Abstract
High-throughput screening and subsequent hit optimization identified 1-piperidinylbenzimidazoles, exemplified by compound 1, as TRPV4 inhibitors. Lead optimization identified potent TRPV4 blocker 19, which has good target activity and pharmacokinetic properties. Inhibitor 19 was then profiled in an in vivo rat model, demonstrating its ability to inhibit TRPV4-mediated pulmonary edema.
Keywords: ion channel, calcium channel, vanilloid receptor, transient receptor potential, TRPV4, heart failure, pulmonary edema, benzimidazole
TRPV4 (transient receptor potential vanilloid receptor 4) is a member of the vanilloid family of transient receptor potential (TRP) ligand-gated ion channels. TRPV4 channels are tetrameric with each monomeric unit comprising six trans-membrane domains. The pore region, located between TM5 and TM6, mediates Ca2+ and Na+ entry across cell membranes in response to pressure, stretch, temperature, hypotonicity, and ligand activation.1
TRPV4 is expressed in many organs including lung, kidney, brain, bladder, liver, choclea, retina, heart, and the vasculature.2,2b Its abundant expression in vascular endothelium and sensitivity to pressure and stretch have prompted studies to determine if TRPV4 is implicated in regulating lung permeability and the formation of pulmonary edema. TRPV4 was linked to elevated pulmonary vascular pressure-mediated Ca2+ uptake by lung endothelium and subsequent acute lung injury.3−3c Disruption of endothelial integrity at the alveolar septal barrier in the lung is a hallmark of acute lung injury in both respiratory distress syndrome and lung congestion associated with heart failure. In heart failure patients, elevated pulmonary venous pressures lead to lung congestion, resulting in fatigue and shortness of breath (dyspnea).4,4b
Direct implication of TRPV4 activity in lung injury was accomplished by studying the effects of TRPV4 agonists on lung permeability in rats and wild-type and TRPV4 knockout mice.5 4αPDD and 5,6-EET, both selective TRPV4 agonists, were found to increase lung permeability in a dose-dependent manner in isolated rat lungs. This agonist effect was blocked in rats pretreated with Ruthenium Red, a nonselective TRP antagonist. Agonist-induced increases in lung permeability were observed in wild-type mice but notably absent in TRPV4 knockout mice.
Similar studies were conducted in mouse models evaluating the effects of heightened pulmonary venous pressure, as occurs during heart failure.3a Isolated lung preparations from wild-type mice showed significant increases in lung permeability and subsequent pulmonary edema in response to elevated pulmonary venous pressures. This response was substantially attenuated in TRPV4 knockout mice and wild-type mice pretreated with the TRPV4 antagonist Ruthenium Red. These studies make a compelling argument for the discovery and development of selective TRPV4 antagonists as a treatment for lung congestion in the heart failure patient.
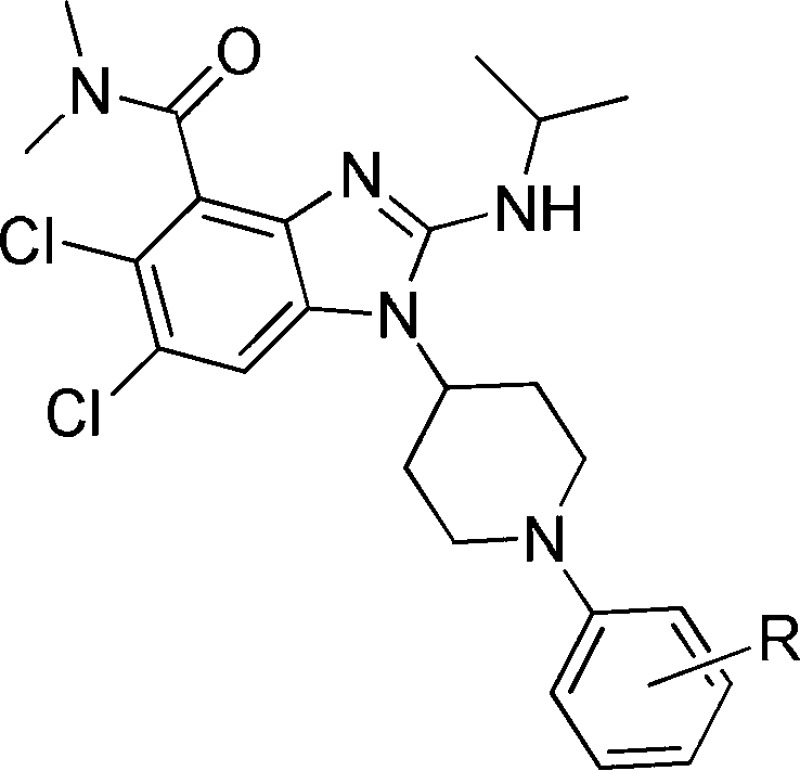
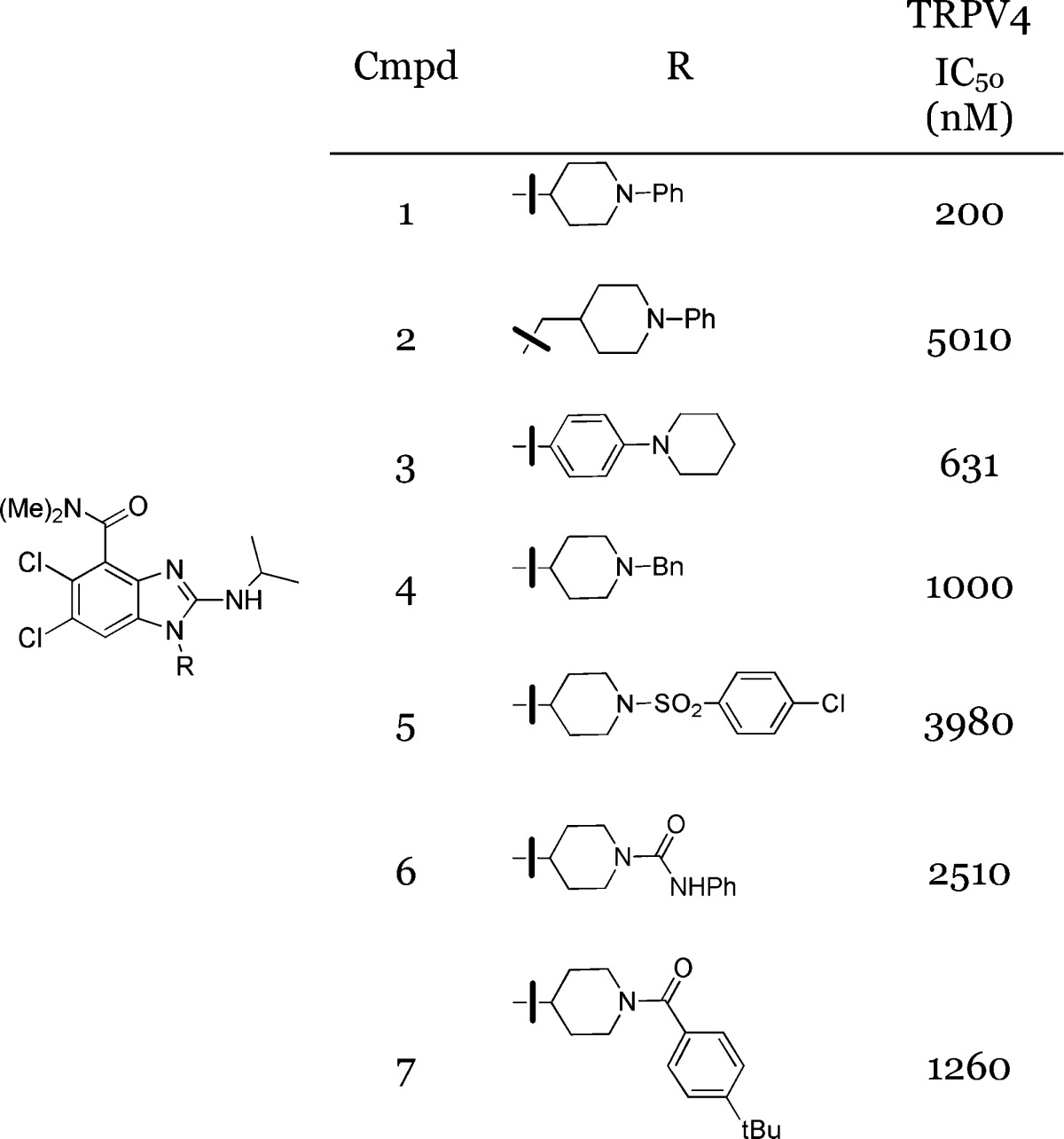
Previously, our group identified a series of orally active quinoline carboxamide TRPV4 antagonists capable of attenuating pulmonary edema in heart failure models.6−6c To further strengthen this proposed mechanism of action, we sought to replicate the prior observation of protection against pulmonary edema via TRPV4 blockade with a novel chemotype. To this end, 1-(4-piperidinyl)-benzimidazoles were identified from early hit-to-lead chemistry as having promising TRPV4 antagonist activity (Table 1). In addition to its potency, the piperidine moiety provided a handle for robust chemical tractability. A survey of standard amine functionalization realized that sulfonamides, ureas, and amides had low micromolar activity (5–7), while the N-phenylpiperidine, 1, was identified as being the most potent TRPV4 inhibitor in the series. Interestingly, analogue 3 was synthesized to evaluate subtle changes in amine disposition and showed a modest decrease (∼3-fold) in TRPV4 potency. Given these results, additional N-arylpiperidines based on lead compound 1 were evaluated.
Table 1. Lead Identification of Benzimidazole 1(7).
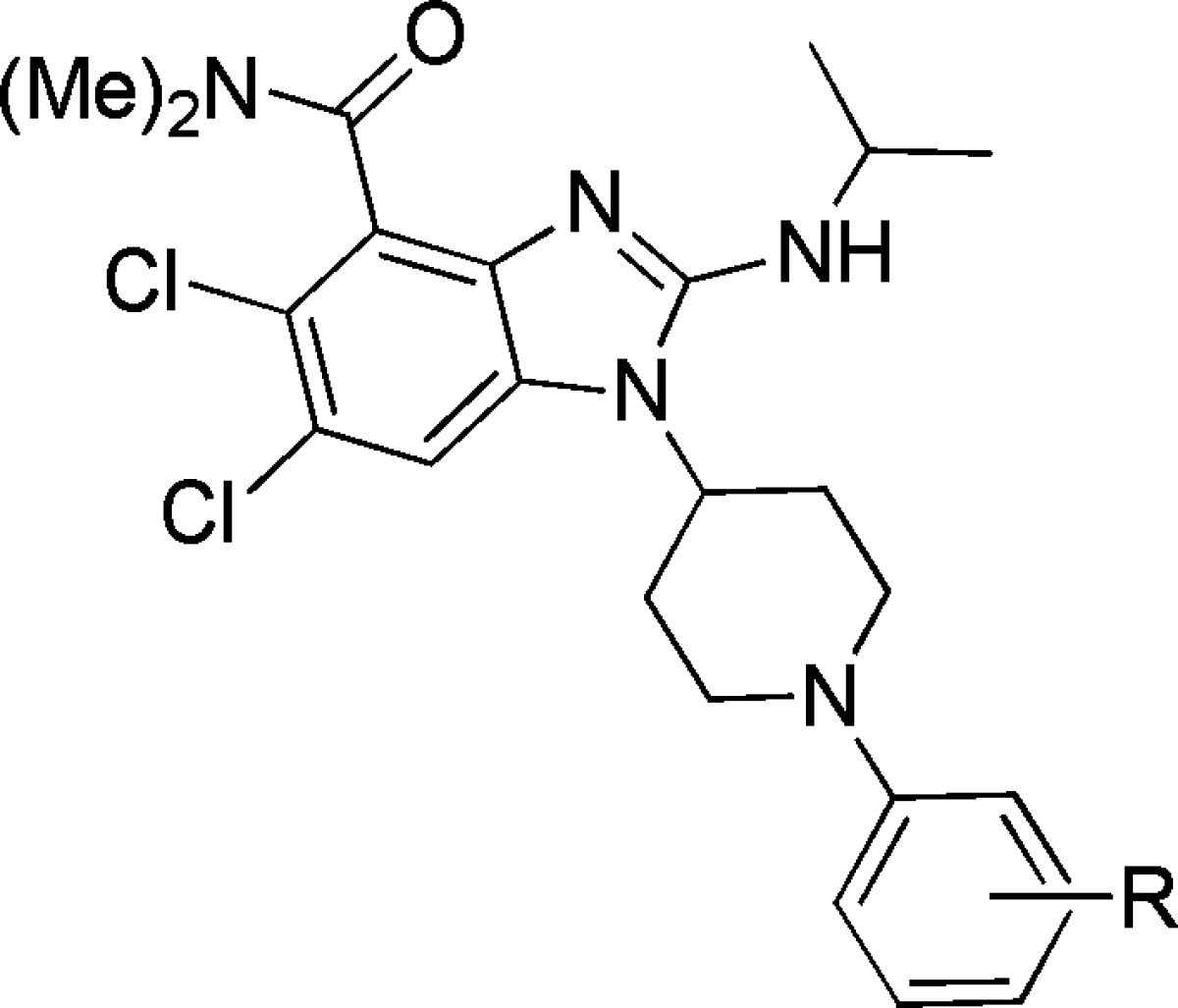
Additional structure–activity relationship (SAR) focused on functionalization of the 2-amino group and the N,N-dimethylamide. The isopropylamino moiety was found to be optimal in the 2-position of the benzimidazole with amine moieties larger than isopropylamine having a substantial loss in TRPV4 potency. A survey of alternative amide group substitution also revealed that amides other than N,N-dimethylamide were not tolerated for TRPV4 activity. As a result, these residues were conserved with further optimization focused on surveying SAR at the N-arylpiperidine.
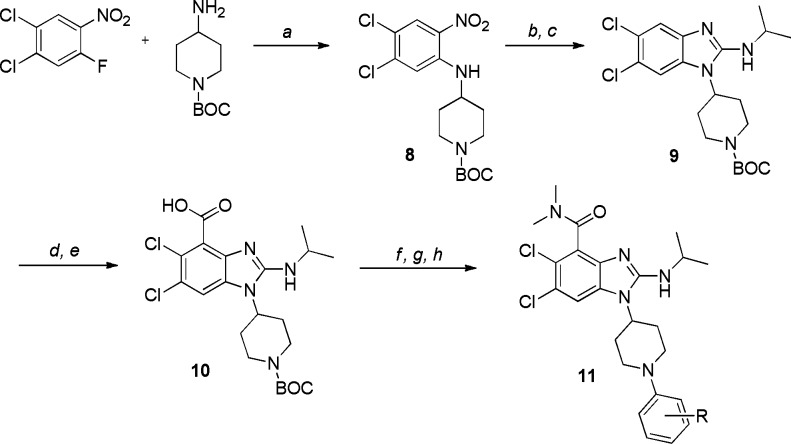
Compounds were synthesized by first preparing 2-nitroaniline, 8, by SNAr2 addition of 1-tert-butoxycarbonyl (BOC)-4-aminopiperidine into the requisite 2-fluoronitrobenzene (Scheme 1). An iron reduction of the nitro group followed by condensation of the phenylenediamine intermediate with isopropylisothiocyanate provided benzimidazole 9. The N,N-dimethylamide group was installed via selective deprotonation at the C4-position of the benzimidazole followed by alkylation of the aryl lithium with ethylchloroformate. The resulting ethyl ester was subject to hydrolysis conditions to afford acid 10. Subsequent amide coupling with dimethylamine followed by BOC deprotection yielded the piperidine substrate required for surveying the N-aryl moiety. This was accomplished through a palladium-catalyzed coupling of an arylbromide to afford the N-arylpiperidine generically exemplified by 11.
Scheme 1. Synthetic Route.
Reagents and conditions: (a) Na2CO3, MeCN, 25 °C. (b) Fe, NH4Cl, EtOH/H2O, 70 °C. (c) Isopropylisothiocyanate, pyridine, 70 °C, then EDC. (d) sec-BuLi, THF, −78 °C, then ClCO2Et. (e) KOH, THF/EtOH/H2O, 70 °C. (f) Me2NH, T3P, (iPr)2NEt, DCM, 0 °C. (g) 1 N HCl, DCM, 25 °C. (h) Aryl bromide, Pd(OAc)2, (ortho-biphenyl)(tBu)2P, Cs2CO3, 1,4-dioxane, 100 °C.
A survey of N-arylpiperidine groups indicated that a wide variety of substitution was tolerated for TRPV4 activity (Table 2). In addition, favorable pharmacokinetic properties could be realized as exemplified by early analogue 12. It became evident that incorporating large hydrophobic groups in the aryl group’s para-position achieved the highest levels of TRPV4 potency, but this often resulted in decreased oral exposure in the rat as exemplified by analogue 15. Interestingly, ester 17 was devised in an effort to maintain the potency of tert-butyl analogue 14 and incorporate a synthetic handle for further functionalization and was found to have excellent potency. Unfortunately, this compound proved to be highly unstable in vivo in the rat, with no quantifiable concentrations observed following either iv or oral administration. Analysis of plasma samples did reveal the presence of the corresponding carboxylic acid, 18. Believing ester hydrolysis to be the principle clearance mechanism, carboxylic acid 18 was surveyed and found to have no activity against TRPV4. We hypothesized that the improved potency of ester 17 was due to the incorporation of a hydrogen bond acceptor and reasoned that the combination of the gem-dimethyl group and a metabolically stable H-bond acceptor would lead to an optimized inhibitor. To this end, nitriles 19 and 20 were surveyed and found to have excellent in vitro potency with acceptable rat PK profiles for evaluating TRPV4 activity in vivo.
Table 2. Potency and PK Profiles for N-Aryl Piperidine Analogues11.
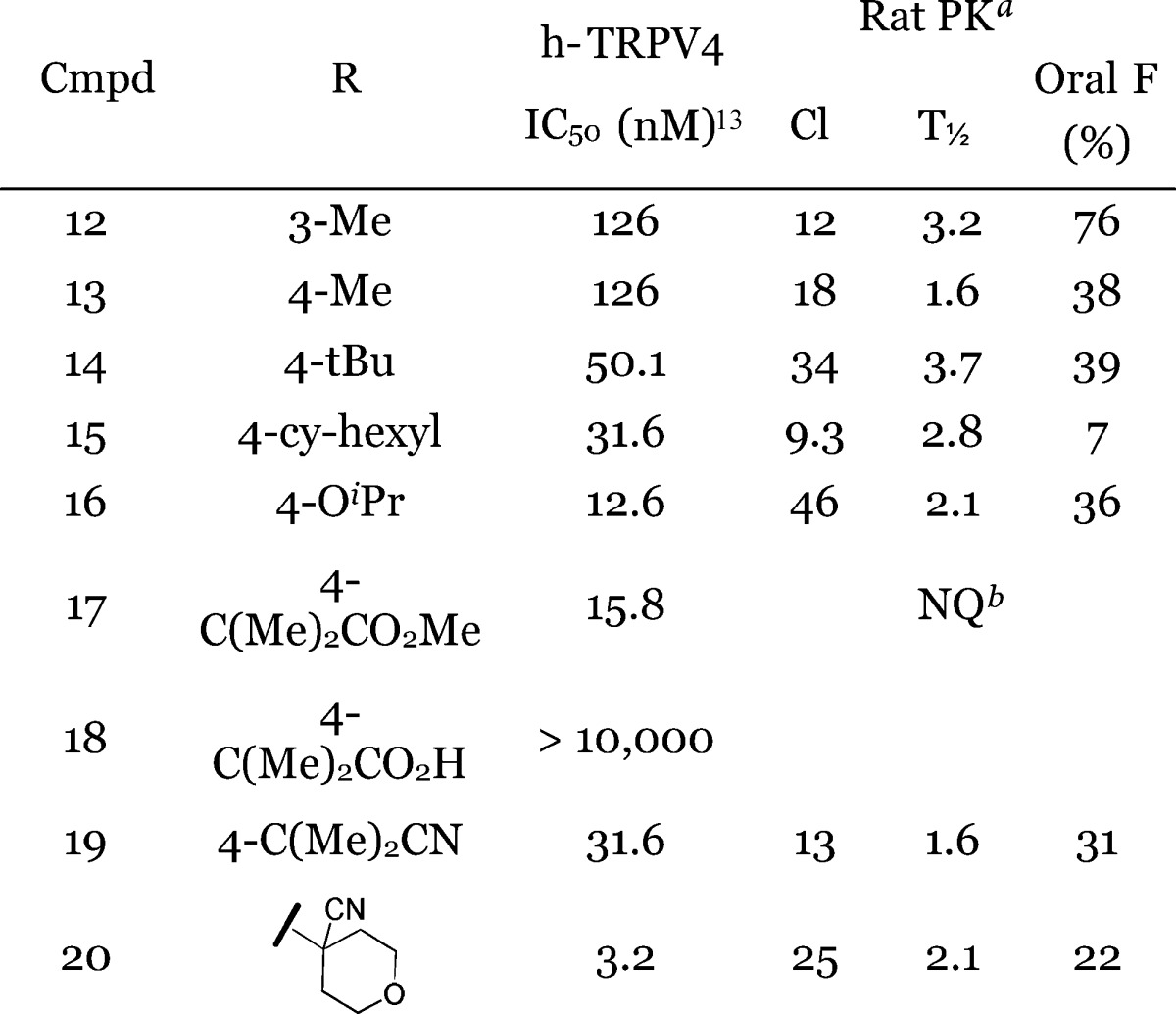
Clearance measurements derived from iv leg in units of mL/min/kg; T1/2 derived from oral leg measured in hours.
Not quatifiable: target compounds were not observed at detectable levels in isolated rat plasma samples.
In an effort to establish a connection between TRPV4 activity and pulmonary edema, a rat in vivo model was developed, whereby lung wet weights and mean arterial pressure are measured with iv administration of a selective TRPV4 agonist, GSK1016790A.8,8b Thirty minutes prior to challenge with the agonist, animals were pretreated with vehicle, 3 or 10 mg/kg iv of TRPV4 inhibitor 19. GSK1016790A in the vehicle-treated group demonstrated a dramatic dose-dependent decrease in mean arterial pressure (MAP) and a significant increase in pulmonary edema (as assessed by wet lung weight/body weight ratio) (Figure 1). Nitrile 19 was evaluated in this study as it represents a good tool compound; typical to this chemical series, its antagonist activity in the rat (IC50 = 32 nM) is identical to its measured human activity and does not have any TRPV4 agonist activity in either species. In addition, ion channel selectivity for 19 is excellent with no observed activity at concentrations greater than 10 μM for the human Ca v1.2 (L-type), K v1.5, or Na v1.5 ion channels.9
Figure 1.
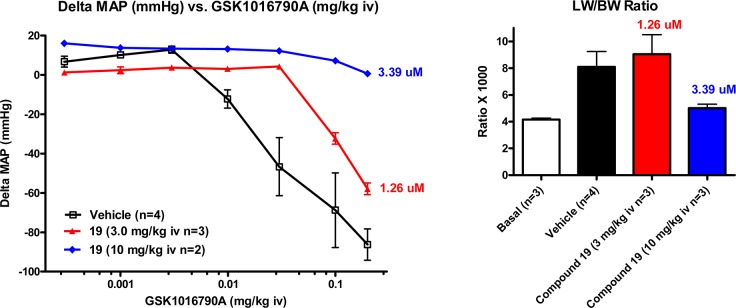
Effect of TRPV4 agonists and antagonists on rat MAP and lung wet weights.11
Nitrile 19 dosed at 3 and 10 mg/kg providing plasma concentrations of 1.26 (42 nM free) and 3.39 μM (112 nM free), respectively.10 A dose-dependent decrease in agonist-induced MAP decrease was observed with complete blockade of the agonist affect with 10 mg/kg of compound 19. No effect on MAP was observed in the pretreatment phase prior to agonist challenge. While no effect on the lung/body weight ratio was observed at 3 mg/kg, a significant decrease in wet lung weight was observed at the 10 mg/kg dose as compared to vehicle-treated rats. These results indicate that compound 19 is active in vivo and able to inhibit TRPV4 activity, consistent with prior observations.6−6c
In conclusion, a novel series of small molecules have been identified with potent TRPV4 antagonist activity and good ion channel selectivity. In addition, many compounds in this series demonstrate good DMPK properties, making this series useful in studying the pharmacology of TRPV4 activity in vivo. To this end, compound 19 demonstrated protection against TRPV4-mediated pulmonary edema in the rat. These preliminary results showing in vivo activity with a second chemical class of TRPV4 antagonists compliment our previous studies.6−6c Together, this body of data adds weight to the evidence that lung permeability is closely linked to TRPV4 activity and that future TRPV4 antagonists have the potential to alleviate respiratory distress in patients suffering from heart failure.
Glossary
Abbreviations
- TRPV4
transient receptor potential vanilloid receptor 4
- SAR
structure–activity relationship
- BOC
tert-butoxycarbonyl
- T3P
1-propanephosphonic acid cyclic anhydride
- MAP
mean arterial pressure
- hERG
human ether-a-go-go related gene potassium channel
- LW/BW ratio
wet lung weight/body weight ratio
Supporting Information Available
Synthetic procedures, assay details, and procedures for pharmacokinetic and pharmacodynamic studies. This material is available free of charge via the Internet at http://pubs.acs.org.
Author Present Address
⊥ Chimie ParisTech, 11, rue Pierre et Marie Curie, 75231 Paris, France.
Author Present Address
# Department of Biology, The Pennsylvania State University, University Park, Pennsylvania 16802, United States.
The authors declare no competing financial interest.
Supplementary Material
References
- Everaerts W.; Nilius B.; Owsianik G. The vanilloid transient receptor potential channel TRPV4: From structure to disease. Prog. Biophys. Mol. Biol. 2010, 103, 2–17. [DOI] [PubMed] [Google Scholar]
- Vincent F.; Duncton A. J. TRPV4 Agonists and Antagonists. Curr. Top. Med. Chem. 2011, 11172216–2226. [DOI] [PubMed] [Google Scholar]
- Bakthavatchalam R.; Kimball S. D. Modulators of Transient Receptor Potential Ion Channels. Annu. Rep. Med. Chem. 2010, 45, 37–53and references therein. [Google Scholar]
- Jian M.-Y.; King J. A.; Al-Mehdi A.-B.; Liedtke W.; Townsley M. I. High Vascular Pressure-Induced Lung Injury Requires P450 Epoxygenase-Dependent Activation of TRPV4. Am. J. Respir. Cell Mol. Biol. 2008, 38, 386–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin J.; Hoffmann J.; Kaestle S. M.; Neye N.; Wang L.; Baeurle J.; Liedtke W.; Wu S.; Kuppe H.; Pries A. R.; Kuebler W. M. Negative-feedback loop attenuates hydrostatic lung edema via a cGMP-dependent regulation of transient receptor potential Vanilloid 4. Circ. Res. 2008, 103, 966–974. [DOI] [PubMed] [Google Scholar]
- Kuebler W. M.; Ying X.; Bhattacharya J. Pressure-induced endothelial Ca2+ oscillations in lung capillaries. Am. J. Physiol. Lung Cell Mol. Physiol. 2002, 282, L917–L923. [DOI] [PubMed] [Google Scholar]
- Bernard G. R.; Artigas A.; Brigham K. L.; Carlet J.; Falke K.; Hudson L.; Lamy M.; LeGall J. R.; Morris A.; Spragg R. The American European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am. J. Respir. Crit. Care Med. 1994, 149, 818–824. [DOI] [PubMed] [Google Scholar]
- Matthay M. A.; Zimmerman G. A.; Esmon C.; Bhattacharya J.; Coller B.; Doerschuk C. M.; Floros J.; Gimbrone M. A. Jr.; Hoffman E.; Hubmayr R. D.; Leppert M.; Matalon S.; Munford R.; Parsons P.; Slutsky A. S.; Tracey K. J.; Ward P.; Gail D. B.; Harabin A. L. Future research directions in acute lung injury: Summary of National Heart, Lung, and Blood Institute working group. Am. J. Respir. Crit. Care Med. 2003, 167, 1027–1035. [DOI] [PubMed] [Google Scholar]
- Alvarez D. F.; King J. A.; Weber D.; Addison E.; Liedtke W.; Townsley M. I. Transient Receptor Potential Vanilloid 4-Mediated Disruption of the Alveolar Septal Barrier: A Novel Mechanism of Acute Lung Injury. Circ. Res. 2006, 99, 988–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorneloe K. S.; Cheung M.; Bao W.; Alsaid H.; Lenhard S.; Jian M.-Y.; Costell M.; Maniscalco-Hauk K.; Krawiec J. A.; Olzinski A.; Gordon E.; Lozinskaya I.; Elefante L.; Qin P.; Matasic D. S.; James C.; Tunstead J.; Donovan B.; Kallal L.; Waszkiewicz A.; Vaidya K.; Davenport E. A.; Larkin J.; Burgert M.; Casillas L. N.; Marquis R. W.; Ye G.; Eidam H. S.; Goodman K. B.; Toomey J. R.; Roethke T. J.; Jucker B. M.; Schnackenberg C. G.; Townsley M. I.; Lepore J. J.; Willette R. N. An Orally Active TRPV4 Channel Blocker Prevents and Resolves Pulmonary Edema Induced by Heart Failure. Sci. Transl. Med. 2012, 4, 159ra148. [DOI] [PubMed] [Google Scholar]
- Brooks C. A.; Cheung M.; Eidam H. S.; Fox R. M.; Hilfiker M. A.; Manas E. S.; Ye G.. 4-Quinolinecarboxamide derivatives as TRPV4 antagonists and their preparation and use for the treatment of diseases. WO 2011/119704 A1, September 29, 2011.
- Brooks C. A.; Cheung M.; Eidam H. S.; Fox R. M.; Hilfiker M. A.; Manas E. S.; Ye G.. 4-Quinolinecarboxamide derivatives as TRPV4 antagonists and their preparation and use for the treatment of diseases. WO 2011/119701 A1, September 29, 2011.
- TRPV4 potency was determined by measuring the blockade of agonist GSK634775-induced calcium immobilization through human, recombinant TRPV4 channels in HEK cells on a fluorescent light imaging plate reader (FLIPR). The reported potencies are an average of at least two measurements with a SEM ± 0.1 for the pIC50. Assay details can be found in the Supporting Information.
- Willette R. N.; Bao W.; Nerurkar S.; Yue T-l.; Doe C. P.; Stankus G.; Turner G. H.; Ju H.; Thomas H.; Fishman C. E.; Sulpizio A.; Behm D. J.; Hoffman S.; Lin Z.; Lozinskaya I.; Cassillas L. N.; Lin M.; Trout R. E. L.; Bartholomew J. V.; Thorneloe K.; Lashinger E. S. R.; Figueroa D. J.; Marquis R.; Xu X. Systematic Activation of the Trasient Receptor Potential Vanilloid Subtype 4 Channel Causes Endothelial Failure and Circulatory Collapse: Part 2. J. Pharmacol. Exp. Ther. 2008, 326, 443. [DOI] [PubMed] [Google Scholar]
- Mendoza S. A.; Fang J.; Gutterman D. D.; Wilcox D. A.; Bubolz A. H.; Li R.; Suzuki M.; Zhang D. X. TRPV4-mediated endothelial Ca2+ influx and vasodilation in response to shear stress. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Details for the Ca v1.2 (L-type), K v1.5, Na v1.5, and hERG ion channel selectivity assays can be found in the Supporting Information.
- Plasma protein binding was measured for compound 19 and found to be 4.4 and 3.3% unbound in human and rat plasmas, respectively.
- All animal studies were conducted in accordance with the GSK Policy on the Care, Welfare, and Treatment of Laboratory Animals and were reviewed by the Institutional Animal Care and Use Committee at GSK.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.