Abstract
Purpose
In the United States, human immunodeficiency virus (HIV) incidence rates continue to increase among young gay, bisexual and other men have sexual intercourse with men. Young men who have sex with men (YMSM) indicate interest in HIV prevention programming that is implemented in the social venues that they frequent when they want to socialize with other men. We sought to understand YMSM venues as a networked space to provide insights into venue-based HIV prevention intervention delivery.
Methods
The present study used survey data reported by 526 YMSM (ages 18–24) in 2005 to conduct a venue-based social network analysis. The latter sought to determine if the structure and composition of the networks in Los Angeles could be used to facilitate the delivery of HIV prevention messages to YMSM. Degree of person sharing between venues was used to demonstrate interconnectivity between venues classified as low-risk (e.g., coffee shops) and high-risk (e.g., bars, clubs) by a Community Advisory Board.
Results
Sixty-five percent of the 110 venues nominated were bars and clubs. Nearly all YMSM were connected by a single venue and over 87% were connected by the 6 most central venues. A handful of highly connected low-risk venues were central to the venue network and connected to popular high-risk venues.
Conclusions
Venue-based network analysis can inform tailored HIV prevention messaging for YMSM. Targeted delivery of prevention messaging at low-risk centralized venues may lead to widespread diffusion among venue-attending YMSM.
Keywords: gay, bisexual, young men who have sex with men (YMSM), venues, network analysis
Young gay, bisexual and other men who have sexual intercourse with men face developmental challenges related to their sexual identity during adolescence and emerging adulthood, which may include coming out to friends and family, harassment and discrimination, and difficulties forming romantic relationships and/or friendships with similar peers (Tolman & McClelland, 2011). Young men who have sex with men (hereafter YMSM) are disproportionately affected by mental health difficulties, including depression and suicidality (Kipke et al., 2007). YMSM also engage in frequent substance use and risky sexual behaviors, which may put them at risk for contracting HIV (Clatts, Goldsamt, & Yi, 2005). YMSM may receive social support during adolescence and young adulthood through connection to gay communities. However, YMSM are often first exposed to gay communities through their attendance at social venues, such as bars and clubs, where many attendees engage in behaviors that increase their risk for contracting HIV (Stall, Friedman, & Catania, 2007). Social venues that cater to members of the various gay communities may offer HIV service organizations with opportunities to deliver their HIV education and prevention programs to men who may not be willing to go to the site where the organization is located.
Epidemiological data documents a 34% increase in HIV infection among YMSM (ages 13–29) between 2006 and 2009 (Prejean et al., 2011). Yet, evidence points to a disconnect between current HIV prevention programming and interest in those approaches among YMSM (Holloway, Cederbaum, Ajayi, & Shoptaw, 2012). For example, Orellana and colleagues (2006) found that among high-risk, sexually active MSM, those ages 20 – 24 years old were nearly three times as likely to not enroll in a brief telephone-delivered HIV prevention intervention compared MSM 40 and above; those ages 25 – 29 years old were twice as likely not to enroll compared to MSM 40 and above. Some researchers have suggested that many young people hold the erroneous belief that HIV is an infection that older people contract (Rutledge, Roffman, Picciano, Kalichman, & Berghuis, 2002). If so, young persons may feel that there is less immediate need for them to change the behavior that puts them at risk of infection. Others have suggested that YMSM who reached sexual maturity in the age of highly active antiretroviral therapies may feel complacency about sexual risk behavior because HIV can now be managed as many other chronic diseases (Valdiserri, 2004). A qualitative study conducted in Los Angeles, CA found that YMSM would be interested in HIV programming delivered through their social networks and/or in the social contexts that they were already attending (Holloway, Cederbaum, Ajayi, & Shaptaw, 2012). These findings are consistent with early HIV prevention research which took place in gay male social contexts, such as bars and clubs (Kelly et al., 1991; Kelly et al., 1992).
HIV researchers have explored the role of social contexts in facilitating both substance use and sexual risk behavior among MSM in general, and to a lesser extent YMSM. It is well documented that sexual risk behavior is common among gay men who socialize in venues where substances are used (Vicioso, Parsons, Nanin, Purcell, & Woods, 2005). The venues most studied include bathhouses, circuit parties, and sex parties. However, attendance at gay bars and clubs is also associated with both alcohol/drug use and risky sexual behavior (Grov & Crow, 2012). These social spaces may be especially important to YMSM, who are in the developmental stage termed “emerging adulthood” (Arnett, 2007) and are learning to express their sexual identity in the context of a larger society that is often homophobic and hostile. YMSM may seek out social contexts that are accepting of their sexual identity, which include gay bars and clubs, where there are significant opportunities for both social support yet where community norms exist that are tolerant (and sometimes encouraging) of substance use and unprotected sex (Harper, 2007). As YMSM socialize in these venues, they may learn to associate substance use and sexual risk behavior with gay venue attendance (Stall et al., 2007). Indeed, researchers have found that there is a positive association between gay bar attendance and cigarette smoking (Holloway et al., 2012), a positive association between gay bar attendance and binge drinking (Wong, Kipke, & Weiss, 2008), and a positive association between gay bar attendance and illicit substance use and sexual risk behaviors (Greenwood et al., 2001).
To date, relatively few studies have sought to document the characteristics of venues in which YMSM socialize and whether those venue choices are associated with risk behaviors (Binson et al., 2001; Choi et al., 2004; Garofalo et al., 2007; Solomon et al., 2011). A recent study of MSM compared demographic and behavioral characteristics of participants recruited in bathhouses, online, or in gay bars and clubs. The study found that the participants recruited in gay bars and clubs were younger than the participants recruited in other venues and had the strongest attachment to the gay community (Grov, 2012). Social venues, such as bars and clubs, may represent a prime opportunity for targeted HIV prevention with YMSM. However, in order to engage YMSM in venue-based HIV prevention, researchers must better understand the socialization patterns of YMSM, their interaction with gay communities, and the venues in which YMSM may be most amenable to HIV prevention efforts. The present study used a venue-based network analysis to describe connections among social venues frequented by YMSM who reside in Los Angeles, CA. Ultimately, this knowledge will enable researchers to develop and provide more effective community-based HIV prevention interventions for YMSM.
Conceptualizing YMSM Social Venues as Networked Space
Network analysis has become a popular methodology that prevention scientists have used to understand health behaviors and the factors associated with their occurrence. These behaviors include substance use (Bauman et al., 2007) and HIV risk among young people (Rice, Milburn, & Monro, 2011). In contrast, public health researchers often focus their analysis on the individual and seldom examine the ways that social connections to other individuals influence risk behavior (Ennet et al., 2008; Killeya-Jones, & Costanzo, 2007; Lakon, Ennett, & Norton, 2006). Conceptualizing YMSM social venues as a networked space allows for novel insights into intervention delivery possibilities. Despite the fact that most venues stand alone as physical brick-and-mortar entities, they represent a social space connected by the men who frequent those venues. For example, a gay dance club is connected to a coffee shop by the men who regularly socialize in the two venues. Because of the behaviors that attendees enact when they visit certain venues, these venues may be characterized as high-risk venues (e.g., bathhouses or circuit parties). In turn, these venues may be tightly linked to low-risk venues, which are not sites where attendees engage in risky behavior (e.g., bakeries or bookstores). The venues are linked because they share patrons who frequent both venues at different times of the day or week, not because the patrons necessarily enact the same risk behaviors in each venue. If venues are connected by the patrons they share, we can consider the impact that HIV prevention interventions deployed in one venue may have on persons frequenting other venues.
The Theory of Duality of Persons and Groups (TDPG) provides a conceptual and empirical framework that researchers can use to analyze individuals’ group memberships (e.g., venue attendance) in terms of the networks that are created by sharing patrons (Breiger, 1974). Based on seminal work by Erving Goffman (1971), proposing that “the individual is linked to society through two principal social bonds: to collectivities through membership and to other individuals through social relationships” (p.181), the TDPG highlights the idea that individuals who belong to the same group or attend the same venue are connected to one another through their membership in the group and/or attendance at that venue. Therefore, data that includes information about where individuals socialize can be transformed into two types of matrices: person matrices, which connect individuals by the social spaces they share and venue matrices, which connect venues by individuals who share those social spaces.
The TDPG has been used to understand a range of entities including interlocking directorates of international companies based on individuals’ membership on multiple boards of directors (Levine, 1972), interconnected hospitals based on patient transfers between hospitals (Lee et al., 2011), and social service organizations that are connected through the individuals who receive services from those organizations (Schneider et al., 2012). The extant literature demonstrates the utility of this theoretical framework in public health research. However, to our knowledge, the TDPG has not been applied to YMSM social contexts. The present study sought to understand the extent to which YMSM social spaces are connected by the YMSM who share those social contexts in order to inform the delivery of venue-based HIV prevention programs and services for this population disproportionately affected by HIV.
Methods
Participants
The analyses for the present study utilized baseline data from the Healthy Young Men’s (HYM) study (N=526), which aimed to understand substance use and sexual risk behavior among YMSM in Los Angeles, CA (Ford et al., 2009). All participants were male; 18–24 years old at recruitment; self-identified as gay, bisexual, or uncertain about their sexual orientation and/or reported having sex with a man in their lifetime; self-identified as Caucasian, African American, or Latino of Mexican descent; and were residents of Los Angeles County with no expectation of living outside the County for at least six months following recruitment. An established, context-based probability sampling approach (Muhib et al., 2001) was used to obtain a representative sample of YMSM attending gay venues in Los Angeles County. Venues ranged from large special events such as gay pride festivals, to small venues such as bars and coffee shops. If participants met eligibility criteria, informed consent was obtained and confidential, self-administered survey data were collected using computer-assisted interviews. Each survey (available in English and Spanish) took up to 90 minutes to complete. Participants were given 35 dollars compensation for their time and effort. The Committee on Clinical Investigations at Children’s Hospital Los Angeles approved the study. The Institutional Review Board at the University of California, Los Angeles approved secondary data analysis for this paper.
Procedures
Of the 526 HYM study participants, 484 named their “favorite three gay places to socialize.” This single-item, open-ended name generator was the basis for creating the network of venues. Participants’ responses included bars, dance clubs, coffee shops, and bookstores. Each nominated venue was verified through the use of internet searches, which included the name of the venue listed by the respondent and the following key words: “gay” and “Los Angeles.” Addresses of venues were recorded along with brief notes describing the type of venue (e.g., restaurant, bookstore, etc.). When venues could not be located through the internet search, we drew on the expertise of a community advisory board (CAB), which included YMSM as well as service organization and community leaders. In some instances the names of venues nominated by participants could not be verified; these venues were removed from the final list. In addition, venue nominations that were too broad (e.g., West Hollywood) or too narrow (e.g., my friend’s house) were removed from the final venue list. In total, 110 venues were included in the final analyses; each of these venues was given a unique numeric code.
Participants’ responses were represented by a matrix that had 484 rows and 110 columns (i.e., a row for each person and a column for each venue). Each cell of the matrix was populated with a “1” if the person had named the venue or a “0” if the person had not named the venue. These 1/0 entries represented the connections between a person and the venues that the person named. The matrix corresponding to the 484 study participants’ 110 venue nominations (A) was transposed and multiplied by itself to create a 110 × 110 venue-by-venue matrix (i.e., V=(AT)A) using UCINet (Borgatti., Everett, & Freeman, 2002). In addition to connections between persons and venues being designated dichotomously in the resulting matrices (0 for no connection, 1 for connection), valued matrices representing the degree to which persons and venues were connected were also created. In the venue network matrix, the theoretical range of values was 0 – 484, since the maximum number of persons that could connect any two venues was the number of YMSM in the sample who nominated at least one venue. These valued matrices were used to create venue networks at different thresholds of person sharing.
Measures
Based on information obtained through the internet searches and consultations with the CAB, three measures were developed and used to classify the 110 venues. The first measure classified each venue with respect to type and had seven levels: 1=Dance club, 2=Bar, 3=Service organization, 4=Gym or recreation center, 5=Coffee shop or restaurant, 6=Adult bookstore, and 7=Other. Other venue types included specific places that did not fall into one of the other six categories (e.g., public parks) and specific events that could not be associated with a specific location (e.g., gay pride festival, House/Ball event). The CAB used the classification given by the first measure to develop the second measure that classified each type of venue in terms of the extent to which behaviors enacted in the venue placed an individual at risk for contracting HIV. Venues that were associated with HIV risk were venues where alcohol was served, drugs were available, or public sex was known to occur; venues that were not associated with HIV risk were venues like coffee shops and service organizations. For the third measure, the research team used a venue’s zip code to classify the venue with respect to geographical location. This measure had five levels: 1=West Hollywood, 2= Los Angeles, 3= Long Beach, 4=Orange County, and 5=Other. Venues classified as “Other” were located in a geographic area other than one of the four named areas or they were venues that could not be linked with a specific geographical location.
Data Analysis
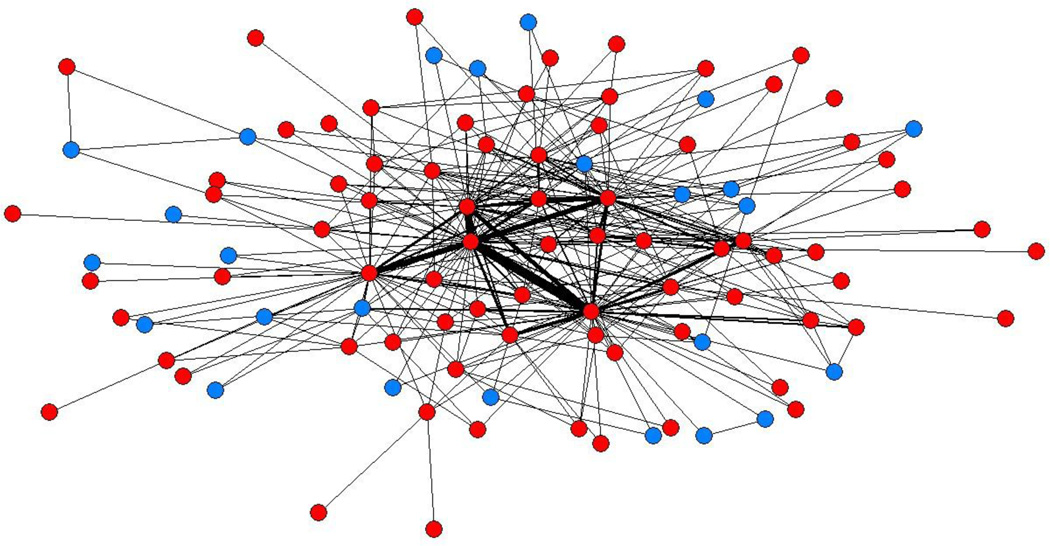
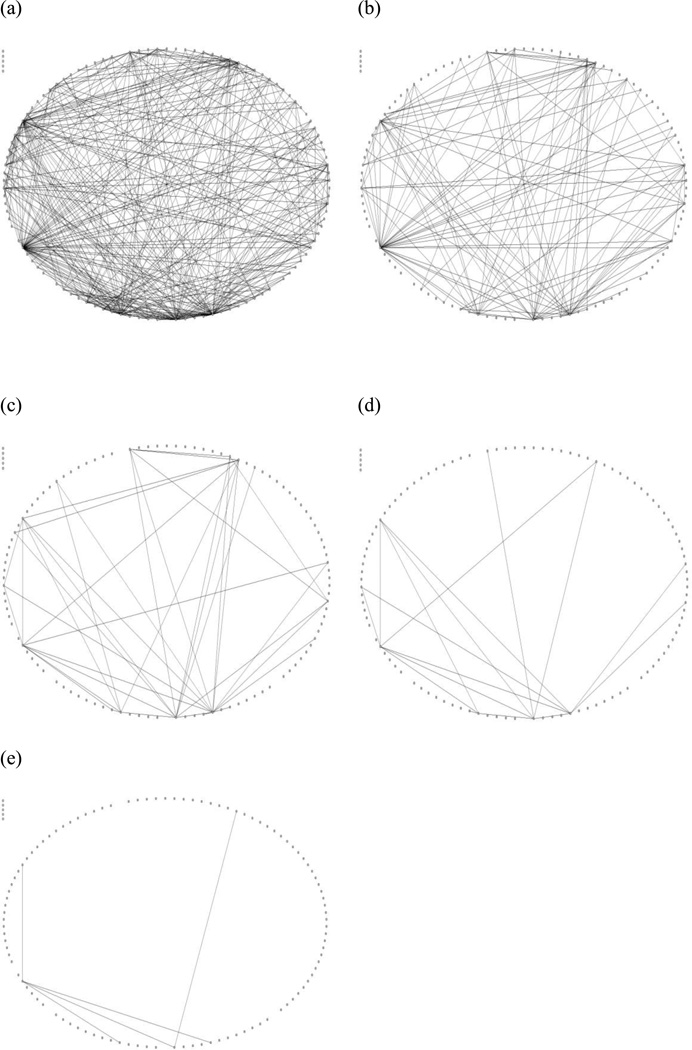
Once the venue network matrix was created it was entered into NETDRAW 2.090 (Borgatti, 2002). The spring embedder routine was used to generate network visualizations. Spring embedding is based on the idea that two nodes in a network push and pull each other simultaneously based on the strength of their connection. Two points located close together represent venues that have a stronger pull (and weaker push) on each other based on the number of YMSM who share those venues, while distant points have a stronger push (and a weaker pull) on each other. The spring embedding algorithm seeks to achieve a global optimum where there is the least amount of stress on the “springs” connecting nodes to each other (Freeman, 2000). In addition to the spring embedder routine (Figure 1), the network was visualized using the circular layout routine in NETDRAW 2.090 (Figure 2), which allowed the research team to easily identify interconnected venues at five levels of increasing person-sharing thresholds based on visual inspection of the network.
Figure 1.
Venue Characteristics with Tie Strength Depicted (n = 110). Smaller components [i.e., isolates (n= 5) and one 3-node single member component] removed for readability. Red nodes indicate venues associated with high risk by CAB; blue nodes indicate venues not associated with high risk by CAB. Legend: Red circles indicate high-risk venues; blue circles indicate low-risk venues.
Figure 2.
Sociograms depicting venue sharing among YMSM in Los Angeles, CA. Diagrams are binary sociograms of the total venue-sharing network at 4 different person-sharing thresholds: (a) 1 person; (b) 2 persons; (c) 5 persons; (d) 10 persons; and (e) 30 persons.
Results
Of the 526 men originally enrolled in the HYM study, 484 (92%) named at least one “favorite gay place to socialize.” Bivariate statistical comparisons using independent sample t-tests and chi-square tests were used to determine any statistically significant differences in demographic characteristics, substance use patterns, HIV risk and HIV testing between HYM participants who answered the venue name generator (n = 484) question and those who did not (n = 42). There were no statistically significant group differences between individuals who answered the name generator question and those who did not with respect to demographic characteristics, substance use patterns, HIV risk or HIV testing. However, when asked to report the frequency with which they attended gay bars and clubs in the past three months (0=“Never,” 1=“Once a month or less,” 2=“Several times a month 3=“About once a week” and 4=“Several times a week or every day”), a greater percentage of men who did not respond to the name generator question (78.6%) reported attending gay bars less than once per week when compared to men who responded to the name generator question (52.4%, p<0.01).
Participant Characteristics
Table 1 provides sociodemographic characteristics of the YMSM included in the analysis (N = 484). YMSM had the opportunity to name up to three favorite venues. Approximately 13% nominated one venue; 26% nominated two venues; and 62% nominated three venues. Small percentages of participants indicated that they “never” attended gay bars or clubs in the past three months (9.3%) or did so “once a month or less” (15.9%); the remainder of the sample reported attending gay bars/clubs “several times a month” to “several times a week or every day” (74.7%).
Table 1.
Sociodemographic Characteristics of Final Sample (N=484)
| Variable | Mean (SD) or n (%) |
|---|---|
| Mean Age | 20.17 (1.56) |
| Age category | |
| 18 – 19 years | 183 (37.8) |
| 20 – 21 years | 187 (38.6) |
| 22+ years | 114 (23.6) |
| Race/Ethnicity | |
| African American | 115 (23.8) |
| Mexican descent | 188 (38.8) |
| Caucasian | 181 (37.4) |
| Residential Status | |
| Family | 261 (53.9) |
| Own place/apartment/dorm | 175 (36.2) |
| With friends/partner | 31 (6.4) |
| No regular place/other | 17 (3.5) |
| School/Employment | |
| In school | 101 (20.9) |
| In school, employed | 134 (27.7) |
| Employed, not In school | 187 (38.6) |
| Not employed, not In school | 62 (12.8) |
| Sexual Identity | |
| Gay | 361 (74.6) |
| Other same-sex identity | 42 (8.7) |
| Bisexual | 81 (16.7) |
| In primary partner relationship | 229 (47.3) |
| Recent gay/bar attendance | |
| Never | 45 (9.3) |
| Once a month or less | 77 (15.9) |
| Several times a month | 131 (27.1) |
| About once a week | 127 (26.3) |
| Several times a week or every day | 103 (21.3) |
| Number of nominated venues | |
| 1 | 60 (12.4) |
| 2 | 126 (26.0) |
| 3 | 298 (61.6) |
| Nominated the same venue in which they were recruited | 97 (21.0) |
Venue Characteristics
The most popular types of venues were bars or clubs (65.4%) followed by smaller numbers of other types of venues, such as coffee shops/restaurants (9.1%), adult bookstores (7.3%), service organizations (7.3%), gymnasiums or recreation centers (4.5%) or other types of venues (6.4%). Venues were located geographically in West Hollywood (30.9%), Los Angeles (43.6%), Long Beach (8.2%), Orange County (8.2%) or another geographic area (9.1%). Based on feedback from CAB members, the research team classified as “high-risk venues” 80 of the 110 venues (72.7%) where alcohol was sold, drugs were available, and/or public sex was known to occur.
The network displayed in Figure 1 is indicative of a core-periphery network structure. This structure is typified by (a) the location of several highly connected venues at the center of the network and (b) the location of a larger number of peripheral venues that have fewer connections to each other than they do to the venues in the center of the network. The thicker lines in Figure 1 represent more person sharing (i.e., a greater number of YMSM naming the two venues connected by the line) and the thinner lines represent less person sharing.
Through the process of visualizing the network with progressively increasing thresholds of person sharing (Figure 2) it becomes apparent that most venues share a small number of individuals. When the person-sharing threshold is set at 1 or more, 102 venues are included in the network (92.7% of all venues nominated). When the person-sharing threshold is set to 2 or more, 44 venues remain in the network (40.0% of all venues nominated). When the person-sharing threshold is set to 5 or more, 18 venues remain in the network (16.4% of all venues nominated). When the person-sharing threshold is set to 10 or more, 11 venues remain in the network (10.7% of all venues nominated). By the time the person-sharing threshold is set to 30 or more, only 6 venues remain in the network (5.4% of all venues nominated).
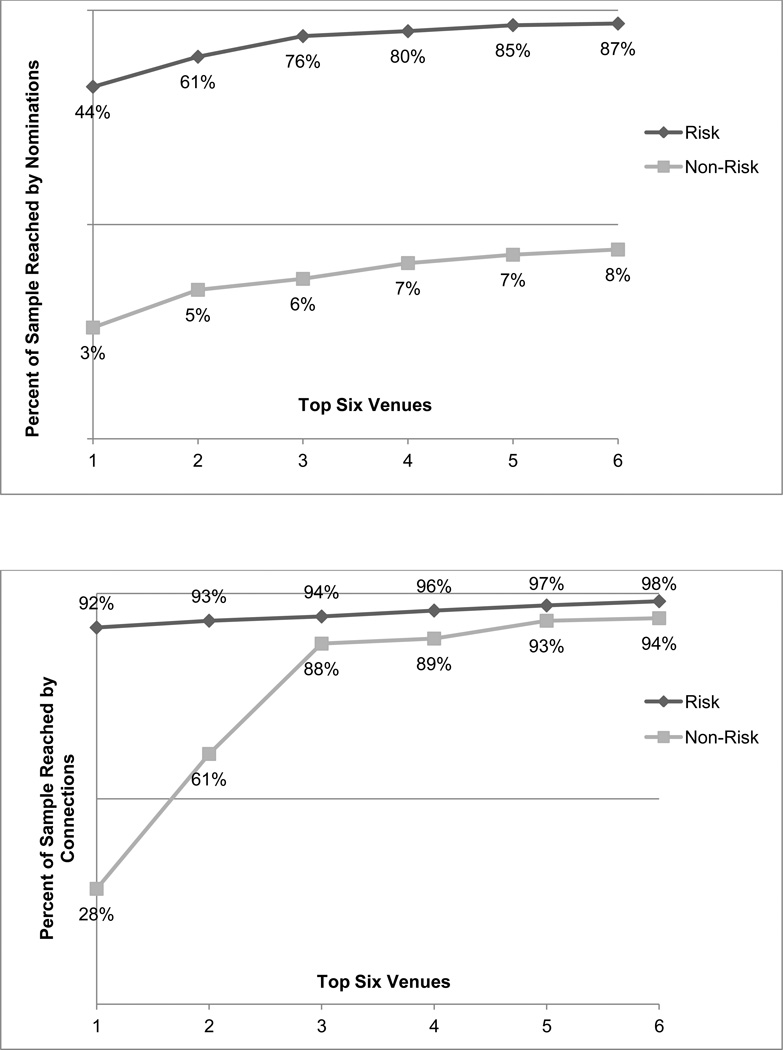
Figure 3 below depicts the percentage of the total sample that can be contacted by the top 6 low-risk (8%) and high-risk venues (84%) when treated as disconnected entities. However, when one or more individuals frequent low- and high-risk venues, the most popular high-risk venues connect 98% of the sample and the most popular low-risk venues connect 94% of the sample. These two percentages indicate that there is extensive interconnectivity between low-and high-risk venues.
Figure 3.
Percentage of sample reached by direct nomination of risk and non-risk venues compared to percentage of the sample reached when risk and non-risk venues are connected by at least one person.
Discussion
YMSM nominated a range of different social venues in which they socialized with other gay men. These venues included recreation centers and social service organizations. However, the vast majority of social venues nominated in this study were bars and clubs. An earlier study by Pollock and Halkitis (2009) examining the link between venue attendance and HIV risk among MSM (88% of whom were 26 years of age or older) found that 42% of those interviewed met their most recent sexual partners at bars and 29% met their most recent sexual partner at a dance club. While that study used percentage of participants who met at particular venues to estimate popularity of those venues for partner seeking, we used percentage of venues nominated to estimate popularity of venues in which YMSM socialize. In our research, 41% of venues nominated were dance clubs and 25% of venues nominated were bars, which may indicate greater popularity of dance clubs among YMSM compared to older MSM. Venues identified as “high-risk venues” by our CAB because alcohol or illicit substances were known to be used in these contexts and/or public sex was known to occur at these venues comprised the majority of nominated venues.
YMSM in Los Angeles have many venues in which to socialize; however, most YMSM nominated a relatively small group of venues as their favorites. Venue-network results demonstrate a distinct core-periphery structure of the venue network suggesting the ability to reach the majority of YMSM in this sample by targeting a handful of the most shared venues. All of the top six most shared venues were located within 4.5 miles of each other. Together, 87% of all YMSM in this sample nominated at least one of these six venues as one of their “favorite gay places to socialize.” Ninety-eight percent of YMSM could be reached either directly in these 6 venues or by one degree of person-sharing. This suggests the high potential for social interaction between these men. As resources for HIV prevention become increasingly limited, it is imperative that money is used wisely. By targeting a small number of highly connected venues, it may possible for an intervention to reach large numbers of YMSM. Social marketing campaigns may be more cost effective in reaching large numbers of YMSM if deliberately placed in maximally shared social venues (Vega & Roland, 2005).
Previous research demonstrates that while venues such as bathhouses, circuit parties, sex parties, and bars/clubs may represent prime opportunities for substance use and sexual risk behavior among YMSM, these venues may also be appropriate locations for HIV prevention service delivery (Mustanski, Newcomb, Du Bois, Garcia & Grov, 2011). Many HIV prevention interventions have been staged in bars and clubs (Kelly et al., 1991; Kelly et al., 1992), circuit parties (Mansergh et al., 2001), African American House and Ball events (Holloway, Traube, Kubicek, Weiss & Kipke, 2012), and bathhouses (Woods, Binson, Mayne, Gore & Rebchook, 2001) in order to bring HIV prevention to communities of gay men. A study by Seal and colleagues (2000), which solicited suggestions from YMSM regarding effective HIV prevention programming, cites venue-based interventions, such as “rap sessions” in cafes, bars, and other venues where YMSM congregate as potentially effective in attracting YMSM. The authors suggest partnering with venue owners and event producers to embed HIV prevention interventions in workshops on topics that might be more compelling to YMSM, such as making safer sex enjoyable and finding the right partner. The results presented here demonstrate that further attention to venue-based HIV prevention among YMSM is needed.
Our findings suggest the potential for innovation in HIV prevention program delivery, based on the interconnectivity of this sample. While bars and clubs may be optimal venues for social marketing interventions, it may be more difficult to engage YMSM in one-on-one HIV prevention activities in these settings. Bars and clubs are often noisy venues attended by individuals seeking to socialize with friends and/or meet romantic partners; oftentimes, alcohol and other substances are also used at these venues. Our data demonstrate high connectivity between high-risk venues (e.g., bars, clubs) and low-risk venues (e.g., coffee shops, recreation centers). YMSM who attend venues associated with high-risk also attend low-risk social venues where they may be more amenable to participation in HIV prevention activities. In fact, when targeting the most popular six low-risk venues it was possible to reach 94% of the total sample of YMSM with only one degree of person-sharing to other venues. Interventions staged in low-risk venues may have the potential for rapid diffusion into high-risk venues. The diffusion of innovations literature suggests that opinion leaders may be instrumental in disseminating interventions through social networks (Rogers, 19176; Valente & Pumpuang, 2007); this strategy has been used by other HIV prevention researchers since the early 1990s (Kelly et al., 1991; Kelly et al., 1992). Targeting opinion leaders in low-risk venues and asking them to disseminate HIV prevention messages in the high-risk social spaces they attend may be a useful new approach for HIV prevention with YMSM.
Limitations
The present study is subject to a number of limitations which should be considered when one interprets the results. First, because the data were collected in 2005 from YMSM who attended social venues located in Los Angeles, the generalizability of the study’s results may be limited to this time, city and group of men. As a result of the recruitment strategy, YMSM may have been more likely to nominate the venue in which they were recruited then they were to nominate another venue. Twenty-one percent of participants nominated the venue in which they were recruited and thirty-seven percent were recruited when they were in a bar or club; this may be one reason for the large numbers of bars and clubs in the venue network. Furthermore, the name generator of “favorite gay places to socialize” may have encouraged some YMSM to nominate bars and clubs more frequently. In future studies, investigators may want to consider alternative strategies to venue-based sampling when they want to conduct research on venue-based networks of YMSM. Sampling through the internet or mobile phone applications, which has been useful in gathering samples of YMSM previously (Bauermeister, Leslie-Santana, Johns, Pingel, & Eisenberg, 2011; Rice et al., 2012), may be more effective ways to gather venue-based network data that is not biased toward the social space in which the data was collected.
Conclusions
Despite the limitations of the current study, this research provides a foundation for further exploration of the ways in which venues influence sexual risk behavior and substance use among YMSM. Social contexts provides cues to behavioral health decision-making and allow for interpersonal interaction, which may promote or reinforce risk behaviors. Data on where YMSM socialize can be useful in tailoring interventions to specific communities of YMSM and targeting interventions to the social spaces where YMSM may be most amenable to receiving and subsequently disseminating HIV prevention information. In many cases, these social spaces may be low-risk venues that are connected to high-risk venues.
Table 2.
Venue Characteristics (N=110)
| Venue Characteristic | n (%) |
|---|---|
| Venue type | |
| Club | 45 (40.9) |
| Bar | 27 (24.5) |
| Service organization | 8 (7.3) |
| Gym/recreation center | 5 (4.5) |
| Coffee shop/restaurant | 10 (9.1) |
| Adult bookstore | 8 (7.3) |
| Other | 7 (6.4) |
| High-risk venues | 80 (72.7) |
| Geographic location | |
| West Hollywood | 34 (30.9%) |
| Los Angeles | 48 (43.6%) |
| Long Beach | 9 (8.2%) |
| Orange County | 9 (8.2%) |
| Other | 10 (9.1%) |
Acknowledgments
This research was supported by the National Institute on Drug Abuse (F31DA031648) and the National Institute of Mental Health (P30MH058107) of the National Institutes of Health.
Footnotes
There are no disclosures or conflicts of interest to report for any authors.
Portions of this work were presented at the 2012 Annual Meeting of the Society for Prevention Research, Washington, DC.
Contributor Information
Ian W. Holloway, Department of Social Welfare, Luskin School of Public Affairs, University of California, Los Angeles, Los Angeles, California
Eric Rice, School of Social Work, University of Southern California, Los Angeles, CA.
Michele D. Kipke, Saban Research Institute, Children’s Hospital Los Angeles, Departments of Pediatrics and Preventive Medicine, University of Southern California, Los Angeles, CA
References
- Arnett JJ. Emerging adulthood: What is it, and what is it good for? Child Development Perspectives. 2007;1:68–73. [Google Scholar]
- Bauermeister JA, Leslie-Santana M, Johns MM, Pingel E, Eisenberg A. Mr. Right and Mr. Right Now: Romantic and casual partner-seeking online among young men who have sex with men. AIDS and Behavior. 2011;15:261–272. doi: 10.1007/s10461-010-9834-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman KE, Faris R, Ennett ST, Hussong A, Foshee VA. Adding valued data to social network measures: Does it add to associations with adolescent substance use? Social Networks. 2007;29:1–10. [Google Scholar]
- Binson D, Woods WJ, Pollack L, Paul J, Stall R, Catania JA. Differential HIV risk in bathhouses and public cruising areas. American Journal of Public Health. 2001;91:1482–1486. doi: 10.2105/ajph.91.9.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiger RL. The duality of persons and groups. Social Forces. 1974;53:181–190. [Google Scholar]
- Borgatti SP. NETDRAW: Graph visualization software (2.090) [software] Cambridge, MA: Analytic Technologies; 2002. [Google Scholar]
- Borgatti SP, Everett MG, Freeman LC. UCINET for Windows: Software for social network analysis. Cambridge, MA: Analytic Technologies; 2002. [Google Scholar]
- Choi KH, McFarland W, Torsten N, Nguyen S, Louie B, Secura G, Valleroy L. An opportunity for prevention: Prevalence, incidence, and sexual risk for HIV among Asian and Pacific Islander men who have sex with men, San Francisco. Sexually Transmitted Diseases. 2004;31:475–480. doi: 10.1097/01.olq.0000135988.19969.62. [DOI] [PubMed] [Google Scholar]
- Clatts MC, Goldsamt LA, Yi H. Club drug use among young men who have sex with men in NYC: A preliminary epidemiological profile. Substance Use & Misuse. 2005;40:1317–1330. doi: 10.1081/JA-200066898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennett ST, Faris R, Hipp J, Foshee VA, Bauman KE, Hussong A, Cai L. Peer smoking, other peer attributes, and adolescent cigarette smoking: A social network analysis. Prevention Science. 2008;9:88–98. doi: 10.1007/s11121-008-0087-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford WL, Weiss G, Kipke MD, Ritt-Olson A, Iverson E, Lopez D. The Healthy Young Men's Study: Sampling methods to recruit a random cohort of young men who have sex with men. Journal of Gay & Lesbian Social Services. 2009;21:357–373. doi: 10.1080/10538720802498280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman LC. Visualizing social networks. Journal of Social Structure. 2000;1 [Google Scholar]
- Garofalo R, Mustanski BS, McKirnan DJ, Herrick A, Donenberg GR. Methamphetamine and young men who have sex with men: Understanding patterns and correlates of use and the association with HIV-related sexual risk. Archives of Pediatric and Adolescent Medicine. 2007;161:591–596. doi: 10.1001/archpedi.161.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman Erving. Relations in public: Microstudies of the social order. New York, NY: Basic Books; 1971. [Google Scholar]
- Greenwood GL, White EW, Page-Shafer K, Bein E, Osmond DH, Paul J, Stall RD. Correlates of heavy substance use among young gay and bisexual men: The San Francisco Young Men's Health Study. Drug and Alcohol Dependence. 2001;61:105–112. doi: 10.1016/s0376-8716(00)00129-0. [DOI] [PubMed] [Google Scholar]
- Grov C. HIV risk and substance use in men who have sex with men surveyed in bathhouses, bars/clubs, and on Craigslist.org: Venue of recruitment matters. AIDS and Behavior. 2012;16:807–817. doi: 10.1007/s10461-011-9999-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Crow T. Attitudes about and HIV risk related to the “most common place” MSM meet their sex partners: Comparing men from bathhouses, bars/clubs, and Craigslist.org. AIDS Education and Prevention. 2012;24:102–116. doi: 10.1521/aeap.2012.24.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper GW. Sex isn't that simple: Culture and context in HIV prevention interventions for gay and bisexual male adolescents. American Psychologist. 2007;62:803–819. doi: 10.1037/0003-066X.62.8.806. [DOI] [PubMed] [Google Scholar]
- Holloway IW, Cederbaum JA, Ajayi A, Shoptaw S. Where are the young men in HIV prevention efforts? Comments on HIV prevention programs and research from young men who sex with men in Los Angeles County. The Journal of Primary Prevention. 2012;33:271–278. doi: 10.1007/s10935-012-0282-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway IW, Traube D, Kubicek K, Weiss G, Kipke MD. HIV prevention service utilization in the Los Angeles house and ball communities: Past experiences and recommendations for the future. AIDS Education and Prevention. 2012;24:431–444. doi: 10.1521/aeap.2012.24.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway IW, Traube DE, Rice E, Schrager SM, Palinkas LA, Richardson J, Kipke MD. Community and individual factors associated with cigarette smoking among young men who have sex with men. Journal of Research on Adolescence. 2012;22:199–205. doi: 10.1111/j.1532-7795.2011.00774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipke MD, Kubicek K, Weiss G, Wong C, Lopez D, Iverson E, Ford W. The health and health behaviors of young men who have sex with men. Journal of Adolescent Health. 2007;40:342–350. doi: 10.1016/j.jadohealth.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfield TL, Andrew ME. HIV risk behavior reduction following intervention with key opinion leaders of a population: An experimental community-level analysis. American Journal of Public Health. 1991;81:168–171. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, Morgan MG. Community AIDS/HIV risk reduction: The effects of endorsements by popular people in three cities. American Journal of Public Health. 1992;82:1483–1489. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killeya-Jones LA, Nakajima R, Costanzo PR. Peer standing and substance use in early-adolescent grade-level networks: A short-term longitudinal study. Prevention Science. 2007;8:11–23. doi: 10.1007/s11121-006-0053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakon CM, Ennett ST, Norton EC. Mechanisms through which drug, sex partner, and friendship network characteristics relate to risky needle use among high risk youth and young adults. Social Science & Medicine. 2006;6:2489–2499. doi: 10.1016/j.socscimed.2006.06.015. [DOI] [PubMed] [Google Scholar]
- Lee BY, McGlone SM, Song Y, Avery TR, Eubank S, Chang C, Platt R. Social network analysis of patient sharing among hospitals in Orange County, California. American Journal of Public Health. 2011;101:707–713. doi: 10.2105/AJPH.2010.202754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine JH. The sphere of influence. American Sociological Review. 1972;37:14–27. [Google Scholar]
- Mansergh G, Colfax GN, Marks G, Rader M, Guzman R, Buchbinder S. The Circuit Party Men's Health Survey: Findings and implications for gay and bisexual men. American Journal of Public Health. 2001;91:953–958. doi: 10.2105/ajph.91.6.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhib FB, Lin LS, Stueve A, Miller RL, Ford WL, Johnson WD, Smith PJ. A venue-based method for sampling hard-to-reach populations. Public Health Reports. 2001;116:216–222. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: A review of epidemiology, risk and protective factors, and interventions. Journal of Sex Research. 2011;48:218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orellana ER, Picciano JF, Roffman RA, Swanson F, Kalichman SC. Correlates of nonparticipation in an HIV prevention program for MSM. AIDS Education & Prevention. 2006;18:348–361. doi: 10.1521/aeap.2006.18.4.348. [DOI] [PubMed] [Google Scholar]
- Pollock JA, Halkitis PN. Environmental factors in relation to unprotected sexual behavior among gay, bisexual, and other MSM. AIDS Education & Prevention. 2009;21:340–355. doi: 10.1521/aeap.2009.21.4.340. [DOI] [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, Hall HI. Estimated HIV incidence in the United States, 2006–2009. PloS one. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice E, Holloway IW, Winetrobe H, Rhoades H, Barman-Adhikari A, Gibbs J, Dunlap S. Sex risk among young men who have sex with men who use Grindr, a smartphone geosocial networking application. Journal of AIDS and Clinical Research. 2012;S4:1–8. [Google Scholar]
- Rice E, Milburn NG, Monro W. Social networking technology, social network composition, and reductions in substance use among homeless adolescents. Prevention Science. 2011;12:80–88. doi: 10.1007/s11121-010-0191-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers EM. New product adoption and diffusion. Journal of Consumer Research. 1976;2:290–301. [Google Scholar]
- Rutledge SE, Roffman RA, Picciano JF, Kalichman SC, Berghuis JP. HIV prevention and attrition: Challenges and opportunities. AIDS and Behavior. 2002;6:69–82. [Google Scholar]
- Schneider JA, Walsh T, Cornwell B, Ostrow D, Michaels S, Laumann EO. HIV health center affiliation networks of black men who have sex with men: Disentangling fragmented patterns of HIV prevention service utilization. Sexually Transmitted Diseases. 2012;39:598–604. doi: 10.1097/OLQ.0b013e3182515cee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal DW, Kelly JA, Bloom FR, Stevenson LY, Coley BI, Broyels LA. HIV prevention with young men who have sex with men: What young men themselves say they need. AIDS Care. 2000;12:5–26. doi: 10.1080/09540120047431. [DOI] [PubMed] [Google Scholar]
- Solomon TM, Halkitis PN, Moeller RM, Siconolfi DE, Kiang MV, Barton SC. Sex parties and young gay, bisexual, and other men who have sex with men in New York City: Attendance and behavior. Journal of Urban Health. 2011;88:1063–1075. doi: 10.1007/s11524-011-9590-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Friedman M, Catania JA. Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: Health disparities affecting gay and bisexual men in the United States. New York, NY: Oxford University Press; 2007. pp. 251–274. [Google Scholar]
- Tolman DL, McClelland SI. Normative sexuality development in adolescence: A decade in review, 2000–2009. Journal of Research on Adolescence. 2011;21:242–255. [Google Scholar]
- Valdiserri RO. Mapping the roots of HIV/AIDS complacency: Implications for program and policy development. AIDS Education and Prevention. 2004;16:426–439. doi: 10.1521/aeap.16.5.426.48738. [DOI] [PubMed] [Google Scholar]
- Valente TW, Pumpuang P. Identifying opinion leaders to promote behavior change. Health Education & Behavior. 2007;34:881–896. doi: 10.1177/1090198106297855. [DOI] [PubMed] [Google Scholar]
- Vega MY, Roland EL. Social marketing techniques for public health communication: A review of syphilis awareness campaigns in 8 US cities. Sexually Transmitted Diseases. 2005;32:S30–S36. doi: 10.1097/01.olq.0000180461.30725.f4. [DOI] [PubMed] [Google Scholar]
- Vicioso KJ, Parsons JT, Nanin JE, Purcell DW, Woods WJ. Experiencing release: Sex environments and escapism for HIV- positive men who have sex with men. Journal of Sex Research. 2005;42:13–19. doi: 10.1080/00224490509552252. [DOI] [PubMed] [Google Scholar]
- Woods WJ, Binson D, Mayne TJ, Gore LR, Rebchook GM. Facilities and HIV prevention in bathhouse and sex club environments. Journal of Sex Research. 2001;38:68–74. [Google Scholar]
- Wong CF, Kipke MD, Weiss G. Risk factors for alcohol use, frequent use, and binge drinking among young men who have sex with men. Addictive Behaviors. 2008;33:1012–1020. doi: 10.1016/j.addbeh.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]