Abstract
Soluble P-selectin (sP-selectin), a biomarker of inflammatory related pathologies including cardiovascular and peripheral vascular diseases, also has pro-atherosclerotic effects including the ability to increase leukocyte recruitment and modulate thrombotic responses in vivo. The current study explores its role in progressing atherosclerotic plaque disease. Apoe −/− mice placed on a high fat diet (HFD) were given daily injections of recombinant dimeric murine P-selectin (22.5 µg/kg/day) for 8 or 16 weeks. Saline or sE-selectin injections were used as negative controls. In order to assess the role of sP-selectin on atherothrombosis an experimental plaque remodelling murine model, with sm22α-hDTR Apoe−/− mice on a HFD in conjunction with delivery of diphtheria toxin to induce targeted vascular smooth muscle apoptosis, was used. These mice were similarly given daily injections of sP-selectin for 8 or 16 weeks. While plaque mass and aortic lipid content did not change with sP-selectin treatment in Apoe−/− or SM22α-hDTR Apoe−/− mice on HFD, increased plasma MCP-1 and a higher plaque CD45 content in Apoe −/− HFD mice was observed. As well, a significant shift towards a more unstable plaque phenotype in the SM22α-hDTR Apoe−/− HFD mice, with increased macrophage accumulation and lower collagen content, leading to a lower plaque stability index, was observed. These results demonstrate that chronically raised sP-selectin favours progression of an unstable atherosclerotic plaque phenotype.
Introduction
Cardiovascular disease (CVD) remains the largest cause of death in the world [1]. A vital mechanism for the development of an unstable atherosclerotic plaque is through increased vascular leukocyte recruitment, which is part of the inflammation hypothesis of atherosclerosis in CVD [2]. Critically, inflammatory plaques lead to extracellular matrix remodelling and vascular smooth muscle cell (VSMC) destruction [2]. These characteristics have been utilised experimentally by generating a VSMC inducible knockout mouse, the SM22α-hDTR Apoe−/− , that presents with a vulnerable plaque phenotype and evidence of plaque rupture [3].
P-selectin is a member of the selectin family, is localised in the membranes of the α-granules of platelets and the Weibel-Palade bodies of endothelial cells and is expressed on the surface of activated platelets and endothelial cells [4]. It contributes to leukocyte recruitment at sites of vascular injury and inflammation and acts via the engagement of the ligand PSGL-1 [5]–[7]. Previous studies have shown that platelet P-selectin engagement of PSGL-1 leads to Mac-1 activation and subsequent firm adhesion [8], [9]. P-selectin deficiency or antibody-mediated inhibition of its adhesive function reduces early atherogenesis in animal models [10], [11]. The soluble form of P-selectin (sP-selectin), arising from either proteolytic cleavage or secretion of an alternatively spliced isoform, is increased in disease states prompting its identification as a potentially valuable clinical biomarker of vascular disease risk [12], [13].
We have previously demonstrated that the elevated levels of sP-selectin present in patients with peripheral vascular disease is not only a biomarker of disease but has functional effects by activating leukocytes and promoting their adhesion to platelet monolayers [14]. We have also shown that sP-selectin promotes leukocyte adhesion through PSGL-1 outside-in signalling through Src and PI3K, leading to Mac-1 integrin activation and subsequent recruitment to arterial and venule micro- and macro-circulation [15], a finding described by others [16].
Given that raised sP-selectin appears to be mediating increased arterial leukocyte recruitment, and more recent data showing that raised sP-selectin can directly affect atherothrombosis in a transgenic mouse model (deltaCT/deltaCT) [17], we hypothesised that chronically raised sP-selectin will exacerbate disease progression in genetically susceptible mouse models of atherosclerosis.
Materials and Methods
Materials
Recombinant murine dimeric soluble E- and P-selectin-Fc Chimera were purchased from R & D systems (USA). Both recombinant proteins were endotoxin free as analysed by the manufacturer and confirmed in independent limulus assays, giving values below 0.01 EU/ml. Diptheria toxin was from Corynebacterium diphtheriae and purchased from Sigma-Aldrich (USA).
Animals
All procedures and protocols were approved by the AMREP Animal Ethics Committee (project approval number: E/0972/2010/B) and conformed to the Guide for the Care and Use of Laboratory Animals (NIH).
Male Apoe−/− mice on the C57BL/6 background and male SM22α-hDTR Apoe−/− were bred and housed at the Precinct Animal Centre, Alfred Medical Research and Education Precinct (AMREP), Melbourne, Australia. SM22α-hDTR Apoe−/− mice were created based on the published model described by Clarke et al [3]. Briefly, the mouse SM22α promoter (−445 to +88 relative to transcriptional start site) was cloned into the pSTEC-1/2 vector upstream of the mDTR-eGFP sequence. DNA was prepared for injection of the vector into oocytes and implantation and generation of chimeric progenitors was provided by the Biomolecular Institute (Australia). SM22a-hDTR mice were born at the expected frequency and developed normally. SM22a-hDTR were subsequently crossed with ApoE−/− and progeny developed normally with no difference in phenotype from ApoE−/−. From 6 weeks of age mice received daily sub-cutaneous (s.c) injections of either vehicle (saline), sE-selectin (22.5 µg/kg/day) or sP-selectin (22.5 µg/kg/day) and were fed high fat diet (HFD) containing 0.15% cholesterol and 22% fat (Speciality Feeds, Western Australia) for 8 or 16 weeks. The dose of selectins was chosen on the basis of raising plasma sP-selectin by approximately 150 ng/ml, which is observed in human pathologies, most notably in cardiovascular and peripheral vascular disease, as previously described [15]. SM22α-hDTR Apoe−/− mice and their Apoe−/− mice controls were injected with Diptheria toxin (5 ng/g; three times weekly) for the last three weeks of the HFD.
Histology
The proximal aorta from within the heart was dissected and sectioned into sinus root, arch, thoracic and abdominal areas and embedded in OCT compound and snap frozen with isopentane chilled by liquid nitrogen. 6–10 µm sections of each aortic segment were analysed for lesion size defined as the cross sectional surface area of Oil Red O staining within the aortic intima, or by immunohistochemistry to identify CD45 (Pharminogen), CD68 (Serotec) and alpha smooth muscle actin (αSMA) expression (Abcam). Briefly, sections were fixed in cold (−20°C) acetone for 20 min. The sections were then sequentially incubated in 3% hydrogen peroxide in PBS, 10% normal goat/horse serum/PBS and biotin/avidin blocking reagents (Vector Laboratories). Thereafter, the sections were incubated with primary antibodies in normal goat serum. Sections were incubated with the corresponding biotynylated secondary antibodies and detected using the Avidin Biotin staining Complex (Vector Laboratories) with DAB (3,3′-Diaminobenzidine) reagent (Vector Laboratories). DAB treated sections were counterstained with hematoxylin and Scotts tap water. Apoptotic cells were identified by the in situ cell death detection kit dUTP nick end -labelling with peroxidase label (TUNEL-POD) (Roche). Collagen was stained with 0.1% Sirius Red F3BA (Sigma-Aldrich) in isopropanol and lipid with Oil Red O or Sudan-IV. Necrotic core was determined by analysis of Mayer’s Hematoxylin and Eosin stained sections with the unstained cellular regions defined as necrotic, as previously described [18].
Images were taken using an FSX100 Olympus microscope and analysed using Fiji 1.47 h software. Stained areas were expressed as a percentage of total plaque area. Stained cells (eg. TUNEL and CD45) were expressed as a percentage of total plaque cells. All mean data including mean lesion size was calculated from the measurement of cross sections taken from every 60 µm of the first 180 µm of the aortic sinus root proximal to the aortic arch or from every 100 µm of the first 600 µm in the ascending aorta proximal to the heart. Only advanced plaques (defined as those displaying necrotic cores) were analysed in this study. Plaque stability scores were defined as ratio of collagen content over lipid area, as previously described [19].
Sudan En Face Staining
Aortae segments (abdominal, thoracic, arch) were cleaned of peri-aortic fat, stained with Sudan IV and imaged by a light microscope (Motic SMZ-168) connected to a digital camera and computer. Stained areas were quantified using Fiji 1.47 h software and expressed as a percentage of total aorta area.
Plasma Protein/Cytokine/Chemokine Measurements
Blood was collected via cardiac puncture and plasma stored in sodium citrate (129 mM) tubes and analysed for soluble E- and P-selectin levels using ELISA (R & D) and mouse MCP-1 (CCL2), Rantes (CCL5), TNF-α, MIP-1α (CCL3), and IL-1β content using a Bio-Plex assay kit (Bio-Rad CA, U.S.A), according to the manufacturers’ instructions.
Statistical Analysis
Results are expressed as mean ± SEM. Comparisons between groups were carried out using a student’s unpaired t-test or for multiple comparisons, by a one way ANOVA followed by Tukey’s post-hoc test. A value of P<0.05 was considered as statistically significant. At least 6 mice per group were analysed for each data set.
Results
Effect of Treatment on Plasma Soluble Markers in Apoe−/− Mice
Plasma sP-selectin and sE-selectin levels were analysed in all animals. Figure 1A shows that following either 8 or 16 weeks of daily injections of recombinant sP-selectin, circulating plasma levels increased to around 300 ng/ml, which is significantly higher than levels observed in saline or sE-selectin treated animals, and is comparable to human pathologies, including CVD and PVD [13], [20]. Similarly sE-selectin injections led to increases in plasma levels of sE-selectin as measured by ELISA (figure 1B).
Figure 1. sP-selectin, sE-selectin and cytokine/chemokine plasma levels in ApoE−/− HFD mice receiving daily injections of recombinant sP-selectin or sE-selectin.
A) Plasma levels of sP-selectin after 8 or 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). B) Plasma levels of sE-selectin after 8 or 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). C) Plasma levels of IL-1β, MCP-1, MIP-1α and RANTES after 8 or 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). n = 9–15 mice per treatment group. Data represented as Mean (ng or pg/ml) ± SEM where *, ** and ** represents P<0.05, <0.01 and <0.001 respectively (from saline treatment) as analysed by One-way ANOVA with Tukey’s post-hoc test.
To generate a picture of the overall systemic inflammatory response following treatments, a plasma BioPlex ELISA was performed. sP-selectin treatment significantly increased plasma levels of IL-1β, MCP-1 and MIP-1α (figure 1C), while a significant decrease in RANTES was also noted (figure 1C).
Effect of sP-selectin on Apoe−/− Plaque Size and Phenotype
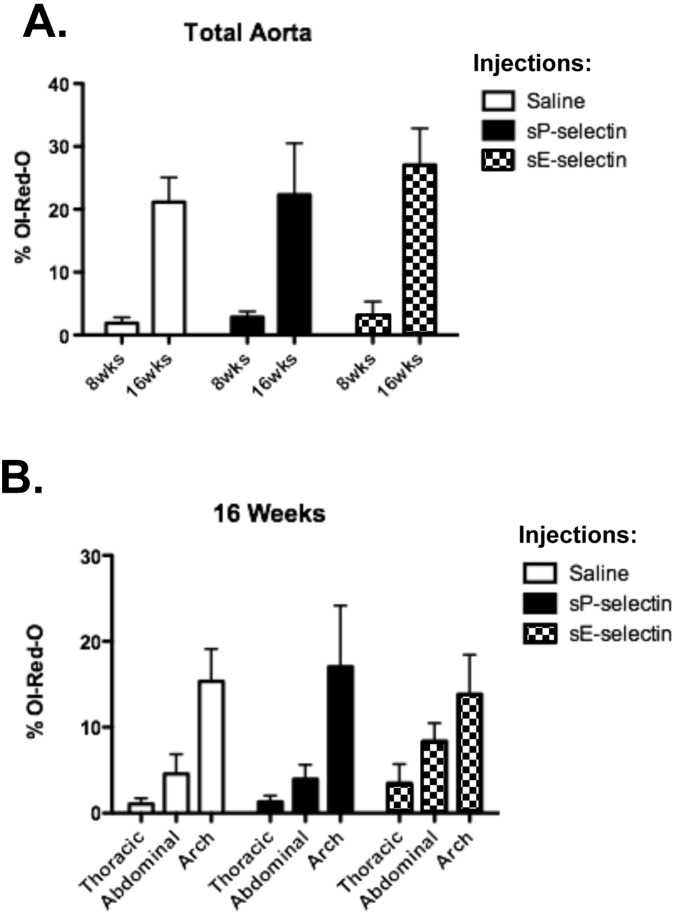
Figure 2 shows plaque size assessed as percentage of Oil-red-O staining in a given field, from daily injections of sP-selectin, or sE-selectin and saline delivered as controls, into HFD fed Apoe −/− mice fed. As expected, aortic sections had significantly greater atherosclerosis in all groups of Apoe −/− mice from 8 to 16 weeks on HFD (figure 2a). However, there were no significant differences between treatment groups. Plaque mass was also assessed for thoracic, abdominal and arch areas. While arch areas did show significantly increased atherosclerosis compared to either the thoracic or abdominal regions, there were no changes in atherosclerosis between treatment groups at either 8 weeks (data not shown) or 16 weeks of treatment (figure 2b).
Figure 2. Oil-Red-O assessment of plaque area in ApoE−/− on HFD with sP-selectin treatment.
Sections of each aortic segment were analysed for lesion size defined as the cross sectional surface area of Oil Red O staining within the aortic intima A) from total aorta after 8 or 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar), B) from indicated aortic sections after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). n = 6–9 mice per treatment group. Data represented as Mean (% ORO) ± SEM.
Figure 3 shows a trend for an increase in plaque CD45+ leukocytes after 8 weeks of sP-selectin treatment which became highly significant at 16 weeks. A small but significant increase in plaque CD45+ leukocyte content following 16 weeks of sE-selectin administration was also observed, although this was half of that observed following sP-selectin (figure 3).
Figure 3. Aortic CD45+ expression in ApoE−/− HFD after sP-selectin treatment.
Sections of each aortic segment were analysed for CD45+ positive cells by immunohistochemistry after 8 or 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). n = 6–9 mice per treatment group. Data represented as Mean (DAB intensity) ± SEM where * and *** represents P<0.05 and <0.001 respectively (from saline treatment) as analysed by One-way ANOVA with Tukey’s post-hoc test.
Effect of sP-selectin on Plasma Inflammatory Markers in SM22α-hDTR Apoe−/−
To further explore the effect of s-P-selectin on plaque phenotype, we applied a published experimental plaque remodelling model (SM22α-hDTR Apoe−/−) [3] in combination with raising plasma sP-selectin over 8 and 16 wks.
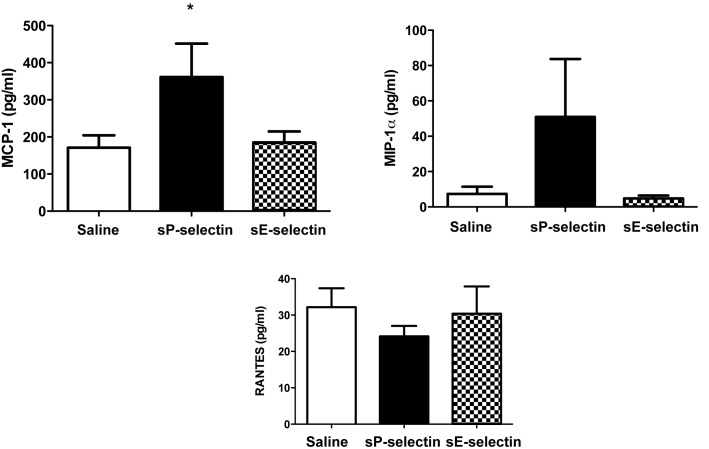
To examine if similar changes in plasma inflammatory markers could also be noted in the SM22α-hDTR Apoe−/− model as in Apoe−/− alone (on HFD), we analysed plasma levels of MCP-1, MIP-1α, IL1β and RANTES after sP-selectin or control treatments (saline, sE-selectin) after 16 wks (8 wk data not shown). Similar to Apoe−/− on HFD alone, sP-selectin increased plasma levels of MCP-1 and MIP-1α in this model (figure 4). This was coupled with a decrease in RANTES after sP-selectin treatment (figure 4). There was no difference in IL1β levels (data not shown).
Figure 4. Plasma cytokine and chemokine levels after sP-selectin treatment for 16weeks in SM22α-hDTR ApoE−/− HFD.
Plasma levels of MCP-1, MIP-1α and RANTES after 8 or 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). n = 9–15 mice per treatment group. Data represented as Mean (pg/ml) ± SEM where * represents P<0.05 (from saline treatment) as analysed by unpaired students t-test.
Effect of sP-selectin on Plaque Morphology in SM22α-hDTR Apoe−/−
A preliminary validation group of 16 wk HFD fed SM22α-hDTR Apoe−/− in comparison to Apoe−/− mice showed a significant change in overall plaque mass (figure 5A). There was a significant increase in necrotic core and αSMA content with a decrease in collagen content (figure 5B–D). These data confirm previous findings using the SM22α-hDTR Apoe−/− mouse model, albeit with less significance [3].
Figure 5. Model validation data.
Sections of each aortic segment were analysed for lesion size, necrotic core, αSMA and collagen content in Apoe −/− HFD or SM22hDTR-ApoE−/− HFD mice, A) lesion size defined as % ORO staining, B) necrotic core defined as % unstained with Mayer’s Hematoxylin and Eosin, C) % α-SMA content, D) % collagen content. n = 6–9 mice per treatment group. Data represented as Mean (% stain) ± SEM where * represents P<0.05 as analysed by unpaired students t-test. Representative images are given for each analysis. Scale bars = 100 µm.
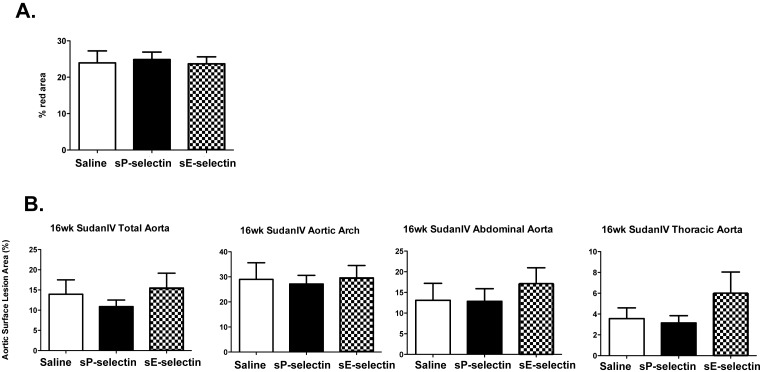
We next applied daily injections of sP-selectin, sE-selectin or saline for 8 and 16 weeks. Figure 6 shows that, as in Apoe −/− mice, SM22α-hDTR Apoe−/− mice on a HFD with daily injections of sP-selectin for 16 weeks exhibited no significant change in total plaque mass lipid content (ORO), as compared to control injections using saline or sE-selectin. This was also noted in all regions of the aorta using en-face Sudan IV staining after 16 wk treatment (figure 6B). No change in lipid content was noted after 8 wk treatments (data not shown).
Figure 6. Oil-Red-O and en face Sudan IV assessment of plaque area in SM22α-hDTR ApoE−/− HFD with sP-selectin treatment for 16 weeks.
A) Sections of each aortic segment were analysed for lesion size defined as the cross sectional surface area of % ORO staining within the aortic intima after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). B) En-face Sudan IV staining from indicated aortic sections after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). n = 6–9 mice per treatment group. Data represented as Mean (%)±SEM.
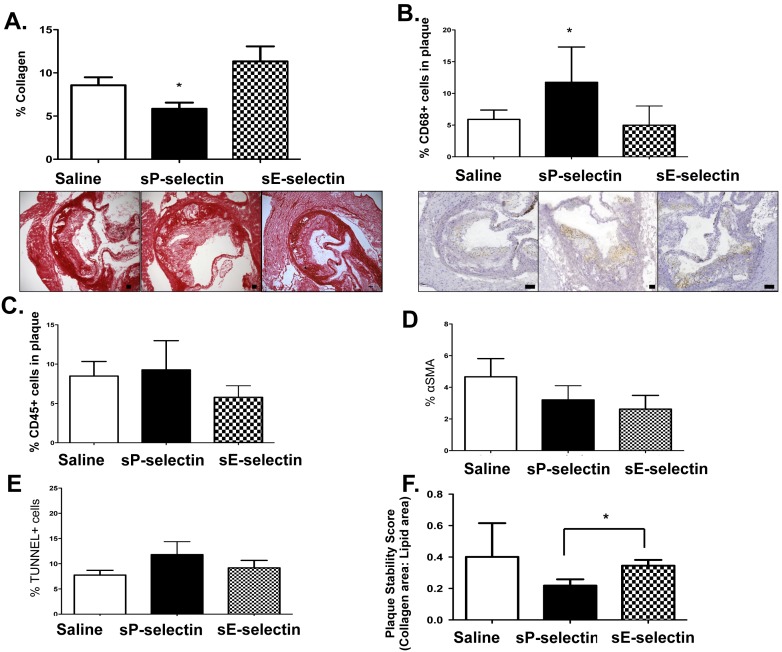
Conversely, sP-selectin treatment led to significantly lower collagen content after 16 weeks (figure 7A) and a significantly higher CD68+ macrophage accumulation (figure 7B) but not total CD45+ cells in the plaque (figure 7C), compared to saline and E-selectin injected controls (8 wk data not shown). No change in collagen content was noted after 8 wk treatments (data not shown) and there was no effect of treatment on αSMA content and apoptotic cells (figure 7D–E) at 16 weeks. Overall a significant reduction in plaque stability score, as assessed by collagen over plaque area, was observed (figure 7F).
Figure 7. Collagen, CD45+, CD68+, α-SMA and apoptotic cell content and plaque stability scores in SM22α-hDTR ApoE−/− HFD after sP-selectin treatment for 16 weeks.
A) Sections of each aortic segment were analysed for collagen content by immunohistochemistry after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). Representative images are given below. Sections of each aortic segment were analysed for B) CD68+ (representative images shown below) and C) CD45+ cells by immunohistochemistry after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar) D) αSMA content or E) apoptotic cell content (% TUNEL) by immunohistochemistry after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). F) Plaque stability scores were defined as ratio of collagen content over lipid area after 16 weeks of daily s.c injections (22.5 µg/kg/day) of vehicle control (saline matched volume; white bar), sP-selectin (black bar) or sE-selectin (checkered bar). n = 6–9 mice per treatment group. Data represented as Mean (% stain or score) ± SEM where * represents P<0.05 (from saline or indicated treatment) as analysed by One-way ANOVA with Tukey’s post-hoc test or unpaired student’s t-test (C, D). Scale bars = 100 µm.
Discussion
Like all selectins, membrane bound P-selectin has an N-terminal lectin domain, an epidermal growth factor motif, and specifically, nine regulatory protein repeats, a transmembrane section and a short intracytoplasmic tail [6]. After activation of endothelial cells by inflammatory mediators such as TNFα, Weibel–Palade bodies can become rapidly mobilised, which results in P-selectin expression extending approximately 40 nm from the endothelial surface, lasting up to 3 hours depending on the vasculature [6], [21]. Similarly, platelets can undergo surface expression of P-selectin upon activation by agonists such as P2 receptor agonists [22]. As P-selectin is a component of the membrane of platelet alpha and dense granules, expression reflects activation [22], [23]. P-selectin is a potent adhesion molecule and has been reported to have procoagulant activities by regulating the production of monocyte derived platelet activating factor and tissue factor [24]. Moreover, P-selectin primes monocytes for increased phagocytosis [25]. However, the role of P-selectin in vascular inflammation is complicated by a circulating soluble form, which can arise from proteolytic cleavage and direct expression of P-selectin lacking the cytoplasmic domain [26]. Evidence that sP-selectin has a direct role in atherosclerosis has been reported [17]. Studies from our laboratory demonstrate a role for sP-selectin in regulating leukocyte adhesion in patients with peripheral arterial occlusive disease in-vivo [14], [15]. Pathophysiological concentrations of sP-selectin engages its ligand, PSGL-1, resulting in Src kinase-dependent Mac-1 (CD11b/CD18) up-regulation and adhesive function [14], [15]. Overall, these earlier studies raised the possibility that sP-selectin may promote leukocyte recruitment to sites of vessel wall injury and vascular endothelium in patients with CVD.
We wanted to explore this issue and examine if chronically raised plasma levels of sP-selectin led to direct changes in atherosclerosis progression and/or phenotype in the Apoe −/− experimental mouse model on HFD. Daily injections of 22.5 µg/kg/day of recombinant Fc-chimera sP-selectin over 8 and 16 weeks, led to significantly raised plasma levels of protein which were similar to pathophysiological levels seen in CVD [13], [20]. We showed that chronically raising plasma levels of sP-selectin had modest effects on atherosclerosis in Apoe −/− mice on HFD, compared to raised sE-selectin and saline injection controls. When initially examining total plaque mass, we observed no significant change in atherosclerosis over 8 and 16 weeks HFD with sP-selectin, compared to controls. This was disappointing given previous reports using the DeltaCT mouse model which exhibits abnormally high concentrations of plasma sP-selectin [27], leading to increased aortic sinus lesion mass after 16 wks on normal chow [17]. These disparate findings may represent variations in effects due to the structure of sP-selectin, which in the DeltaCT model lacks the cytoplasmic domain [27]. Indeed, the DeltaCT mouse model demonstrates significant increases in procoagulant activity [27], which may account for its indirect pro-atherosclerotic effects. Also plasma levels of sP-selectin were approximately 3 fold higher than described here and in clinical human disease [20]. Nevertheless, there was marked plaque infiltration of CD45+ leukocytes after sP-selectin treatment for 16 weeks with Apoe −/− on HFD, with notable increases in plasma inflammatory markers, including the monocyte specific chemokine MCP-1. Therefore, we speculated that chronically raising plasma levels of sP-selectin may alter plaque stability.
In order to test the hypothesis that raised plasma sP-selectin increases plaque vulnerability we employed a plaque destabilising model using the genetically susceptible mouse model, SM22α-hDTR on Apoe −/− and HFD background [3]. Previous work has investigated VSMC apoptosis by generating transgenic mice that express the human diphtheria toxin receptor (hDTR), encoded by heparin-binding EGF-like growth factor from a minimal Tagln (also known as SM22α) promoter [3]. In this model, 50–70% of VSMC apoptosis resulted in normal arteries with no inflammation, thrombosis, remodeling or aneurysm formation [3]. However, the atherosclerotic plaques with VSMC apoptosis in SM22α-hDTR Apoe −/− mice resulted in thinning of the fibrous cap, loss of collagen and intimal inflammation, which are all features of plaque vulnerability [3], [28].
VSMCs together with extracellular matrix components comprise the medial layer of adult arteries. VSMC apoptosis can increase as atherosclerotic plaques develop and rupture [29] [28]. After this initial wave of apoptosis, normal medial cell content can be derived several weeks later [30], suggesting that VSMC apoptosis may initiate repopulation. Moreover, VSMC apoptosis may induce calcification, coagulation and be pro-inflammatory [31]. Importantly, VSMC apoptosis causes release of IL-1α [32], MCP-1 and IL-8 resulting in infiltration of macrophages [33], as we find in sP-selectin treated SM22α-hDTR Apoe −/− mice.
Overall, we would speculate that VSMC apoptosis may lead to evidence of unstable plaque or silent plaque rupture in mouse models of atherosclerosis and that raising plasma sP-selectin levels, would increase the risk of plaque rupture, as suggested by others in the DeltaCT model [17]. As such, we performed a preliminary validation group of 16 wk HFD fed SM22α-hDTR Apoe−/− in comparison to ApoE−/− mice on HFD. The SM22α-hDTR Apoe−/− mice showed significant changes in necrotic core, collagen content, increased apoptosis and αSMA content, but was absent of changes in overall plaque mass. These data confirm previous findings of Clarke et al [3], albeit with reduced significance, and demonstrate that SM22α-hDTR Apoe−/− HFD background mice exhibit signs of unstable plaque, leading to an overall decreased plaque stability score, as is noted in human disease [34]. Interestingly, raising plasma sP-selectin in SM22α-hDTR Apoe−/− HFD mice led to decreased atherosclerotic collagen content and increased CD68+ macrophage plaque infiltration, compared to controls. Moreover, similar to sP-selectin treatment in Apoe−/− HFD alone, sP-selectin treatment in SM22α-hDTR Apoe−/− HFD mice elicited increased plasma levels of MCP-1 and MIP-1α.
MCP-1 and MIP-1α are important chemokines involved in monocyte recruitment, which is integral to vascular inflammation and atherosclerosis. The MCP-1 and MIP-1α chemokine axis may be important in regulating recruitment of specific subsets of monocytes with independent effector functions, specifically CCR2highCD14highCD16l°w and CX3CR1highCD14l°wCD16high human monocytes [35]–[37]. The contribution of these monocyte subsets in atherosclerosis is part of ongoing work by many labs, in which recruitment of CCR2highCD14high monocytes is thought to be particularly important in inflammatory atherosclerosis [35], [38]. More work will be needed to understand if soluble P-selectin mediates differences in monocyte subset numbers or recruitment, and macrophage phenotype in atherosclerosis. Further, in light of a recent study showing that inflammatory plaque progression may be regulated by tissue macrophage proliferation independent of monocyte recruitment [39], the role of monocyte recruitment in vulnerable atherosclerosis progression requires further investigation. Neovascularisation has been noted as a hallmark of atherogenesis and a mechanism by which monocytes can enter atherosclerotic lesions [40]. We did not analyse neovascularisation in our model as it was beyond the scope of the current study. Future studies are necessary, however, to investigate whether unstable plaque progression with high levels of sP-selectin promotes neovascularisation and macrophage accumulation.
RANTES is expressed by T-cells, fibroblasts, mesangial cells and platelets [41], [42] and when overexpressed in atherosclerosis, can engage chemokine receptors on the endothelium, mediating transmigration of monocytes and lymphocytes into the intima [43], [44]. RANTES is also expressed in atherosclerotic plaques [45]. Given this strong association between inflammatory atherosclerosis and RANTES, we would have expected an increase in plasma levels of RANTES after sP-selectin. Unexpectedly, we noted significant decreases in RANTES in our Apoe−/− HFD model. Of interest, recent work in the Atherosclerosis Risk in Communities (ARIC) Carotid MRI study has shown that mean minimum fibrous cap thickness was positively associated with RANTES levels [46]. As the thickness of the fibrous cap dictates the stability of the atherosclerotic plaque [47], it may be that RANTES levels compensate for increased inflammatory burden after sP-selectin treatment. This hypothesis requires further investigation.
Overall, asides from significant decreases in collagen content and significant increases in plaque inflammatory cell infiltrates and plasma inflammatory chemokines, raising plasma levels of sP-selectin in SM22α-hDTR ApoE−/− on HFD as a model of experimental unstable atherosclerosis only led to modest changes in plaque stability scores, as compared to controls. However, collagen content is a primary characteristic of unstable/vulnerable plaque and strategies that have directly targeted collagen content through either experimental regression studies or therapeutically increasing plaque collagen density have proven to have positive outcomes in experimental models of atherosclerosis [48]. Therefore this reduction in collagen with sP-selectin treatment, coupled with macrophage infiltration and systemic inflammatory chemokines, would lead to a significant increased risk of plaque rupture and warrants further investigation as to whether targeting raised plasma sP-selectin would be an effective therapeutic strategy in unstable CVD.
In conclusion, we have shown in two models of experimental atherosclerosis that raising plasma concentrations of sP-selectin to pathophysiological levels had some effects on plaque phenotype related to characteristics of vulnerable plaque, such as reduced collagen content and increased inflammatory cellular content. We propose that an increase in circulating sP-selectin may not only be a marker of vascular disease, but may also contribute to the inflammatory hypothesis of unstable plaque progression.
Acknowledgments
We wish to acknowledge the technical assistance of Dr Iśka Carmichael and Dr Stephen Cody of the Monash Micro-Imaging Department, Baker IDI.
Funding Statement
KJW was supported through National Heart Foundation and British Heart Foundation fellowships and part of this work was supported by a National Heart Foundation project grant. JCD was supported in part through a NHMRC senior fellowship. This study was supported in part by the Victorian Government’s Operational Infrastructure Support Program. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Gersh BJ, Sliwa K, Mayosi BM, Yusuf S (2010) Novel therapeutic concepts: the epidemic of cardiovascular disease in the developing world: global implications. Eur Heart J 31: 642–648. [DOI] [PubMed] [Google Scholar]
- 2. Weber C, Noels H (2011) Atherosclerosis: current pathogenesis and therapeutic options. Nat Med 17: 1410–1422. [DOI] [PubMed] [Google Scholar]
- 3. Clarke MC, Figg N, Maguire JJ, Davenport AP, Goddard M, et al. (2006) Apoptosis of vascular smooth muscle cells induces features of plaque vulnerability in atherosclerosis. Nat Med 12: 1075–1080. [DOI] [PubMed] [Google Scholar]
- 4. Woollard KJ, Chin-Dusting J (2010) P-selectin antagonism in inflammatory disease. Curr Pharm Des 16: 4113–4118. [DOI] [PubMed] [Google Scholar]
- 5. Epperson TK, Patel KD, McEver RP, Cummings RD (2000) Noncovalent association of P-selectin glycoprotein ligand-1 and minimal determinants for binding to P-selectin. J Biol Chem 275: 7839–7853. [DOI] [PubMed] [Google Scholar]
- 6. Johnston GI, Cook RG, McEver RP (1989) Cloning of GMP-140, a granule membrane protein of platelets and endothelium: sequence similarity to proteins involved in cell adhesion and inflammation. Cell 56: 1033–1044. [DOI] [PubMed] [Google Scholar]
- 7. Norman KE, Katopodis AG, Thoma G, Kolbinger F, Hicks AE, et al. (2000) P-selectin glycoprotein ligand-1 supports rolling on E- and P-selectin in vivo. Blood 96: 3585–3591. [PubMed] [Google Scholar]
- 8. Urzainqui A, Serrador JM, Viedma F, Yanez-Mo M, Rodriguez A, et al. (2002) ITAM-based interaction of ERM proteins with Syk mediates signaling by the leukocyte adhesion receptor PSGL-1. Immunity 17: 401–412. [DOI] [PubMed] [Google Scholar]
- 9. Ley K, Laudanna C, Cybulsky MI, Nourshargh S (2007) Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol 7: 678–689. [DOI] [PubMed] [Google Scholar]
- 10. Manka D, Collins RG, Ley K, Beaudet AL, Sarembock IJ (2001) Absence of p-selectin, but not intercellular adhesion molecule-1, attenuates neointimal growth after arterial injury in apolipoprotein e-deficient mice. Circulation 103: 1000–1005. [DOI] [PubMed] [Google Scholar]
- 11. Phillips JW, Barringhaus KG, Sanders JM, Hesselbacher SE, Czarnik AC, et al. (2003) Single injection of P-selectin or P-selectin glycoprotein ligand-1 monoclonal antibody blocks neointima formation after arterial injury in apolipoprotein E-deficient mice. Circulation 107: 2244–2249. [DOI] [PubMed] [Google Scholar]
- 12. Woollard KJ (2005) Soluble bio-markers in vascular disease: much more than gauges of disease? Clin Exp Pharmacol Physiol 32: 233–240. [DOI] [PubMed] [Google Scholar]
- 13. Ridker PM, Buring JE, Rifai N (2001) Soluble P-selectin and the risk of future cardiovascular events. Circulation 103: 491–495. [DOI] [PubMed] [Google Scholar]
- 14. Woollard KJ, Kling D, Kulkarni S, Dart AM, Jackson S, et al. (2006) Raised plasma soluble P-selectin in peripheral arterial occlusive disease enhances leukocyte adhesion. Circ Res 98: 149–156. [DOI] [PubMed] [Google Scholar]
- 15. Woollard KJ, Suhartoyo A, Harris EE, Eisenhardt SU, Jackson SP, et al. (2008) Pathophysiological levels of soluble P-selectin mediate adhesion of leukocytes to the endothelium through Mac-1 activation. Circ Res 103: 1128–1138. [DOI] [PubMed] [Google Scholar]
- 16. Wang HB, Wang JT, Zhang L, Geng ZH, Xu WL, et al. (2007) P-selectin primes leukocyte integrin activation during inflammation. Nat Immunol 8: 882–892. [DOI] [PubMed] [Google Scholar]
- 17. Kisucka J, Chauhan AK, Zhao BQ, Patten IS, Yesilaltay A, et al. (2009) Elevated levels of soluble P-selectin in mice alter blood-brain barrier function, exacerbate stroke, and promote atherosclerosis. Blood 113: 6015–6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen YC, Bui AV, Diesch J, Manasseh R, Hausding C, et al. (2013) A novel mouse model of atherosclerotic plaque instability for drug testing and mechanistic/therapeutic discoveries using gene and microRNA expression profiling. Circ Res 113: 252–265. [DOI] [PubMed] [Google Scholar]
- 19. Gaspari T, Welungoda I, Widdop RE, Simpson RW, Dear AE (2013) The GLP-1 receptor agonist liraglutide inhibits progression of vascular disease via effects on atherogenesis, plaque stability and endothelial function in an ApoE(−/−) mouse model. Diab Vasc Dis Res 10: 353–360. [DOI] [PubMed] [Google Scholar]
- 20. Tan KT, Tayebjee MH, Lynd C, Blann AD, Lip GY (2005) Platelet microparticles and soluble P selectin in peripheral artery disease: relationship to extent of disease and platelet activation markers. Ann Med 37: 61–66. [DOI] [PubMed] [Google Scholar]
- 21. Khew-Goodall Y, Butcher CM, Litwin MS, Newlands S, Korpelainen EI, et al. (1996) Chronic expression of P-selectin on endothelial cells stimulated by the T-cell cytokine, interleukin-3. Blood 87: 1432–1438. [PubMed] [Google Scholar]
- 22. Storey RF, Sanderson HM, White AE, May JA, Cameron KE, et al. (2000) The central role of the P(2T) receptor in amplification of human platelet activation, aggregation, secretion and procoagulant activity. Br J Haematol 110: 925–934. [DOI] [PubMed] [Google Scholar]
- 23. Matzdorff AC, Kemkes-Matthes B, Voss R, Pralle H (1996) Comparison of beta-thromboglobulin, flow cytometry, and platelet aggregometry to study platelet activation. Haemostasis 26: 98–106. [DOI] [PubMed] [Google Scholar]
- 24. Celi A, Pellegrini G, Lorenzet R, De Blasi A, Ready N, et al. (1994) P-selectin induces the expression of tissue factor on monocytes. Proc Natl Acad Sci U S A 91: 8767–8771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Elstad MR, La Pine TR, Cowley FS, McEver RP, McIntyre TM, et al. (1995) P-selectin regulates platelet-activating factor synthesis and phagocytosis by monocytes. J Immunol 155: 2109–2122. [PubMed] [Google Scholar]
- 26. Polgar J, Matuskova J, Wagner DD (2005) The P-selectin, tissue factor, coagulation triad. J Thromb Haemost 3: 1590–1596. [DOI] [PubMed] [Google Scholar]
- 27. Andre P, Hartwell D, Hrachovinova I, Saffaripour S, Wagner DD (2000) Pro-coagulant state resulting from high levels of soluble P-selectin in blood. Proc Natl Acad Sci U S A 97: 13835–13840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Geng YJ, Libby P (1995) Evidence for apoptosis in advanced human atheroma. Colocalization with interleukin-1 beta-converting enzyme. Am J Pathol 147: 251–266. [PMC free article] [PubMed] [Google Scholar]
- 29. Lutgens E, de Muinck ED, Kitslaar PJ, Tordoir JH, Wellens HJ, et al. (1999) Biphasic pattern of cell turnover characterizes the progression from fatty streaks to ruptured human atherosclerotic plaques. Cardiovasc Res 41: 473–479. [DOI] [PubMed] [Google Scholar]
- 30. Clowes AW, Reidy MA, Clowes MM (1983) Kinetics of cellular proliferation after arterial injury. I. Smooth muscle growth in the absence of endothelium. Lab Invest 49: 327–333. [PubMed] [Google Scholar]
- 31. Littlewood TD, Bennett MR (2003) Apoptotic cell death in atherosclerosis. Curr Opin Lipidol 14: 469–475. [DOI] [PubMed] [Google Scholar]
- 32. Schaub FJ, Liles WC, Ferri N, Sayson K, Seifert RA, et al. (2003) Fas and Fas-associated death domain protein regulate monocyte chemoattractant protein-1 expression by human smooth muscle cells through caspase- and calpain-dependent release of interleukin-1alpha. Circ Res 93: 515–522. [DOI] [PubMed] [Google Scholar]
- 33. Schaub FJ, Han DK, Liles WC, Adams LD, Coats SA, et al. (2000) Fas/FADD-mediated activation of a specific program of inflammatory gene expression in vascular smooth muscle cells. Nat Med 6: 790–796. [DOI] [PubMed] [Google Scholar]
- 34. Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM (2000) Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 20: 1262–1275. [DOI] [PubMed] [Google Scholar]
- 35. Woollard KJ, Geissmann F (2010) Monocytes in atherosclerosis: subsets and functions. Nat Rev Cardiol 7: 77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tacke F, Alvarez D, Kaplan TJ, Jakubzick C, Spanbroek R, et al. (2007) Monocyte subsets differentially employ CCR2, CCR5, and CX3CR1 to accumulate within atherosclerotic plaques. J Clin Invest 117: 185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Swirski FK, Libby P, Aikawa E, Alcaide P, Luscinskas FW, et al. (2007) Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata. J Clin Invest 117: 195–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Woollard KJ (2013) Immunological aspects of atherosclerosis. Clin Sci (Lond) 125: 221–235. [DOI] [PubMed] [Google Scholar]
- 39. Robbins CS, Hilgendorf I, Weber GF, Theurl I, Iwamoto Y, et al. (2013) Local proliferation dominates lesional macrophage accumulation in atherosclerosis. Nat Med 19: 1166–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jaipersad AS, Lip GY, Silverman S, Shantsila E (2014) The role of monocytes in angiogenesis and atherosclerosis. J Am Coll Cardiol 63: 1–11. [DOI] [PubMed] [Google Scholar]
- 41. von Hundelshausen P, Petersen F, Brandt E (2007) Platelet-derived chemokines in vascular biology. Thromb Haemost 97: 704–713. [DOI] [PubMed] [Google Scholar]
- 42. Gear AR, Camerini D (2003) Platelet chemokines and chemokine receptors: linking hemostasis, inflammation, and host defense. Microcirculation 10: 335–350. [DOI] [PubMed] [Google Scholar]
- 43. Charo IF, Taubman MB (2004) Chemokines in the pathogenesis of vascular disease. Circ Res 95: 858–866. [DOI] [PubMed] [Google Scholar]
- 44. Baltus T, Weber KS, Johnson Z, Proudfoot AE, Weber C (2003) Oligomerization of RANTES is required for CCR1-mediated arrest but not CCR5-mediated transmigration of leukocytes on inflamed endothelium. Blood 102: 1985–1988. [DOI] [PubMed] [Google Scholar]
- 45. Nomura S, Uehata S, Saito S, Osumi K, Ozeki Y, et al. (2003) Enzyme immunoassay detection of platelet-derived microparticles and RANTES in acute coronary syndrome. Thromb Haemost 89: 506–512. [PubMed] [Google Scholar]
- 46. Virani SS, Nambi V, Hoogeveen R, Wasserman BA, Coresh J, et al. (2011) Relationship between circulating levels of RANTES (regulated on activation, normal T-cell expressed, and secreted) and carotid plaque characteristics: the Atherosclerosis Risk in Communities (ARIC) Carotid MRI Study. Eur Heart J 32: 459–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Davies MJ, Richardson PD, Woolf N, Katz DR, Mann J (1993) Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J 69: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Waxman S, Ishibashi F, Muller JE (2006) Detection and treatment of vulnerable plaques and vulnerable patients: novel approaches to prevention of coronary events. Circulation 114: 2390–2411. [DOI] [PubMed] [Google Scholar]