Abstract
Incisional hernia is a common postoperative complication following open abdominal surgery with incidence varying between 3% and 20%.1 Approximately half of all incisional hernias are diagnosed within 1 year following surgery. In the United Kingdom alone, about 10,000 incisional hernia repairs are performed annually. Incisional hernia repairs are generally elective with emergency repair due to incarceration or strangulation constituting about 15% of repairs.1 Incisional hernia repair is not a low-risk operation and generally has relatively poor results due to chronic postoperative pain and high recurrence rates.2−3 Little has been published on patients' awareness of incisional hernia following open abdominal surgery. Moreover, there are very few publications on indications for incisional hernia repair and on the natural course of such hernias. The literature suggests that symptoms and complaints usually presented by patients include pain, discomfort, cosmetic complaints, skin problems, incarceration, strangulation, functional disability, and pulmonary dysfunction.4−6 The aim of this study was to investigate whether patients were aware that they had a hernia. In addition, we sought to determine symptoms for those who knew that they had an incisional hernia.
Key words: Incisional hernia, Awareness, Symptoms, Recurrence, Complications
A prospective study of all patients attending a surgical clinic between 2009 and 2010 was conducted. Inclusion criteria encompassed all those that had previous open abdominal surgery at least 1 year previously. Informed consent was obtained from all participants. All patients were examined by either a consultant or senior surgical trainee. A standard pro forma that recorded presence or absence of an incisional hernia on clinical examination and classification according to their localization, size, reducibility and symptoms, was completed. Pain, discomfort, cosmetic complaints, and functional disability in those with a hernia were depicted on a visual analogue scale (VAS) of 0 to 10, with 0 being no symptoms and 10 the worst possible that the patient could imagine. Finally, patients with a hernia were also asked if they were aware that they had a hernia. All hernias were identified by clinical examination only.
Statistical Analysis
Continuous data are reported as median and interquartile range. P values were obtained using the t test for numerical data and chi-square test for categorical data. The results are presented with a 95% confidence interval and a P-value of <0.05 was considered as statistically significant. All statistical analyses were performed using Microsoft Excel (version 14.2.5, Microsoft, Redmond, Washington, USA) software.
Results
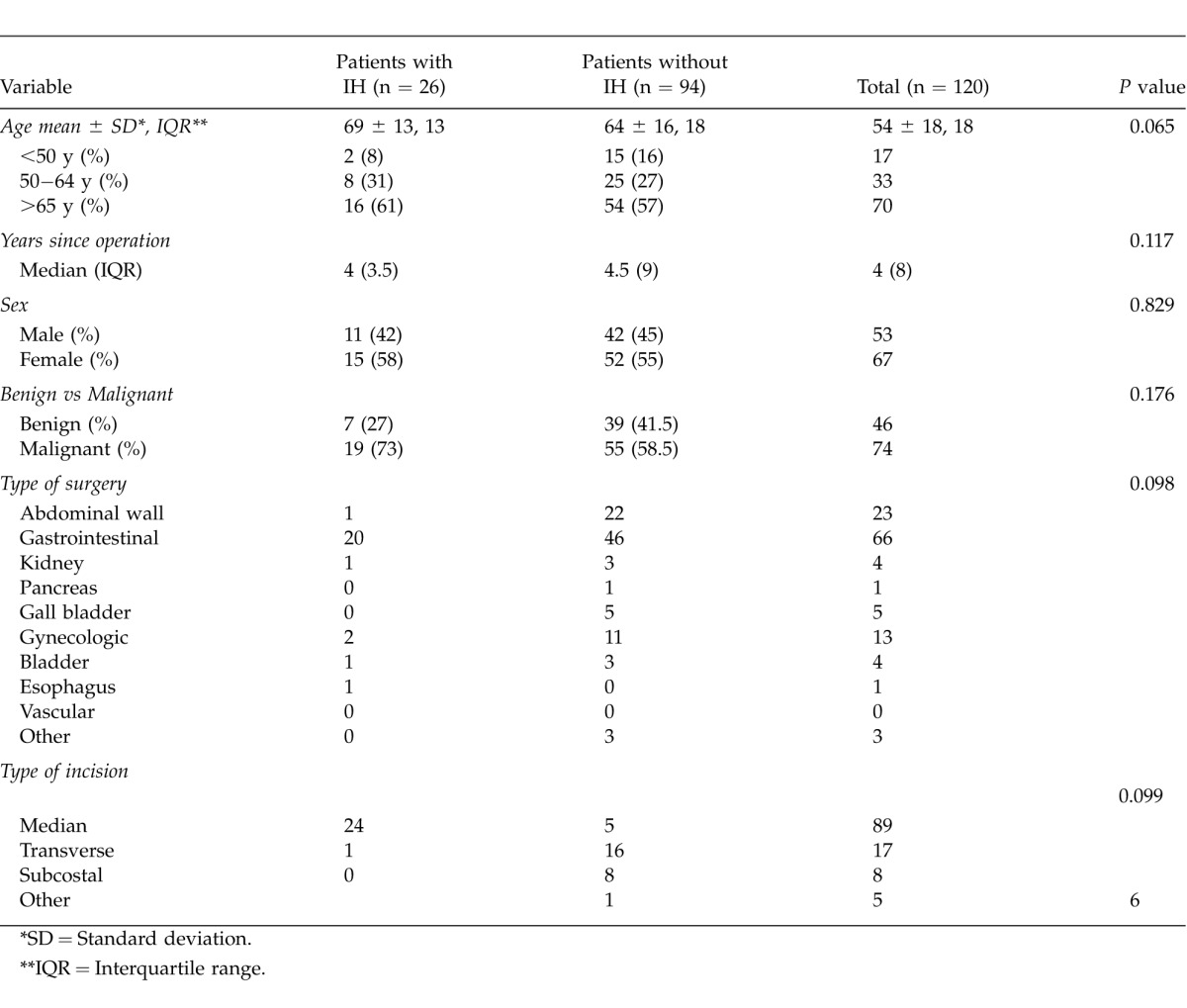
One hundred twenty patients participated in this study and 26 (21.6%) had clinical evidence of an incisional hernia. No significant differences were found between those that had a hernia and the rest of the study population. Moreover, there was no significant difference in incidence of incisional hernias between patients with a benign compared to those with a neoplastic condition. The 26 incisional hernias were categorized as midline (n = 18), lateral (n = 5) or midline and lateral (n = 3) using the classification of incisional hernias suggested by the European Hernia Society.7 Length (cm) and width (cm) were recorded for all hernias. Twenty of the 26 hernias were reducible while 6 were irreducible. The irreducible hernias were large incisional hernias of more than 10 cm in width or length. Baseline and clinical characteristics of the entire study population at the time of index surgery are shown in Table 1.
Table 1.
Baseline and clinical characteristics of study population at the time of index surgery
Awareness and symptoms
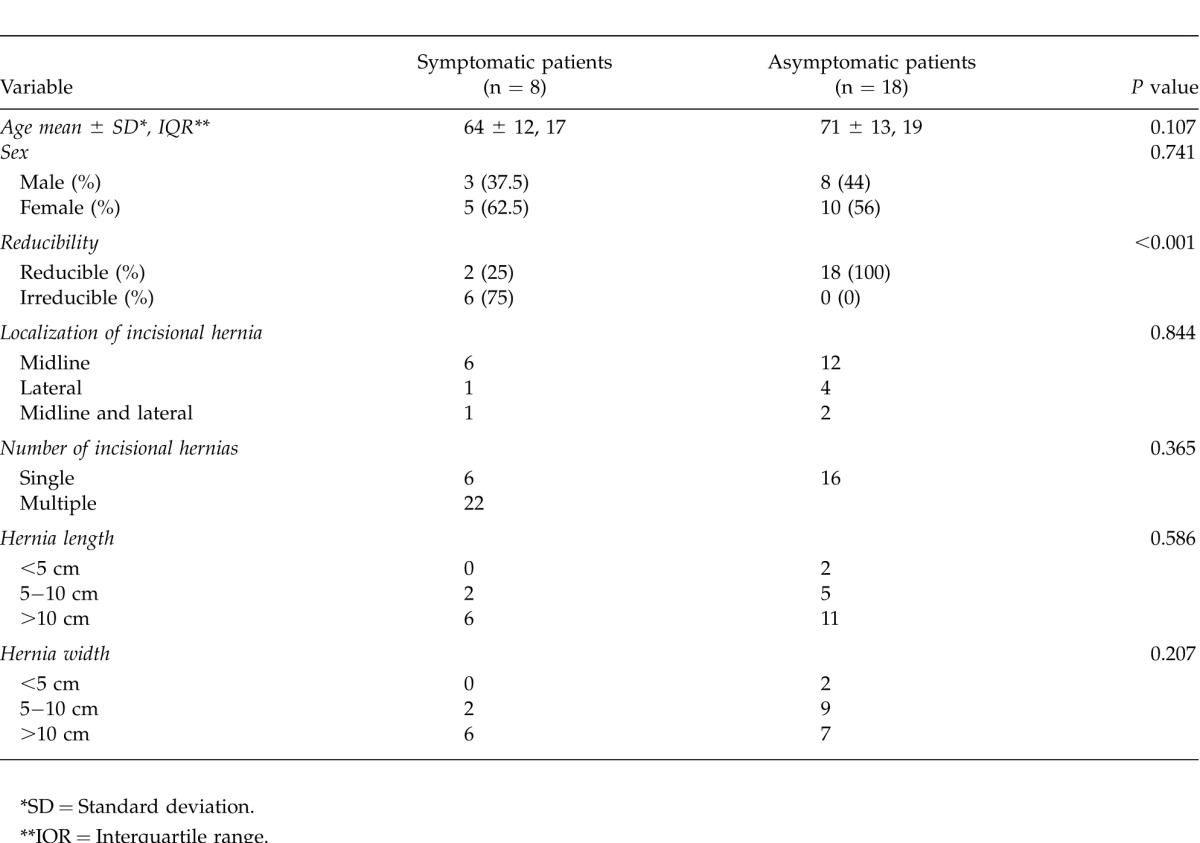
Eight of the 26 patients (30.8%) were not aware that they had an incisional hernia. These patients were significantly older (P = 0.003) and had smaller hernias (P = 0.04; Table 2). An additional 10 patients while aware of a lump recorded no symptoms from their hernia. Eight (30.8%) were symptomatic; symptoms reported were pain (n = 6), discomfort (n = 7), cosmetic complaints (n = 3), and functional disability (n = 4; Table 3). Only 1 patient expressed discomfort as a sole complaint. Pain was always associated with discomfort, cosmetic problems, or functional disability. One patient reported pain, discomfort, impaired body image, and functional disability. This patient had undergone 14 operations over 10 years and had a large incisional hernia measuring 25 cm by length and 20 cm by width. Patients with a symptomatic hernia were significantly more likely to have an irreducible hernia (Table 4).
Table 2.
Characteristics of patients aware and not aware of an incisional hernia
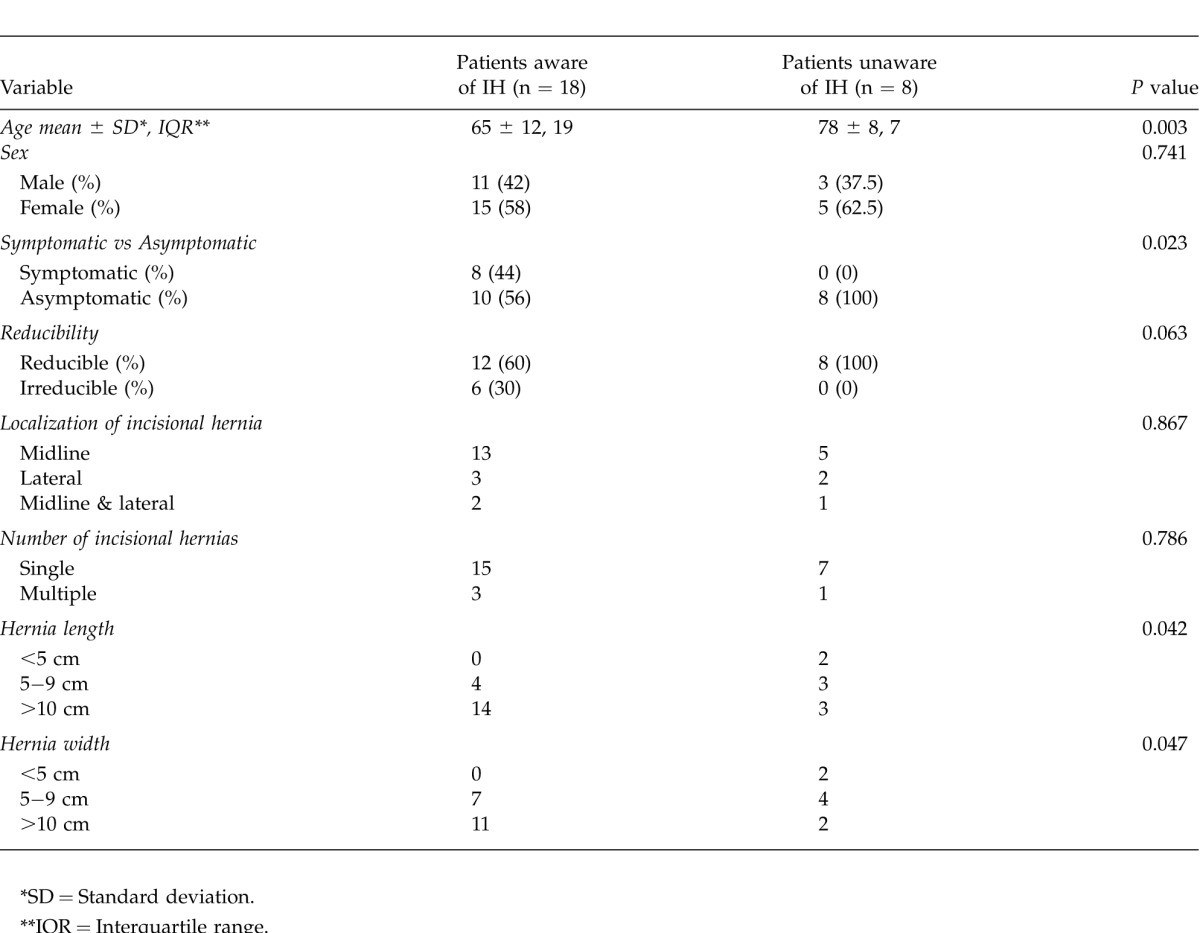
Table 3.
Characterization of complaints reported by the symptomatic patients

Table 4.
Characteristics of symptomatic and asymptomatic patients with an incisional hernia
Patients with clinical evidence of an incisional hernia have been followed up for a minimum of 2 years. None of the asymptomatic patients have had an operation while 3 (37.5%) of the symptomatic patients went on to have an incisional hernia repair; the first complained of discomfort and poor cosmetic appearance, the second had pain and discomfort, while the third complained of pain, discomfort, and poor cosmetic appearance. Symptoms were chronic in all patients and none required urgent operation.
Discussion
This study demonstrates that up to one third of patients may not be aware that they have an incisional hernia. These patients are likely to be older and have smaller hernias. Only half of the patients aware of a hernia were symptomatic. At 2 years or longer follow-up, none of the asymptomatic patients had undergone an operation whereas 37.5 % of the symptomatic patients went on to have an incisional hernia repair.
Incisional hernias may also affect patient-centered outcomes such as body image and functional status.8 Van Ramshorst et al demonstrated that patients with an incisional hernia had lower mean scores on physical components of health related quality of life and body image.9 However, the fact that these patients were significantly older and had a significantly higher BMI compared to patients without an incisional hernia may have accounted for these differences. Results from their study showed that 84% of the patients with an incisional hernia were symptomatic. Furthermore, 68% reported complaints, which is a relatively high proportion compared to similar studies by Hesselink et al2 and Pollock and Evans10 who found that complaints were reported in 53% and 12% of patients, respectively.
Incisional hernia repair is a common surgical procedure, but remains a challenge for the surgeon due to relatively poor postoperative outcomes. In a nationwide prospective study from Denmark, both elective open and laparoscopic repairs were associated with high rates of readmission and reoperation for recurrent incisional hernias. Poor early outcomes post-repair were linked to advanced age, open repair, large hernia defect, and vertical incision at the primary surgery.11 Burger et al have showed that mesh repair is associated with significantly lower rates of recurrence and discomfort postoperatively compared to suture repair. However, the 10-year cumulative recurrence rate was still high for both techniques with 63% for suture repair and 32% for mesh repair. Additionally, the complication rate after long-term follow up was 17% in the mesh-repair group versus 8% in the suture-repair group. Complications associated with mesh repair, included small bowel obstruction, mesh infection, and enterocutaneous fistula. The study concluded that it is important to justify repair for patients with an incisional hernia to avoid unnecessary surgery.12 A recent study by Lauscher and colleagues assessing benefits of incisional hernia repair for symptomatic patients and those with minimal symptoms concluded that high recurrence rates (13.3% at 18 months) and chronic pain cast doubts on the value of repair in the latter group of patients.13
It has been our routine practice not to recommend operation for patients with asymptomatic or minimally symptomatic incisional hernias. This is a policy that has been undertaken over a 25-year period. All patients undergoing cancer surgery, mostly for colorectal cancer or retroperitoneal sarcomas, are followed for life. While we are confident that around 1 in 5 of these will have developed an incisional hernia, to the best of our knowledge we are not aware of anyone from this group with an asymptomatic or minimally symptomatic hernia requiring an operation over this period. This, however, has to be interpreted with caution as up to 20% of patients will be lost to clinical follow-up. Moreover the patients main concern is more likely to reside with being disease free from their cancer rather than whether they have an incisional hernia.
One of the main strengths of our study was that multiple outcomes such as awareness and symptoms have been investigated. Moreover, outcome criteria were well defined and applied in this study. The main limitation of the study is the small sample size of the study population. Another limitation is the lack of a standard quality of life assessment such as SF-36 or Carolinas Comfort Scale (CCS).14,15 This, however, would only be of value if measured in all patients with or without an incisional hernia. In addition, any comparison between such groups would suffer from other differences that emerge from nonrandomized groups of patients.
In the past, randomized controlled trials have suggested that watchful waiting is a viable option for inguinal hernias.16−18 Similar prospective randomized studies with long follow-up evaluations for incisional hernias are necessary to compare outcomes of watchful waiting versus surgery for minimally symptomatic patients with incisional hernias. This would ultimately reduce the socioeconomic impact of incisional hernia repair. More reports on the natural course are also required in order to evaluate and modify the risk factors associated with incisional hernias.
Acknowledgments
The authors report no conflicts of interest and no funding for this study.
References
- 1.Sanders DL, Kingsnorth AN. The modern management of incisional hernias. BMJ. 2012;344:e2843. doi: 10.1136/bmj.e2843. [DOI] [PubMed] [Google Scholar]
- 2.Hesselink VJ, Luijendijk RW, de Wilt JH, Heide R, Jeekel J. An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet. 1993;176(3):228–234. [PubMed] [Google Scholar]
- 3.Bansal VK, Misra MC, Babu D, Singhal P, Rao K, Sagar R, et al. Comparison of long-term outcome and quality of life after laparoscopic repair of incisional and ventral hernias with suture fixation with and without tacks: a prospective, randomized, controlled study. Surg Endoscop. 2012;26(12):3476–3485. doi: 10.1007/s00464-012-2390-5. [DOI] [PubMed] [Google Scholar]
- 4.Nieuwenhuizen J, Halm JA, Jeekel J, Lange JF. Natural course of incisional hernia and indications for repair. Scand J Surg. 2007;96(4):293–296. doi: 10.1177/145749690709600406. [DOI] [PubMed] [Google Scholar]
- 5.Itani KM, Hur K, Kim LT, Anthony T, Berger DH, Reda D, et al. Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Arch Surg. 2010;145(4):322–328. doi: 10.1001/archsurg.2010.18. [DOI] [PubMed] [Google Scholar]
- 6.Itani KM, Neumayer L, Reda D, Kim L, Anthony T. Repair of ventral incisional hernia: the design of a randomized trial to compare open and laparoscopic surgical techniques. Am J Surg. 2004;188((6A Suppl)):22S–29S. doi: 10.1016/j.amjsurg.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 7.Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13(4):407–414. doi: 10.1007/s10029-009-0518-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nieuwenhuizen J, Kleinrensink GJ, Hop WC, Jeekel J, Lange JF. Indications for incisional hernia repair: an international questionnaire among hernia surgeons. Hernia. 2008;12(3):223–225. doi: 10.1007/s10029-007-0322-4. [DOI] [PubMed] [Google Scholar]
- 9.van Ramshorst GH, Hasan HE, Hop WC, Jeekel J, Lange JF. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012;204(2):144–150. doi: 10.1016/j.amjsurg.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg. 1989;76(9):953–954. doi: 10.1002/bjs.1800760926. [DOI] [PubMed] [Google Scholar]
- 11.Helgstrand F, Rosenber J, Kehlet H, Jorgensen LN, Bisgaard T. Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll Surg. 2013;216(2):217–228. doi: 10.1016/j.jamcollsurg.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 12.Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240(4):578–583. doi: 10.1097/01.sla.0000141193.08524.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lauscher JC, Loh JC, Rieck S, Buhr HJ, Ritz JP. Long-term follow-up after incisional hernia repair: are there only benefits for symptomatic patients? Hernia. 2013;17(2):203–209. doi: 10.1007/s10029-012-0955-9. [DOI] [PubMed] [Google Scholar]
- 14.Rogmark P, Peterson U, Bringman S, Eklund A, Ezra E, Sevonius D, et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. 2013;258(1):37–45. doi: 10.1097/SLA.0b013e31828fe1b2. [DOI] [PubMed] [Google Scholar]
- 15.Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW. Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg. 2008;206(4):638–644. doi: 10.1016/j.jamcollsurg.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 16.Fitzgibbons RJ, Jr, Giobbie-Hurder A, Gibbs JO, Dunlop DD, Reda DJ, McCarthy M, Jr, et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA. 2006;295(3):285–292. doi: 10.1001/jama.295.3.285. [DOI] [PubMed] [Google Scholar]
- 17.O'Dwyer PJ, Norrie J, Alani A, Walker A, Duffy F, Horgan P. Observation or operation for patients with an asymptomatic inguinal hernia: a randomised clinical trial. Ann Surg. 2006;244(2):167–173. doi: 10.1097/01.sla.0000217637.69699.ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fitzgibbons RJ, Jonasson O, Gibbs J, Dunlop DD, Henderson W, Reda D, et al. The development of a clinical trial to determine if watchful waiting is an acceptable alternative to routine herniorrhaphy for patients with minimal or no hernia symptoms. J Am Coll Surg. 2003;196(5):737–742. doi: 10.1016/S1072-7515(03)00003-6. [DOI] [PubMed] [Google Scholar]


