Abstract
Metastases to the breast from extramammary tumors are rare. Several clinical, radiologic, and histologic signs can help to distinguish metastases from breast primary tumors. In the present study, we present a case of a left-sided breast metastasis from renal cancer in a 44-year-old woman whose clinical presentation was a mammary nodule in the upper internal quadrant. The patient underwent quadrantectomy with sentinel lymph node biopsy. The histology revealed a clear cell carcinoma. On computed tomography scan a 5×8-cm left renal mass with pulmonary, liver, and intrapericardial nodules was found. The patient underwent palliative care and died after 4 months. Metastasis to the breast is rare, but all of those clinical, radiologic, and histologic signs more typical of extramammary malignancies should always be considered in order to choose the best treatment strategy.
Key words: Renal cell metastases, Clear cell carcinoma, Breast cancer, Metastases to the breast
A 44-year-old woman with no significant medical history presented to the breast outpatient clinic after noticing a solitary, painless, left-sided breast mass.
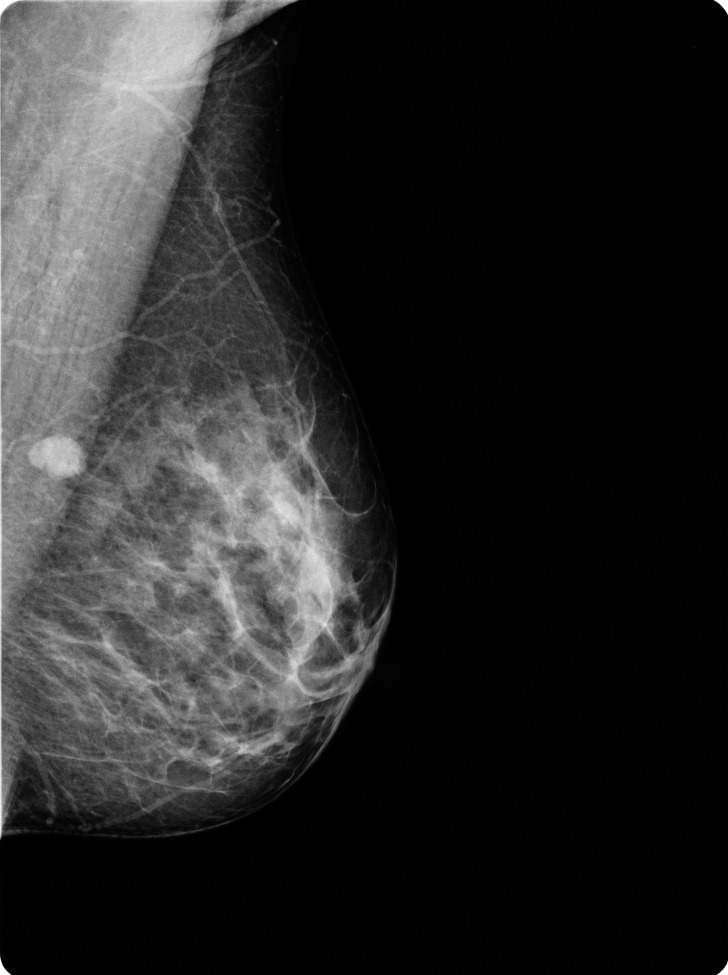
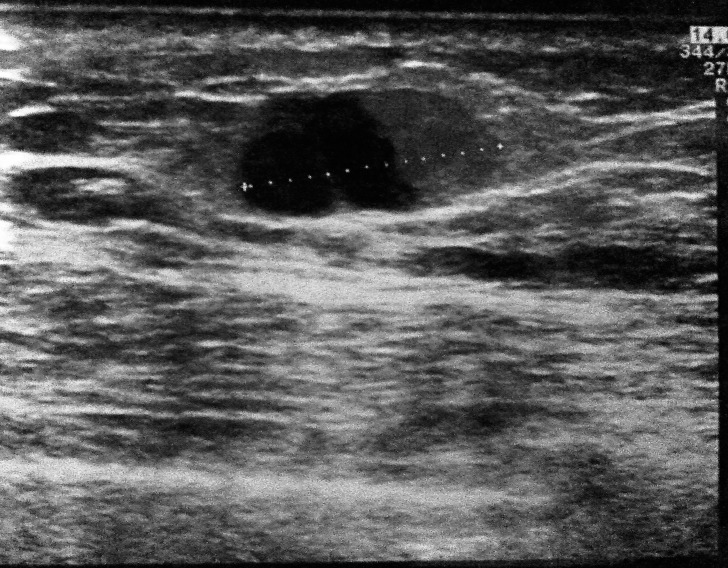
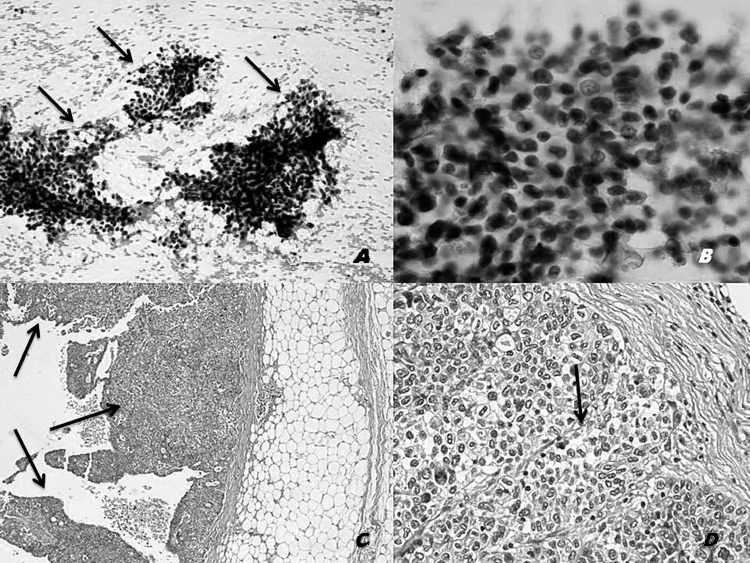
Physical examination revealed a focal, round, smooth, mobile mass at the 10-o'clock position of the left breast. She had no nipple discharge or skin changes, and no palpable axillary or supraclavicular lymphadenopathy. The right breast was normal to palpation. Mammography revealed a solid, smooth nodule in the upper internal quadrant of the left breast (Fig. 1). Ultrasound demonstrated an oval mass in the 10-o'clock position of the left breast measuring 15×10 mm (Fig. 2). Fine-needle aspiration cytology (FNAC) revealed malignancy (grade C5) (Fig. 3A and 3B). Quadrantectomy with sentinel lymph node biopsy was carried out. Histopathology revealed high-grade neoplasia with focal clear cell features and without ductal or lobular in situ components, which suggested metastasis from an extramammary neoplasm (Fig. 3C and 3D). Nevertheless, at immunohistochemistry only E-cadherin and pancytokeratin were positive, and a primary tumor could not be defined. Therefore, a full-body computed tomography scan was performed, and it showed a 50×80-mm left renal mass, multiple liver nodules, para-aortic lymphadenopathies, and a 22-mm pericardial lesion. The patient underwent palliative care and died after 4 months.
Fig. 1.
Left mammography identifying a solid, smooth nodule in the upper internal quadrant.
Fig. 2.
Breast ultrasound showing a 15×10-mm oval mass of the left breast.
Fig. 3.
(A and B) Papanicolaou stain [×10 (A) and ×40 (B)]. Cellular aspirate consisting of poorly differentiated malignant epithelial cells with a high nuclear to cytoplasm ratio (arrows) surrounded by red blood cells. (C and D) H&E [×4 (C) and ×20 (D)]. Poorly differentiated neoplastic cells with papillary architecture (C, arrows) and focal clear cell features (D, arrow).
Discussion
Breast metastasis from extramammary tumors is extremely rare, and metastatic renal cell carcinoma to the breast is extraordinary. It has been reported that metastases from extramammary malignant neoplasm to the breast account for approximately 0.3% to 2.7% of all malignant mammary tumors.1 In about 25% to 40% of breast metastases from extramammary carcinomas, the breast lesion is the initial manifestation of the disease. On examination, a nodule from metastatic carcinoma to the breast is relatively well circumscribed and freely movable. Axillary node involvement is variable.1
On mammography, solitary or multiple round or oval masses with circumscribed margins are described as the most common pattern of breast metastases. Microcalcifications can be found in 10% of cases.2 On ultrasound, a metastasis from a nonmammary malignancy is typically hypoechoic, oval or round in shape, with microlobulated or circumscribed margins, and with posterior acoustic enhancement.2 The exclusive use of FNAC for tumor diagnosis is disputed: several authors consider FNAC to be the best approach to tumor diagnosis,3–5 whereas others believe FNA findings insufficient to distinguish metastases from primary breast cancer.6 The medical history often helps the pathologist diagnose a metastatic disease to the breast only with FNAC, but in our case there were no significant medical records that could have raised the suspicion of an extramammary disease. The histologic features in nonhematologic metastases to the breast are helpful in the diagnosis. A circumscribed nodule with surrounding normal breast tissue without calcifications or signs of carcinoma in situ would strongly support the diagnosis of metastasis to the breast from extramammary malignancy. Immunohistochemistry is an important tool to define the primary tumor: renal cell carcinoma is usually positive for the renal cell carcinoma markers, whereas estrogen receptor, GCDFP-15, and cytokeratin 7 are rarely expressed.7 Immunohistochemistry was unhelpful in our case because specific cytokeratins were all negative and the final diagnosis was confirmed only with computed tomography scan.
Metastasis to the breast is extremely rare, but all of those clinical, radiologic, and pathologic signs more typical of extramammary malignancies must always be considered to choose the best treatment strategy.
References
- 1.Lee SK, Kim WW, Kim SH, Hur SM, Kim S, Choi JH, et al. Characteristics of metastasis in the breast from extramammary malignancies. J Surg Oncol. 2010;101(2):137–140. doi: 10.1002/jso.21453. [DOI] [PubMed] [Google Scholar]
- 2.Surov A, Fiedler E, Holzhausen HJ, Ruschke K, Schmoll HJ, Spielmann RP. Metastases to the breast from non-mammary malignancies: primary tumors, prevalence, clinical signs, and radiological features. Acad Radiol. 2011;18(5):565–574. doi: 10.1016/j.acra.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 3.Akcay MN. Metastatic disease in the breast. Breast. 2002;11(6):526–528. doi: 10.1054/brst.2002.0467. [DOI] [PubMed] [Google Scholar]
- 4.Gupta D, Merino MI, Farhood A, Middleton LP. Metastases to breast simulating ductal carcinoma in situ: report of two cases and review of the literature. Ann Diagn Pathol. 2001;5(1):15–20. doi: 10.1053/adpa.2001.21476. [DOI] [PubMed] [Google Scholar]
- 5.Domanski HA. Metastases to the breast from extramammary neoplasm: a report of six cases with diagnosis by fine needle aspiration cytology. Acta Cytol. 1996;40(6):1293–1300. doi: 10.1159/000334024. [DOI] [PubMed] [Google Scholar]
- 6.Smymiotis V, Theodosopoulos T, Marinis A, Goula K, Psychogios J, Kondi-Pafiti A. Metastatic disease in the breast from non-mammary neoplasms. Eur J Gynaecol Oncol. 2005;26(5):547–550. [PubMed] [Google Scholar]
- 7.Lee AHS. The histological diagnosis of metastases to the breast from extramammary malignancies. J Clin Pathol. 2007;60(12):1333–1341. doi: 10.1136/jcp.2006.046078. [DOI] [PMC free article] [PubMed] [Google Scholar]