolation, properties and behavior of a vaccine strain. Bull. World Health Organ. 19 711–724 [PMC free article] [PubMed] [Google Scholar]
- Ellestad-Sayed J. J., Haworth J. C., Hildes J. A. (1978). Disaccharide malabsorption and dietary patterns in two Canadian Eskimo communities. Am. J. Clin. Nutr. 31 1473–1478 [DOI] [PubMed] [Google Scholar]
- Enattah N. S., Jensen T. G., Nielsen M., Lewinski R., Kuokkanen M., Rasinpera H., et al. (2008). Independent introduction of two lactase-persistence alleles into human populations reflects different history of adaptation to milk culture. Am. J. Hum. Genet. 82 57–72 10.1016/j.ajhg.2007.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etxeberria F. (1994). Vertebral epiphysitis: early signs of brucellar disease. J. Paleopathol. 6 41–49 [Google Scholar]
- Evans A. C. (1918). Further studies on bacterium abortus and related bacteria: a comparison of bacterium abortus with bacterium bronchisepticus and with the organism that causes Malta fever. J. Infect. Dis. 22 580–593 10.1093/infdis/22.6.580 [DOI] [Google Scholar]
- Evershed R. P., Payne S., Sherratt A. G., Copley M. S., Coolidge J., Urem-Kotsu D., et al. (2008). Earliest date for milk use in the Near East and southeastern Europe linked to cattle herding. Nature 455 528–531 10.1038/nature07180 [DOI] [PubMed] [Google Scholar]
- Ewald P. W. (2004). Evolution of virulence. Infect. Dis. Clin. North Am. 18 1–15 10.1016/S0891-5520(03)00099-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferroglio E., Tolari F., Bollo E., Bassano B. (1998). Isolation of Brucella melitensis from alpine ibex. J. Wildl. Dis. 34 400–402 10.7589/0090-3558-34.2.400 [DOI] [PubMed] [Google Scholar]
- Fogel G. B., Fogel D. B. (2011). Simulating natural selection as a culling mechanism on finite populations with the hawk-dove game. Biosystems 104 57–62 10.1016/j.biosystems.2011.01.002 [DOI] [PubMed] [Google Scholar]
- Forbes L. B. (1991). Isolates of Brucella suis biovar 4 from animals and humans in Canada, 1982–1990. Can. Vet. J. 32 686–688 [PMC free article] [PubMed] [Google Scholar]
- Foster J. T., Price L. B., Beckstrom-Sternberg S. M., Pearson T., Brown W. D., Kiesling D. M., et al. (2012). Genotyping of Brucella species using clade specific SNPs. BMC Microbiol. 12:110. 10.1186/1471-2180-12-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallego Romero I., Basu Mallick C., Liebert A., Crivellaro F., Chaubey G., Itan Y., et al. (2012). Herders of Indian and European cattle share their predominant allele for lactase persistence. Mol. Biol. Evol. 29 249–260 10.1093/molbev/msr190 [DOI] [PubMed] [Google Scholar]
- Gandon S., Day T. (2007). The evolutionary epidemiology of vaccination. J. R. Soc. Interface 4 803–817 10.1098/rsif.2006.0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandon S., Mackinnon M. J., Nee S., Read A. F. (2001). Imperfect vaccines and the evolution of pathogen virulence. Nature 414 751–756 10.1038/414751a [DOI] [PubMed] [Google Scholar]
- Gardner E., Reichel M. P. (1997). No evidence of Brucella canis infections in New Zealand dogs. Surveillance 24 17–18 [Google Scholar]
- Garofolo G., Di Giannatale E., De Massis F., Zilli K., Ancora M., Cammà C., et al. (2013). Investigating genetic diversity of Brucella abortus and Brucella melitensis in Italy with MLVA-16. Infect. Genet. Evol. 19 59–70 10.1016/j.meegid.2013.06.021 [DOI] [PubMed] [Google Scholar]
- Gentry E. R., Ferenbaugh T. L. (1911). Endemic Malta (Mediterranean) fever in Texas. JAMA 57 1045–1048 10.1001/jama.1911.04260090267008 [DOI] [Google Scholar]
- Gibby I. W., Gibby A. M. (1965). Host–parasite relationships with Brucella neotomae. J. Bacteriol. 89 9–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillen M., Flynn M., Browning Y. (1989). The Founders of Australia: A Biographical Dictionary of the First Fleet. Sydney: Library of Australian History [Google Scholar]
- Giuffra E., Kijas J. M., Amarger V., Carlborg O., Jeon J. T., Andersson L. (2000). The origin of the domestic pig: independent domestication and subsequent introgression. Genetics 154 1785–1791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfroid J., Scholz H. C., Barbier T., Nicolas C., Wattiau P., Fretin D., et al. (2011). Brucellosis at the animal/ecosystem/human interface at the beginning of the 21st century. Prev. Vet. Med. 102 118–131 10.1016/j.prevetmed.2011.04.007 [DOI] [PubMed] [Google Scholar]
- Gomo C., de Garine-Wichatitsky M., Caron A., Pfukenyi D. M. (2012). Survey of brucellosis at the wildlife-livestock interface on the Zimbabwean side of the Great Limpopo Transfrontier Conservation Area. Trop. Anim. Health Prod. 44 77–85 10.1007/s11250-011-9890-5 [DOI] [PubMed] [Google Scholar]
- González D., Grilló M. J., De Miguel M. J., Ali T., Arce-Gorvel V., Delrue R. M., et al. (2008). Brucellosis vaccines: assessment of Brucella melitensis lipopolysaccharide rough mutants defective in core and O-polysaccharide synthesis and export. PLoS ONE 3:e2760. 10.1371/journal.pone.0002760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilló M. J., Blasco J. M., Gorvel J. P., Moriyón I., Moreno E. (2012). What have we learned from brucellosis in the mouse model? Vet. Res. 43 29 10.1186/1297-9716-43-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross J. E., Wang G. (2005). Effects of Population Control Strategies on Retention of Genetic Diversity in National Park Service Bison (Bison bison) Herds. Final Report Submitted to Yellowstone Research Group USGS-BRD. Bozeman, MT: Department of Biology, Montana State University [Google Scholar]
- Gudoshnik A. N. (1958). Role of pasture ticks and rodents in dissemination of Brucella. Zh. Mikrobiol. Epidemiol. Immunobiol. 29 113–117 [PubMed] [Google Scholar]
- Guerra M. A., Nicoletti P. (1986). Comparison of the susceptibility of Brucella abortus isolates obtained before and after cows were treated with oxytetracycline and streptomycin. Am. J. Vet. Res. 47 2612–2613 [PubMed] [Google Scholar]
- Guzmán-Verri C., González-Barrientos R., Hernández-Mora G., Morales J. A., Baquero-Calvo E., Chaves-Olarte E., et al. (2012). Brucella ceti and brucellosis in cetaceans. Front. Cell. Infect. Microbiol. 2:3. 10.3389/fcimb.2012.00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyuranecz M., Szeredi L., Rónai Z., Dénes B., Dencso L., Dán Á., et al. (2011). Detection of Brucella canis-induced reproductive diseases in a kennel. J. Vet. Diagn. Invest. 23 143–147 10.1177/104063871102300127 [DOI] [PubMed] [Google Scholar]
- Hars J., Rautureau S., Jaÿ M., Game Y., Gauthier D., Herbaux J.-P., et al. (2013). Un foyer de brucellose chez les ongulés sauvages du massif du Bargy en Haute-Savoie. Bull. Epidemiol. Santé Anim. Alim. 60 2–6 [Google Scholar]
- Henderson L., Clements A., Damery S., Wilkinson C., Austoker J., Wilson S., et al. (2011). ‘A false sense of security’? Understanding the role of the HPV vaccine on future cervical screening behaviour: a qualitative study of UK parents and girls of vaccination age. J. Med. Screen. 18 41–45 10.1258/jms.2011.010148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J. A. (2013). Genetic Natural Resistance to Brucellosis in Yellowstone National Park Bison (Bison bison): A Preliminary Assessment. M.Sc. thesis, College of Veterinary Medicine and Biomedical Sciences, Colorado State University [Google Scholar]
- Herrera-López E., Rivera A., Palomares E. G., Hernández-Castro R., Díaz-Aparicio E. (2011). Isolation of Brucella melitensis from a RB51-vaccinated seronegative goat. Trop. Anim. Health Prod. 43 1069–1070 10.1007/s11250-011-9822-4 [DOI] [PubMed] [Google Scholar]
- Herrera-López E., Suárez-Güemes F., Hernández-Andrade L., Córdova-López D., Díaz-Aparicio E. (2010). Epidemiological study of brucellosis in cattle, immunized with Brucella abortus RB51 vaccine in endemic zones. Vaccine 28 (Suppl.) 5 F59–F63 10.1016/j.vaccine.2010.03.057 [DOI] [PubMed] [Google Scholar]
- Higgins J., Stuber T., Quance C., Edwards W. H., Tiller R. V., Linfield T., et al. (2012). Molecular epidemiology of Brucella abortus isolates from cattle, elk, and bison in the United States, 1998 to 2011. Appl. Environ. Microbiol. 78 3674–3684 10.1128/AEM.00045-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkins J. M. (2002). The tale that tail bones tell about the antiquity of the human disease brucellosis. Am. J. Phys. Anthropol. S36 115 [Google Scholar]
- Hofer E., Bag Z. N., Revilla-Fern Ndez S., Melzer F., Tomaso H., L Pez-Go I. I., et al. (2012). First detection of Brucella canis infections in a breeding kennel in Austria. New Microbiol. 35 507–150 [PubMed] [Google Scholar]
- Hollett R. B. (2006). Canine brucellosis: outbreaks and compliance. Theriogenology 66 575–587 10.1016/j.theriogenology.2006.04.011 [DOI] [PubMed] [Google Scholar]
- Hornaday W. T. (1889). The Extermination of the American Bison. From the Report of the National Museum 1886–1887 EBook #17748. Washington: Washington Government Printing Office, Project Gutenberg [Google Scholar]
- Hou Q., Sun X., Zhang J., Liu Y., Wang Y., Jin Z. (2013). Modeling the transmission dynamics of sheep brucellosis in Inner Mongolia Autonomous Region, China. Math. Biosci. 242 51–58 10.1016/j.mbs.2012.11.012 [DOI] [PubMed] [Google Scholar]
- Itan Y., Jones B. L., Ingram C. J., Swallow D. M., Thomas M. G. (2010). A worldwide correlation of lactase persistence phenotype and genotypes. BMC Evol. Biol. 10:36. 10.1186/1471-2148-10-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H., Wang H., Xu L., Hu G., Ma J., Xiao P., et al. (2013). MLVA genotyping of Brucella melitensis and Brucella abortus isolates from different animal species and humans and identification of Brucella suis vaccine strain S2 from cattle in China. PLoS ONE 8:e76332. 10.1371/journal.pone.0076332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez de Bagüés M. P., Ouahrani-Bettache S., Quintana J. F., Mitjana O., Hanna N., Bessoles S., et al. (2010). The new species Brucella microti replicates in macrophages and causes death in murine models of infection. J. Infect. Dis. 202 3–10 10.1086/653084 [DOI] [PubMed] [Google Scholar]
- Joshi M. B., Rout P. K., Mandal A. K., Tyler-Smith C., Singh L., Thangaraj K. (2004). Phylogeography and origin of Indian domestic goats. Mol. Biol. Evol. 21 454–462 10.1093/molbev/msh038 [DOI] [PubMed] [Google Scholar]
- Keeling M. J., Tildesley M., House T., Danon L. (2013). The mathematics of vaccination. Math. Today 49 40–43 [Google Scholar]
- Kousoulis A. A., Economopoulos K. P., Poulakou-Rebelakou E., Androutsos G., Tsiodras S. (2012). The plague of Thebes, a historical epidemic in Sophocles’ Oedipus Rex. Emerg. Infect. Dis. 18 153–157 10.3201/eid1801.AD1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S., Nagarajan M., Sandhu J. S., Kumar N., Behl V. (2007). Phylogeography and domestication of Indian river buffalo. BMC Evol. Biol. 7:186. 10.1186/1471-2148-7-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledbetter E. C., Landry M. P., Stokol T., Kern T. J., Messick J. B. (2009). Brucella canis endophthalmitis in 3 dogs: clinical features, diagnosis, and treatment. Vet. Ophthalmol. 12 183–191 10.1111/j.1463-5224.2009.00690.x [DOI] [PubMed] [Google Scholar]
- Le Flèche P., Jacques I., Grayon M., Al Dahouk S., Bouchon P., Denoeud F., et al. (2006). Evaluation and selection of tandem repeat loci for a Brucella MLVA typing assay. BMC Microbiol. 6:9. 10.1186/1471-2180-6-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard J. A., Wayne R. K., Wheeler J., Valadez R., Guillén S., Vilà C. (2002). Ancient DNA evidence for Old World origin of New World dogs. Science 298 1613–1616 10.1126/science.1076980 [DOI] [PubMed] [Google Scholar]
- Li Y. J., Li X. L., Liang S., Fang L. Q., Cao W. C. (2013). Epidemiological features and risk factors associated with the spatial and temporal distribution of human brucellosis in China. BMC Infect. Dis. 13:547. 10.1186/1471-2334-13-547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucero N. E., Ayala S. M., Escobar G. I., Jacob N. R. (2008). Brucella isolated in humans and animals in Latin America from 1968 to 2006. Epidemiol. Infect. 136 496–503 10.1017/S0950268807008795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundquist L. (2012). State Agencies and B Politicians Push for New brucellosis Listing: Bozeman Daily Chronicle. Available at: http://www.Bozemandailychronicle.com/news/wildlife (accessed April 29, 2014) [Google Scholar]
- Madsen M., Anderson E. C. (1995). Serologic survey of Zimbabwean wildlife for brucellosis. J. Zoo Wildl. Med. 26 240–245 [Google Scholar]
- Mailles A., Rautureau S., Le Horgne J. M., Poignet-Leroux B., d’Arnoux C., Dennetière G., et al. (2012). Re-emergence of brucellosis in cattle in France and risk for human health. Eurosurveillance 17 pii: 20227 [PubMed] [Google Scholar]
- Mancini F. R., Bella A., Graziani C., Marianelli C., Mughini-Gras L., Pasquali P., et al. (2013). Trends of human brucellosis in Italy, 1998–2010. Epidemiol. Infect. 18 1–8 10.1017/S0950268813002227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantur B. G., Amarnath S. K. (2008). Brucellosis in India – a review. J. Biosci. 33 539–547 10.1007/s12038-008-0072-1 [DOI] [PubMed] [Google Scholar]
- Maquart M., Le Flèche P., Foster G., Tryland M., Ramisse F., Djønne B., et al. (2009). MLVA-16 typing of 295 marine mammal Brucella isolates from different animal and geographic origins identifies 7 major groups within Brucella ceti and Brucella pinnipedialis. BMC Microbiol. 9:145. 10.1186/1471-2180-9-145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martirosyan A., Moreno E., Gorvel J. P. (2011). An evolutionary strategy for a stealthy intracellular Brucella pathogen. Immunol. Rev. 240 211–234 10.1111/j.1600-065X.2010.00982.x [DOI] [PubMed] [Google Scholar]
- Marzetti S., Carranza C., Roncallo M., Escobar G. I., Lucero N. E. (2013). Recent trends in human Brucella canis infection. Comp. Immunol. Microbiol. Infect. Dis. 36 55–61 10.1016/j.cimid.2012.09.002 [DOI] [PubMed] [Google Scholar]
- Maves R. C., Castillo R., Guillen A., Espinosa B., Meza R., Espinoza N., et al. (2011). Antimicrobial susceptibility of Brucella melitensis isolates in Peru. Antimicrob. Agents Chemother. 55 1279–1281 10.1128/AAC.00979-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDaniel C. J., Cardwell D. M., Moeller R. B., Jr., Gray G. C. (2013). Humans and cattle: a review of bovine zoonoses. Vector Borne Zoonotic Dis. 14 1–19 10.1089/vbz.2012.1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald W. L., Jamaludin R., Mackereth G., Hansen M., Humphrey S., Short P., et al. (2006). Characterization of a Brucella strain as a marine-mammal type despite isolation from a patient with spinal osteomyelitis in New Zealand. J. Clin. Microbiol. 44 4363–4370 10.1128/JCM.00680-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meagher M., Meyer M. E. (1994). On the origin of brucellosis in bison of Yellowstone National Park. Conserv. Biol. 8 645–653 10.1046/j.1523-1739.1994.08030645.x [DOI] [Google Scholar]
- Meltzer E., Sidi Y., Smolen G., Banai M., Bardenstein S., Schwartz E. (2010). Sexually transmitted brucellosis in humans. Clin. Infect. Dis. 51 12–15 10.1086/653608 [DOI] [PubMed] [Google Scholar]
- Meyer K. F., Shaw E. B. (1920). A comparison of the morphologic, cultural and biochemical characteristics of B. abortus and B. melitensis studies on the genus Brucella Nov. Gen. J. Infect. Dis. 27 173–184 10.1093/infdis/27.3.173 [DOI] [Google Scholar]
- Meyer M. E. (1966). Identification and virulence studies of Brucella strains isolated from Eskimos and reindeer in Alaska, Canada, and Russia. J. Vet. Res. 27 353–358 [PubMed] [Google Scholar]
- Meyer M. E. (1977). “Epidemiological odds and ends,” in Bovine Brucellosis eds Crawford R. P., Hidalgo R. J. (Galveston, TX: Texas A&M University Press; ) 35–142 [Google Scholar]
- Meyer M. E. (1990). “Evolutionary development and taxonomy of the genus Brucella,” in Advances in Brucellosis Research ed. Adams L. G. (Galveston, TX: Texas A&M University Press; ) 12–35 [Google Scholar]
- Mi J. C., Zhang Q. H., Wei R. P., Song L. T., Zheng Z. (2010). The epidemiological characteristics of human brucellosis in Inner Mongolia. Chin. J. Control Endem. Dis. 1 34–37 [Google Scholar]
- Mick V., Le Carrou G., Corde Y., Game Y., Jaÿ M., Garin-Bastuji B. (2014). Brucella melitensis in France: persistence in wildlife and probable spillover from Alpine ibex to domestic animals. PLoS ONE 9:e94168. 10.1371/journal.pone.0094168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minas M., Minas A., Gourgulianis K., Stournara A. (2007). Epidemiological and clinical aspects of human brucellosis in Central Greece. Jpn. J. Infect. Dis. 60 362–366 [PubMed] [Google Scholar]
- Mohler J. R. (1917). “Report of the Chief of the Bureau of Animal Industry, Pathological Division, Abortion Disease,” in Annual Reports of the Department of Agriculture(1917). Washington DC: United States Department of Agriculture [Google Scholar]
- Moreno E. (1992). “Brucella evolution,” in Prevention of brucellosis in Mediterranean Countries ed. Plommet M. (Wageningen: Pudoc Scientific Publishers; ) 198–218 [Google Scholar]
- Moreno E. (1998). Genome evolution within the alpha Proteobacteria: why do some bacteria not possess plasmids and others exhibit more than one different chromosome? FEMS Microbiol. Rev. 22 255–275 10.1111/j.1574-6976.1998.tb00370.x [DOI] [PubMed] [Google Scholar]
- Moreno E. (2002). Brucellosis in Central America. Vet. Microbiol. 90 31–38 10.1016/S0378-1135(02)00242-0 [DOI] [PubMed] [Google Scholar]
- Moreno E., Moriyón I. (2002). Brucella melitensis: a nasty bug with hidden credentials for virulence. Proc. Natl. Acad. Sci. U.S.A. 99 1–3 10.1073/pnas.022622699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno E., Moriyón I. (2006). “The genus Brucella,” in The Prokaryotes Vol. 5 Part 1, Section 31 eds Dworkin M., Falkow S., Rosenberg E., Schleifer K.-H., Stackebrant E. (New York: Springer-Verlag; ) 315–456 [Google Scholar]
- Moriyón I., Grilló M. J., Monreal D., González D., Marín C., López-Goñi I., et al. (2004). Rough vaccines in animal brucellosis: structural and genetic basis and present status. Vet. Res. 35 1–38 10.1051/vetres:2003037 [DOI] [PubMed] [Google Scholar]
- Mutolo M. J., Jenny L. L., Buszek A. R., Fenton T. W., Foran D. R. (2012). Osteological and molecular identification of brucellosis in ancient Butrint, Albania. Am. J. Phys. Anthropol. 147 254–263 10.1002/ajpa.21643 [DOI] [PubMed] [Google Scholar]
- Naderi S., Rezaei H. R., Pompanon F., Blum M. G., Negrini R., Naghash H. R., et al. (2008). The goat domestication process inferred from large-scale mitochondrial DNA analysis of wild and domestic individuals. Proc. Natl. Acad. Sci. U.S.A. 105 17659–17664 10.1073/pnas.0804782105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neglia G., Veneziano V., De-Carlo E., Galiero G., Borriello G., Francillo M., et al. (2013). Detection of Brucella abortus DNA and RNA in different stages of development of the sucking louse Haematopinus tuberculatus. BMC Vet. Res. 9:236. 10.1186/1746-6148-9-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neiland K. A. (1975). Rangiferine brucellosis in Alaskan canids. J. Wildl. Dis. 6 136–139 10.7589/0090-3558-6.3.136 [DOI] [PubMed] [Google Scholar]
- Nelson S. M. (1998). Ancestors for the Pigs. Pigs in Prehistory. Philadelphia, PA: University of Pennsylvania Museum of Archeology; University of Pennsylvania Press [Google Scholar]
- Nicoletti P. (1989). “Relationship between animal and human disease,” in Brucellosis Clinical and Laboratory Aspects eds Young E., Corbel M. J. (Boca Raton, FL: CRC Press; ) 42–51 [Google Scholar]
- Nicoletti P. (1990). Vaccinations against Brucella. Adv. Biotechnol. Processes 13 147–168 [PubMed] [Google Scholar]
- Office International des Épizooties. (eds). (2013). Manual of Diagnostic Tests and Vaccines for Terrestrial Animals 7th Edn Vol. 1 and 2 Chap. 2.4.3., 2.7.2., and 2.7.9. (Paris: OIE). Available at: http://www.oie.int/en/international-standard-setting/terrestrial-manual/access-online/ (accessed April 29, 2014) [Google Scholar]
- Ohishi K., Fujise Y., Maruyama T. (2008). Brucella spp. in the western North Pacific and Antarctic cetaceans: a review. J. Cetacean Res. Manag. 10 67–72 [Google Scholar]
- Ortner J. D. (2003). “Infectious diseases: introduction, biology, osteomyelitis, periostitis, brucellosis, glanders, and septic arthritis,” in Identification of Pathological Conditions in Human Skeletal Remains ed. Ortner J. E. (San Diego: Academic Press; ) 179–226 [Google Scholar]
- Oseguera-Montiel D., Frankena K., Udo H., Keilbach Baer N. M, van der Zijpp A. (2013). Prevalence and risk factors for brucellosis in goats in areas of Mexico with and without brucellosis control campaign. Trop. Anim. Health Prod. 45 1383–1389 10.1007/s11250-013-0375-6 [DOI] [PubMed] [Google Scholar]
- Ovodov N. D., Crockford S. J., Kuzmin Y. V., Higham T. F. G., Hodgins G. W. L, van der Plicht J. (2011). A 33,000-year-old incipient dog from the Altai Mountains of Siberia: evidence of the earliest domestication disrupted by the last glacial maximum. PLoS ONE 6:e22821. 10.1371/journal.pone.0022821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas G., Memish Z. A. (2007). Brucellosis in the middle East: a persistent medical, socioeconomic and political issue. J. Chemother. 19 243–248 10.1179/joc.2007.19.3.243 [DOI] [PubMed] [Google Scholar]
- Pariset L., Mariotti M., Gargani M., Joost S., Negrini R., Perez T., et al. (2011). Genetic diversity of sheep breeds from Albania, Greece, and Italy assessed by mitochondrial DNA and nuclear polymorphisms (SNPs). Sci. World J. 11 1641–1659 10.1100/2011/186342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pashaei S., Azari M. A., Hasani S., Khanahmadi A., Rostamzadeh J. (2009). Genetic diversity in mazandaranian native cattle: a comparison with Holstein cattle, using ISSR marker. Pak. J. Biol. Sci. 12 717–721 10.3923/pjbs.2009.717.721 [DOI] [PubMed] [Google Scholar]
- Pearce-Duvet J. M. (2006). The origin of human pathogens: evaluating the role of agriculture and domestic animals in the evolution of human disease. Biol. Rev. Camb. Philos. Soc. 81 369–382 10.1017/S1464793106007020 [DOI] [PubMed] [Google Scholar]
- Pedro-Pons A., Farreras P., Foz A., Surós J., Surinyach R., Frouchtman R. (1968). Enfermedades Infecciosas. II.A. Enfermedades Producidas por Bacterias. Brucelosis. Patología y Clínica Médicas Vol. VI. Madrid: Salvat Ediciones S.A [Google Scholar]
- Perrett L. L., Brew S. D., Stack J. A., MacMillan A. P., Bashiruddin J. B. (2004). Experimental assessment of the pathogenicity of Brucella strains from marine mammals for pregnant sheep. Small Rumin. Res. 51 221–228 10.1016/S0921-4488(03)00233-5 [DOI] [Google Scholar]
- Peters J. (1997). The dromedary: ancestry, history of domestication and medical treatment in early historic times. Tierarztl. Prax. Ausg. G Grosstiere Nutztiere 25 559–565 [PubMed] [Google Scholar]
- Plantinga T. S., Alonso S., Izagirre N., Hervella M., Fregel R., van der Meer J. W., et al. (2012). Low prevalence of lactase persistence in Neolithic South-West Europe. Eur. J. Hum. Genet. 20 778–782 10.1038/ejhg.2011.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plommet M. (1992). Prevention of Brucellosis in Mediterranean Countries. Wageningen: Pudoc Scientific Publishers [Google Scholar]
- Plommet M., Serre A., Fensterbank R. (1987). Vaccines, vaccination in brucellosis. Ann. Inst. Pasteur Microbiol. 138 117–121 10.1016/0769-2609(87)90089-5 [DOI] [PubMed] [Google Scholar]
- Pu D. R., Li L. Y., Zhao H. Y., Cui B. Y. (2009). Epidemic situation analysis of human brucellosis in Inner Mongolia during 1952 to 2007. Chin. J. Control Endem. Dis. 4 420–423 [Google Scholar]
- Puto K., Papa S., Hila N. (2010). Dynamic spread of brucellosis in humans in the area of Korca for the years 1999–2009. J. IMAB 16 11–16 10.5272/jimab.1632010_11-16 [DOI] [Google Scholar]
- Radwan A. I., Bekairi S. I., al-Bokmy A. M., Prasad P. V., Mohamed O. M., Hussain S. T. (1993). Successful therapeutic regimens for treating Brucella melitensis and Brucella abortus infections in cows. Rev. Sci. Tech. 12 909–922 [DOI] [PubMed] [Google Scholar]
- Rafai M. (2002). Incidence and control of brucellosis in the Near East region. Vet. Microbiol. 90 81–110 10.1016/S0378-1135(02)00248-1 [DOI] [PubMed] [Google Scholar]
- Rashidi J. S., Ortner D. J., Frohlich B., Jonsdottir B. (2001). Brucellosis in early Bronze age Jordan and Bahrain: an analysis of possible cases of Brucella spondylitis. Am. J. Phys. Anthropol. 114 122 [Google Scholar]
- Rasouli M., Asaei S., Kalani M., Kiany S., Moravej A. (2013). Interleukin-17A genetic variants can confer resistance to brucellosis in Iranian population. Cytokine 61 297–303 10.1016/j.cyto.2012.10.012 [DOI] [PubMed] [Google Scholar]
- Rautureau S., Dufour B., Jaÿ M., Garin-Bastuji B. (2013). Deux cas de brucellose bovine en 2012 appellent à la vigilance. Bull. Epidemiol. Santé Anim. Alim. 59 11–14 [Google Scholar]
- Ravanel N., Gestin B., Maurin M. (2009). In vitro selection of fluoroquinolone resistance in Brucella melitensis. Int. J. Antimicrob. Agents 34 76–81 10.1016/j.ijantimicag.2009.01.002 [DOI] [PubMed] [Google Scholar]
- Read A. F., Mackinnon M. J. (2008). “Pathogen evolution in a vaccinated world,” in Evolution in Health and Disease 2nd edition eds Stearns S. C., Koella J. C. (Oxford: Oxford University Press; ) 139–152 [Google Scholar]
- Reynes E., López G., Ayala S. M., Hunter G. C., Lucero N. E. (2012). Monitoring infected dogs after a canine brucellosis outbreak. Comp. Immunol. Microbiol. Infect. Dis. 35 533–537 10.1016/j.cimid.2012.05.004 [DOI] [PubMed] [Google Scholar]
- Rhyan J. C., Gidlewski T., Ewalt D. R., Hennager S. G., Lambourne D. M., Olsen S. C. (2001a). Seroconversion and abortion in cattle experimentally infected with Brucella sp. isolated from a Pacific harbor seal (Phoca vitulina richardsi). J. Vet. Diagn. Invest. 13 379–382 10.1177/104063870101300502 [DOI] [PubMed] [Google Scholar]
- Rhyan J. C., Gidlewski T., Roffe T. J., Aune K., Philo L. M., Ewalt D. R. (2001b). Pathology of brucellosis in bison from Yellowstone National Park. J. Wildl. Dis. 37 101–109 10.7589/0090-3558-37.1.101 [DOI] [PubMed] [Google Scholar]
- Rhyan J. C., Nol P., Quance C., Gertonson A., Belfrage J., Harris L., et al. (2013). Transmission of brucellosis from elk to cattle and bison, greater Yellowstone area, USA, 2002–2012. Emerg. Infect. Dis. 19 1992–1995 10.3201/eid1912.130167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røed K. H., Flagstad Ø., Bjørnstad G., Hufthammer A. K. (2011). Elucidating the ancestry of domestic reindeer from ancient DNA approaches. Quat. Int. 238 83–88 10.1016/j.quaint.2010.07.031 [DOI] [Google Scholar]
- Román K., Castillo R., Gilman R. H., Calderón M., Vivar A., Céspedes M., et al. (2013). A foodborne outbreak of brucellosis at a police station cafeteria, Lima, Peru. Am. J. Trop. Med. Hyg. 88 552–558 10.4269/ajtmh.12-0606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubach M. P., Halliday J. E., Cleaveland S., Crump J. A. (2013). Brucellosis in low-income and middle-income countries. Curr. Opin. Infect. Dis. 26 404–412 10.1097/QCO.0b013e3283638104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Castañeda M. (1986). Brucelosis 3rd Edn. México: Copilco-Universidad, Ediciones Científicas, Prensa Médica Mexicana [Google Scholar]
- Ryder M. L. (1981). A survey of European primitive breeds of sheep. Genet Sel. Evol. 13 381–418 10.1186/1297-9686-13-4-381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahi T. (1994). Genetics and epidemiology of adult-type hypolactasia. Scand. J. Gastroenterol. Suppl. 202 7–20 10.3109/00365529409091740 [DOI] [PubMed] [Google Scholar]
- Scherer A., McLean A. (2002). Mathematical models of vaccination. Br. Med. Bull. 62 187–199 10.1093/bmb/62.1.187 [DOI] [PubMed] [Google Scholar]
- Scholz H. C., Nöckler K., Göllner C., Bahn P., Vergnaud G., Tomaso H., et al. (2010). Brucella inopinata sp. Nov., isolated from a breast implant infection. Int. J. Syst. Evol. Microbiol. 60 801–808 10.1099/ijs.0.011148-0 [DOI] [PubMed] [Google Scholar]
- Schurig G. G., Roop R. M., II, Bagchi T., Boyle S., Buhrman D., Sriranganathan N. (1991). Biological properties of RB51; a stable rough strain of Brucella abortus. Vet. Microbiol. 28 171–188 10.1016/0378-1135(91)90091-S [DOI] [PubMed] [Google Scholar]
- Senra-Valera A. (2006). Las enfermedades de Santa Teresa. Religión Cult. (Spain) 52 605–814 [Google Scholar]
- Shemesh A. A., Yagupsky P. (2013). Increasing incidence of human brucellosis in southern Israel after the cessation of a veterinarian control campaign. Air Water Borne Dis. 2 2 10.4172/2167-7719.10001122013 [DOI] [Google Scholar]
- Shimol S. B., Dukhan L., Belmaker I., Bardenstein S., Sibirsky D., Barrett C., et al. (2012). Human brucellosis outbreak acquired through camel milk ingestion in southern Israel. Isr. Med. Assoc. J. 14 475–478 [PubMed] [Google Scholar]
- Spink W. W. (1956). The Nature of Brucellosis. Minneapolis: The University of Minnesota Press [Google Scholar]
- Stoenner H. G., Lackman D. B. (1957). A new species of Brucella isolated from the desert wood rat, Neotoma lepida Thomas. Am. J. Vet. Res. 18 947–951 [PubMed] [Google Scholar]
- Tabak F., Hakko E., Mete B., Ozaras R., Mert A., Ozturk R. (2008). Is family screening necessary in brucellosis? Infection 36 575–577 10.1007/s15010-008-7022-6 [DOI] [PubMed] [Google Scholar]
- Teasdale M. D., Bradley D. G. (2012). The Origins of Cattle. Bovine Genomics. Oxford: Wiley-Blackwell. 10.1002/9781118301739.ch1 [DOI] [Google Scholar]
- Terwagne M., Ferooz J., Rolán H. G., Sun Y. H., Atluri V., Xavier M. N., et al. (2013). Innate immune recognition of flagellin limits systemic persistence of Brucella. Cell. Microbiol. 15 942–960 10.1111/cmi.12088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessaro S. V., Forbes L. B. (2004). Experimental Brucella abortus infection in wolves. J. Wildl. Dis. 40 60–65 10.7589/0090-3558-40.1.60 [DOI] [PubMed] [Google Scholar]
- Tiller R. V., Gee J. E., Frace M. A., Taylor T. K., Setubal J. C., Hoffmaster A. R., et al. (2010a). Characterization of novel Brucella strains originating from wild native rodent species in North Queensland, Australia. Appl. Environ. Microbiol. 76 5837–5845 10.1128/AEM.00620-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiller R. V., Gee J. E., Lonsway D. R., Gribble S., Bell S. C., Jennison A., et al. (2010b). Identification of an unusual Brucella strain (BO2) from a lung biopsy in a 52-year old patient with chronic destructive pneumonia. BMC Microbiol. 10:23. 10.1186/1471-2180-10-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tishkoff S. A., Reed F. A., Ranciaro A., Voight B. F., Babbitt C. C., Silverman J. S., et al. (2007). Convergent adaptation of human lactase persistence in Africa and Europe. Nat. Genet. 39 31–40 10.1038/ng1946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traum J. (1914). Report of the Chief of the Bureau of Animal Industry. Washington: United States Department of Agriculture (USDA) [Google Scholar]
- Tuemmers C., Lüders C., Rojas C., Serri M., Castillo C., Espinoza R. (2013). Detección de Brucella canis por método de inmunocromatografía en perros vagos capturados en la ciudad de Temuco, Chile, 2011. Rev. Chilena Infectol. 30 395–401 10.4067/S0716-10182013000400007 [DOI] [PubMed] [Google Scholar]
- Van Bressem M. F., Raga J. A., Di Guardo G., Jepson P. D., Duignan P. J., Siebert U., et al. (2009). Emerging infectious diseases in cetaceans worldwide and the possible role of environmental stressors. Dis. Aquat. Organ. 86 143–157 10.3354/dao02101 [DOI] [PubMed] [Google Scholar]
- van Kolfschoten T., van der Jagt I., Beeren Z., Argiti V., van der Leije J., van Essen H., et al. (2011). A remarkable collection of Late Pleistocene reindeer (Rangifer tarandus) remains from Woerden (The Netherlands). Quat. Int. 238 4–11 10.1016/j.quaint.2010.12.033 [DOI] [Google Scholar]
- Vargas F. J. (2002). Brucellosis in Venezuela. Vet. Microbiol. 90 39–44 10.1016/S0378-1135(02)00243-2 [DOI] [PubMed] [Google Scholar]
- Verger J. M., Grayon M., Zundel E., Lechopier P., Olivier-Bernardin V. (1995). Comparison of the efficacy of Brucella suis strain 2 and Brucella melitensis Rev. 1 live vaccines against a Brucella melitensis experimental infection in pregnant ewes. Vaccine 13 191–196 10.1016/0264-410X(95)93135-V [DOI] [PubMed] [Google Scholar]
- Verger J. M., Grimont F., Grimont P. A., Grayon M. (1985). Brucella, a monospecific genus as shown by deoxyribonucleic acid hybridization. Int. J. Syst. Evol. Microbiol. 35 292–295 [Google Scholar]
- Wang Y., Ke Y., Wang Z., Yuan X., Qiu Y., Zhen Q., et al. (2012). Genome sequences of three live attenuated vaccine strains of Brucella species and implications for pathogenesis and differential diagnosis. J. Bacteriol. 194 6012–6013 10.1128/JB.01483-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittem J. H. (1978). Bovine brucellosis eradication Australia. Proc. Annu. Meet. U. S. Anim. Health Assoc. 82 139–141 [PubMed] [Google Scholar]
- Wise R. I. (1980). Brucellosis in the United States. Past, present, and future. JAMA 244 2318–2322 10.1001/jama.1980.03310200058031 [DOI] [PubMed] [Google Scholar]
- Wyatt H. V. (2000). Dr. G. Caruana Scicluna, the first Maltese microbiologist. J. Med. Biogr. 8 191–193 [DOI] [PubMed] [Google Scholar]
- Wyatt H. V. (2005). How Themistocles Zammit found Malta fever (brucellosis) to be transmitted by the milk of goats. J. R. Soc. Med. 98 451–454 10.1258/jrsm.98.10.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyatt H. V. (2009a). Brucellosis and Maltese goats in the Mediterranean. J. Maltese Hist. 1 4–18 [Google Scholar]
- Wyatt H. V. (2009b). James Crawford Kennedy and the sexual transmission of brucellosis. J. R. Army. Med. Corps 155 239–240 10.1136/jramc-155-03-17 [DOI] [PubMed] [Google Scholar]
- Wyatt H. V. (2010). Surgeon Captain Sheldon F. Dudley and the person to person spread of brucellosis by inhalation. J. R. Nav. Med. Serv. 96 185–187 [PubMed] [Google Scholar]
- Wyatt H. V. (2011). The curious affair of the identity of Fioravanti Sammut (b.1863) and Temistocle Zammit (d.1935). J. Med. Biogr. 19 128–131 10.1258/jmb.2010.010058 [DOI] [PubMed] [Google Scholar]
- Yagupsky P., Baron E. J. (2005). Laboratory exposures to brucellae and implications for bioterrorism. Emerg. Infect. Dis. 11 1180–1185 10.3201/eid1108.041197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Paijmans J. L., Chang F., Wu X., Chen G., Lei C., et al. (2013). Morphological and genetic evidence for early Holocene cattle management in northeastern China. Nat. Commun. 4 2755 10.1038/ncomms3755 [DOI] [PubMed] [Google Scholar]
- Zhang W. Y., Guo W. D., Sun S. H., Jiang J. F., Sun H. L., Li S. L., et al. (2010). Human brucellosis, Inner Mongolia, China. Emerg. Infect. Dis. 16 2001–2003 10.3201/eid1612.091081 [DOI] [PMC free article] [PubMed] [Google Scholar]