Abstract
Objective
This study was performed to assess the postoperative pain of brain tumor patients who underwent elective craniotomy and to evaluate the factors associated with pain intensity.
Methods
From January 2010 to December 2011, 47 patients with newly diagnosed brain tumors who underwent craniotomy were enrolled. The postoperative pain status was assessed daily until discharge using the visual analogue scale (VAS).
Results
The study participants comprised of 22 males and 25 females with ages ranging from 18-76 years (median age, 50 years). Patients were divided into two groups: the painful group included patients who had a VAS score of more than 3 during their hospital stay after the craniotomy, and the tolerable group included patients who had a VAS score of 1 to 3 during their hospital stay. There were no differences between the two groups in terms of age, sex, location of surgery, history of diabetes, hypertension and smoking, body mass index, and hospital stay. Univariate analysis revealed that operating time, length of wound, head fixation, and perioperative administration of opioid were not associated with the intensity of postoperative pain. Daily assessment of VAS revealed the two peaks of pain on the operation day and the 4th postoperative day. The intensity of pain during the ambulation period was higher than that during intensive care unit (ICU) stay.
Conclusion
Pain following elective craniotomy for brain tumor removal is insufficiently managed, especially after discharge from the ICU. More attention needs to be paid to patients' pain throughout the hospital stay.
Keywords: Brain neoplasm, Postoperative pain, Craniotomy, Visual analogue scale, Pain management, Analgesia
INTRODUCTION
Little is known about pain in patients undergoing neurosurgical procedures. It has been previously pointed out that postoperative pain after neurosurgery was modest and less worrying than during other surgical procedures [1]. There are relatively few studies in which the incidence and severity of pain have actually been assessed in patients undergoing neurosurgical procedures [2,3].
Risk factors for postoperative pain have been extensively investigated and include female sex, preoperative pain severity, younger age, surgical procedure, expected incision size, and psychological profile [4,5]. Recent studies have reported that postoperative pain following craniotomy is a persistent concern, and that new analgesic strategies are needed [6-8].
The primary purpose of brain tumor surgery is the precise diagnosis and total resection of the tumor if necessary. It is widely believed that patients do not experience intense pain following intracranial surgery due to the fact that surgical treatment of the brain parenchyma is not painful. However, it is common practice to infiltrate the scalp with lidocaine plus epinephrine to reduce postoperative pain after craniotomy [9]. A reasonable goal is to achieve relief of the patients' symptoms such as headache and neurologic deficits as well as postoperative pain following brain tumor surgery.
The incidence and severity of pain have rarely been assessed in Korean patients. We conducted an observational study of pain intensity and its' associated factors in Korean brain tumor patients undergoing elective craniotomy at a single institution.
MATERIALS AND METHODS
The inclusion criteria for the study were patients with newly diagnosed brain tumors, normal mental function, good performance, and oriented status who underwent elective craniotomy. The exclusion criteria were patients with psychological or severe medical diseases, those who had undergone previous brain surgery such as craniotomy for vascular disease, transsphenoidal approach, burr hole surgery, or reoperation for brain tumors. Patients with newly developed neurological deficits after craniotomy were excluded in order to strictly evaluate pain status. Patients who were not able to estimate the amount of pain because of decreased awareness were also excluded. Finally, patients with postoperative wound problems were excluded.
Between January 2010 and December 2011, 47 patients were enrolled according to the above criteria. We serially assessed postoperative pain in patients who underwent elective craniotomy for the treatment of various brain tumors. To measure the extent of pain, we used a visual analog scale (VAS), in which the score can range from 0 (no pain) to 10 (worst pain imaginable). Pain was categorized as 1-3 (mild pain), 4-6 (moderate pain), and 7-10 (severe pain) according to VAS assessment. In the operating room, scalp infiltrations with 1% lidocaine and 1 : 100,000 epinephrine were performed before the scalp incision. Perioperative opioid administration was left to the anesthesiologists' discretion in the recovery room. Postoperative analgesia was managed as follows: all patients received 75 mg intramuscular diclofenac sodium or 30 mg intravenous ketorolac tromethamine during 1 to 3 days after surgery. Acetaminophen and tramadol were orally administered afterword. Opioid was given for selected patients, when necessary.
The duration of the operation, the site of the surgery, the length of the wound, head fixation, surgical position, medical/social history, body mass index (BMI), and intensive care unit (ICU) stay were collected from each patient's medical records, and we searched for clinical factors associated with postoperative pain.
Statistical analysis
All statistical analyses were performed using SPSS (version 16.0, SPSS Inc., Chicago, IL, USA). Exploratory analyses of the demographic and medical data were performed by calculating the means and standard deviations for the continuous outcomes. Chi-square tests and independent 2-sample t-test were used to assess statistical differences between groups. Logistic regression analysis was used for univariate analysis for variables associated with postoperative pain scores. Statistical significance was accepted at a probability value of less than 0.05.
RESULTS
The study participants comprised of 22 males and 25 females with ages ranging from 18-76 years (mean age, 50.1 years). Patients' tumors included 21 meningiomas, 10 gliomas, 6 metastatic brain tumors, 4 acoustic neuromas, 3 hemangiomblastomas, and 3 granulomas. The median operating time was 358 minutes (range, 160-733). The median length of the surgical wound was 15.3 cm (range, 7-30).
Pain scores of 4 or greater are associated with moderate to severe pain [10]. We divided the patients into two groups (painful group versus tolerable group). The painful group included patients who had a VAS score of more than 3 during their hospital stay after the craniotomy. The tolerable group included patients who had a VAS score of 1 to 3 during their hospital stay. The characteristics of the two groups are summarized in Table 1. There were no differences between the two groups in terms of age, sex, location of surgery, history of diabetes, hypertension and smoking, BMI, or hospital stay. Univariate analysis revealed that age, sex, location, operating time, length of wound, head fixation, and perioperative administration of opioid were not associated with the intensity of postoperative pain.
Table 1.
Clinical characteristics of brain tumor patients who underwent elective craniotomy
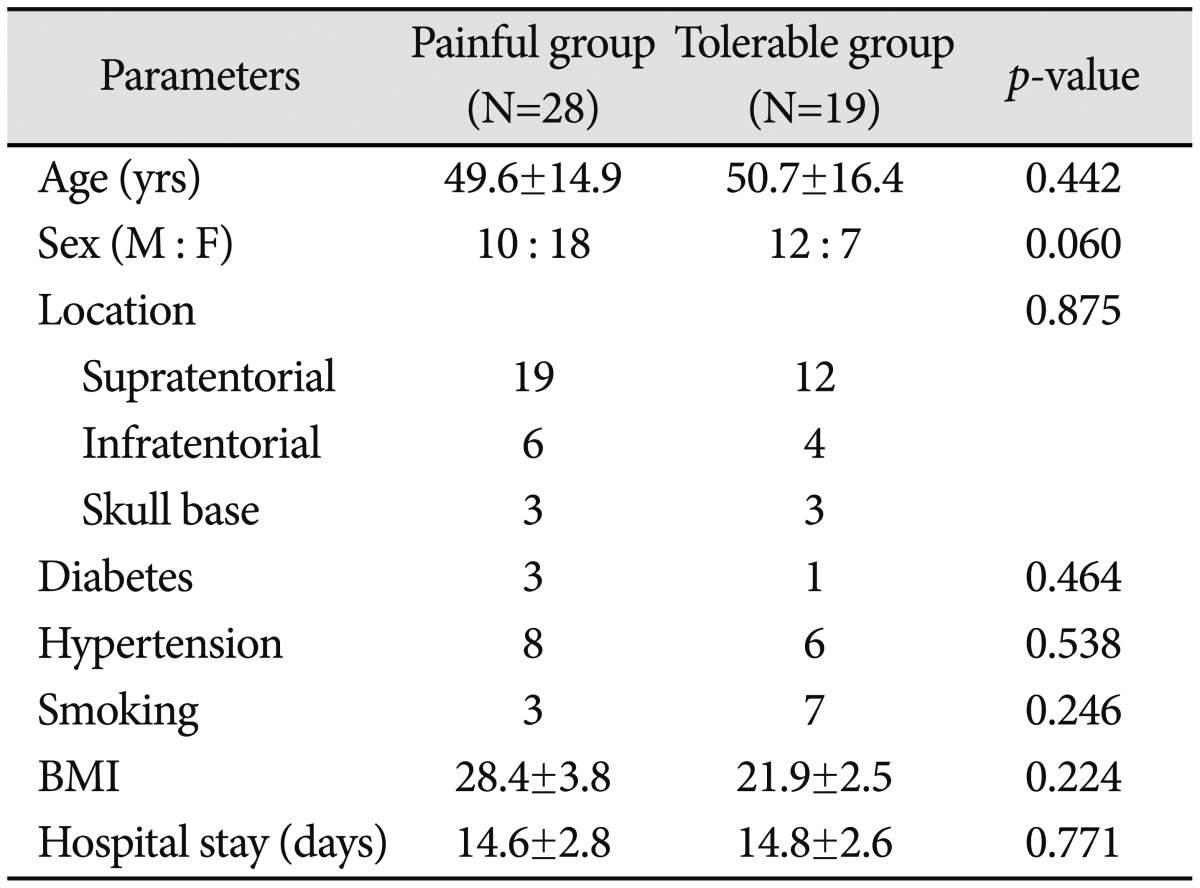
Data are presented as mean±standard deviation. BMI: body mass index
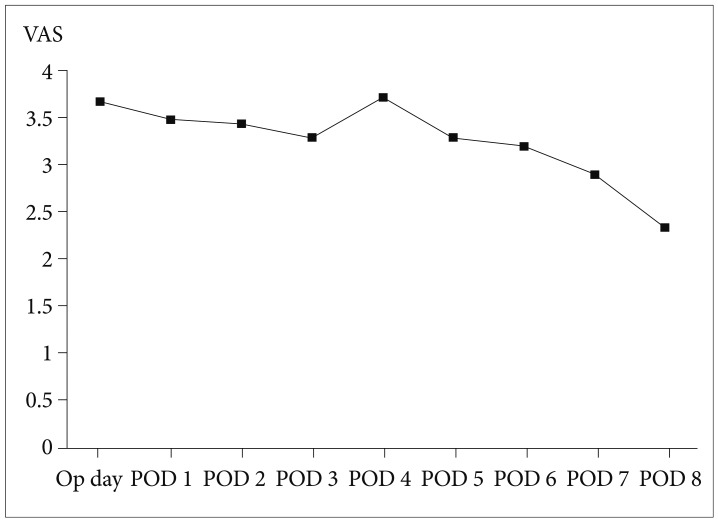
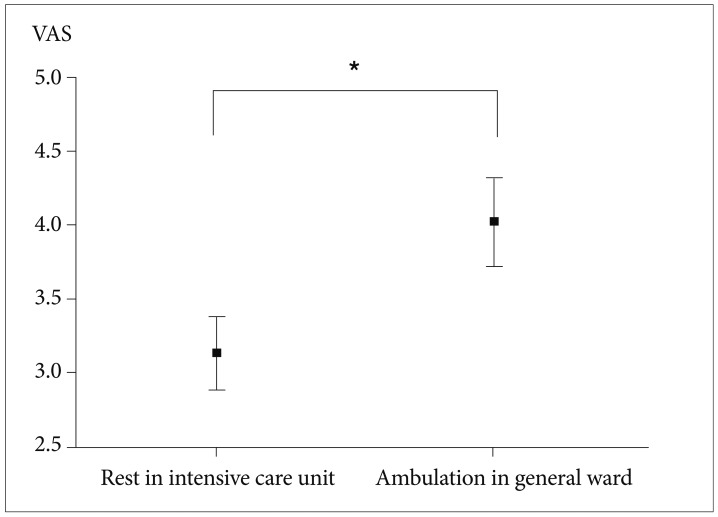
Daily assessment of VAS revealed the two peaks of postoperative pain on the operation day and the 4th postoperative day (Fig. 1). VAS of the operation day and 4th postoperative day was not statistically different from that of the other days. However, VAS of the operation day and 4th postoperative day was higher than that of the 8th postoperative day (p-value 0.009 and 0.016, respectively). Postoperative pain during ICU stay (except for operation day) was compared with that during the ambulation periods on the general wards. The intensity of pain during the ambulation period was higher than that during ICU stay (p-value 0.009) (Fig. 2).
Fig. 1.
Sequential changes of visual analog scales (VAS) after brain tumor surgery.
Fig. 2.
Higher visual analog scales (VAS) scores during ambulation in the general ward (4.02±0.3) than at rest in the ICU (3.13±0.25). Data are presented as mean±SE. *p<0.05. ICU: intensive care unit.
DISCUSSION
This study showed that brain tumor patients undergoing craniotomy had severe pain during the ambulation period rather than during the ICU stay. Most studies have only addressed the perioperative period, which averaged from the day of operation to 1 or 2 days postoperatively [11]. In Western studies, the reported prevalence of moderate to severe pain during the first 24 postoperative hours has ranged from 41 to 84% [12,13]. It has been found that pain is common for the first 2 days after a major elective intracranial surgery, with approximately two-thirds of patients reporting moderate to severe pain at some point during their hospitalization [14]. At our institution, patients with brain tumors are hospitalized for approximately 14 days. Therefore, we were able to serially assess the postoperative pain up to 14 days. On the 4th postoperative day, most patients begin to attempt to ambulate actively in the general wards. During this period, clinicians pay more attention to the neurological status of and wound care for patients rather than the subjective pain of neurologically and medically stable patients. According to the review of randomized double-blinded trials, scalp infiltrations with local anesthetic agents provide adequate analgesia in the first few postoperative hours, and cyclo-oxygenase type 2 inhibitors and morphine may cause a reduction in pain scores in the 24-hour study [15,16]. In our study, most patients received acetaminophen (usually, 900-1,950 mg) postoperatively. Alternatively, administration of muscle relaxants or anti-depressants is preferred for patients complaining of pain or discomfort during acetaminophen usage. There is a need for further study on pain management in the ambulation period following craniotomy.
We suggest that the postoperative pain of brain tumor patients undergoing craniotomy is an important and often neglected clinical problem that deserves greater attention from neurosurgeons in order to provide better and more appropriate treatment. Previous studies have revealed that age, sex, expected incision size, and surgical procedure have been shown to affect postoperative pain intensity [4,17]. In the current study, we found no significant differences in these previously known factors between the painful group and tolerable group. It has been reported that women seem to experience greater intensity of pain after orthopedic surgery [18]. Similarly, our study showed a trend toward greater pain reported by women, but it was not statistically significant.
One large retrospective study found that craniotomy was associated with less pain and analgesic consumption than surgery of the facial bones or the lumbar spine [1]. Interestingly, patients who underwent infratentorial procedures reported more severe pain compared to those who underwent supratentorial procedures. The amount of postoperative pain after intracranial surgery may depend on the extent of muscle damage associated with the operative approach [19]. Because surgical approaches to the posterior fossa often involve considerable muscle dissection, infratentorial procedures cause more pain compared to supratentorial procedures. Opioids have had a limited role in the analgesic management of patients who have undergone major intracranial surgery because of a presumed lack of need and a concern that opioids will affect the postoperative neurological examination [20,21]. Excessive administration of painkillers before the end of surgery may delay neurologic effect and may also exacerbate pain and alter the level of consciousness [22]. Perioperative opioid administration was left to the anesthesiologists' discretion at our institution. Therefore, it is important to take into consideration both the patients' comfort as well as the neurological objectives in managing postoperative pain after brain tumor surgery.
In this study, pain with movement in the general ward was aggravated compared with at rest in the ICU. The pain of brain tumor patients after ICU discharge is often inadequately treated. Pain following elective craniotomy for brain tumor removal is insufficiently managed, especially after discharge from the ICU. Thorough attention need to be paid to patients' pain throughout the entire hospital stay, especially just after discharge from the ICU.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Dunbar PJ, Visco E, Lam AM. Craniotomy procedures are associated with less analgesic requirements than other surgical procedures. Anesth Analg. 1999;88:335–340. doi: 10.1097/00000539-199902000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Kalkman CJ, Visser K, Moen J, Bonsel GJ, Grobbee DE, Moons KG. Preoperative prediction of severe postoperative pain. Pain. 2003;105:415–423. doi: 10.1016/S0304-3959(03)00252-5. [DOI] [PubMed] [Google Scholar]
- 3.Thomas T, Robinson C, Champion D, McKell M, Pell M. Prediction and assessment of the severity of post-operative pain and of satisfaction with management. Pain. 1998;75:177–185. doi: 10.1016/s0304-3959(97)00218-2. [DOI] [PubMed] [Google Scholar]
- 4.Morin C, Lund JP, Villarroel T, Clokie CM, Feine JS. Differences between the sexes in post-surgical pain. Pain. 2000;85:79–85. doi: 10.1016/s0304-3959(99)00248-1. [DOI] [PubMed] [Google Scholar]
- 5.Scott LE, Clum GA, Peoples JB. Preoperative predictors of postoperative pain. Pain. 1983;15:283–293. doi: 10.1016/0304-3959(83)90063-5. [DOI] [PubMed] [Google Scholar]
- 6.Rahimi SY, Vender JR, Macomson SD, French A, Smith JR, Alleyne CH., Jr Postoperative pain management after craniotomy: evaluation and cost analysis. Neurosurgery. 2006;59:852–857. doi: 10.1227/01.NEU.0000232646.35678.D8. discussion 857. [DOI] [PubMed] [Google Scholar]
- 7.Roberts GC. Post-craniotomy analgesia: current practices in British neurosurgical centres--a survey of post-craniotomy analgesic practices. Eur J Anaesthesiol. 2005;22:328–332. doi: 10.1017/s0265021505000554. [DOI] [PubMed] [Google Scholar]
- 8.Thibault M, Girard F, Moumdjian R, Chouinard P, Boudreault D, Ruel M. Craniotomy site influences postoperative pain following neurosurgical procedures: a retrospective study. Can J Anaesth. 2007;54:544–548. doi: 10.1007/BF03022318. [DOI] [PubMed] [Google Scholar]
- 9.Law-Koune JD, Szekely B, Fermanian C, Peuch C, Liu N, Fischler M. Scalp infiltration with bupivacaine plus epinephrine or plain ropivacaine reduces postoperative pain after supratentorial craniotomy. J Neurosurg Anesthesiol. 2005;17:139–143. doi: 10.1097/01.ana.0000171730.41008.da. [DOI] [PubMed] [Google Scholar]
- 10.Jensen MP, Smith DG, Ehde DM, Robinsin LR. Pain site and the effects of amputation pain: further clarification of the meaning of mild, moderate, and severe pain. Pain. 2001;91:317–322. doi: 10.1016/S0304-3959(00)00459-0. [DOI] [PubMed] [Google Scholar]
- 11.Klimek M, Ubben JF, Ammann J, Borner U, Klein J, Verbrugge SJ. Pain in neurosurgically treated patients: a prospective observational study. J Neurosurg. 2006;104:350–359. doi: 10.3171/jns.2006.104.3.350. [DOI] [PubMed] [Google Scholar]
- 12.De Benedittis G, Lorenzetti A, Migliore M, Spagnoli D, Tiberio F, Villani RM. Postoperative pain in neurosurgery: a pilot study in brain surgery. Neurosurgery. 1996;38:466–469. doi: 10.1097/00006123-199603000-00008. discussion 469-70. [DOI] [PubMed] [Google Scholar]
- 13.Quiney N, Cooper R, Stoneham M, Walters F. Pain after craniotomy. A time for reappraisal? Br J Neurosurg. 1996;10:295–299. doi: 10.1080/02688699650040179. [DOI] [PubMed] [Google Scholar]
- 14.Gottschalk A, Berkow LC, Stevens RD, et al. Prospective evaluation of pain and analgesic use following major elective intracranial surgery. J Neurosurg. 2007;106:210–216. doi: 10.3171/jns.2007.106.2.210. [DOI] [PubMed] [Google Scholar]
- 15.Hansen MS, Brennum J, Moltke FB, Dahl JB. Pain treatment after craniotomy: where is the (procedure-specific) evidence? A qualitative systematic review. Eur J Anaesthesiol. 2011;28:821–829. doi: 10.1097/EJA.0b013e32834a0255. [DOI] [PubMed] [Google Scholar]
- 16.Saringcarinkul A, Boonsri S. Effect of scalp infiltration on postoperative pain relief in elective supratentorial craniotomy with 0.5% bupivacaine with adrenaline 1:400,000. J Med Assoc Thai. 2008;91:1518–1523. [PubMed] [Google Scholar]
- 17.Block AR, Ohnmeiss DD, Guyer RD, Rashbaum RF, Hochschuler SH. The use of presurgical psychological screening to predict the outcome of spine surgery. Spine J. 2001;1:274–282. doi: 10.1016/s1529-9430(01)00054-7. [DOI] [PubMed] [Google Scholar]
- 18.Taenzer AH, Clark C, Curry CS. Gender affects report of pain and function after arthroscopic anterior cruciate ligament reconstruction. Anesthesiology. 2000;93:670–675. doi: 10.1097/00000542-200009000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Talke PO, Gelb AW. Postcraniotomy pain remains a real headache! Eur J Anaesthesiol. 2005;22:325–327. doi: 10.1017/s0265021505000542. [DOI] [PubMed] [Google Scholar]
- 20.Stoneham MD, Walters FJ. Post-operative analgesia for craniotomy patients: current attitudes among neuroanaesthetists. Eur J Anaesthesiol. 1995;12:571–575. [PubMed] [Google Scholar]
- 21.Verchère E, Grenier B, Mesli A, Siao D, Sesay M, Maurette P. Postoperative pain management after supratentorial craniotomy. J Neurosurg Anesthesiol. 2002;14:96–101. doi: 10.1097/00008506-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Guignard B, Bossard AE, Coste C, et al. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000;93:409–417. doi: 10.1097/00000542-200008000-00019. [DOI] [PubMed] [Google Scholar]