Abstract
Objective
This study assessed attitudes, behaviors, and barriers among general dentists in California, Pennsylvania, and West Virginia, related to patient tobacco cessation counseling.
Methods
From 2004 to 2008, a baseline survey was mailed to 271 study dentists randomly selected from a master Delta Dental Insurance Company provider list in each state who had agreed to participate in a tobacco cessation randomized clinical trial. Four backward logistic regression models assessed correlates of the five As related to tobacco cessation: Asking about tobacco use, Advising users to quit, Assessing readiness to quit, Assisting with quitting, and Arranging follow-up.
Results
Most respondents (n = 265) were male, had practiced dentistry for over 15 years, asked about tobacco use (74%), and advised tobacco users to quit (78%). Only 19% assessed readiness to quit; 39% assisted with quitting; 4% arranged follow-up; and 42% had formal training in tobacco cessation. Believing that tobacco cessation counseling was an important professional responsibility, practicing <15 years, and asking about tobacco use significantly related to advising users to quit. Providing cessation advice and feeling effective intervening related to assessing readiness to quit. Advising users to quit, assessing readiness to quit, feeling effective intervening, and having had formal tobacco cessation training related to assisting with quitting. Barriers to cessation counseling were perceived patient resistance (66%), lack of insurance reimbursement (56%), not knowing where to refer (49%), and lack of time (32%).
Conclusion
Study dentists reported not fully performing the five As. Advising, assessing, having formal training, and feeling effective increased the likelihood of cessation counseling.
Keywords: tobacco cessation, dentists, dental practices, survey
Introduction
Smoking is the single greatest cause of avoidable morbidity and mortality in the United States and represents a significant public health concern. Over 400, 000 people die each year from tobacco-related diseases (1). Moreover, smoking is associated significantly with oral cancer (2), periodontal diseases (3, 4), failure of periodontal therapy (5), failure of dental implants (6, 7), impaired oral wound healing (8, 9), oral pain (10), and dental caries (11). Currently, smoking prevalence among US adults is 19.3% (12). In 2010, approximately 68.8% of smokers in the United States wanted to quit, 52.4% tried to quit (13), and less than 6.2% achieved abstinence (13). To address the major health risk of tobacco use, the US Public Health Service came out with the Clinical Practice Guideline for the Treatment of Tobacco Use in Clinical Settings (14) and updated it in 2008 (15). This guideline recommends that all healthcare providers incorporate tobacco-use cessation counseling as part of routine clinical care. The “5 As approach” is recommended for tobacco users who are willing to quit and the “5 Rs Approach” is for tobacco users who are not willing to quit. The 5 As Approach includes: Asking patients about tobacco use; Advising users to quit; Assessing their readiness to quit; Assisting them with the quitting process; and Arranging follow-up to check on their progress (15). The “5 Rs approach” involves a motivational counseling intervention that emphasizes to the patient: the personal Relevance of quitting; the Risks of continued tobacco use; the Rewards associated with quitting; the Roadblocks to quitting; and the need for clinician ongoing Repetition of the “5 Rs” to promote patients’ decision to quit (15).
Studies report that brief interventions by nonphysician clinicians that involve only asking patients about tobacco use and advising them to quit have resulted in approximately 16% of patients who smoke to abstain for at least 1 year (15–17). In addition, several studies report that patients expect and appreciate such advice (18–20). Although dental professionals have the opportunity to play an important role in motivating and assisting their patients to quit tobacco use, tobacco cessation often is not included routinely in dental care (21–25). The purpose of this paper is to report the results of a mailed survey to assess the attitudes, behaviors and barriers of general dentists in California (CA), Pennsylvania (PA), and West Virginia (WV) related to the assessment and treatment of their patients’ tobacco use. In addition, correlates of dentists’ five A behaviors were determined. This study was part of a larger randomized controlled trial (RCT) to assess various intervention approaches to promote tobacco cessation activities by dentists.
Methods
Study design
Cross-sectional survey data collected at baseline as part of a larger RCT are reported in this paper. The Institutional Review Boards at the Delta Dental Insurance Company and at the University of California, San Francisco approved the study.
Eligibility criteria
For a dentist to be eligible for study participation, he or she needed to be a Delta Dental (DD) provider in CA, PA, or WV, who worked at least 4 days per week in general clinical practice, and who agreed to participate in a larger research study to assess various oral disease prevention approaches, such as tobacco screening and cessation counseling activities by dentists.
Sample selection and recruitment
The survey was administered to a sample of general dentists recruited from 2004 to 2008. The baseline data collection was a necessary precursor for the RCT planned as a second stage to determine whether attitudes and behaviors could be changed using various interventions (13). DD, the largest dental insurer in the nation (14), provided researchers with a list of 2, 174 randomly selected DD general dentists in CA, PA, and WV, states which all had administration in the same DD division. All the dentists were contacted for study participation by mail until the RCT target sample size of 271 (12%) agreeing to participate was reached. Subsequently, a survey along with an informed consent, cover letter, and a return-addressed stamped envelope was mailed to these dentists. A $10 bill was included as a token of appreciation. The cover letter explained the study’s purpose, methods, risks, potential benefits, alternatives, costs, and voluntary nature. It also provided information regarding the confidentiality of responses. Returning a completed questionnaire indicated informed consent. For nonrespondents, the initial mailing was followed by a second mailing 2 weeks later, and a phone call 2 weeks later if no response was received from the second mailing. Surveys were coded for ease of follow-up and to ensure confidentiality.
Survey development
Initially, we modified items reported by Dolan and colleagues (26) which were based on extensive work by an ad hoc committee of the National Dental Tobacco Free Steering Committee. The selection of survey items also was influenced by findings from our previous studies of pediatric dentists’ tobacco-related knowledge, attitudes, and behaviors (27, 28). Prior to beginning the study, we submitted all candidate survey items for review and feedback to our 16-member National Advisory Board. This Board was composed of many experts in the field of tobacco control including dentists, psychologists, representatives of professional organizations, and one lay member. Additional face and content validity were assessed when the survey was pilot tested among a convenience sample of 20 practicing dentists (11 females, nine males) in the East and South Bay areas of Northern California. Upon completion of the pilot survey, each practitioner was interviewed to gain feedback on the overall acceptability of the survey in terms of length, language clarity, and time, and on the feasibility of dentists completing and returning it. Based on this feedback, we refined or eliminated items. Although test–retest reliability was not assessed, we calculated Spearman rank correlations between items assessing three aspects of self-efficacy (feeling effective versus feeling knowledgeable, feeling effective versus feeling well prepared, and feeling knowledgeable versus feeling well prepared) that yielded consistency correlations of 0.66, 0.81, and 0.71, respectively (P = 0.0001). In addition, Cronbach’s coefficient alpha of the reliability of the 5-point Likert scale items of knowing how to assess tobacco use, feeling well-prepared to intervene, feeling effective in intervening with patients, and having sufficient knowledge of related pharmaceutical products was 0.87, indicating excellent reliability.
Survey measures
The survey assessed general dentists’ self-reported attitudes and practices related to the assessment and treatment of tobacco use, high caries risk, periodontal disease, and diabetes. This paper reports only on the tobacco-related responses.
Description of tobacco-related items
The final survey contained 49 items to assess dentists’ attitudes and behaviors related to tobacco use assessment and counseling with their patients. The attitude items assessed the dentists’ perception of: “the importance of intervening with tobacco using patients as part of their professional role,” with five response levels ranging from “very unimportant” to “very important”; potential barriers to providing tobacco cessation counseling, with five levels ranging from “not a barrier” to “a strong barrier”; knowing how to assess for tobacco use; feeling well prepared to intervene with patients regarding tobacco use; feeling quite effective intervening; and having sufficient knowledge of related pharmaceutical products, with five levels ranging from “strongly disagree” to “strongly agree.”
Behavioral items assessed the frequency of performing: components of the five A behaviors; treatment behaviors related to counseling patients who are ready to quit; and components of the five Rs related to motivating patients who are not ready to quit. All these behavioral items had four levels ranging from “almost always” to “almost never.” In addition, time spent in the past month counseling patients based on readiness to quit was assessed with seven response options (“Did not discuss,” “<1 minute,” “1–3 minutes,” “4–10 minutes,” “11–30 minutes,” “31–60 minutes,” and “60 minutes”).
Additional items also asked questions related to formal training in tobacco use assessment and treatment (i.e., dental school course/lecture, or Continuing Dental Education) (Yes/ No) and the likelihood to perform tobacco use assessment and treatment behaviors if it was included as a benefit in the patient’s dental insurance (“very unlikely” to “very likely”).
Data analysis
Data were coded without personal identifiers and entered into password-protected computer files and hard copies securely stored. Data analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Descriptive summaries were performed for all questionnaire variables. Items assessing attitudes and potential barriers on a 5-point Likert scale ranging from “very unimportant” to “very important,” “not a barrier” to “a strong barrier,” and “strongly disagree” to “strongly agree” were dichotomized into “Important/Extremely Important,” “Agreed/Strongly Agreed,” and “Barrier/Strong Barrier,” respectively. Items assessing frequency of reported five A or five R behavior on a 4-point Likert scale ranging from “Almost Never” to “Almost Always” were dichotomized to create measures of “Almost never vs. Almost Always.” Analyses included frequency distributions; chi-square, and Fisher’s exact tests when categorical variables were compared, and t-tests and Mann–Whitney tests for continuous variables. Univariate analyses were conducted initially to identify candidate variables to be included in the multivariable analyses. Four separate backward logistic regression models assessed correlates of the following dependent five A behaviors, respectively: Ask, Advise, Assess, and Assist. The “Arrange” variable was not modeled due to the small number of dentists who reported arranging follow-up. Variables with P values ≤0.05 were retained in the model, while those >0.05 were removed. The independent variables included in the multivariable regression models were identified based on univariate analysis and by findings reported in other studies (8). The regression model for the dependent variable “Ask” included as independent variables the following: tobacco cessation training, feeling well-prepared, feeling effective, perceived importance of one’s role in tobacco cessation counseling, age, gender, and number of years in practice. For the dependent variable “Advise,” multi-variable models included these above-listed independent variables plus “Ask” was added as an independent variable. Similarly, the model for the dependent variable “Assess” added the variables “Ask” and “Advise” as independent variables along with the base variables; the model for the dependent variable “Assist” added the variables “Ask,” “Advise,” and “Assess” as independent variables in addition to base variables.
Results
Of the 271 mailed surveys, 265 (98%) were completed and returned (42% from CA, 35% from PA, and 23% from WV). Among the respondents, 86% were male, 80% were Caucasian, 3% smoked daily, and 23% had smoked more than 100 cigarettes in their lifetime, and 42% had prior formal tobacco cessation training. In terms of practice characteristics, 74% had practiced for at least 15 years; 89% asked about tobacco use on the health history form; over half had patient tobacco cessation-related educational materials (58%) and reported adequate staff to address tobacco use (53%); over one-fifth-had a formal system to remind staff to ask about tobacco use (22%) and offered tobacco cessation services (21%). Only 12% reported having an office policy to intervene regarding tobacco use. With regard to time spent counseling patients about quitting, 14% reported they did not discuss tobacco use; 14% spent less than 1 minute; 39% spent 1–3 minutes; and 33% spent more than 3 minutes but less than 30 minutes. Table 1 shows dentists’ attitudes toward intervening with tobacco-using patients in the dental office. Over half felt that it was very important as part of their role as a dentist to intervene, but less than a third felt quite effective doing so, or felt well-prepared.
Table 1.
Dentists’ Attitudes and Behaviors towards Intervening with Tobacco-Using Patients in the Dental Office
| (n = 265) | % |
|---|---|
| Attitudes | |
| It is very important as part of the dentist’s role to intervene regarding patients’ tobacco use* | 58 |
| I know how to assess patients for tobacco use** | 46 |
| I feel well-prepared to intervene** | 26 |
| I am quite effective intervening with patients** | 18 |
| I have sufficient therapeutic knowledge of the appropriate pharmaceutical products | 14 |
| Behavior*** | |
| Verbally asked about tobacco use | 74 |
| Documented the patient’s tobacco use in chart | 74 |
| Pointed out oral health effects of tobacco use in patients’ mouth | 78 |
| Advised tobacco users to quit | 78 |
| Assessed readiness to quit | 19 |
| Assist with quitting (talk about ways to quit) | 39 |
| Arrange follow-up | 4 |
Scored 4 or 5 (Important/Very Important) on a 5-point scale ranging from 1 = ”Very Unimportant” to 5 = ”Very Important.”
Scored 4 or 5 (Agree/Strongly Agree) on a 5-point scale ranging from 1 = ”Strongly Disagree” to 5 = ”Strongly Agree.”
Scored 3 or 4 (Often/Almost Always) on a 4-point scale ranging from 1 = ”Almost Never” to 4 = ”Almost Always.”
Table 1 also shows the percentage of dentists who reported performing the various components of the five A behaviors. While most dentists verbally asked patients about tobacco use and advised users to quit, less than one fifth assessed readiness to quit, about one-third provided quitting assistance, and few arranged follow-up care.
The frequency of dentists who reported performing additional components of “Assist” behaviors related to counseling patients ready to quit is in shown in Table 2. About one-third “often or almost always” asked about reasons for quitting and recommended nicotine replacement therapy; almost one-quarter provided written materials on quitting tobacco use; and less than 20% reported doing anything else routinely to assist with the quitting process.
Table 2.
Percentage of Dentists Who Reported Performing “Often/Almost Always” for Patients Ready to Quit
| Behavior* (n = 265) | % |
|---|---|
| Ask reasons for quitting | 39 |
| Provide written materials on quitting | 20 |
| Assess patterns of tobacco use | 18 |
| Assess level of nicotine dependence | 11 |
| Assess for symptoms of depression | 4 |
| Help set a quit date | 6 |
| Suggest ways to cope with temptation to use | 19 |
| Encourage to tell others for support | 18 |
| Recommend nicotine replacement therapy | 36 |
| Prescribe sustained-release Buproprion (e.g., Zyban) | 3 |
| Offer in-office tobacco cessation assistance | 2 |
| Refer to a toll-free telephone tobacco quitline | 7 |
| Fax patients’ consent form to quitline so that they can be contacted by a telephone counselor for help in quitline | 1 |
| Refer to external tobacco quit program | 6 |
Scored 3 or 4 (Often/Almost Always) on a 4-point scale ranging from 1 = ”Almost Never” to 4 = ”Almost Always.”
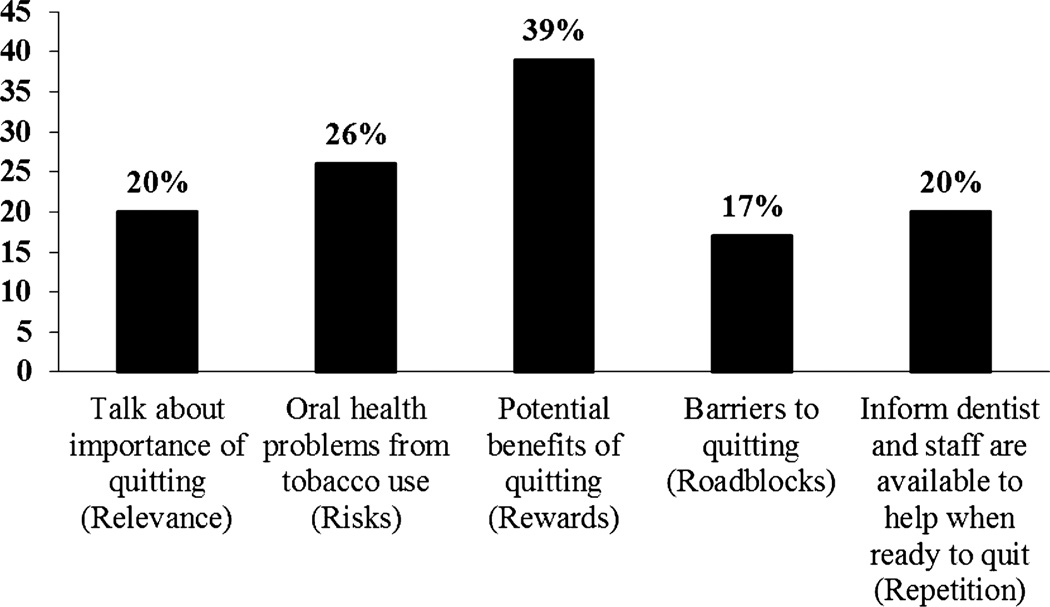
Figure 1 shows the frequency of dentists who reported performing the five Rs appropriate for motivational counseling of patients identified as being not ready to quit. About one-third talked about potential benefits of quitting and about one-quarter discussed problems experienced from tobacco use.
Figure 1.
Percentage of dentists reported “often/almost always” using five Rs’ approach when counseling patients not ready to quit.
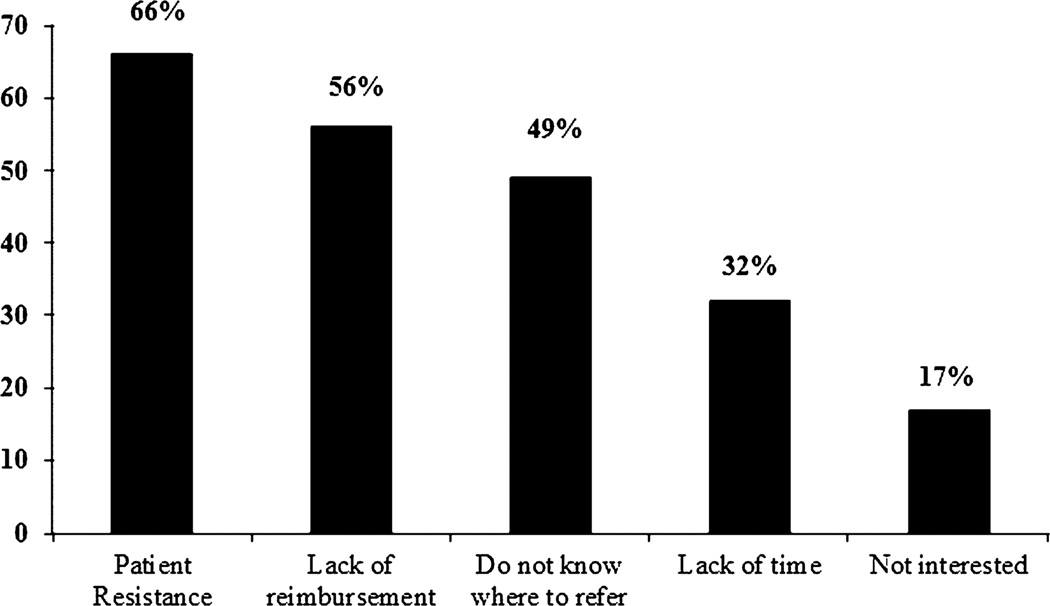
Figure 2 shows perceived barriers to providing tobacco cessation services. The most frequently reported barriers were patient resistance and lack of reimbursement. Seventy-seven percent reported that they would “likely or very likely” provide tobacco cessation counseling if it was included as a benefit in their patients’ dental insurance. There were no significant differences in dentists’ reported barriers based on gender or number of years in practice.
Figure 2.
Dentists’ reported barriers towards intervening with tobacco-using patients in the dental office.
Table 3 includes results of the univariate analyses that identified candidate variables selected for use in the multivariable analyses. Candidate variables that were significantly associated with five A behaviors were “receiving formal training in tobacco cessation activities,” “feeling intervening with tobacco users was an important role of the dentist,” “feeling one knew how to assess tobacco use,” “feeling well-prepared to intervene,” and “feeling effective in intervening with patients.” Data for the “Arrange follow-up” behavior are not included in the table due to insufficient responses that would allow for meaningful analyses.
Table 3.
Univariate Analyses Used to Identify Candidate Variables for Use in Multivariable Analyses to Determine Correlates of Dentists’ Performance of Components of the Five A Behaviors
| Ask* | Advise* | Assess* | Assist* | |
|---|---|---|---|---|
| (N = 265) | (%) | (%) | (%) | (%) |
| Received training in school/CE | ||||
| Yes | 49 | 58 | 11 | 26 |
| No | 34 | 43 | 4 | 7 |
| OR† (95% CI) | 1.9 (1.1–3.1) | 1.8 (1.1–3.0) | 3.0 (1.1–8.2) | 4.4 (2.0–9.3) |
| Feel dentist play important role | ||||
| Important/Very important‡ | 48 | 61 | 11 | 23 |
| Unimportant/Very unimportant | 31 | 31 | 2 | 5 |
| OR (95% CI) | 2.0 (1.2–3.4) | 3.6 (2.1–5.9) | 6.8 (1.5–30.1) | 6.3 (2.4–16.8) |
| Dentist is/was a smoker | ||||
| Yes | 30 | 48 | 5 | 12 |
| No | 44 | 49 | 8 | 16 |
| OR (95% CI) | 0.5 (0.3–1.0) | 0.9 (0.5–1.7) | 0.6 (0.2–2.2) | 0.7 (0.3–1.6) |
| Know how to assess | ||||
| Agree§ | 55 | 67 | 12 | 26 |
| Disagree | 29 | 33 | 3 | 6 |
| OR (95% CI) | 3.0 (1.8–4.9) | 4.1 (2.4–6.8) | 4.8 (1.5–14.7) | 5.9 (2.6–13.4) |
| Feel effective intervening | ||||
| Agree§ | 49 | 66 | 21 | 40 |
| Disagree | 39 | 45 | 4 | 10 |
| OR (95% CI) | 1.4 (0.8–2.8) | 2.4 (1.2–4.6) | 6.3 (2.4–16.4) | 6.4 (3.1–13.3) |
| Feeling well-prepared | ||||
| Agree§ | 55 | 71 | 16 | 33 |
| Disagree | 36 | 40 | 4 | 9 |
| OR (95% CI) | 2.2 (1.3–3.9) | 3.6 (2.0–6.5) | 4.4 (1.7–11.5) | 5.2 (4.8–10.6) |
Arrange behavior not reported due to insufficient responses for analyses.
Scored 4 Almost Always on a 4-point scale ranging from 1 = ”Almost Never” to 4 = ”Almost Always.”
Chi-square test.
Scored 4 or 5 (Important/Very Important) on a 5-point scale ranging from 1 = ”Very Unimportant” to 5 = ”Very Important.”
Scored 4 or 5 (Agree/Strongly Agree) on a 5-point scale ranging from 1 = ”Strongly Disagree” to 5 = ”Strongly Agree.”
Table 4 shows correlates of dentists five A behaviors based on multivariable analyses. Dentists who agreed that they knew how to assess tobacco use were significantly more likely to ask their patients about tobacco use (odds ratio = 3.0; 95% confidence interval; 1.8–5.1). Dentists who reported they knew how to assess tobacco use, felt tobacco cessation intervention was important to their role as a dentist, were in practice less than 15 years, and asked about tobacco use were significantly likely to advise users to quit. In addition, dentists who reported feeling effective intervening and those who advised users to quit were significantly likely to assess readiness to quit. Significant correlates of assisting with the quitting process were knowing how to assess tobacco use, advising users to quit, assessing readiness to quit, feeling effective intervening, having had formal training in tobacco cessation and younger age (younger dentists).
Table 4.
Correlates of Dentists’ Five A Behaviors – Multivariable analysis*
| Dependent | Independent | OR | 95% CI | P value |
|---|---|---|---|---|
| Ask | Know how to assess | 3.0 | 1.8–5.1 | <0.001 |
| Advise | Ask | 7.3 | 3.9–13.9 | <0.001 |
| Feel they have important role | 3.0 | 1.6–5.7 | 0.001 | |
| Know how to assess | 3.1 | 1.7–5.8 | <0.001 | |
| Age | 1.06 | 1.01–1.1 | 0.026 | |
| <15 years in practice | 2.5 | 1.1–6.0 | 0.032 | |
| Assess | Advise | 8.4 | 1.0–71.4 | 0.05 |
| Feel effective intervening | 4.8 | 1.6–14.1 | 0.004 | |
| Assist | Advise | 6.0 | 1.9–19.2 | 0.003 |
| Assess | 41.6 | 6.8–255.0 | <0.001 | |
| Feel effective | 3.2 | 1.1–8.7 | 0.027 | |
| Received training | 2.8 | 1.05–7.4 | 0.041 | |
| Age | 0.93 | 0.9–0.99 | 0.014 | |
| Arrange† | Too few responses |
Backward logistic regression models.
Arrange behavior not reported due to insufficient responses for analyses.
Discussion
Most dentists in this study believed that intervening with patients about their tobacco use was an important professional responsibility. This finding is encouraging in that willingness to address this important public health issue in the dental setting appears to exist. This perception among our study dentists is consistent with findings reported for other health professionals (23, 24).
We found that 74% of our study dentists “often or almost always” Asked their patients about tobacco use. This finding is higher than that reported by previous studies (21, 26, 29, 30). In 1997, Dolan et al. reported that 33% of a national random sample of 934 general dentists (26) asked most or nearly all patients whether they smoked. In 2005, Albert et al. reported that 28% of dentists participating in a national managed care plan in 29 states (21) asked their patients if they used tobacco at least 41% or more of the time. In 2011, Succar et al. reported that 59% of a random sample of 6, 000 dentists practicing in Florida routinely asked about tobacco use (29). The discrepancy between our findings and those of others (21, 26, 29, 30) may be due to regional effects, or to differences in study eligibility criteria, and survey measurement.
Moreover, among the general dentists in our study, 78% reported “often or always” advising known tobacco users to stop using tobacco compared to 65% reported by Dolan et al. (26), 46% reported by Albert et al. (21), and 46% reported by Succar et al. (29). This discrepancy again may be explained by measurement differences. Dolan and colleagues (26) reported the percentage who indicated that they “ever” advised patients who use tobacco to quit, whereas we report the percentage of dentists who reported that they “always or often” advised patients who used tobacco to quit.
Another possible explanation for the higher prevalence of asking and advising behaviors in our study may be the temporal effect of changes between study time periods. It is likely that it is now more acceptable to “Ask and Advise” precisely because of the increased translation of evidence related to the connection between tobacco use and adverse oral health effects (2–11) especially with regard to oral cancer (31), smoking, and periodontal disease (4, 5, 7), and the success of dental implants (6, 7). Our findings fall just short of the US Department of Health and Human Services Healthy People 2020 objective to increase to at least 85% the proportion of dentists who advise cessation (32). Because of the cross-sectional nature of our study, however, they should be interpreted with caution.
Although most dentists in this study Asked and Advised patients about tobacco use, Assess, Assist and Arrange behaviors overall were low. Only 19% of dentists reported they Assessed readiness to quit, an essential step in providing appropriate assistance with the quitting process. For Assist behaviors, about one-third (39%) reported that they talked about ways to quit or cut down tobacco use with patients, a slight improvement compared to the 29% reported by Dolan et al. (26). In this study, only 4% reported Arranging follow-up care to check on and support their patients’ quit attempt.
Moreover, less than half of the study dentists (20%) reported having tobacco cessation patient educational materials in their dental office; and only half (51%) reported knowing where to refer patients for help with stopping their tobacco use. Despite differences in measurement, there appears to be consistent reporting in the literature (21, 26–29) of low involvement in assisting patients with the quitting process in dental practices. Perhaps, this lack of engagement is due to feeling unprepared to do so.
Indeed, few of our study dentists felt well-prepared to intervene with patients about their tobacco use, or felt effective doing so. These findings may be explained by the fact that less than half of them (42%) reported having had formal training in tobacco cessation. Interventions are needed to address this void. It is important to note that in this study, having had formal training was a significant predictor of actually assisting patients with the quitting process. This finding, consistent with that of Albert et al. (21), emphasizes the importance of training for adoption of the new guidelines to treat tobacco use in dental practice and supports the premise that formal training helps in developing confidence and feelings of effectiveness.
In our study, dentists who agreed that they knew how to assess for tobacco use were significantly more likely to ask their patients about tobacco use; dentists who asked about tobacco use were significantly more likely to advise tobacco users to quit; dentists who advised patients to quit were significantly more likely to assess readiness to quit; and dentists who assessed readiness to quit were significantly more likely to assist patients with the quitting process. These findings also are consistent with those of Albert et al. (21) and support their conclusion that if we encourage dentists to ask about tobacco use and advise their patients to quit and to seek formal tobacco cessation training, then assisting patients with the quitting process and feeling effective in doing so will eventually follow. Our findings extend those of Albert et al. (21), however, in that formal training in tobacco cessation and feeling effective intervening was also significantly correlated with the assist behavior.
Moreover, dentists who felt that intervening with patients about their tobacco use was an important part of their professional role were more likely to provide cessation advise; and dentists who provided advise and who felt effective intervening were more likely to perform the Assess and Assist behaviors than dentists who did not perceive tobacco cessation as important to their professional role and who did not feel effective intervening. Similar findings have been reported in the literature for pediatric dentists (27) and for healthcare professionals in general (23, 24). In a national survey of health professionals, three factors emerged consistently across most healthcare professional groups that were positively associated with tobacco-use cessation counseling: belief that it was part of one’s professional role, perceived self-efficacy to engage in effective counseling, and knowledge of community cessation resources (10).
Consistent with the findings of others (21, 27, 28), our data suggest that formal tobacco cessation training for dentists is needed to increase their sense of self-efficacy with regard to tobacco cessation counseling (i.e., feeling effective when intervening with tobacco-using patients). Few dentists in this study used tobacco, consistent with reports that smoking prevalence among dentists is the lowest among all health professionals (23, 33).
The present study has some limitations. The data obtained via the survey instrument may not represent current practices of all dentists in the United States. Subjects were recruited from a list of DD insurance dentists who had been recruited to participate in a two-stage tobacco intervention study. As a result, they may have had greater interest in tobacco cessation compared to the general dentist population. This limited inclusion criterion may have created selection bias which would limit generalizability. However, almost three quarters of dentists nationally subscribe to DD (34), and the effect on generalizability may not be substantial. Nevertheless, generalizing findings to all dentists who are DD providers should be made cautiously. Although 98% of surveys of dentists who agreed to participate in the study were returned, initial recruitment participation in the study was low (12%), and recruitment was halted once the target number of dentists for the trial were recruited. The failure to include more recent graduates from dental school also limits our findings. It should be noted, however, that even the overly conservative study participation rate is consistent with those reported by others for dental intervention studies (21, 35) and all participating dentists recruited to participate in the subsequent tobacco intervention study completed the baseline survey. Moreover, the demographic and practice characteristics of our sample are comparable to those of the dentists’ samples reported in national surveys (36, 37).
Most dentists in our study sample did not fully perform the “5As” or the “5 Rs.” Major barriers cited for not doing so were “patient resistance,” “lack of reimbursement,” “lack of time,” and “not knowing where to refer.” These barriers are consistent with findings of other studies reporting the most frequent reasons dentists cite for not providing tobacco cessation counseling (21, 26). Other studies also cited “lack of training,” “advice not effective,” and “forget to bring it up” (21, 26). Similar to those studies, we also found that most of our study dentists did not feel confident or well prepared to treat tobacco-using patients.
It is important to note that in this study previous formal training made a significant difference in feelings of confidence and dentists’ reported behavior. Since tobacco use is such an important US public health issue, it is very important for both private practice and public health dentists to have the knowledge and skills to identify tobacco users in their practices and, at a minimum, to refer them to community-based programs for further help with quitting. Valuable resources for acquiring tobacco cessation-related information for dentists have been published by the American Dental Association (ADA) (31). The ADA Web site also provides information on oral health and tobacco use, and some research information which can be useful to both patients and healthcare professionals. These resources can help dentists to acquire more information about: assessment and management of tobacco use and dependence in the dental setting. Skills-based approaches may be needed to enhance feelings of self-confidence, preparedness, and effectiveness.
Dental professionals are favorably positioned to provide brief tobacco cessation treatment using the five As approach since dental care often involves multiple visits providing opportunity to initiate and reinforce tobacco cessation activities (21). Since more than 50% of smokers see a dentist during a year (38, 39), if all dentists routinely engaged in brief tobacco cessation counseling, then approximately 23 million of the estimated 46 million adult smokers in the United States could be treated by a dentist to quit smoking in a single year. This type of public health intervention could reduce the burden of tobacco-related disease in the United States. Moreover, if 10% of smokers who see a dental professional annually could be influenced to consider quitting, then each year, 2.3 million US tobacco users could be treated. Given that one-third of all smokers die prematurely (40), an estimated 766, 667 premature deaths from smoking could be prevented by dental professionals being involved in tobacco cessation counseling.
Conclusion
Dentists can play an important role in primary prevention of adverse health effects by promoting cessation of tobacco use among patients to whom they provide care. Although most dentists in this study considered intervening with patients about their tobacco use an important part of their professional responsibility; and asked and advised patients about tobacco use, few felt well prepared, effective, or had formal training in cessation counseling. Educational interventions are needed to increase smoking cessation activities by dentists. In this study, dentists who felt effective and considered their role as important were likely to fully perform the five A behaviors when intervening with their patients about tobacco use.
Acknowledgments
Funded by US DHHS NIH NIDA grant 1 R01DA017973; Delta Dental of California Delta Dental of California; and by NIH/NCRR UCSF-CTSI Grant Number UL1 RR024131. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors wish to thank the 267 dentists who participated in this study; Carl Ludwig and Michael McGinley for coordination of Delta Dental’s participation and Joanna Hill for technological assistance.
References
- 1.U.S. Centers for Disease Control and Prevention. Annual smoking-attributed mortality, years of potential life lost, and productivity losses: United States, 1997–2001. MMWR. 2005;54:625–628. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. The health consequences of smoking a report of the surgeon general. Washington, DC: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 3.Molloy J, Wolff LF, Lopez-Guzman A, Hodges JS. The association of periodontal disease prameters with systemic medical conditions and tobacco use. J Clin Periodontol. 2004;31:625–632. doi: 10.1111/j.1600-051X.2004.00539.x. [DOI] [PubMed] [Google Scholar]
- 4.Tomar S, Asma S. Smoking-attributable periodontitis in the U.S.: findings from NHANES III National Health and Nutritional Survey. J Periodontol. 2000;71:743–751. doi: 10.1902/jop.2000.71.5.743. [DOI] [PubMed] [Google Scholar]
- 5.Bergstrom J, Eliasson S, Dock J. A 10-year prospective study of tobacco smoking and periodontal health. J Periodontol. 2000;71:1338–1347. doi: 10.1902/jop.2000.71.8.1338. [DOI] [PubMed] [Google Scholar]
- 6.Chuang SK, Wei LJ, Douglass CW, Dodson TB. Risk factors for dental implant failure: a strategy for the analysis of clustered failure-time observations. J Dent Res. 2002;81:572–577. doi: 10.1177/154405910208100814. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Periodontology Research Science and Therapy Committee. Position paper: tobacco use and the periodontal patient. J Periodontol. 1999;70:1419–1427. doi: 10.1902/jop.1999.70.11.1419. [DOI] [PubMed] [Google Scholar]
- 8.Jones J, Triplett R. The relationship of cigarette smoking to impaired intraoral wound healing: a review of evidence and implications for patient care. J Oral Maxillofac Surg. 1992;50:237–239. doi: 10.1016/0278-2391(92)90318-t. [DOI] [PubMed] [Google Scholar]
- 9.Preber H, Bergstrom J. Effect of smoking on periodontal healing following surgical therapy. J Clin Periodontol. 1990;17:324–328. doi: 10.1111/j.1600-051x.1990.tb01098.x. [DOI] [PubMed] [Google Scholar]
- 10.Riley J, Tomar S, Gilbert G. Smoking and smokeless tobacco: increased risk for oral pain. J Pain. 2004;5:218–225. doi: 10.1016/j.jpain.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Tomar SL, Winn D. Chewing tobacco use and dental caries among U.S. men. J Am Dent Assoc. 1999;130(11):1601–1610. doi: 10.14219/jada.archive.1999.0099. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Smoking and tobacco use: trends in current cigarette smoking among high school students and adults, United States, 1965–2010. Atlanta, GA: US Department of Health and Human Services, CDC; 2011. [Accessed Jan 27, 2012]. Available from: http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Quitting smoking among adults United States. 2001–2010 and 1991. Morb Mortal Wkly Rep. 2011;60:1513–1519. [PubMed] [Google Scholar]
- 14.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, Heyman RB, Jaén CR, Kottke TE, Lando HA, Macklenburg RE, Mullen PD, Nett LM, Robinson L, Stitzer ML, Tommasello AC, Villejo L, Wewers ME, Backer TB, Fox BJ, Hasselblad V. Treating Tobacco Use and Dependence. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2000. Jun, [Google Scholar]
- 15.Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, Dorfman SF, Froelicher ES, Goldstein MG, Healton CG, Henderson PN, Heyman RB, Koh HK, Kottke TE, Lando HA, Mecklenburg RE, Mermelstein RJ, Mullen PD, Orleans CT, Robinson L, Stitzer ML, Tommasello AC, Villejo L, Wewers ME. Treating Tobacco Use and Dependence, 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. May, [Google Scholar]
- 16.Gordon JS, Andrews JA, Lichtenstein E, Severson HH. The impact of a brief tobacco-use cessation intervention in public health dental clinics. J Am Dent Assoc. 2005;136(2):179–186. doi: 10.14219/jada.archive.2005.0139. [DOI] [PubMed] [Google Scholar]
- 17.Warnakulasuriya S. Effectiveness of tobacco counseling in the dental office. J Dent Educ. 2002;66(9):1079–1087. [PubMed] [Google Scholar]
- 18.Campbell H, Sletten M, Petty T. Patient perceptions of tobacco cessation services in dental offices. J Am Dent Assoc. 1999;130(2):219–226. doi: 10.14219/jada.archive.1999.0171. [DOI] [PubMed] [Google Scholar]
- 19.Owen N, Davies MJ. Smokers’ preferences for assistance with cessation. Prev Med. 1990;19(4):424–431. doi: 10.1016/0091-7435(90)90040-q. [DOI] [PubMed] [Google Scholar]
- 20.Severson H, Eakin E, Stevens V, Lichtenstein E. Dental office practices for tobacco users. independent practice HMO clinics. Am J Public Health. 1990;80(12):1503–1505. doi: 10.2105/ajph.80.12.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albert DA, Severson H, Gordon J, Ward A, Andrews J, Sadowsky D. Tobacco attitudes, practices, and behaviors: a survey of dentists participating in managed care. Nicotine Tob Res. 2005;7(Suppl 1):S9–S18. doi: 10.1080/14622200500078014. [DOI] [PubMed] [Google Scholar]
- 22.Hu S, Pallonen U, McAllister AL, Howard B, Kaminski R, Stevenson G, Servos T. Knowing how to help tobacco users. Dentists’ familiarity and compliance with the clinical practice guideline. J Am Dent Assoc. 2006;137(2):170–179. doi: 10.14219/jada.archive.2006.0141. [DOI] [PubMed] [Google Scholar]
- 23.Tong EK, Strouse R, Hall J, Kovac M, Schrowder SA. National survey of U.S. health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. 2010;12(7):724–733. doi: 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tremblay J, Cournoyer D, O’Laughlin J. Do the correlates of smoking cessation counseling differ across health professional groups? Nicotine Tob Res. 2009;11:1330–1338. doi: 10.1093/ntr/ntp142. [DOI] [PubMed] [Google Scholar]
- 25.Watt RG, McGlone P, Dykes J, Smith M. Barriers limiting dentists’ active involvement in smoking cessation. Oral Health Prev Dent. 2004;2:95–102. [PubMed] [Google Scholar]
- 26.Dolan T, McGorray S, Skigen C, Mecklenburg R. Tobacco control activities in US dental practices. J Am Dent Assoc. 1997;128:1669–1679. doi: 10.14219/jada.archive.1997.0129. [DOI] [PubMed] [Google Scholar]
- 27.Gansky SA, Ryan JL, Ellison JA, Isong U, Miller AJ, Walsh MM. Patterns and correlates of tobacco control behavior among American Association of Pediatric Dentistry members: a cross-sectional national study. BMC Oral Health. 2007;7:13–23. doi: 10.1186/1472-6831-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yee C, Gansky S, Ellison J, Miller A, Walsh M. Tobacco control in pediatric dental practices: a survey of practitioners 2006 national study. J Pediatr Dent. 2009;30(15):211–215. [PMC free article] [PubMed] [Google Scholar]
- 29.Succar CT, Hardigan PC, Fleisher JM, Godel JH. Survey of tobacco control among Florida dentists. J Community Health. 2011;36(2):211–218. doi: 10.1007/s10900-010-9299-5. [DOI] [PubMed] [Google Scholar]
- 30.Simoyan OM, Badner VM, Freeman KD. Tobacco cessation service in dental offices. Are we doing all we can? NY State Dent J. 2002;68:34–40. [PubMed] [Google Scholar]
- 31.American Dental Association. [Accessed Aug 5, 2011];Oral health topics: smoking and tobacco cessation. Available from: http://www.ada.org/5170.aspx?currentTab=1.
- 32.U.S. Department of Health and Human Services. [Accessed January 27, 2012];Healthy People.gov. 2020 Available from: http://healthypeople.gov/2020.
- 33.Smith DR, Leggat PA. A comparison of tobacco smoking among dentists in 15 countries. Int Dent J. 2006;56(5):283–288. doi: 10.1111/j.1875-595x.2006.tb00102.x. [DOI] [PubMed] [Google Scholar]
- 34. [Accessed January 27, 2012];Delta Dental Insurance Company Website [homepage on the internet]. Update Cited 1-20-2009. Available from: http://www.deltadental.com/Public/Company/stats2.jsp?DView=AboutDeltaDentalStats.
- 35.Gerbert B, Coates T, Sahnd E. Dentists as smoking cessation counselors. J Am Dent Assoc. 1989;118:29–32. doi: 10.14219/jada.archive.1989.0017. [DOI] [PubMed] [Google Scholar]
- 36.American Dental Association Survey Center. 2004 survey of dental practice: characteristics of dentists in private practice and their patients. Chicago, IL: The American Dental Association; 2006. [Google Scholar]
- 37.American Dental Association Survey Center. Distribution of dentists in the United States by Region and State, 2003. Chicago, IL: The American Dental Association; 2005. [Google Scholar]
- 38.Mucci IA, Brooks DR. Lower use of dental services among long term cigarette smokers. J Epidemiol Community Health. 2001;55:38–393. doi: 10.1136/jech.55.6.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tomar SL. Dentistry’s role in tobacco control. J Am Dent Assoc. 2001;132:30S–35S. doi: 10.14219/jada.archive.2001.0386. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Projected smoking-related deaths among youth. United States. MMWR. 1996;45:971–974. [PubMed] [Google Scholar]