Abstract
The optimal timing of early oral intake after surgery has not been fully established. The objective of this study was to compare early oral intake at postoperative day 1 after resection of colorectal cancer with that of day 2 to identify the optimal timing for resumption of oral intake in such patients. Consecutive patients with colorectal cancer who underwent elective colorectal resection were separated into two groups. Sixty-two patients began a liquid diet on the first postoperative day (POD1 group) and 58 patients began on POD2 (POD2 group) and advanced to a regular diet within the next 24 hours as tolerated. As for gastrointestinal recovery, the first passage of flatus was experienced, on average, on postoperative day 3.1 ± 1.0 in the POD2 group and on day 2.3 ± 0.7 in the POD1 group. The first defecation was also significantly earlier in patients in the POD1 group than those in the POD2 group (POD 3.2 ± 1.2 versus 4.2 ± 1.4, respectively). No statistical difference was found between the two groups in terms of postoperative complications. Our results suggest that very early feeding on POD1 after colorectal resection is safe and feasible and that induced a quicker recovery of postoperative gastrointestinal movement in patients.
Key words: Early oral feeding, Postoperative ileus, Colorectal surgery
Traditionally, postoperative oral intake has been withheld until clinical signs of the return of bowel function. Surgical treatment induces dysmotility and causes temporal paralytic ileus. Postoperative ileus is a frequent cause of complications and is an inevitable adverse consequence of surgical procedures.1−4 However, scientific evidence for this traditional method is lacking, and the small bowel is known to recover normal function 4−8 hours after surgery.5−10 Thus, the current thought is oral intake should be resumed as soon as possible after surgery. There are also potential benefits from early postoperative oral intake. Early oral feeding after colorectal surgery is one of the factors that enhance bowel motility after surgery, and it particularly counteracts postoperative paralytic ileus.10−15 Recently, several studies have reported that early oral intake helps enhance recovery after surgery compared with the traditional method of resuming oral intake only after clinical signs of resolution of postoperative paralytic dysmotility.10−15 However, these studies compared “early” feeding with “traditional” timing; investigation of the optimal timing of early oral intake after surgery has not been performed. The objective of this study was to compare very early oral intake at postoperative day (POD) 1 with that at day 2 for patients after resection of colorectal cancer. We assessed the impact of very early postoperative oral intake at POD 1 in patients who had undergone elective colorectal surgery.
Methods
Patients and methods
Consecutive patients with colorectal cancer who underwent elective colorectal resection at the Department of General Surgical Science, Graduate School of Medicine, Gunma University, from 2010 to 2011, were identified for inclusion in this study. Patients were separated into two groups. Fifty-eight patients who underwent elective colorectal resection in 2010 began a liquid diet on the second postoperative day (POD2 group) and advanced to a regular diet within the next 24 hours as tolerated.
Sixty-two patients who underwent elective colorectal resection in 2011 began a liquid diet on the first postoperative day (POD1 group) and advanced to a regular diet within the next 24 hours as tolerated. Patients who underwent simple colostomy and colostomy closure were not included, nor were those with emergency opera ions and surgery with stoma creation. Data were collected retrospectively. Informed consent for study participation was obtained from all patients. Postoperative ileus is defined as impairment in gastrointestinal motility or intestinal obstruction following surgery and all cases were diagnosed and confirmed by X-ray. Blood samples were obtained preoperatively and on POD 7. With the exception of those cases with intestinal stenosis, nasogastric tubes were not routinely used.
Clinical and surgical variables recorded for each patient included age, gender, location of tumor, stage of tumor, length of operation, intraoperative blood loss, body mass index (BMI), history of diabetes, serum albumin, C-reactive protein, and laparoscopic surgery. The times of the first passage of flatus and defecation, tolerance of liquid or solid diet, and postoperative complications including incisional surgical site infections, anastomotic leakage, and postoperative ileus were recorded precisely.
Univariate statistical analyses were conducted using the chi-square test for qualitative variables and the 2-tailed Fisher's exact test for some data, as well as unpaired, one-tailed t-tests. Differences were considered to be significant when P < 0.05.
Results
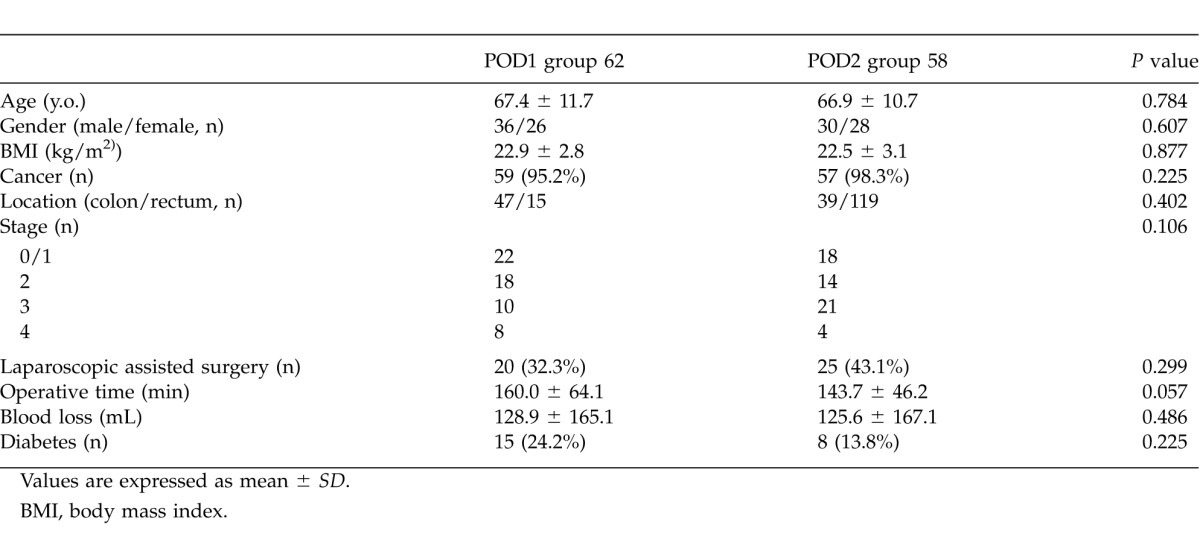
Table 1 summarizes the characteristics of the patients who underwent colorectal resection. The POD2 group consisted of 58 patients, including 30 males and 28 females with a mean age of 66.9 ± 10.7 years, whereas the POD1 group consisted of 62 patients, including 36 males and 26 females with a mean age of 67.4 ± 11.7 years. As can be seen in Table 1, clinical characteristics of the two groups were similar.
Table 1.
Patient and surgical characteristics
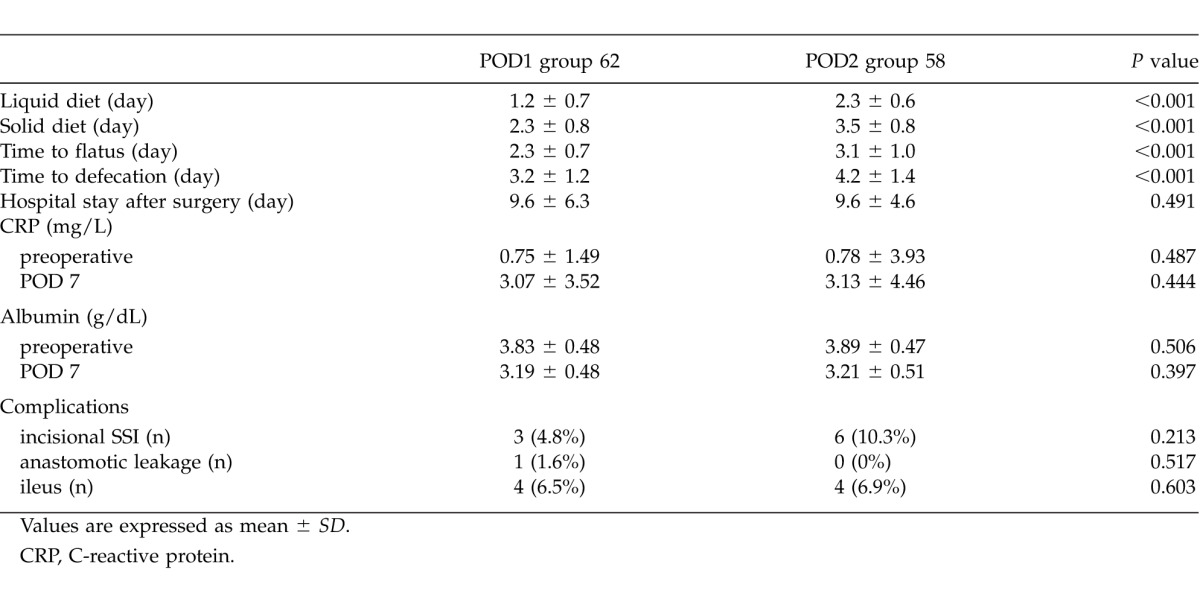
The majority of patients of both groups tolerated the early feeding schedule. The liquid diet was tolerated by patients in the POD1 group significantly earlier than those in the POD2 group (1.2 ± 0.7 versus 2.3 ± 0.6, respectively). The regular diet was also tolerated by patients in the POD1 group significantly earlier than those in the POD2 group (2.3 ± 0.8 versus 3.5 ± 0.8, respectively). As for gastrointestinal recovery, the first passage of flatus was seen on postoperative day 3.1 ± 1.0 in the POD2 group and on day 2.3 ± 0.7 in the POD1 group (P < 0.001). The first defecation was also significantly earlier in patients from the POD1 group than the POD2 group [POD 3.2 ± 1.2 versus 4.2 ± 1.4, respectively (P < 0.001)]. No statistical difference was found between the two groups regarding all the postoperative complications, including incisional SSI, anastomotic leakage and postoperative ileus (Table 2). There was no mortality in either group. The postoperative hospital stays were not significantly different between the two groups (9.6 ± 4.6 versus 9.6 ± 6.3, respectively).
Table 2.
Gastrointestinal recovery parameters and postoperative complications
Discussion
Postoperative ileus is a relatively common condition after colorectal surgery. Because of dysmotility early oral feeding after surgery has been avoided; however, many studies have demonstrated that early oral feeding is feasible and safe in patients undergoing colorectal surgery.5−10 Previous studies have revealed that the small bowel recovers normal contractile function 4−8 hours after laparotomy and that gastric emptying resumes on the first postoperative day.5−10 The pathophysiology of postoperative ileus is multifactorial. Early oral feeding after colorectal surgery is one of the factors that help to enhance recovery of gastrointestinal function and prevent postoperative ileus. The key observations made in this study can be summarized as follows: Time to flatus and defecation were significantly earlier in patients in POD1 patients than in POD2 patients.
These results suggest that early oral intake enhanced recovery postoperative gastrointestinal movement. Furthermore, complication rates and acceptance of diet were similar in the two groups. In short, the current findings imply that very early oral feeding should start on POD 1, and that oral intake should be resumed as soon as possible.
One of the potential advantages of early postoperative feeding is a shorter hospital stay; however, in this study hospital stay was not significantly different between the two groups. Information regarding the effect of early feeding on length of stay remains controversial.14−19 Several studies have failed to demonstrate that early oral feeding reduces the length of hospital stay.16 The length of hospital stay may be affected by many factors, including medical, psychological, or social factors. Although the current study, like previous literature,18−20 showed no association with a shorter length of hospital stay, early oral feeding did not increase the incidence of anastomotic leakage or other complications, which is clinically important.
This study has several potential limitations. The major limitation is the use of retrospective methods of data collection. Further laboratory and epidemiologic studies are necessary, and further studies should focus on the cost effectiveness of early oral intake and the patient's satisfaction.
In conclusion, we have demonstrated that very early feeding on postoperative day 1 after colorectal resection is safe and feasible. Time to flatus and defecation were significantly shorter in patients starting feeding on the first postoperative day than in those starting on the second postoperative day; very early oral intake enhanced the recovery of postoperative gastrointestinal movement.
Acknowledgments
The authors would like to thank Saitoh Y, Yano T, Matsui Y, and Ishida A for their secretarial assistance. This work was supported in part by Grants-in-Aid from the Japanese Ministry of Education, Culture, Sports, Science, and Technology (T.F.). The authors declare that they have no competing financial interests.
References
- 1.Luckey A, Livingston E, Tache Y. Mechanisms and treatment of postoperative ileus. Arch Surg. 2003;138(2):206–214. doi: 10.1001/archsurg.138.2.206. [DOI] [PubMed] [Google Scholar]
- 2.Baig MK, Wexner SD. Postoperative ileus: a review. Dis Colon Rectum. 2004;47(4):516–526. doi: 10.1007/s10350-003-0067-9. [DOI] [PubMed] [Google Scholar]
- 3.Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001;182((5A Suppl)):3S–10S. doi: 10.1016/s0002-9610(01)00781-4. [DOI] [PubMed] [Google Scholar]
- 4.Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C, et al. Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World J Surg. 2008;32(7):1495–1500. doi: 10.1007/s00268-008-9491-2. [DOI] [PubMed] [Google Scholar]
- 5.Ortiz H, Armendariz P, Yarnoz C. Is early postoperative feeding feasible in elective colon and rectal surgery? Int J Colorectal Dis. 1996;11(3):119–121. doi: 10.1007/s003840050032. [DOI] [PubMed] [Google Scholar]
- 6.Silk DBA, Gow NM. Postoperative starvation after gastrointestinal surgery. BMJ. 2001;323(7316):761–762. doi: 10.1136/bmj.323.7316.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rothnie NG, Kemp Harper RA, Catchpole BN. Early postoperative gastrointestinal motility. Lancet. 1963;2(7298):64–67. doi: 10.1016/s0140-6736(63)90064-3. [DOI] [PubMed] [Google Scholar]
- 8.El Nakeeb A, Fikry A, El Metwally T, Fouda E, Youssef M, Ghazy H, et al. Early oral feeding in patients undergoing elective colonic anastomosis. Int J Surg. 2009;7(3):206–209. doi: 10.1016/j.ijsu.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Bauer JJ, Gelernt JM, Salky BA, Keel J. Is routine postoperative nasogastric decompression really necessary? Ann Surg. 1985;201(2):233–236. doi: 10.1097/00000658-198502000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dag A, Colak T, Turkmenoglu O, Gundogdu R, Aydin S. A randomized controlled trial evaluating early versus traditional oral feeding after colorectal surgery. Clinics (Sao Paulo) 2011;66(12):2001–2005. doi: 10.1590/S1807-59322011001200001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lobato Dias Consoli M, Maciel Fonseca L, Gomes da Silva R, Toulson Davisson Correia MI. Early postoperative oral feeding impacts positively in patients undergoing colonic resection: results of a pilot study. Nutr Hops. 2010;25(5):806–809. [PubMed] [Google Scholar]
- 12.Gianotti L, Nespoli L, Torselli L, Panelli M, Nespoli A. Safety, feasibility, and tolerance of early oral feeding after colorectal resection outside an enhanced recovery after surgery (ERAS) program. Int J Colorectal Dis. 2011;26(6):747–753. doi: 10.1007/s00384-011-1138-3. [DOI] [PubMed] [Google Scholar]
- 13.Wang G, Jiang ZW, Xu J, Gong JF, Bao Y, Xie LF, et al. Fast-track rehabilitation program vs conventional care after colorectal resection: a randomized clinical trial. World J Gastroenterol. 2011;17(5):671–676. doi: 10.3748/wjg.v17.i5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reissman P, Teoh TA, Cohen SM, Weiss EG, Noguera JJ, Wexner SD. Is early oral feeding safe after elective colorectal surgery? A prospective randomized trial. Ann Surg. 1995;222(1):73–77. doi: 10.1097/00000658-199507000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zingg U, Miskovic D, Pasternak I, Meyer P, Hamel CT, Metzger U. Effect of bisacodyl on postoperative bowel motility in elective colorectal surgery: prospective, randomized trial. Int J Colorectal Dis. 2008;23(12):1175–1183. doi: 10.1007/s00384-008-0536-7. [DOI] [PubMed] [Google Scholar]
- 16.Cheatham ML, Chapman WC, Key SP, Sawyers JL. A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Ann Surg. 1995;222(5):469–476. doi: 10.1097/00000658-199505000-00004. discussion 476−478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steed HL, Capstic V, Flood C, Schepansky A, Shultz J, Mayes DC. A randomized controlled trial of early versus “traditional” postoperative oral intake after major abdominal gynecologic surgery. Am J Obstet Gynecol. 2002;186(5):861–865. doi: 10.1067/mob.2002.123057. [DOI] [PubMed] [Google Scholar]
- 18.Feo CV, Romanini B, Sortini D, Ragazzi R, Zamboni P, Pansini GC, et al. Early oral feeding after colorectal resection: a randomized controlled study. ANZ J Surg. 2004;74(5):298–301. doi: 10.1111/j.1445-1433.2004.02985.x. [DOI] [PubMed] [Google Scholar]
- 19.Schoetz DJ, Jr, Bockler M, Rosenblatt MS, Malhotra S, Roberts PL, Murray JJ, et al. “Ideal” length of stay after colectomy: whose ideal? Dis Colon Rectum. 1997;40(7):806–810. doi: 10.1007/BF02055437. [DOI] [PubMed] [Google Scholar]
- 20.Han-Geurts IJ, Jeekel J, Tilanus HW, Brouwer KJ. Randomized clinical trial of patient-controlled versus fixed regimen feeding after elective abdominal surgery. Br J Surg. 2001;88(12):1578–1582. doi: 10.1046/j.0007-1323.2001.01934.x. [DOI] [PubMed] [Google Scholar]


