Abstract
Objective To identify whether changes in pubertal status and self-efficacy for diabetes management are associated with longitudinal declines in parental responsibility for diabetes, and to determine whether these factors moderate associations between declining parental responsibility and deteriorating adherence across adolescence. Methods Adolescents (N = 252; 53.6% females) with type 1 diabetes, mothers, and 188 fathers participated in a 2.5-year longitudinal study. Self-reports of pubertal status, adolescent efficacy, parental responsibility, and adherence were completed every 6 months (6 time points). Results Latent growth curve modeling revealed that longitudinal increases in efficacy and pubertal maturation were uniquely associated with longitudinal declines in parental responsibility. Declines in parental responsibility were related to deterioration in adherence especially when adolescents did not report concomitant growth in self-efficacy. Conclusions Transfer of responsibility for diabetes management across adolescence may be more optimal when adolescents’ increased independence is titrated to their changing self-efficacy beliefs.
Keywords: adherence, adolescents, longitudinal research, parenting, puberty, self-efficacy, type 1 diabetes
Type 1 diabetes involves a demanding treatment regimen that is difficult to maintain during adolescence. Families must coordinate multiple daily behaviors (i.e., insulin injections, blood glucose monitoring, diet, exercise) to normalize blood glucose levels (Silverstein et al., 2005). Adherence declines across adolescence (King, Berg, Butner, Butler, & Wiebe, 2013), increasing one’s risk for poor metabolic control and serious long-term complications (Hood, Peterson, Rohan, & Drotar, 2009). Such difficulties may occur because adolescents assume responsibility for diabetes management while they are still developing the skills necessary to manage diabetes independently (Anderson, Brackett, Ho, & Laffel, 1999; Hanna & Decker, 2010; Wysocki et al., 1996). Diabetes management is better when transfer of responsibility matches the youth’s psychosocial maturity (Wysocki et al., 1996, 2006), but other factors may be associated with declines in parental responsibility for diabetes. In cross-sectional studies, broad developmental factors such as age and pubertal status are strongly associated with lower parental responsibility (Hanna & Decker, 2010; Palmer et al., 2004, 2009), but are imperfect markers of the skills necessary for independent diabetes management (Holmes et al., 2006). Few longitudinal studies of the transfer of responsibility for diabetes exist, and those that do have focused on parental responsibility as a direct predictor of diabetes management, rather than considering it in the multifaceted developmental context in which it occurs. The present study explored the developmental processes associated with longitudinal declines in parental responsibility, and examined whether declining parental responsibility across adolescence was associated with poorer adherence primarily when it was not matched to key aspects of the adolescent’s development.
Parental responsibility decreases with age, but its association with diabetes self-management has been inconsistent. Both cross-sectional (Palmer et al., 2009; Wiebe et al., 2005) and longitudinal data (Anderson et al., 1999; Ingerski, Anderson, Dolan, & Hood, 2010) reveal that parental responsibility decreases across adolescence at the same time that adherence (e.g., King et al., 2013) and metabolic control (Helgeson, Siminerio, Escobar, & Becker, 2009) often deteriorate. Nevertheless, there is mixed evidence that decreases in parental responsibility predict poorer diabetes management. Some studies report lower parental responsibility is associated with poorer adherence (Hsin, La Greca, Valenzuela, Moine, & Delamater, 2010; Ingerski et al., 2010; Ott, Greening, Palardy, Holderby, & DeBell, 2000; Vesco et al., 2010) and metabolic control (Ingerski et al., 2010), others report no association with adherence (Helgeson, Reynolds, Siminerio, Escobar, & Becker, 2008; Holmes et al., 2006; Miller & Drotar, 2003; Palmer et al., 2009; Wiebe et al., 2005) or metabolic control (Helgeson et al., 2008; Hsin et al., 2010; Miller & Drotar, 2003; Palmer et al., 2009; Vesco et al., 2010; Wiebe et al., 2005), and still others report associations with better metabolic control (Cameron et al., 2008; Vesco et al., 2010). Thus, although current treatment standards recommend parents remain involved and only gradually transfer responsibility (Silverstein et al., 2005), support for a direct relationship between lower parental responsibility for diabetes and poorer diabetes management is mixed.
One reason for this inconsistency is that transfer of responsibility for diabetes may be problematic primarily if it occurs prematurely before adolescents are capable of managing diabetes independently. Transfer of responsibility may be optimal when it is attuned to adolescents’ self-efficacy for diabetes management, rather than when it is cued by broad developmental factors such as pubertal status or age (Hanna & Decker, 2010; Holmes et al., 2006). Self-efficacy or the belief in one’s ability to manage diabetes in challenging situations is an important longitudinal predictor of declines in adherence across adolescence (King et al., 2013). Palmer et al. (2009) specifically found self-efficacy moderated cross-sectional associations between parental responsibility and diabetes management, indicating that lower parental responsibility was associated with poorer management when adolescents had lower self-efficacy beliefs. This suggests that self-efficacy beliefs may be an important indicator of readiness to assume responsibility for diabetes. Furthermore, because self-efficacy reflects a sense of mastery that results from experience (Bandura, 1982; Ott et al., 2000), growth in self-efficacy is likely to occur as adolescents gain experience in managing diabetes more independently and such increases in self-efficacy across time may be an important marker of success in the transfer of responsibility from parent to adolescent.
Pubertal maturation is also occurring across adolescence, and has been associated with adolescents’ greater independence in diabetes management (Holmes et al., 2006; Palmer et al., 2004, 2009). Unfortunately, however, puberty disrupts the metabolic system, making it more difficult to achieve glycemic control. Puberty also activates the neural substrates of social-emotional processing that enhance sensation- and reward-seeking, and may play a role in adolescent risk behaviors (Steinberg, 2008). Such developments may be problematic for youth with diabetes, who often need to resist temptation and maintain self-control to manage their illness (e.g., Hughes, Berg, & Wiebe, 2012). Thus, transfer of responsibility that occurs in the context of more rapid pubertal maturation may be problematic because independent management is occurring at a time when adolescents need additional support.
The present longitudinal study examined whether pubertal maturation and self-efficacy beliefs are differentially effective cues for transferring responsibility for diabetes from parent to adolescent. Aim 1 examined whether longitudinal trajectories of parental responsibility across adolescence covaried with trajectories of adolescent efficacy for diabetes management and pubertal maturation. Each variable has been associated with lower levels of parental responsibility in cross-sectional studies (Holmes et al., 2006; Kaugars, Kichler, & Alemzadeh, 2011; Palmer et al., 2004, 2009), but has not been examined longitudinally. By examining whether rates of decline in parental responsibility are associated with rates of increase in each variable, we provide a more compelling test of the hypothesized developmental process. We expected that parental responsibility would decline across adolescence, and that the rate of decline would be associated with the rate of growth in each variable. Aim 2 examined whether declines in parental responsibility were differentially associated with longitudinal deterioration in adherence as a function of concomitant growth in self-efficacy or pubertal maturation. We hypothesized that more rapid deterioration in adherence would be evidenced among adolescents who (a) experienced declines in parental responsibility without also experiencing concurrent increases in self-efficacy, or (b) experienced more rapid declines in parental responsibility concurrent with more rapid pubertal maturation.
Method
Participants
Participants included 252 adolescents (53.6% females) diagnosed with type 1 diabetes, their mothers, and 188 fathers recruited from a university/private partnership clinic (85%) and a community-based private practice (15%). At enrollment, adolescents were between 10 and 14 years old, mean (standard deviation) [M (SD)] = 12.49 (1.53), had diabetes for >1 year, M (SD) = 4.13 (2.98), were able to read and write English or Spanish, and lived with their mother (a goal of the full study was to examine mother–child transactions). At enrollment, 50.8% of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections; at the final wave of data collection (2.5 years later), 63% of adolescents were on a pump.
Of the eligible individuals approached, 66% agreed to participate. Reasons for refusal included distance (18%), too busy (21%), not interested (30%), uncomfortable with being studied (14%), and time commitments (5%). Most families were Caucasian (91.7%) and middle class, with 63.5% reporting household incomes ≥$50,000 annually. An average Hollingshead index of 41.19 indicated a medium business, minor professional, technical status; 52.4% of mothers and 44% of fathers reported education levels of 2 years of college or beyond.
Procedure
This study was approved by the institutional review board. Parents gave written informed consent and adolescents gave written assent. Families completed assessments every 6 months for 2.5 years. At each assessment, adolescents completed questionnaires at home, and additional assessments at a laboratory appointment. Participants received $50 each for completing assessments at Times 1–5, and $100 for completing Time 6. Participants could skip time points while remaining in the study for subsequent assessments. Over the course of the study, 49 adolescents withdrew or were considered lost to follow-up because they skipped all subsequent assessments (81% retention). Figure 1 provides full information on the number of participants who completed measures at each time point and who remained in the study across time. There were no baseline differences in age, gender, or any study variable between families who did and did not participate at each time point, with one exception: fathers who participated at Times 2, 4, and 5 reported higher baseline adolescent efficacy than fathers who did not, p<.05. Primary reasons for withdrawing included changes in family circumstances such as not living with mother or death in the family (19%), too busy (12%), and study demands (12%).
Figure 1.
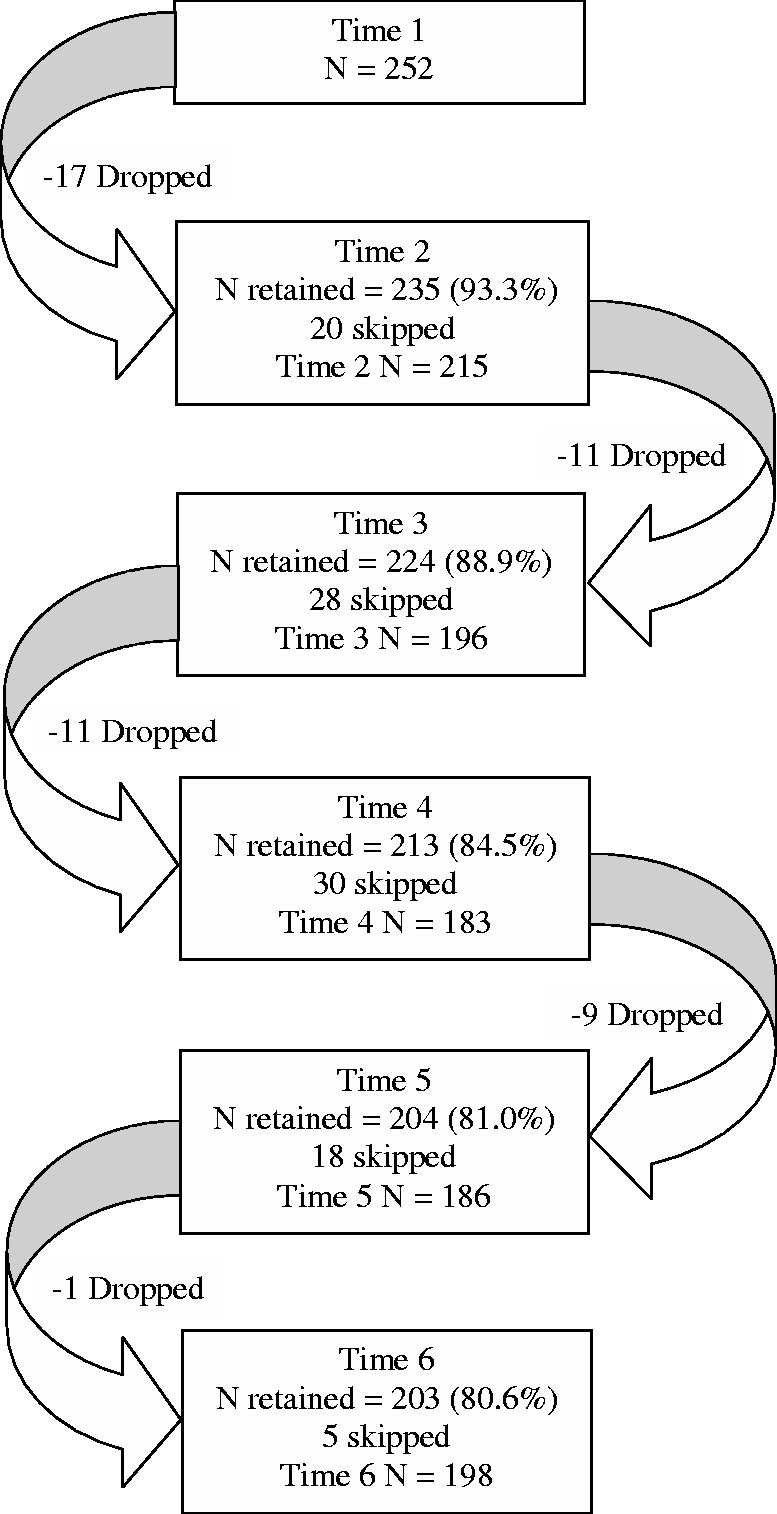
Flow chart of family attrition and skipped data points across time. Participants were designated as skipped if they did not complete a given time point, but did complete a subsequent time point. Participants were designated as dropped if they officially withdrew or skipped all subsequent time points.
Measures
Adherence
Adolescents, mothers, and fathers completed the Self-Care Inventory (La Greca, Follansbee, & Skyler, 1990) to indicate adherence to the diabetes regimen over the preceding month. The original 14-item scale was adapted through consultation with a certified diabetes educator by adding two items that reflected current treatment standards (i.e., “How well have you followed recommendations for counting carbohydrates?” and “How well have you followed recommendations for calculating insulin doses based on carbohydrates in meals and snacks?”). Behaviors were rated on a scale from 1 (never did it) to 5 (always did it as recommended without fail). Average scores across items were analyzed. At all time points, α ≥ .86 for adolescent reports, α ≥ .85 for mother reports, and α ≥ .83 for father reports.
Parental Responsibility for Diabetes Management
Adolescents and parents completed the Diabetes Responsibility Scale (Rubin, Young-Hyman, & Peyrot, 1989), reporting on the extent to which adolescents or parents are responsible for 23 aspects of diabetes management (e.g., “Who determines the insulin dose?”). Items were completed on a scale from 1 (adolescent alone) to 3 (share equally) to 5 (parent alone). Five items related to the use of an insulin pump were added through consultation with a certified diabetes educator; participants who did not use an insulin pump were instructed to endorse a not applicable option for these items. The scale was scored by taking an average value for all relevant items (i.e., average of 23 items for those prescribed MDI, average of 28 items for insulin pump users). At all time points, α ≥ .91 for adolescent reports, α ≥ .86 for mother reports, and α ≥ .91 for father reports.
Efficacy for Diabetes
Adolescents, mothers, and fathers completed the Self-Efficacy for Diabetes Management Scale (Iannotti et al., 2006), reporting confidence in their own (adolescent self-efficacy) or their adolescent’s (parent report of adolescent efficacy) ability to manage diabetes across 10 problematic situations (e.g., “How sure are you that you can manage insulin intake when you have eaten more or less than usual). Items were rated from 1 (not at all sure) to 10 (completely sure) and averaged. At all time points, α ≥ .82 for adolescent reports, α ≥ .91 for mother reports, and α ≥ .93 for father reports.
Pubertal Status
Each participant reported the extent to which the adolescent displayed signs of puberty (Petersen, Crockett, Richards, & Boxer, 1988). Three items applied to all adolescents (height, body hair, skin changes), and two items applied specifically to males (voice deepening, facial hair growth) or females (breast growth, menstruation). Items were completed on 1 (has not yet started) to 4 (seems completed) scale and averaged. This scale correlates well with physician Tanner ratings (Petersen et al., 1988; Schmitz et al., 2004). At all time points, α ≥ .81 for adolescent reports, α ≥ .85 for mother reports, and α ≥ .79 for father reports.
Analysis Plan
Data were analyzed with Structural Equation Modeling implemented in Mplus 6.11 (Muthén & Muthén, 2010). Missing data were addressed using full information maximum likelihood (Hofer & Hoffman, 2007). Separate models were estimated for each reporter. Preliminary analyses examined the presence of linear versus nonlinear change in each study variable, using measurement occasion as the marker of time, centered at Time 1. Unconditional latent growth curve (LGC) models were computed to examine the presence of linear change, and latent basis growth models were computed to allow for nonlinear change (McArdle, 2012). For each study variable, a linear change model fit the constructs well, and allowing for nonlinear change did not improve model fit. Thus, all results are based on linear growth models. In all analyses, adolescents’ age, sex, and time since diagnosis at time 1 were covaried because these characteristics have predicted parental responsibility in the past (Palmer et al., 2004).
To identify the variables associated with longitudinal declines in parental responsibility (Aim 1), we specified a series of conditional LGC models in which parental responsibility slope was treated as the outcome variable predicted simultaneously by (1) latent intercepts of parental responsibility, adolescent efficacy, and pubertal status, and (2) latent slopes of adolescent efficacy and pubertal status. Parental responsibility intercept was also predicted by latent intercepts of adolescent efficacy and puberty.
To examine whether growth in adolescent efficacy or pubertal status moderated associations between declining parental responsibility and deteriorating adherence (Aim 2), we specified conditional LGC models in which adherence slope was treated as the outcome variable, predicted by an interaction between the latent slopes of parental responsibility and either self-efficacy or pubertal status. The interaction terms for adolescent efficacy and pubertal status were examined in separate models because the model did not converge when both moderation effects were tested simultaneously. In both models, the moderation effect was tested after entering the latent intercepts of adherence, parental responsibility, adolescent efficacy, and pubertal status, and the latent slopes of parental responsibility, adolescent efficacy, and pubertal status.
Results
Trajectories of Efficacy, Pubertal Maturation, and Parental Responsibility
Unconditional LGC models revealed that, consistently across reporter, parental responsibility decreased linearly over time, with between-subject variability in both the latent intercepts (initial level) and slopes (rate of change over time) (ps < .05). The average intercepts of 2.591 (standard error, SE = .039), 2.886 (SE = .036), and 2.938 (SE = .045) for adolescent, mother, and father report suggest families were generally sharing responsibility for diabetes tasks at baseline. The average slopes across time of −.090 (SE = .007), −.109 (SE = .005), and −.103 (SE = .008) for adolescent, mother, and father report suggest adolescents were assuming primary but not sole responsibility for diabetes management by the end of the study.
Results from the conditional LGC models predicting parental responsibility from efficacy and pubertal status simultaneously are presented in Table I. Consistently across reporters, lower initial levels of parental responsibility were displayed among adolescents who were older, had shorter illness duration, and higher pubertal maturation at baseline. Mothers who reported higher initial adolescent efficacy also reported lower initial responsibility. Results predicting linear declines in parental responsibility showed adolescents who reported higher initial levels of parental responsibility, self-efficacy, and pubertal maturation displayed steeper declines in parental responsibility across time. In addition, for both adolescent and mother reports, faster linear increases in adolescent efficacy and pubertal maturation were associated with steeper declines in parental responsibility. Notably, adolescent age at baseline did not predict rate of decline in parental responsibility, and associations between self-efficacy or pubertal status and responsibility occurred after age was statistically controlled.
Moderators of the Association Between Declines in Parental Responsibility and Adherence
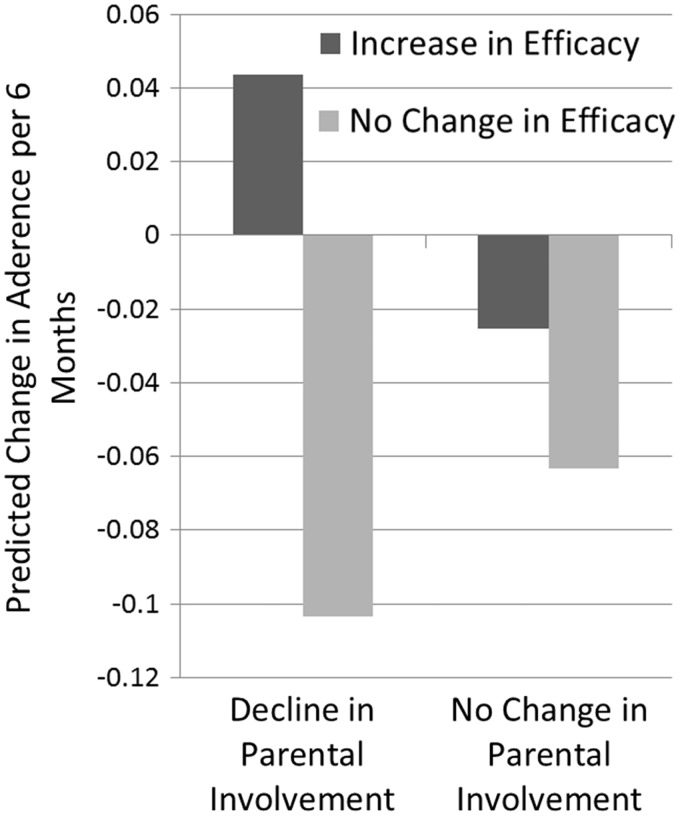
We have previously reported unconditional LGC models indicating that, for all reporters, adherence decreased linearly over time (King et al., 2013). Conditional LGC models predicting these declines in adherence were conducted to examine whether declines in parental responsibility were associated with deteriorating adherence over time, and whether increases in efficacy or puberty moderated this association. By adolescent report, declines in parental responsibility were not significantly associated with declines in adherence, b(SE) = .241 (.142), p > .05, but this association was moderated by more rapid growth in self-efficacy. Specifically, a significant interaction between the slopes of adolescent reported self-efficacy and parental responsibility predicted the slope of adherence, b(SE) = −1.522 (.001), p < .01. The shape of this interaction was examined by computing predicted mean changes in adherence as a function of more rapid increases in self-efficacy (identified as 1 SD above the mean increase in adolescent self-efficacy) versus no change in self-efficacy, and more rapid decreases in parental involvement (1 SD below the mean decrease in parental responsibility) versus no change in parental involvement. As shown in Figure 2, declines in adherence were steepest among adolescents who reported more rapid declines in parental responsibility without experiencing increases in self-efficacy. Interestingly, the only participants for whom adherence did not deteriorate across time were those reporting declines in parental responsibility while experiencing increases in self-efficacy.
Figure 2.
Changes in adherence at each time point predicted from change in adolescents' self-efficacy and parental responsibility over time. Increase in self-efficacy was identified as 1 SD above the mean increase in adolescent self-efficacy, and decrease in parental involvement was identified as 1 SD below the mean decrease in parental responsibility.
Neither parental responsibility change, b(SE) = .506 (.543) and −.095 (.237), ps > .10, nor its interaction with adolescent efficacy change, b(SE) = −1.378 (.900) and −1.366 (1.729), ps > .10, predicted declines in adherence in mother- and father-reported data, respectively. In addition, increases in pubertal status did not moderate associations between declines in parental responsibility and adherence for any reporter, b(SE) = −1.605 (.861), −1.761 (1.503), and −1.677 (1.572), ps > .065 for adolescent, mother, and father reports, respectively.
Discussion
This study is among the first to examine longitudinal trajectories of parental responsibility for diabetes management across adolescence. Our findings indicated adolescence is a time of risk for type 1 diabetes management partially because transfer of responsibility from parent to adolescent does not match the adolescent’s developing self-efficacy beliefs. Adolescents displayed linear declines in parental responsibility for diabetes, and these declines were steeper among those who displayed more rapid growth in self-efficacy and pubertal status. Furthermore, the rate of decline in parental responsibility was associated with deterioration in adolescent-reported adherence especially when it occurred without concomitant growth in adolescent self-efficacy. These findings add to our understanding of the factors that may contribute to poor adherence across adolescence and identify self-efficacy as an important variable to consider as responsibility for diabetes is transferred from parent to adolescent.
Table I.
Latent Growth Curve Model Predicting Parental Responsibility Initial Status and Linear Change From Pubertal Status and Efficacy
| Predictors | Adolescent report |
Mother report |
Father report |
|||
|---|---|---|---|---|---|---|
| Responsibility initial status | Responsibility linear change | Responsibility initial status | Responsibility linear change | Responsibility initial status | Responsibility linear change | |
| Adolescent gender | −.005 (.072) | .008 (.015) | −.083 (.063) | −.015 (.017) | −.054 (.079) | .007 (.018) |
| Adolescent age | −.159 (.033)** | .003 (.007) | −.137 (.027)** | .001 (.003) | −.205 (.034)** | .005 (.009) |
| Time since diagnosis | .030 (.010)** | −.001 (.002) | .023 (.009)** | .000 (.008) | .047 (.012)** | −.004 (.004) |
| Puberty initial status | −.140 (.030)** | −.050 (.015)** | −.146 (.020)** | .008 (.016) | −.131 (.026)** | −.030 (.023) |
| Efficacy initial status | −.131 (.071)† | −.014 (.007)* | −.146 (.057)* | .006 (.006) | −.081 (.081) | −.002 (.006) |
| Responsibility initial status | – | −.099 (.017)** | – | .000 (.020) | – | −.034 (.023) |
| Puberty linear change | – | −.300 (.074)** | – | −.226 (.109)* | – | −.067 (.118) |
| Efficacy linear change | – | −.079 (.041)* | – | −.197 (.093)* | – | −.118 (.092) |
| Fit statistics | ||||||
| χ2 | 360.998/197 | 435.852/197 | 333.155/197 | |||
| RMSEA | .057 | .069 | .052 | |||
| CFI | .953 | .943 | .951 | |||
| TLI | .951 | .940 | .949 | |||
Note. All parameters are unstandardized with standard errors in parentheses. Paths from efficacy and pubertal status linear change to parental involvement initial status were not estimated. RMSEA = root mean square error of approximation; CFI = comparative fit index; TLI = Tucker Lewis index. †p < .10, *p < .05, **p < .01.
There was a gradual decline in parental responsibility across ages 10–17 years. That is, by enrolling participants aged 10–14 years and assessing every 6 months, we were able to examine longitudinal change across early (e.g., 10–13 years), middle (e.g., 12–15 years), and late adolescence (e.g., 14–17 years). A linear model fit the pattern of decline in responsibility for all reporters. Furthermore, although participants who were older at baseline had lower initial levels of parental responsibility, age did not predict the rate of subsequent decline in responsibility. This gradual ceding of responsibility from parent to adolescent is likely to provide an important training ground for adolescents to practice new skills and develop competence and confidence as they assume new responsibilities. It is notable that scores on the parental responsibility scale declined from averages reflecting shared responsibility at Time 1 to averages suggesting the adolescent is primarily, but not solely responsible by Time 6. Thus, even in early adolescence (i.e., 10-year olds), our participants were actively managing their illness by sharing responsibilities with parents.
Although average scores across items on the diabetes responsibility scale suggested a gradual linear decline in parental responsibility, these averages may mask considerable heterogeneity in how families completed various diabetes tasks. For example, an average score of 3 (adolescent and parent share equally) on the Diabetes Responsibility Scale could occur if parent and adolescent shared responsibility for each of the regimen tasks, or if the adolescent assumed responsibility for some tasks while the parent assumed responsibility for others. It has been suggested that the assumption of responsibility is task-specific, beginning earlier for some regimen tasks and later for others, and that there is individual variability in how this assumption of responsibility for different tasks occurs (Hanna & Decker, 2010). Recurrent cycles of responsibility transfer for different tasks could allow adolescents to explore independence in one domain while having the safety net of parental involvement in other domains. This possibility is consistent with our findings, but was not tested directly.
Adolescents differed in their rate of decline in parental responsibility as a function of multiple ongoing developments including outward signs of physical maturation and self-efficacy for diabetes. Declines in parental responsibility were related to increases in pubertal status, independent of concomitant growth in adolescent efficacy and age. Thus, consistent with cross-sectional research (Holmes et al., 2006; Palmer et al., 2004, 2009), outward signs of physical maturation may cue families that adolescents are growing up and may be ready to assume increased responsibility. We had hypothesized that transfer of responsibility that occurred in the context of more rapid pubertal maturation would be problematic given the dysregulating effects of pubertal hormones. However, increases in puberty did not moderate associations between declines in parental responsibility and adherence. Different results may have been found had we obtained direct measures of the hormonal fluctuations that accompany pubertal maturation.
Growth in adolescents’ self-efficacy beliefs appeared to provide unique information about how families can meet the challenges of managing diabetes across adolescence. When declines in parental responsibility occurred without concomitant growth in adolescent self-efficacy, there was more rapid deterioration in adherence across adolescence. In contrast, when declines in parental responsibility occurred in the presence of growth in self-efficacy, there appeared to be slight improvement in adherence across adolescence. These data need to be interpreted with caution given that the moderation effect occurred only for adolescent report of self-efficacy. If replicable, however, the data suggest that adolescents’ confidence in their ability to manage diabetes in relevant problematic situations provides a targeted metric to consider in the complex process of them assuming increasing independence in diabetes management.
A small set of studies has demonstrated that it is the premature transfer of responsibility, rather than transfer of responsibility per se, that is associated with poorer adolescent diabetes management, but the present study is the first to examine this process across time. Previous cross-sectional work by Wysocki et al. (1996), for example, found that adolescents with excessive self-care autonomy (i.e., low parental responsibility relative to adolescents’ low psychosocial maturity) displayed poorer adherence than those whose responsibility was better matched to their maturity. The present study extends this work by demonstrating the unfolding developmental process linking changes in parental involvement, adolescent self-efficacy, and adherence across time.
Because associations between longitudinal changes (i.e., slopes) in parental responsibility, adolescent efficacy, and adherence were analyzed concurrently, we cannot infer causality. It remains possible that increases in efficacy were responsive to the experience of heightened responsibility rather than cueing the assumption of responsibility. Self-efficacy is theorized to develop out of competence experiences (Bandura, 1982), and some independence in diabetes management may be necessary for its development (Helgeson et al., 2008; Ott et al., 2000). If so, future research to increase competence experiences and facilitate the growth of self-efficacy will be important. It is also possible that adolescent efficacy and parental responsibility mutually influenced each other across time, and that these mutual dependencies facilitated or undermined diabetes management. For example, adolescents who experience mastery as they assume responsibility for diabetes tasks are likely to develop increased confidence in their abilities (Ott et al., 2000), maintain adherence in the face of difficulties, and generate parents’ confidence that they can assume more responsibility. Difficulties in management, however, may undermine adolescents’ and parents’ confidence (Berg, Butner, Butler, King, Hughes, & Wiebe, 2013), which ideally would slow the transfer of responsibility until such difficulties are resolved. Through such ongoing mutual influences, adherence may be maintained across adolescence to the extent that gradual declines in parental responsibility map onto growth in adolescent self-efficacy. Our findings are consistent with this possibility, but we did not directly test these more complex transactional dynamics.
One strength of the study is that we included data from adolescent, mother, and father perspectives. Although some results were consistent across reporters, the expected patterns were most apparent in adolescent reported data. In particular, only adolescent self-efficacy moderated associations between deteriorations in parental responsibility and adherence. It is not surprising that adolescents’ beliefs in their own efficacy are most predictive of their ability to maintain adherence as they assume increasing responsibility, but patterns across reporter must be interpreted cautiously. We were unable to directly compare coefficients across reporter owing to the complexity of the models (L. K. Muthén, personal communication, October 4, 2012).
There are limitations to this study that should be considered when interpreting the findings. The sample was primarily Caucasian, middle-class, and on an intensive treatment regimen delivered in a pediatric endocrinology clinic with opportunities for frequent contact with providers. In this context, lower levels of parental responsibility for diabetes care may be less damaging (Wysocki et al., 2006), and opportunities for warm and accepting parent–adolescent relationships that support adherence may be increased (Drew et al., 2011). Thus, different results may occur in a more diverse sample. The data were self-report, which may be biased relative to objective indices, and correlational; causal directions of association cannot be inferred. Although self-efficacy was identified as a key construct in the transfer of responsibility, other beliefs and skills should also be examined (e.g., self-control, executive functions).
Multiple developmental processes play a role in how transfer of responsibility for diabetes management occurs, but self-efficacy beliefs may provide unique information about adolescents’ readiness to assume responsibility. These findings hold important clinical implications. It may be useful for parents and providers to monitor self-efficacy beliefs as they guide adolescents to more independent management. The self-efficacy scale is brief and could readily be completed during clinic visits. Overall scores could be used to track changes in self-efficacy beliefs and individual items could identify specific problems that undermine adolescents’ confidence and guide-targeted problem-solving. Interventions to facilitate adolescent self-efficacy development may also be useful. Brief psychoeducational or cognitive behavioral approaches that have been developed to promote mastery experiences and self-efficacy for other chronic illnesses (Marks & Allegrante, 2005) may be adapted for adolescents with type 1 diabetes. Growth in self-efficacy for diabetes may also occur when parents support adolescent autonomy by providing some behavioral independence (Ott et al., 2000), while maintaining high-quality relationships and remaining aware of their adolescent’s diabetes activities (King et al., 2013). Thus, family-based interventions may facilitate the smooth transfer of responsibility in this vulnerable population.
Acknowledgments
We thank members of the ADAPT research group for their valuable assistance, the physicians and staff at the Utah Diabetes Center and Mountain Vista Medicine, and the adolescents and parents who participated in this study.
Funding
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (R01 DK063044).
Conflicts of interest: None declared.
References
- Anderson B J, Brackett J, Ho J, Laffel L M. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Impact on parent involvement, family conflict, and subsequent glycemic control. Diabetes Care. 1999;22:713–721. doi: 10.2337/diacare.22.5.713. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self efficacy mechanism in human agency. American Psychologist. 1982;37:122–147. [Google Scholar]
- Berg C A, Butner J E, Butler J M, King P S, Hughes A E, Wiebe D J. Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychology. 2013;32:719–728. doi: 10.1037/a0029427. doi:10.1037/a0029427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron F J, Skinner T C, de Beaufort C E, Hoey H, Swift P G, Aanstoot H, Aman J, Martul P, Chiarelli F, Daneman D, Danne T, Dorchy H, Kaprio E A, Kaufman F, Kocova M, Mortensen H B, Njølstad P R, Phillip M, Robertson K J, Schoenle E J, Urakami T, Vanelli M, Ackermann R W, Skovlundt S E, Hvidoere Study Group on Childhood Diabetes Are family factors universally related to metabolic outcomes in adolescents with Type 1 diabetes? Diabetic Medicine. 2008;25:463–468. doi: 10.1111/j.1464-5491.2008.02399.x. doi:10.1111/j.1464-5491.2008.02399.x. [DOI] [PubMed] [Google Scholar]
- Drew L D, Berg C A, King P, Verdant C, Griffith K, Butler J, Wiebe D J. Depleted parental psychological resources as mediators of the association of income with adherence and metabolic control. Journal of Family Psychology. 2011;25:751–758. doi: 10.1037/a0025259. doi:10.1037/a0025259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna K M, Decker C L. A concept analysis: Assuming responsibility for self-care among adolescents with type 1 diabetes. Journal for Specialists in Pediatric Nursing. 2010;15:99–110. doi: 10.1111/j.1744-6155.2009.00218.x. doi:10.1111/j.1744-6155.2009.00218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson V S, Reynolds K A, Siminerio L, Escobar O, Becker D. Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. Journal of Pediatric Psychology. 2008;33:497–508. doi: 10.1093/jpepsy/jsm081. doi:10.1093/jpepsy/jsm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson V S, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: A 4-year longitudinal study. Journal of Pediatric Psychology. 2009;34:254–270. doi: 10.1093/jpepsy/jsn079. doi:10.1093/jpepsy/jsn079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer S, Hoffman L. Statistical analysis with incomplete data: A developmental perspective. In: Little T, Bovaird J, Card N, editors. Modeling contextual effects in longitudinal studies. Mahwah, NJ: Erlbaum; 2007. pp. 13–32. [Google Scholar]
- Holmes C S, Chen R, Streisand R, Marschall D E, Souter S, Swift E E, Peterson C C. Predictors of youth diabetes care behaviors and metabolic control: A structural equation modeling approach. Journal of Pediatric Psychology. 2006;31:770–784. doi: 10.1093/jpepsy/jsj083. [DOI] [PubMed] [Google Scholar]
- Hood K K, Peterson C M, Rohan J M, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics. 2009;124:1171–1179. doi: 10.1542/peds.2009-0207. doi:10.1542/peds.2009-0207. [DOI] [PubMed] [Google Scholar]
- Hughes A E, Berg C A, Wiebe D J. Emotional processing and self-control in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2012;37:925–934. doi: 10.1093/jpepsy/jss062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsin O, La Greca A M, Valenzuela J, Moine C T, Delamater A. Adherence and glycemic control among Hispanic youth with type 1 diabetes: Role of family involvement and acculturation. Journal of Pediatric Psychology. 2010;35:156–166. doi: 10.1093/jpepsy/jsp045. doi:10.1093/jpepsy/jsp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannotti R J, Schneider S, nansel T R, Haynie D L, Plotnick L P, Clark L M, Sobel D O, Simons-Morton B. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. Journal of Developmental and Behavioral Pediatrics. 2006;27:98–105. doi: 10.1097/00004703-200604000-00003. [DOI] [PubMed] [Google Scholar]
- Ingerski L M, Anderson B J, Dolan L M, Hood K K. Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. Journal of Adolescent Health. 2010;47:191–197. doi: 10.1016/j.jadohealth.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaugars A S, Kichler J C, Alemzadeh R. Assessing readiness to change the balance of responsibility for managing type 1 diabetes mellitus: Adolescent, mother, and father perspectives. Pediatric Diabetes. 2011;12:547–555. doi: 10.1111/j.1399-5448.2010.00737.x. doi:10.1111/j.1399-5448.2010.00737.x. [DOI] [PubMed] [Google Scholar]
- King P S, Berg C A, Butner J, Butler J M, Wiebe D J. Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents’ adherence. Health Psychology. 2013 doi: 10.1037/a0032804. Advance online publication. doi:10.1037/a0032804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A M, Follansbee D, Skyler J S. Developmental and behavioral aspects of diabetes management in youngsters. Children's Health Care. 1990;19:132–139. [Google Scholar]
- Marks R, Allegrante J P, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part II) Health Promotion Practice. 2005;6:148–156. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- McArdle J J. Foundational issues in the contemporary modeling of longitudinal trajectories. In: Laursen B, Little T D, Card N A, editors. Handbook of developmental research methods. New York, NY: Guilford Press; 2012. pp. 385–410. [Google Scholar]
- Miller V A, Drotar D. Discrepancies between mother and adolescent perceptions of diabetes-related decision-making autonomy and their relationship to diabetes-related conflict and adherence to treatment. Journal of Pediatric Psychology. 2003;28:265–274. doi: 10.1093/jpepsy/jsg014. [DOI] [PubMed] [Google Scholar]
- Muthén L K, Muthén B O. Mplus User's Guide. 6th ed. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Ott J, Greening L, Palardy N, Holderby A, DeBell W K. Self-efficacy as a mediator variable for adolescents' adherence to treatment for insulin-dependent diabetes mellitus. Children's Heath Care. 2000;29:47–63. [Google Scholar]
- Palmer D L, Berg C A, Butler J, Fortenberry K, Murray M, Lindsay R, Donaldson D, Swinyard M, Foster C, Wiebe D J. Mothers’, fathers’, and children's perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. Journal of Pediatric Psychology. 2009;34:195–204. doi: 10.1093/jpepsy/jsn073. doi:10.1093/jpepsy/jsn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer D L, Berg C A, Wiebe D J, Beveridge R M, Korbel C D, Upchurch R, Swinyard M T, Lindsay R, Donaldson D L. The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology. 2004;29:35–46. doi: 10.1093/jpepsy/jsh005. [DOI] [PubMed] [Google Scholar]
- Petersen A, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Rubin R R, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38:28A. [Google Scholar]
- Schmitz K E, Hovell M F, Nichols J F, Irvin V L, Keating K, Simon G M, Gehrman C, Jones K L. A validation study of early adolescents’ pubertal self-assessments. Journal of Early Adolescence. 2004;24:357–384. doi:10.1177/0272431604268531. [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister L A, Clark N. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- Steinberg L. A social neuroscience perspective on adolescent risk-taking. Developmental Review. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. doi:10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesco A T, Anderson B J, Laffel L M, Dolan L M, Ingerski L M, Hood K K. Responsibility sharing between adolescents with type 1 diabetes and their caregivers: Importance of adolescent perceptions on diabetes management and control. Journal of Pediatric Psychology. 2010;35:1168–1177. doi: 10.1093/jpepsy/jsq038. doi:10.1093/jpepsy/jsq038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe D J, Berg C A, Korbel C, Palmer D L, Beveridge R M, Upchurch R, Lindsay R, Swinyard M T, Donaldson D L. Children's appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30:167–178. doi: 10.1093/jpepsy/jsi004. doi:10.1093/jpepsy/jsm043. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris M A, Buckloh L M, Wilkinson K, Sadler M, Mauras N, White N H. Self-care autonomy and outcomes of intensive therapy or usual care in youth with type 1 diabetes. Journal of Pediatric Psychology. 2006;31:1036–1045. doi: 10.1093/jpepsy/jsj017. doi:10.1093/jpepsy/jsj017. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Taylor A, Hough B S, Linscheid T R, Yeates K O, Naglieri J A. Deviation from developmentally appropriate self-care autonomy. Association with diabetes outcomes. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]