Abstract
The long-term outcomes of laparoscopic splenectomy (LS) versus open splenectomy (OS) in patients with idiopathic thrombocytopenic purpura (ITP) are not known. A retrospective analysis of 73 patients who underwent splenectomy (32 LS and 41 OS) for refractory ITP between April 2003 and June 2012 was conducted. LS was associated with shorter hospital stay (P = 0.01), less blood loss and blood transfusion during surgery, quicker resumption of oral diet (P < 0.0001), and earlier drain removal (P < 0.01). Conversion to OS was required in 4 patients (12.5%). Operation time was significantly longer in LS (P < 0.0001). Deep venous thrombosis (DVT) was observed in 1 patient after LS and in 4 patients after OS (P = 0.52). One patient died from intraperitoneal bleeding after OS, another patient developed pulmonary embolism. Median follow-up of 36 months was performed in LS group (29 of 32, 91%) and of 46 months in OS group (35 of 41, 85%), 25 patients (86%) in LS group and 32 (91%) in OS group reached sustained complete response (P = 0.792). Kaplan-Meier analysis showed that there was no significant difference in the relapse-free survival rate between the groups (P = 0.777). In conclusion, the long-term outcome of laparoscopic splenectomy is not different from that of open splenectomy for patients with ITP.
Key words: Idiopathic thrombocytopenic purpura, Splenectomy, Laparoscopy, Postsplenic complications, Relapse-free survival rate
Idiopathic thrombocytopenic purpura (ITP) is related to increased platelet destruction along with reduced platelet production via the specific autoantibodies and may cause a potentially life-threatening hemorrhage. Most ITP can be managed medically, yet some patients are refractory to medical agents such as prednisone, or anti-D globulin therapy,1 and require splenectomy. Splenectomy can be performed as open splenectomy (OS) or laparoscopic splenectomy (LS).1,2
In the past decade, LS has rapidly become recognized as the gold standard for the management of nontraumatic splenic disorders, such as ITP, thrombotic thrombocytopenic purpura, and hemolytic anemia purpuras.1–3 Systematic review studies have demonstrated a complete response or durable remission following splenectomy in 66% of adult patients with ITP.4 Several retrospective studies have compared the outcomes of OS and LS1,5–7 and have shown comparable perioperative results, and the recent guidelines of the American Society of Hematology for ITP suggested that a similar efficacy is achieved with both LS and OS, the long-term efficacy of LS for this disorder is uncertain. Therefore, we have retrospectively studied 32 consecutive LS (LS group) and compared them with a historical control group of 41 consecutive OS (OS group) performed for ITP in order to compare the outcomes of LS with OS for ITP.
Patients and Methods
A consecutive series of 41 patients underwent elective OS between April 2003 and October 2007; since then, a laparoscopic technique was introduced, and 32 patients underwent LS between November 2007 and June 2012. The clinical work and study were approved by the hospital ethical review board, and all patients provided their written consent to the treatment; the document was stored in the hospital medical database. ITP was diagnosed based principally on a medical history, physical examination, complete blood count, and examination of the peripheral smear. Inclusion conditions of the study included ITP diagnosis followed by total splenectomy. Other etiologies of thrombocytopenia rather than ITP were excluded through the peripheral blood smear, including ITP associated with systemic lupus, chronic lymphocytic leukemia, and low-grade lymphoma.
Symptomatic ITP patients or those with low platelet count (<3000/μL) were administered and treated with prednisolone initially, then azathioprine, or vincristine, or intravenous immunoglobulin in case of failure of prednisolone treatment. Indications of splenectomy for ITP were a patient who was failed standard medical treatment with low platelet count (<3000/μL), or a patient who could not tolerate the side effects of the steroid. Clinical data, including splenic weight, operative time, estimated blood loss, intraoperative blood transfusion, time of resumption of oral diet, postoperative morbidity, hospital stay, and rate of conversion to laparotomy were compared. The preoperative spleen size was determined by ultrasound, computed tomography scan, or magnetic resonance imaging and by direct measure after surgery. Complete response to splenectomy was considered if platelet count was at least 100,000/μL 3 months after splenectomy with no medical treatment or under tapering down of the steroid treatment. “No response” was defined as platelet counts falling below 100,000/μL, or requiring medical treatment to maintain platelet counts above 100,000/μL.
Surgical technique
OS patients were placed in the supine position, and the surgical table could be rotated as needed. A subcostal incision was made in patients having OS; whereas patients having LS were placed in a right lateral decubitus position, an optic trocar was placed 4 cm above the umbilicus, and 3 trocars were introduced along a hypothetical bilateral subcostal incision. Any accessory spleen was checked carefully and removed prior to mobilization of the spleen. For proximal control and dissection of the splenic artery, the spleno-colic and then the spleno-reno ligaments were freed first, the hilus artery, vein, and short gastric vessels were invariably controlled and resected by electrocautery and endoscopic vascular stapler. The spleen was then completely freed and crushed inside the plastic bag and extracted from the abdominal cavity. The pieces were reassembled by the pathologist and measured. All spleens were investigated histologically.
An aspiration drain was routinely left in place. Postoperative medical treatment included a prophylactic pneumococcal and hemophilus B vaccine, chronic antiplatelet medication, and long-term prophylactic antibiotics. Meningococcal vaccines were not routinely given.
Statistical analysis
The SPSS 13.0 (SPSS Inc, Chicago, IL) was used for all analysis. A test of normality was performed. Results are expressed as mean ± SD for parametric data. Fisher's exact test and the Mann-Whitney test were used to compare the proportions of outcomes and continuous variables in both groups, respectively. A P value less than 0.05 was accepted as statistically significant.
Results
Table 1 shows that the baseline conditions including age, platelet count, and splenic weights are similar in both LS and OS groups. The operation time was significantly longer in OS than in LS (P = 0.001). Postoperative platelet count increased significantly in both groups compared with before surgery (P < 0.0001). LS was converted to OS in 4 of 32 patients (12.5%). The reasons for conversion were uncontrollable bleeding (n = 2) and difficult laparoscopic handling of intensive dense vascular adhesions around spleen (n = 2).
Table 1.
Baseline and perioperative features of patientsa
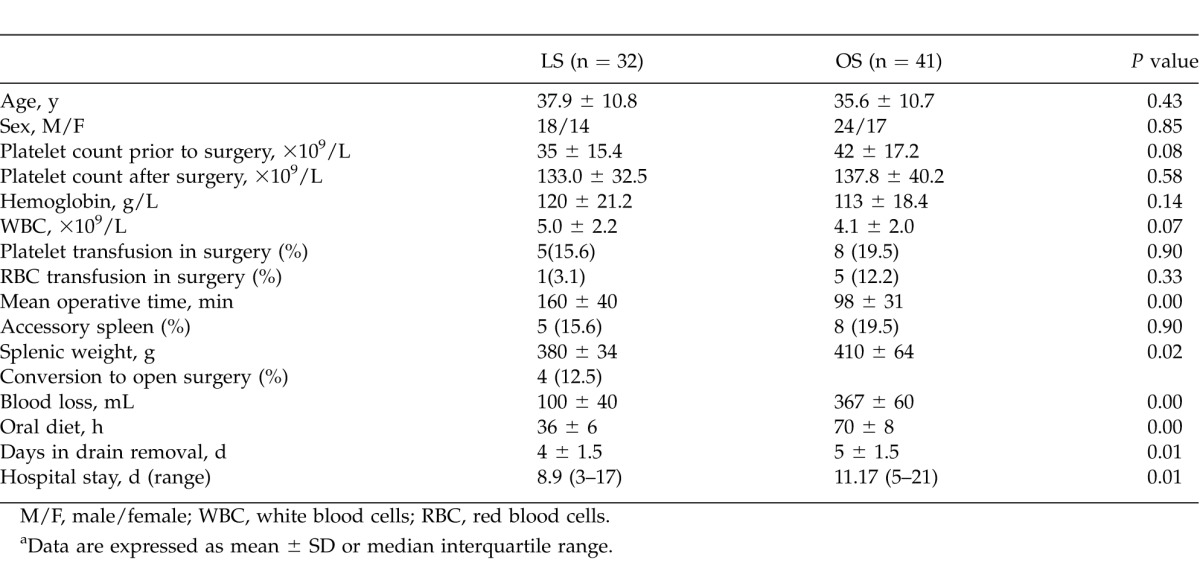
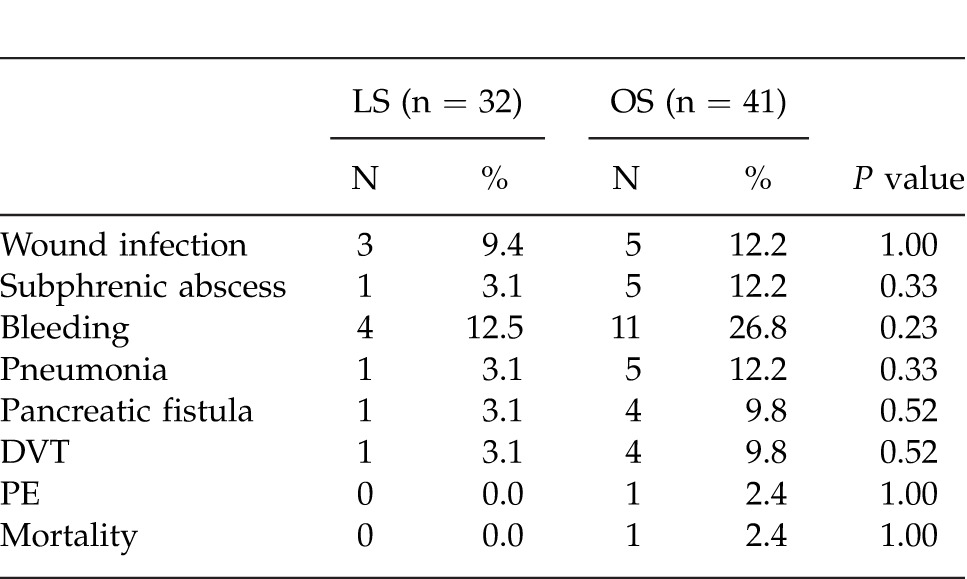
The volume of intraoperative blood loss was significantly higher in OS patients than in LS patients (P < 0.0001). Median hospital stay of patients in the LS group was shorter than for the OS group (P = 0.01). The time to resumption of oral diet after surgery in the LS group was less than in the OS group (36 ± 6 hours versus 70 ± 8 hours; P < 0.0001). No perioperative mortality occurred after LS, but in the OS group, 1 patient died from intraperitoneal bleeding and subsequent multiorgan failure 20 days following reexploration for postsplenic hemorrhage. The rate of postoperative complications, including pneumonia, subphrenic abscess, postoperative intraoperative bleeding, and pancreatic fistula and thromboembolic events was higher in the OS group but did not achieve statistical difference when compared with the LS group (Table 2). Two patients in each group had postoperative fever of unknown origin and were managed with antibiotics. Deep venous thrombosis was observed in 1 patient after LS and in 4 patients after OS (P = 0.52). One patient had a pulmonary embolism on day 6 after OS, and the platelet count reached 490 × 109/L; it was not life threatening (Table 2).
Table 2.
Perioperative complications
Platelet counts improved in 28 LS patients (87.5%) and 39 OS patients (95.1%). Median follow-up of 36 months (range, 19–49 months) was performed in 29 LS patients (91%), and median follow-up of 46 months (range, 33.5–75 months) was performed in OS patients (85%); 25 LS patients (86%) and 32 OS (91%) reached sustained response rates (P = 0.792). Median relapse-free survival time was 90 days in LS group and 108 days in OS group, respectively; Kaplan-Meier analysis showed that the difference in the relapse-free survival rate between groups was not significant (Fig. 1, P = 0.777).
Fig. 1.
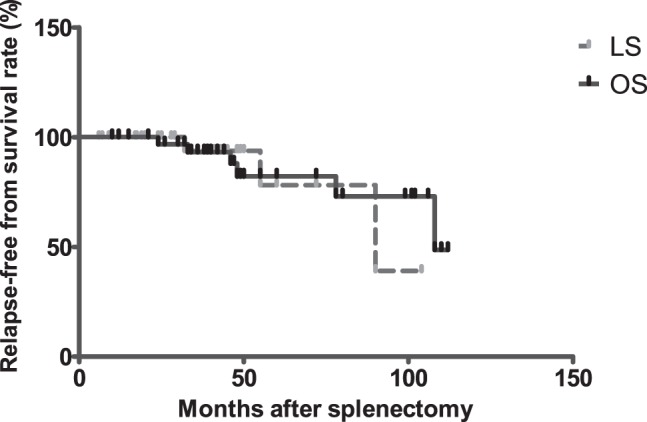
Kaplan-Meier estimates of long-term relapse-free survival rate in complete response ITP patients post splenectomy (LS versus OS, P = 0.777).
Discussion
The benefit of this study is that the long-term relapse-free survival rates are comparable in both groups, and the outcome of LS is same as OS in management of ITP patients. In addition, our retrospective study showed that LS patients had shorter hospital stay and less operative time than OS patients. Postoperative platelet count increased significantly in both groups in comparison with that before the operation.
LS has become the modality of choice for the elective treatment of many splenic diseases, particularly for ITP patients who are refractory to medical treatment. Most articles1,6 report longer surgical time for LS than for OS, but several authors8–11 have demonstrated a significant decrease in LS surgical time with gaining experience in LS. The LS is a safe procedure in comparison with OS.12–15
The common difficulty in LS was manipulation of a splenomegaly, as it consumed more operative time. A multivariate analysis performed by Friedman et al9 showed that a splenomegaly was a major determinant of operative time, postoperative stay, and costs. In comparison with open surgery, it takes more time to position the patient, make pneumoperitoneum, place the resected spleen into a bag, and finally to morcel and extract it via a trocar site. Yet, some authors8–11 reported that equal or less time was spent in LS compared with OS.
In order to prevent intraoperative bleeding, management of the splenic hilar and the short gastric vessels using an endovascular stapler can help secure hemostasis and avoid the cumbersome for laparoscopic suturing. A vascular clip used to collapse the splenic hilar vessels can dislodge and should be used carefully. We had one case of intraoperative bleeding as a result of the dislodgement of vascular clips in short gastric artery.
Conversion of LS to OS is indicated in case of difficulty controlling the operative bleeding or poor access to the splenic hilum. There were 2 patients in our group who had extensive tense vascular adhesion tissue around the splenic hilar, and the LS was converted to OS. Another 2 cases had uncontrollable operative bleeding during LS and had to be converted to OS.
Deep venous thrombosis (DVT) and or pulmonary embolism (PE) can occur after splenectomy especially when the platelet count increases above the normal range.16
Four patients had DVT, and 1 patient developed PE in our OS group and was managed successfully with anticoagulation and thrombolysis. It is helpful to monitor platelet levels closely post splenectomy and to use heparin and or warfarin prophylactically to prevent the formation of DVT or PE.
In a meta-analysis of splenectomy for ITP, Kojouri et al>4 reported that complications in LS are lower than in OS. Vecchio et al1 reported that the effect of LS is superior to OS. Our results showed that the postoperative complication rate and relapse-free survival rate were similar in the LS and OS groups. The discrepancy between our results and the literature might be owing to the limited number of patients studied.
The limitation of this study includes the retrospective study, the small number of patients reviewed, and the historical comparison of 2 study groups. This study precludes making statements regarding differences in outcomes between 2 groups. Patients in the OS group underwent open surgery and postoperative care several years earlier than those in the LS group; the postoperative care system may have improved, which could impact the outcomes of treatment.
In conclusion, laparoscopic splenectomy is associated with less operative time and a shorter hospital stay, and the long-term outcomes of LS are comparable with open splenectomy for patients with ITP. Laparoscopic splenectomy should be considered as the modality of choice in managing refractory ITP. Yet, randomized controlled trials are warranted to confirm these results.
Acknowledgments
Yikun Qu and Jian Xu contributed to this article equally.
References
- 1.Vecchio R, Marchese S, Intagliata E, Swehli E, Ferla F, Cacciola E. Long-term results after splenectomy in adult idiopathic thrombocytopenic purpura: comparison between open and laparoscopic procedures. J Laparoendosc Adv Surg Tech A. 2013;23(3):192–198. doi: 10.1089/lap.2012.0146. [DOI] [PubMed] [Google Scholar]
- 2.Qu Y, Ren S, Li C, Qian S, Liu P. Management of postoperative complications following splenectomy. Int Surg. 2013;98(1):55–60. doi: 10.9738/CC63.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kühne T, Blanchette V, Buchanan GR, Ramenghi U, Donato H, Tamminga RY, et al. Splenectomy in children with idiopathic thrombocytopenic purpura: a prospective study of 134 children from the Intercontinental Childhood ITP Study Group. Pediatr Blood Cancer. 2007;49(6):829–834. doi: 10.1002/pbc.21108. [DOI] [PubMed] [Google Scholar]
- 4.Kojouri K, Vesely SK, Terrell DR, George JN. Splenectomy for adult patients with idiopathic thrombocytopenic purpura: a systematic review to assess long-term platelet count responses, prediction of response, and surgical complications. Blood. 2004;104(9):2623–2634. doi: 10.1182/blood-2004-03-1168. [DOI] [PubMed] [Google Scholar]
- 5.Meyer G, Wichmann MW, Rau HG, Hiller E, Schildberg FW. Laparoscopic splenectomy for idiopathic thrombocytopenic purpura: a 1-year follow-up study. Surg Endosc. 1998;12(11):1348–1352. doi: 10.1007/s004649900854. [DOI] [PubMed] [Google Scholar]
- 6.Mohamed SY, Abdel-Nabi I, Inam A, Bakr M, El Tayeb K, Saleh AJ, et al. Systemic thromboembolic complications after laparoscopic splenectomy for idiopathic thrombocytopenic purpura in comparison to open surgery in the absence of anticoagulant prophylaxis. Hematol Oncol Stem Cell Ther. 2010;3(2):71–77. doi: 10.1016/s1658-3876(10)50038-4. [DOI] [PubMed] [Google Scholar]
- 7.Mikhael J, Northridge K, Lindquist K, Kessler C, Deuson R, Danese M. Short-term and long-term failure of laparoscopic splenectomy in adult immune thrombocytopenic purpura patients: a systematic review. Am J Hemat. 2009;84(11):743–748. doi: 10.1002/ajh.21501. [DOI] [PubMed] [Google Scholar]
- 8.Brunt LM, Langer JC, Quasebarth MA, Whitman ED. Comparative analysis of laparoscopic versus open splenectomy. Am J Surg. 1996;172(5):596–599. doi: 10.1016/s0002-9610(96)00241-3. discussion 599–601. [DOI] [PubMed] [Google Scholar]
- 9.Friedman RL, Hiatt JR, Korman JL, Facklis K, Cymerman J, Phillips EH. Laparoscopic or open splenectomy for hematologic disease: which approach is superior? J Am Coll Surg. 1997;185(1):49–54. [PubMed] [Google Scholar]
- 10.Glasgow RE, Yee LF, Mulvihill SJ. Laparoscopic splenectomy: the emerging standard. Surg Endosc. 1997;11(2):108–112. doi: 10.1007/s004649900308. [DOI] [PubMed] [Google Scholar]
- 11.Smith CD, Meyer TA, Goretsky MJ, Hyams D, Luchette FA, Fegelman EJ, et al. Laparoscopic splenectomy by the lateral approach: a safe and effective alternative to open splenectomy for hematologic diseases. Surgery. 1996;120(5):789–794. doi: 10.1016/s0039-6060(96)80085-7. [DOI] [PubMed] [Google Scholar]
- 12.Vecchio R, Cacciola E, Lipari G, Privitera V, Polino C, Cacciola R. Laparoscopic splenectomy reduces the need for platelet transfusion in patients with idiopathic thrombocytopenic purpura. JSLS. 2005;9(4):415–418. [PMC free article] [PubMed] [Google Scholar]
- 13.Berends FJ, Schep N, Cuesta MA, Bonjer HJ, Kappers-Klunne MC, Huijgens P, et al. Hematological long-term results of laparoscopic splenectomy for patients with idiopathic thrombocytopenic purpura: a case control study. Surg Endosc. 2004;18(5):766–770. doi: 10.1007/s00464-003-9140-7. [DOI] [PubMed] [Google Scholar]
- 14.Pace DE, Chiasson PM, Schlachta CM, Mamazza J, Poulin EC. Laparoscopic splenectomy for idiopathic thrombocytopenic purpura (ITP) Surg Endosc. 2003;17(1):95–98. doi: 10.1007/s00464-002-8805-y. [DOI] [PubMed] [Google Scholar]
- 15.Cordera F, Long KH, Nagorney DM, McMurtry EK, Schleck C, Ilstrup D, et al. Open versus laparoscopic splenectomy for idiopathic thrombocytopenic purpura: clinical and economic analysis. Surgery. 2003;134(1):45–52. doi: 10.1067/msy.2003.204. [DOI] [PubMed] [Google Scholar]
- 16.Ojima H, Kato T, Araki K, Okamura K, Manda R, Hirayama I, et al. Factors predicting long-term responses to splenectomy in patients with idiopathic thrombocytopenic purpura. World J Surg. 2006;30(4):553–559. doi: 10.1007/s00268-005-7964-0. [DOI] [PubMed] [Google Scholar]


