Abstract
Primary effusion lymphoma (PEL) is a human herpes virus 8 (HHV8)-positive large B-cell neoplasm that presents as an effusion with no detectable tumor in individuals with human immunodeficiency virus infection or other immune deficiencies. PEL is an aggressive neoplasm with a poor prognosis. PEL cells show diverse morphologies, ranging from immunoblastic or plasmablastic to anaplastic. The immunophenotype of PEL is distinct, but its lineage can be misdiagnosed if not assessed thoroughly. PEL cells usually express CD45, lack B- and T-cell-associated antigens, and characteristically express lymphocyte activation antigens and plasma cell-associated antigens. Diagnosis of PEL often requires the demonstration of a B-cell genotype. HHV8 must be detected in cells to diagnose PEL. In most cases, PEL cells also harbor the Epstein-Barr virus (EBV) genome. Similar conditions associated with HHV8 but not effusion-based are called "extracavitary PELs." PELs should be differentiated from HHV8-negative, EBV-positive, body cavity-based lymphomas in patients with long-standing chronic inflammation; the latter can occur in tuberculous pleuritis, artificial pneumothorax, chronic liver disease and various other conditions. Despite their morphological similarity, these various lymphomas require different therapeutic strategies and have different prognostic implications. Correct diagnosis is essential to manage and predict the outcome of patients with PEL and related disorders.
Keywords: Lymphoma, primary effusion; Human herpes virus 8
Primary effusion lymphoma (PEL), also known as body cavity-based lymphoma, is a distinct large B-cell neoplasm typically presenting as an isolated effusion involving the pleural, peritoneal, or pericardial cavities with no detectable tumor in individuals with human immunodeficiency virus (HIV) infection or other immune deficiencies, such as solid organ transplant recipients.1,2 In rare cases, patients are non-immunocompromised elderly individuals from regions where human herpes virus 8 (HHV8) is endemic, such as Mediterranean regions.1,2
In PEL, HHV8 (also called Kaposi's sarcoma-associated herpesvirus [KSHV]) is present in tumor tissue. In most cases, PEL cells also contain the Epstein-Barr virus (EBV) genome.3 PEL is diagnosed when a cytological specimen shows characteristic large pleomorphic, immunoblastic, plasmablastic, or anaplastic cells with a peculiar "null-cell phenotype." Solid HHV8-positive lymphomas in which tumor cells have a similar morphology and immunotype to PEL cells, but which are not effusion-based, are termed "extracavitary PELs."4 Extracavitary PELs have slightly different clinicopathologic characteristics compared to PEL.2 PEL cells typically do not express B-cell-associated antigens, and the diagnosis often requires the demonstration of a B-cell genotype.1,2,5 PEL should be distinguished from HHV8-negative effusion-based lymphomas in patients with long-standing chronic inflammation, which arises from various conditions including tuberculous pyothorax, artificial pneumothorax, and chronic liver disease.6,7,8,9,10 This review summarizes the characteristics of PEL, with an emphasis on its differential diagnosis.
EPIDEMIOLOGY
PEL is a rare lymphoma that represents approximately 4% of all acquired immunodeficiency syndrome (AIDS)-related lymphomas, as well as 0.1% to 1% of all aggressive lymphomas in HIV-negative immunodeficient patients in regions where HHV8 is not endemic.3 In Korea, PEL comprises approximately 0.1% of non-Hodgkin lymphomas.11,12 Most cases occur in HIV-infected, young to middle-aged, severely immunocompromised, homosexual/bisexual men.1 In the HIV-negative population, PELs have been reported in elderly individuals primarily from regions where HHV8 is endemic, such as Mediterranean regions, but not from Africa, or in solid organ transplant recipients.3,13 Extracavitary PEL accounts for approximately 5% of all AIDS-related lymphomas.5
HHV8 is a geographically restricted virus. The seroprevalence of HHV8 is >50% in high incidence zones in Africa and parts of the Amazon Basin, 5% to 20% in intermediate incidence zones in Mediterranean countries, and <5% in low incidence zones in North America, Northern Europe, and Asia.14 In Korea, the seroprevalence of HHV8 is 4.93% in the female general population15 and 3.5% in hospitalized children.16 In comparison, the seroprevalence of HHV8 is higher among immunocompromised people; it is 15% among solid organ transplant patients in the United States, and 30% among HIV-infected homosexual/bisexual men.17,18
ETIOLOGY AND PATHOGENESIS
HHV8, like EBV, belongs to the lymphotropic gamma herpesvirus family.13,19,20 HHV8 is transmitted through bodily fluids, such as saliva. Following the primary infection, HHV8 establishes life-long latency in B-cells. During latency, no viral particles are produced, but a set of viral genes that promote cellular proliferation are expressed, which enable the virus to perpetuate in the host B-cell population.13,19 Cytotoxic T-cells normally limit this virally driven cellular proliferation by recognizing viral proteins. Cellular proliferation is unchecked when host immunity is compromised, which increases the chance of malignant clone emergence.5 Viral proteins that have a transforming role in PEL include HHV8/KSHV latent nuclear antigen 1 (LANA-1), v-cyclin, vFLIP (K13), LANA-2 (vIRF-3), vIL-6, K1, kaposin, and K5. These proteins have proliferative, pro-mitotic, anti-apoptotic, pro-inflammatory, and angiogenic functions.5,20 Unknown stimuli can induce HHV8 to transform from its latent state into a lytic state, after which infectious virions are produced and released in saliva. Up to 25% of PEL cells express HHV8 lytic phase genes, which may underlie the reinfection of cells with HHV8, as well as the infection of cells not previously infected.21 During lytic infection, viral genes with pro-inflammatory and angiogenic functions are upregulated, especially those encoding vIL-6, chemokine homologs and their ligands, and transmembrane signaling proteins, which provide further pro-proliferative signals to PEL cells.20
In PEL, genetic lesions commonly seen in other types of AIDS-related lymphomas are absent, with no MYC or BCL6 gene rearrangements, and no mutations of the RAS oncogene or the TP53 tumor suppressor gene.5,22,23,24 The presence of multiple chromosomal abnormalities suggests that secondary genetic events contribute to neoplastic transformation of PEL cells.24 During latency, HHV8 expresses microRNAs that promote cellular survival, for example, by augmenting nuclear factor-κB activity induced by vFLIP, by targeting IκB, or by preventing cell-cycle arrest through targeting p21 mRNA.5,20
The vast majority of PEL cells also harbor EBV.3 In HIV-positive patients, PELs are invariably positive for EBV, which are monoclonal in most cases.2 However, the role of EBV in PEL is uncertain because it has a restricted latency pattern with only EBNA1 and EBV-encoded small RNA (EBER) gene expression (latency 1).2,5
CLINICAL PRESENTATION
In HIV-infected populations, patients with PEL are older and more immunosuppressed than those with Burkitt lymphoma.2 According to Said,2 most HIV-positive PEL patients are in their thirties and have been diagnosed with AIDS, with T-cell counts of <100/mm3. Kaposi's sarcoma lesions are identified in one-third of PEL patients.23 PEL typically presents as a lymphomatous effusion in the pleural, pericardial, or peritoneal cavities, without any extracavitary tumors.1 Typically, a single body cavity is involved. Symptoms include dyspnea and ascites,1,2 and patients usually have B symptoms. While the majority of patients present with no associated mass, a subset of patients develop extension of the pleura or surrounding organs. In approximately one-third of patients,5 the lymphoma disseminates to extracavitary sites, including lymph nodes and bone marrow.
In extracavitary PEL, tumors occur that have a similar morphology, immunophenotype, and gene expression profile to classical PEL.4,25 Extracavitary PEL commonly involves the gastrointestinal tract, skin, lungs, central nervous system, and lymph nodes.4,22,26 Extracavitary PEL occurs at a slightly earlier stage of HIV infection than PEL, and presents with severe systemic symptoms, generalized lymphadenopathy, and multiple extranodal involvement, with patients frequently showing anemia, hypoalbuminemia, autoimmune thrombocytopenia, and a positive Coomb's test.22
MORPHOLOGICAL FEATURES
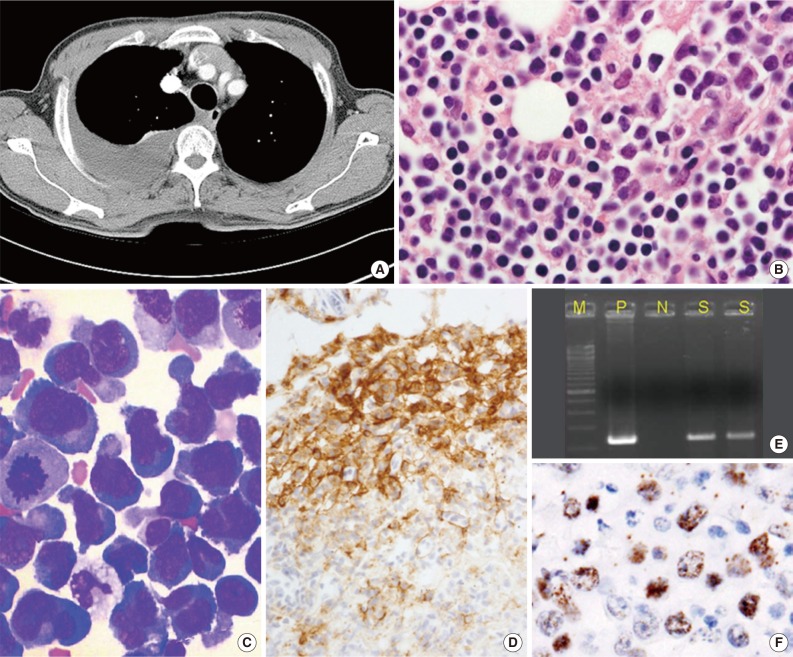
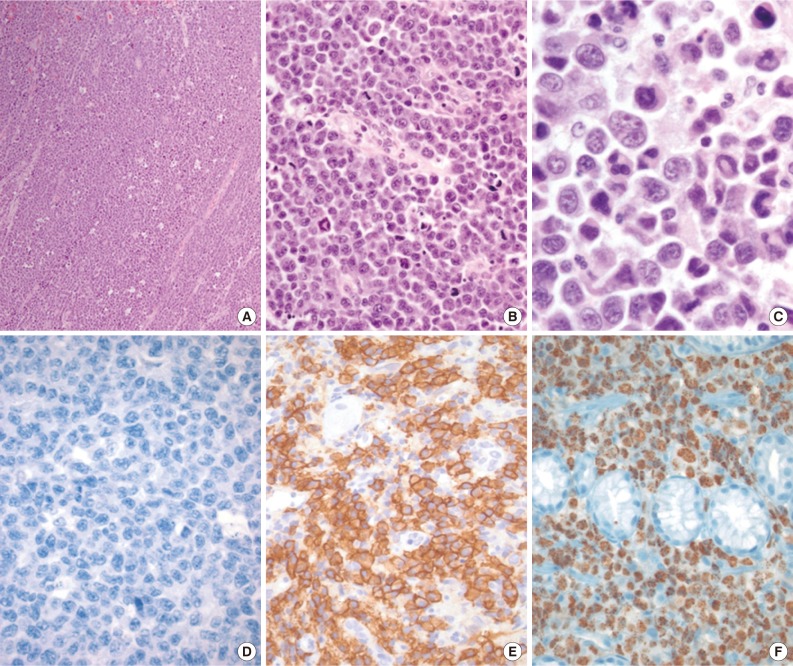
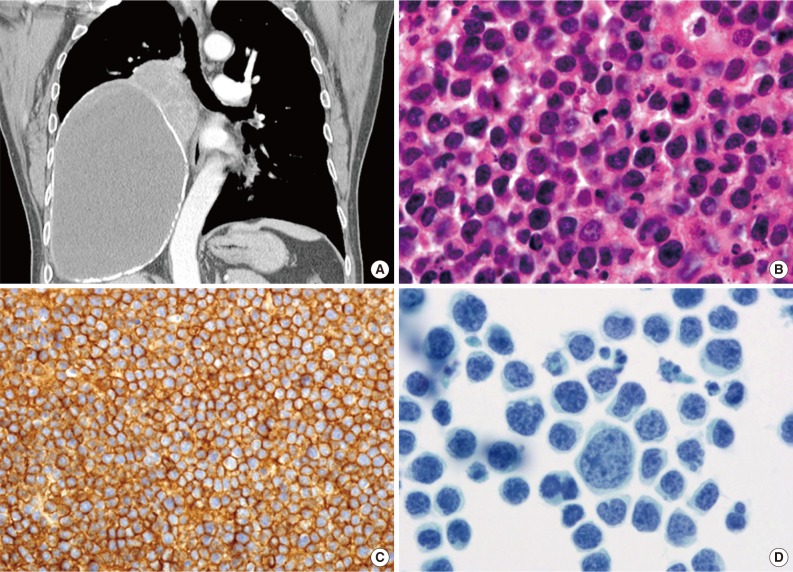
PEL is typically diagnosed on the basis of cytological (cytospin or cell block) preparations of effusion fluid. PEL cells show features that are intermediate between those of immunoblastic and anaplastic large cell lymphomas (ALCLs), with or without plasma cell differentiation (Figs. 1B, 1C, 2C).1,2,22 PEL cells are large, and pleomorphic or monotonous, with marked variation in size (Figs. 1C, 2C). The nuclei of these cells are large, and round to lobated, with prominent nucleoli. These cells contain a variable amount of cytoplasm that is deeply basophilic and often vacuolated. Poorly defined paranuclear hofs are often observed, and anaplastic cells may be detected that resemble Reed-Sternberg cells in classical Hodgkin lymphoma. Similar cells are observed in tissue sections, with tingible body macrophages and numerous mitotic figures with or without a starry-sky appearance (Fig. 2A).1 The marked pleomorphism characteristically seen in cytological specimens may not be apparent in tissue sections.1,27
Fig. 1.
Primary effusion lymphoma (PEL). (A) Axial computed tomography scan shows pleural effusion of the right hemithorax with pleural enhancement. No marked parenchymal lesion is identified in either lung, apart from passive atelectasis owing to the effusion. Neither lymphadenopathy nor organomegaly is observed. (B) PEL cells show anaplastic/plasmablastic cytological features (cell block). (C) Cytospin showing large anaplastic tumor cells with features of plasmacytoid or immunoblastic features (Wright stain). (D) A subset of PEL cells is positive for CD138. Human herpes virus 8 can be identified in PEL cells by performing polymerase chain reaction (E) and immunocytochemistry (F) to detect latent nuclear antigen 1 on a cell block.
Fig. 2.
Solid primary effusion lymphoma (Solid PEL) tumor. (A) Starry-sky pattern. (B) Numerous mitoses. (C) Solid PEL cells, like PEL cells, show anaplastic/plasmablastic cytologic features, and some resemble Reed-Sternberg cells. (D-F) Immunohistochemical studies reveal that the tumor cells are CD20-negative (D), CD138-positive (E), and human herpes virus 8-positive (labeling for latent nuclear antigen 1) (F).
IMMUNOPHENOTYPE
PEL has a "null" lymphocyte phenotype.27 PEL cells usually express CD45, but lack pan-B-cell antigens (CD19, CD20, CD79a, and surface and cytoplasmic immunoglobulins [Igs]), and T-cell antigens (CD3, CD4, and CD8).1,2,28 These cells are generally positive for markers associated with lymphocyte activation, including CD30, CD38, CD71, epithelial membrane antigen, the human leukocyte antigen DR, and plasma cell differentiation-related antigens (CD138, VS38c, and MUM-1/IRF4) (Figs. 1D, 2E). In a subset of cases, PEL cells are positive for aberrant T-cell markers, such as CD45RO (90%), CD7 (30%), and CD4 (20%), by flow cytometry.29 PEL cells do not usually express Bcl-6,1 are negative for anaplastic lymphoma kinase 1, and usually have a high Ki-67 labeling index. Rare PEL cases with a T-cell phenotype and T-cell receptor gene rearrangement have been reported, and these cases appear to be of T-cell origin.30
HHV8 must be detected in cells to diagnose PEL. A monoclonal antibody against LANA-1, which is encoded by open reading frame 73, is a highly sensitive and specific marker of HHV8 infection in paraffin-embedded tissue sections (Figs. 1F, 2F).1,2 EBV infection can be demonstrated by in situ hybridization to detect EBER. Lymphoma cells do not express EBV latent membrane protein 1, whereas a subset of cells expresses viral interleukin-6.
MOLECULAR GENETIC FEATURES
Ig genes are clonally rearranged in PEL, and some cases have rearrangements of both Ig and T-cell receptor genes.2 Somatic hypermutations also occur in PEL. Common genetic abnormalities that are seen in diffuse large B-cell lymphomas are not detected in PEL, including MYC and BCL6 gene rearrangements, and mutations of the RAS oncogene and TP53 tumor suppressor gene.22,23 Gene expression profiling indicates that PEL cells show features of both immunoblasts and plasma cells, but not of germinal center or memory B-cells; MUM-1/IRF-4, CD30, interleukin 10, and vascular endothelial growth factor are upregulated, whereas CD19, CD20, and CD79a/b are downregulated.31 These finding suggests that PEL cells are post-germinal center B-cells or activated B-cells that undergo terminal plasma cell differentiation.22
Polymerase chain reaction (PCR) detection of HHV8 DNA can demonstrate the presence of the viral genome in tumor tissue (Fig. 1E), which has diagnostic significance.1,2,21 However, the utility of PCR testing for HHV8 DNA in blood and other specimens is limited.21 HHV8 viremia is suggestive of PEL, but cannot be used to definitively diagnose PEL. HHV8 viremia is only observed in 10% to 60% of PEL cases; therefore, PEL cannot be excluded when HHV8 DNA is not detected by PCR.
DIFFERENTIAL DIAGNOSIS
When a smear and/or cell block of the effusion shows large malignant cells that are present singly, this can be indicative of undifferentiated carcinoma as well as malignant lymphoma. Cells that have a plasmacytoid morphology and nuclei containing condensed chromatin are likely of a lymphoid origin. However, it may be impossible to rule out carcinoma without performing immunophenotypic studies.
In patients without a tumor mass but with an effusion that is confirmed to contain cells of a lymphoid origin, PEL must be distinguished from several other types of lymphomas using morphological, immunophenotypic, and clonality analyses, as necessary. PEL and its main differential diagnoses are summarized in Table 1.1,2,9,29,32
Table 1.
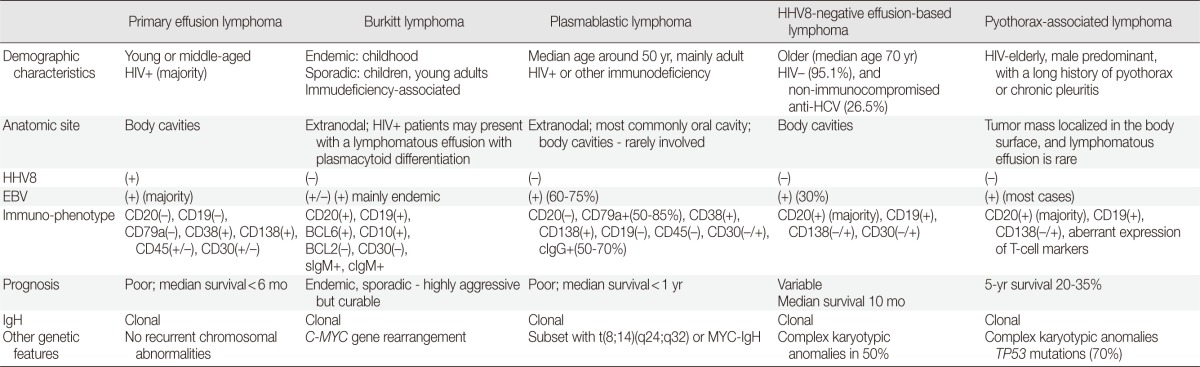
HHV8, human herpesvirus 8; HIV, human immunodeficiency virus; HCV, hepatitis C virus; EBV, Epstein-Barr virus; sIg, surface immunoglobulin; cIg, cytoplasmic immunoglobulin; IgH, immunoglobulin heavy chain gene rearrangement.
'Burkitt lymphoma' may present in HIV-positive individuals as a lymphomatous effusion with plasmacytoid differentiation.27 In addition to the distinctive phenotype of Burkitt lymphoma cells (CD20-positive, CD19-positive, BCL6-positive, CD10-positive, BCL2-negative, sIgM-positive, and cIgM-positive), HHV8 negativity and a C-MYC gene rearrangement are also characteristic.2
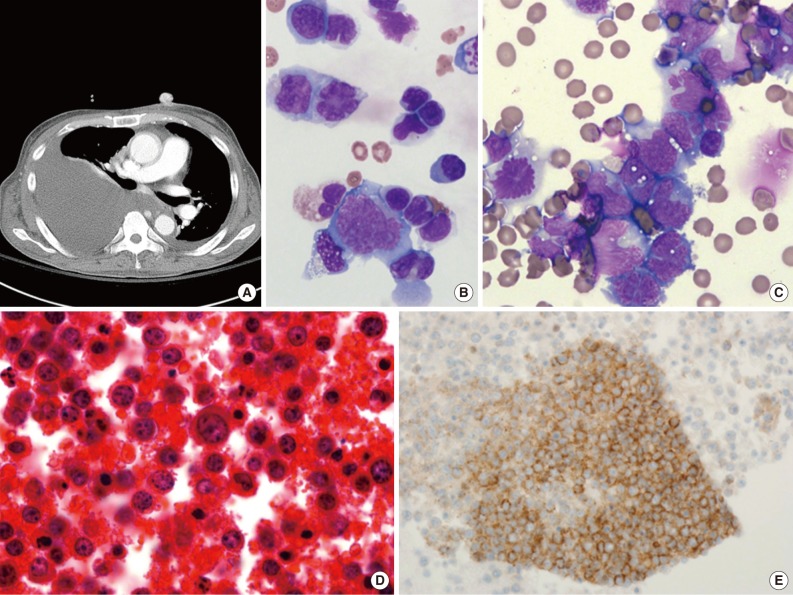
'HHV8-negative effusion-based lymphomas' resembling PELs have been reported. These have been named PEL-like lymphoma, HHV8-unrelated PEL, and body cavity-based high-grade lymphoma.2,8,9,33,34 Patients with HHV8-negative effusion-based lymphomas tend to be elderly (median age 70 years), Japanese (60%), HIV-negative (95.1%), and non-immunocompromised, and there is a slight male predominance (male:female ratio, 3:2). These patients frequently have anti-hepatitis C antibodies (26.5%) and pre-existing medical diseases (>50%) that predispose them to fluid overload, including cirrhosis (hepatitis B, hepatitis C, and alcoholism) and cardiac problems.8,9,33,34 In contrast to PEL, tumor cells in these lymphomas are medium- to large-sized, have an immunoblastic, plasmacytoid, or plasmablastic morphology, and express B-cell-associated antigens (Fig. 3). According to the Hans classification, these tumors have a germinal center B or a mixed germinal center B/activated B-cell signature.9 Moreover, 30% of these tumors are EBV-positive. The prognosis of patients with these types of tumors is more favorable than that of PEL patients.9 Of patients with HHV8-negative effusion-based lymphomas, 70% who were managed with aspiration only and 82.1% who received chemotherapy achieved complete or partial remission,9 with a median survival time of 10 months, which is in sharp contrast to the uniformly poor outcome of PEL patients.
Fig. 3.
Human herpes virus 8-negative effusion-based lymphoma. (A) A chest computed tomography scan reveals a large amount of pleural effusion. Pleural enhancement is characteristically observed on both sides of the chest. Mediastinal lymphadenopathy is also observed. Massive ascites with multiple lymphadenopathy is sometimes detected. (B, C) The effusion contains large pleomorphic cells with large blastic nuclei (Giemsa stain). Tumor cells are large, immunoblastic or plasmablastic (D), and express the B-cell-associated antigen CD20 (E).
'Pyothorax-associated lymphoma (PAL)' presents as a pleural effusion in HIV-negative elderly people, usually males (male: female ratio, 12:3), with a long history of pyothorax or chronic pleuritis resulting from therapeutic artificial pneumothorax or tuberculous pleuritis.35 Most cases have been reported in Japan. PAL develops 20 to 64 years after the onset of tuberculosis and primarily presents as a tumor mass on the body surface. Lymphomatous effusions are rarely detected. PAL cells are morphologically similar to diffuse large B-cell lymphoma, not otherwise specified, with centroblastic or immunoblastic appearances (Fig. 4). All PAL cells express B-cell markers and aberrant T-cell markers, and a fraction express plasma cell markers. PAL cells are HHV8-negative, and, in most cases, EBV-positive.
Fig. 4.
Pyothorax-associated lymphoma. (A) Two masses are located in the middle to lower right hemithorax. The larger of the two masses shows fluid attenuation and air bubbles, which is consistent with chronic empyema. Abutting the superomedial side of this mass is a smaller heterogeneously enhanced solid mass. The left lung is unremarkable, and mediastinal lymphadenopathy is not observed. (B) The lymphoma cells are morphologically similar to diffuse large B-cell lymphoma, not otherwise specified, with centroblastic or immunoblastic appearances. (C) The tumor cells express CD20. (D) Cytologically, the tumor cells are markedly pleomorphic (Papanicolaou stain).
'Plasmablastic lymphoma' is a rare variant of diffuse large B-cell lymphoma. It is characterized by B-immunoblast-like cells with the same immunotype as plasma cells36 and a similar morphology to PEL cells. This condition mainly affects HIV-positive patients, but is also seen in patients with other immunodeficient conditions.36,37 It commonly involves the oral cavity or jaw. Tumor cells can be immunoblastic with prominent central nucleoli, or plasmablastic with abundant basophilic cytoplasm. The immunophenotype of these cells is similar to that of PEL cells, because they are CD20-negative and CD138-positive. Moreover, 50% to 85% and 50% to 70% of plasmablastic lymphoma cases are CD79a-positive and cytoplasmic IgG-positive, respectively.36 EBV infection is found in most plasmablastic lymphoma cases (60-75%), whereas HHV8 is absent.
'ALCL' can present as pleural effusion that mimics PEL in rare cases. However, in contrast to PEL, ALCL affects young, HIV-negative individuals. ALCL cells are large lymphoid cells with marked nuclear atypia reminiscent of PEL cells.27,38 ALCL cells have a distinctive phenotype; they are strongly CD30-positive in all cases and frequently positive for epithelial membrane antigen, cytotoxic granule proteins (TIA-1, granzyme, and perforin), CD45, and T-cell-specific markers. In approximately one-third of cases, ALCL cells have a null-cell immunophenotype, despite having a T-cell genotype.38 ALCL cases that have a translocation of the ALK gene still express the ALK protein. ALCL can be distinguished from similar conditions on the basis of the absence of HHV8 and EBV.
'Plasma cell myeloma' of a plasmablastic or anaplastic type can mimic PEL. Morphologically, plasmablastic myeloma can be indistinguishable from PEL. Neoplastic plasma cells express CD138 and cytoplasmic IgG, may express CD79a, CD56, and cyclin D1, and may not express CD45 or CD30.39,40,41
'ALK-positive large B-cell lymphoma' may exhibit plasmablastic differentiation and mimic PEL. However, these cells do not express CD30,42 are negative for HHV8 and EBV (as determined by labeling for EBER and latent membrane protein 1), and are strongly positive for ALK protein. In most cells, staining for ALK has a granular cytoplasmic pattern that is highly indicative of the t(2;17)(p23;q23) translocation or a CLTC-ALK fusion protein.
'Large B-cell lymphoma associated with multicentric Castleman's disease' occurs in patients with or without HIV infection and mainly involves lymph nodes and the spleen.43 It is distinctive from PEL in many ways, although both are associated with HHV8 infection. In large B-cell lymphoma associated with multicentric Castleman's disease, HHV8-positive plasmablasts express high levels of cytoplasmic IgM. In contrast, PEL cells generally do not express cytoplasmic Igs. In large B-cell lymphoma associated with multicentric Castleman's disease, cells harbor non-mutated Ig variable region genes and are derived from CD27- and CD138-negative naive B-cells. By contrast, PEL cells usually express CD138 and harbor hypermutated rearranged Ig genes, suggesting they originate from germinal center or post-germinal center B cells.41,43 Whereas PEL is commonly associated with EBV infection, large B-cell lymphoma associated with multicentric Castleman's disease is not.41,43
'Primary pleural effusion post-transplant lymphoproliferative disorder (PTLD)' can occur in transplant recipients.44,45 Most cases of effusion-based PTLD are secondary to widespread solid organ involvement. Primary effusion presentation of PTLD is very uncommon. In this condition, lymphoid cells are monotonous, intermediate to large sized, transformed, have irregular multilobated nuclei and scant cytoplasm, and are located in regions containing abundant karyorrhectic debris. PTLD cells express pan-B-cell markers and are CD30-negative, HHV8-negative, and EBER-positive.
TREATMENT AND PROGNOSIS
There is no standard treatment for PEL. Attempts have been made to treat PEL with a standard chemotherapy using the CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone) regimen; however, the prognosis for patients with PEL remains extremely poor. Their median survival time is <6 months, and most patients die within 1 year of diagnosis.1,2,27 Causes of death include progression of the disease, opportunistic infections, and other HIV-related complications.27
HIV-associated PEL should be treated with highly active antiretroviral therapy.46 As mentioned above, treatment of PEL patients with the standard CHOP regimen treatment had disappointing result, whereas treatment with bortezomib-containing regimens reportedly improved the survival of PEL patients.47 Chemotherapy should be coupled with immune reconstitution, as well as treatment with interferon-α in combination with azidothymidine.48
CONCLUSION
PEL is an HHV8-related lymphoma that typically presents as a malignant serous effusion with no evidence of a solid tumor mass. Extracavitary PEL typically presents as a solid tumor mass in locations such as lymph nodes and the gastrointestinal tract without any effusion. These conditions are often difficult to diagnose owing to the null-cell phenotype of the cells. Other tumors with a similar clinical presentation, morphology, and immunophenotype to PEL should be carefully excluded to properly manage and predict the outcome of PEL patients. HHV8 must be detected in cells to diagnose PEL.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Said J, Cesarman E. Primary effusion lymphoma. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 260–261. [Google Scholar]
- 2.Said J. Hematopathology of human Immunodeficiency virus (HIV) infection. In: Jaffe ES, Harris NL, Vardiman JW, Campo E, Arber DA, editors. Hematopathology. Philadelphia: Elsevier Saunders; 2011. pp. 867–883. [Google Scholar]
- 3.Cesarman E, Chang Y, Moore PS, Said JW, Knowles DM. Kaposi's sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. N Engl J Med. 1995;332:1186–1191. doi: 10.1056/NEJM199505043321802. [DOI] [PubMed] [Google Scholar]
- 4.Chadburn A, Hyjek E, Mathew S, Cesarman E, Said J, Knowles DM. KSHV-positive solid lymphomas represent an extra-cavitary variant of primary effusion lymphoma. Am J Surg Pathol. 2004;28:1401–1416. doi: 10.1097/01.pas.0000138177.10829.5c. [DOI] [PubMed] [Google Scholar]
- 5.Cesarman E. Gammaherpesvirus and lymphoproliferative disorders in immunocompromised patients. Cancer Lett. 2011;305:163–174. doi: 10.1016/j.canlet.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petitjean B, Jardin F, Joly B, et al. Pyothorax-associated lymphoma: a peculiar clinicopathologic entity derived from B cells at late stage of differentiation and with occasional aberrant dual B- and T-cell phenotype. Am J Surg Pathol. 2002;26:724–732. doi: 10.1097/00000478-200206000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Ohsawa M, Tomita Y, Kanno H, et al. Role of Epstein-Barr virus in pleural lymphomagenesis. Mod Pathol. 1995;8:848–853. [PubMed] [Google Scholar]
- 8.Ichinohasama R, Miura I, Kobayashi N, et al. Herpes virus type 8-negative primary effusion lymphoma associated with PAX-5 gene rearrangement and hepatitis C virus: a case report and review of the literature. Am J Surg Pathol. 1998;22:1528–1537. doi: 10.1097/00000478-199812000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Alexanian S, Said J, Lones M, Pullarkat ST. KSHV/HHV8-negative effusion-based lymphoma, a distinct entity associated with fluid overload states. Am J Surg Pathol. 2013;37:241–249. doi: 10.1097/PAS.0b013e318267fabc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ha SY, Choi YL, Kim SJ, Ko YH. Diffuse large B-cell lymphoma associated with chronic inflammation manifested as a soft tissue mass: incidental discovery on histological examination. Korean J Pathol. 2011;45:417–422. [Google Scholar]
- 11.Yoon SO, Suh C, Lee DH, et al. Distribution of lymphoid neoplasms in the Republic of Korea: analysis of 5,318 cases according to the World Health Organization classification. Am J Hematol. 2010;85:760–764. doi: 10.1002/ajh.21824. [DOI] [PubMed] [Google Scholar]
- 12.Kim JM, Ko YH, Lee SS, et al. WHO classification of malignant lymphomas in Korea: report of the third nationwide study. Korean J Pathol. 2011;45:254–260. [Google Scholar]
- 13.Ariza-Heredia EJ, Razonable RR. Human herpes virus 8 in solid organ transplantation. Transplantation. 2011;92:837–844. doi: 10.1097/TP.0b013e31823104ec. [DOI] [PubMed] [Google Scholar]
- 14.Moore PS, Chang Y. Molecular virology of Kaposi's sarcoma-associated herpesvirus. Philos Trans R Soc Lond B Biol Sci. 2001;356:499–516. doi: 10.1098/rstb.2000.0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Sanjose S, Mbisa G, Perez-Alvarez S, et al. Geographic variation in the prevalence of Kaposi sarcoma-associated herpesvirus and risk factors for transmission. J Infect Dis. 2009;199:1449–1456. doi: 10.1086/598523. [DOI] [PubMed] [Google Scholar]
- 16.Han TH, Chung JY, Kim SW. Seroprevalence of human herpesvirus 8 in children in Seoul, Korea. Pediatr Infect Dis J. 2005;24:476. doi: 10.1097/01.inf.0000160990.10452.0f. [DOI] [PubMed] [Google Scholar]
- 17.Lennette ET, Blackbourn DJ, Levy JA. Antibodies to human herpesvirus type 8 in the general population and in Kaposi's sarcoma patients. Lancet. 1996;348:858–861. doi: 10.1016/S0140-6736(96)03240-0. [DOI] [PubMed] [Google Scholar]
- 18.Jenkins FJ, Hoffman LJ, Liegey-Dougall A. Reactivation of and primary infection with human herpesvirus 8 among solid-organ transplant recipients. J Infect Dis. 2002;185:1238–1243. doi: 10.1086/340237. [DOI] [PubMed] [Google Scholar]
- 19.Edelman DC. Human herpesvirus 8: a novel human pathogen. Virol J. 2005;2:78. doi: 10.1186/1743-422X-2-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ganem D. KSHV and the pathogenesis of Kaposi sarcoma: listening to human biology and medicine. J Clin Invest. 2010;120:939–949. doi: 10.1172/JCI40567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gantt S, Casper C. Human herpesvirus 8-associated neoplasms: the roles of viral replication and antiviral treatment. Curr Opin Infect Dis. 2011;24:295–301. doi: 10.1097/QCO.0b013e3283486d04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carbone A, Gloghini A. AIDS-related lymphomas: from pathogenesis to pathology. Br J Haematol. 2005;130:662–670. doi: 10.1111/j.1365-2141.2005.05613.x. [DOI] [PubMed] [Google Scholar]
- 23.Nador RG, Cesarman E, Chadburn A, et al. Primary effusion lymphoma: a distinct clinicopathologic entity associated with the Kaposi's sarcoma-associated herpes virus. Blood. 1996;88:645–656. [PubMed] [Google Scholar]
- 24.Ansari MQ, Dawson DB, Nador R, et al. Primary body cavity-based AIDS-related lymphomas. Am J Clin Pathol. 1996;105:221–229. doi: 10.1093/ajcp/105.2.221. [DOI] [PubMed] [Google Scholar]
- 25.Deloose ST, Smit LA, Pals FT, Kersten MJ, van Noesel CJ, Pals ST. High incidence of Kaposi sarcoma-associated herpesvirus infection in HIV-related solid immunoblastic/plasmablastic diffuse large B-cell lymphoma. Leukemia. 2005;19:851–855. doi: 10.1038/sj.leu.2403709. [DOI] [PubMed] [Google Scholar]
- 26.Pan ZG, Zhang QY, Lu ZB, et al. Extracavitary KSHV-associated large B-Cell lymphoma: a distinct entity or a subtype of primary effusion lymphoma? Study of 9 cases and review of an additional 43 cases. Am J Surg Pathol. 2012;36:1129–1140. doi: 10.1097/PAS.0b013e31825b38ec. [DOI] [PubMed] [Google Scholar]
- 27.Patel S, Xiao P. Primary effusion lymphoma. Arch Pathol Lab Med. 2013;137:1152–1154. doi: 10.5858/arpa.2012-0294-RS. [DOI] [PubMed] [Google Scholar]
- 28.Carbone A, Gloghini A, Larocca LM, et al. Expression profile of MUM1/IRF4, BCL-6, and CD138/syndecan-1 defines novel histogenetic subsets of human immunodeficiency virus-related lymphomas. Blood. 2001;97:744–751. doi: 10.1182/blood.v97.3.744. [DOI] [PubMed] [Google Scholar]
- 29.Vega F. Primary effusion lymphoma (PEL) and solid variant of PEL. In: Medeiros LJ, Miranda RN, Wang SA, editors. Diagnostic pathology: lymph nodes and spleen with extranodal lymphomas. Vol. 7. Altona: Amirsys; 2011. pp. 78–85. [Google Scholar]
- 30.Coupland SE, Charlotte F, Mansour G, Maloum K, Hummel M, Stein H. HHV-8-associated T-cell lymphoma in a lymph node with concurrent peritoneal effusion in an HIV-positive man. Am J Surg Pathol. 2005;29:647–652. doi: 10.1097/01.pas.0000157937.01624.1d. [DOI] [PubMed] [Google Scholar]
- 31.Klein U, Gloghini A, Gaidano G, et al. Gene expression profile analysis of AIDS-related primary effusion lymphoma (PEL) suggests a plasmablastic derivation and identifies PEL-specific transcripts. Blood. 2003;101:4115–4121. doi: 10.1182/blood-2002-10-3090. [DOI] [PubMed] [Google Scholar]
- 32.Ferry JA. Extramodal lymphomas. Philadelphia: Saunders-Elsevier; 2011. pp. 81–132. [Google Scholar]
- 33.Kang SY, Park CJ, Huh JR, Kang YG, Lee YS, Chi HS. Three cases of primary effusion lymphoma. Korean J Hematol. 2003;38:136–141. [Google Scholar]
- 34.Kim YA, Huh J, Yoon SO, et al. Primary effusion lymphoma and human herpesvirus 8-negative effusion-based lymphoma: analysis of 17 cases in Korea. Korean J Pathol. 2013;47(Suppl 1):S100. [Google Scholar]
- 35.Chan JK, Aozasa K, Gaulard P. DLBCL associated with chronic inflammation. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 245–246. [Google Scholar]
- 36.Stein H, Harris NL, Campo E. Plasmablastic lymphoma. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 256–257. [Google Scholar]
- 37.Lee HI, Koo HR, Han EM, et al. Fine needle aspiration cytology of the plasmablastic lymphoma in human immunodeficiency virus (HIV) negative patient: a case report. Korean J Cytopathol. 2005;16:47–51. [Google Scholar]
- 38.Delsol G, Falini B, Muller-Hermelink HK, et al. Anaplastic large cell lymphoma (ALCL), ALK-positive. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO cclassification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 312–316. [Google Scholar]
- 39.McKenna RW, Kyle RA, Kuehl WM, Grogan TM, Harris NL, Coupland RW. Plasma cell neoplasms. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 200–213. [Google Scholar]
- 40.Vega F, Chang CC, Medeiros LJ, et al. Plasmablastic lymphomas and plasmablastic plasma cell myelomas have nearly identical immunophenotypic profiles. Mod Pathol. 2005;18:806–815. doi: 10.1038/modpathol.3800355. [DOI] [PubMed] [Google Scholar]
- 41.Kim Y, Leventaki V, Bhaijee F, Jackson CC, Medeiros LJ, Vega F. Extracavitary/solid variant of primary effusion lymphoma. Ann Diagn Pathol. 2012;16:441–446. doi: 10.1016/j.anndiagpath.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 42.Delsol G, Campo E, Gascoyne RD. ALK-positive large B-cell lymphoma. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 254–255. [Google Scholar]
- 43.Isaacson PG, Campo E, Harris NL. Large B-cell lymphoma arising in HHV8-associated multicentric Castleman diseae. In: Swerdlow SH, Campo E, Harris NL, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press; 2008. pp. 258–259. [Google Scholar]
- 44.Ohori NP, Whisnant RE, Nalesnik MA, Swerdlow SH. Primary pleural effusion posttransplant lymphoproliferative disorder: Distinction from secondary involvement and effusion lymphoma. Diagn Cytopathol. 2001;25:50–53. doi: 10.1002/dc.2001. [DOI] [PubMed] [Google Scholar]
- 45.Lechapt-Zalcman E, Rieux C, Cordonnier C, Desvaux D. Posttransplantation lymphoproliferative disorder mimicking a nonspecific lymphocytic pleural effusion in a bone marrow transplant recipient. A case report. Acta Cytol. 1999;43:239–242. doi: 10.1159/000330985. [DOI] [PubMed] [Google Scholar]
- 46.Ripamonti D, Marini B, Rambaldi A, Suter F. Treatment of primary effusion lymphoma with highly active antiviral therapy in the setting of HIV infection. AIDS. 2008;22:1236–1237. doi: 10.1097/QAD.0b013e3282fc732b. [DOI] [PubMed] [Google Scholar]
- 47.Siddiqi T, Joyce RM. A case of HIV-negative primary effusion lymphoma treated with bortezomib, pegylated liposomal doxorubicin, and rituximab. Clin Lymphoma Myeloma. 2008;8:300–304. doi: 10.3816/CLM.2008.n.042. [DOI] [PubMed] [Google Scholar]
- 48.Ghosh SK, Wood C, Boise LH, et al. Potentiation of TRAIL-induced apoptosis in primary effusion lymphoma through azidothymidine-mediated inhibition of NF-kappa B. Blood. 2003;101:2321–2327. doi: 10.1182/blood-2002-08-2525. [DOI] [PubMed] [Google Scholar]