Abstract
BACKGROUND:
Many children requiring acute care receive suboptimal analgesia.
OBJECTIVES:
To describe paediatric pain management practices and policies in emergency departments (EDs) in Alberta.
METHODS:
A descriptive survey was distributed to each of the EDs in Alberta.
RESULTS:
A response rate of 67% (72 of 108) was obtained. Seventy-one percent (42 of 59) of EDs reported the use of a pain tool, 29.3% (17 of 58) reported mandatory pain documentation and 16.7% (10 of 60) had nurse-initiated pain protocols. Topical anesthetics were reported to be used for intravenous line insertion by 70.4% of respondents (38 of 54) and for lumbar puncture (LP) by 30.8% (12 of 39). According to respondents, infiltrated anesthetic was used for LP by 69.2% (27 of 39) of respondents, and oral sucrose was used infrequently for urinary catheterization (one of 46 [2.2%]), intravenous line insertion (zero of 54 [0%]) and LP (one of 39 [2.6%]).
CONCLUSIONS:
Few Alberta EDs use policies and protocols to manage paediatric pain. Noninvasive methods to limit procedural pain are underutilized. Canadian paediatricians must advocate for improved analgesia to narrow this knowledge-to-practice gap.
Keywords: Analgesia, Emergency, Pain, Paediatrics, Survey
Abstract
HISTORIQUE :
De nombreux enfants qui ont besoin de soins aigus reçoivent une analgésie sous-optimale.
OBJECTIFS :
Décrire les pratiques et politiques de gestion de la douleur en pédiatrie dans les salles d’urgence (SU) albertaines.
MÉTHODOLOGIE :
Chaque SU de l’Alberta a reçu un sondage descriptif.
RÉSULTATS :
Les chercheurs ont obtenu un taux de réponse de 67 % (72 sur 108). Au total, 71 % des SU (42 sur 59) ont déclaré utiliser un outil de gestion de la douleur, 29,3 % (17 sur 58) ont déclaré exiger de consigner la douleur et 16,7 % (dix sur 60) disposaient de protocoles de gestion de la douleur initiés par les infirmières. Ainsi, 70,4 % des répondants (38 sur 54) recouraient à l’anesthésie topique pour insérer un cathéter intraveineux et 30,8 % (12 sur 39), pour effectuer une ponction lombaire (PL). De plus, 69,2 % des répondants (27 sur 39) utilisaient des injections d’anesthésique pour les PL et, rarement, du saccharose par voie orale pour un cathétérisme urinaire (un cas sur 46 [2,2 %]), l’insertion d’un cathéter intraveineux (zéro sur 54 [0 %]) et une PL (un sur 39 [2,6 %]).
CONCLUSIONS :
Un petit nombre de SU albertaines sont dotées des politiques et protocoles pour gérer la douleur en pédiatrie. Les méthodes non invasives sont sous-utilisées pour limiter la douleur liée à des interventions. Les pédiatres canadiens doivent prôner une meil-leure analgésie pour réduire cet écart entre le savoir et la pratique.
Appropriate pain management is considered to be a fundamental human right, and the importance of analgesia in paediatrics has become increasingly recognized (1,2). It is also known that inadequate pain management in infancy or childhood can lead to negative consequences later in life (2–4).
Children are known to be at high risk for undertreatment of pain, or oligoanalgesia. Multiple factors may contribute to this, including difficulty in recognizing and assessing pain in the paediatric patient, a fear of dependency or overprescribing, or the myth that children experience pain differently than adults (1,5,6). The paediatric patient in an emergency setting is at particularly high risk for oligoanalgesia (7,8). Up to three-quarters of patients experience pain in the emergency department (ED) and it is well established that undertreatment of this pain is common (6–10). In the ED setting, children receive less analgesia than adults for similar presentations, and younger children receive less analgesia than older children (5,11,12).
Many safe and effective interventions to lessen pain in paediatric patients are known (13–15), and multiple paediatric and pain societies have endorsed the importance of paediatric pain management. The American Academy of Pediatrics (AAP) recently reaffirmed guidelines for appropriate use of analgesia in the emergency setting (2). However, translation of this knowledge into practice remains an issue (16,17). We sought ED administrator reports of current paediatric pain management strategies in their departments. Because the majority of acutely ill and injured children are treated in general EDs (18,19), we surveyed ED administrators in both paediatric and general EDs, and assessed reported paediatric pain management practices, policies and procedures.
METHODS
Study design
The present study was a descriptive, cross-sectional survey of all ED administrators in Alberta. Of the 108 EDs in Alberta, two are paediatric specific. Nurse managers and medical directors from each of the province’s EDs were contacted simultaneously in 2009. A research assistant initially contacted administrators by telephone, using a database of contact information from a previous study (20). Informed consent was obtained from the administrator at the initiation of the interview, followed by verbal administration of the survey. All ‘failed’ telephone respondents, defined as such after five unsuccessful telephone calls, received a paper-based survey by mail. The Health Research Ethics Board at the University of Alberta (Edmonton, Alberta) approved the present study before its initiation.
Survey tool
Given that no appropriate tool existed in the literature, a novel survey tool was created. Questions were developed based on expert opinion, and were pilot tested for face and content validity (21). Information regarding demographic characteristics of the ED and policies and procedures for pain assessment, documentation and management, as well as perceived barriers and facilitators to optimal paediatric pain management, were assessed. Consistent with current survey implementation practice and ethics board requirements, respondents were permitted to answer or skip any of the questions, leading to a variable response rate for each question.
Data analysis
For dichotomous data, proportions were calculated. Differences among groups were analyzed using Fisher’s exact test (two groups) or the Kruskall-Wallis test for ordered categories. For continuous data, means and SDs were calculated. Comparisons between groups were made using an unpaired t test.
RESULTS
ED characteristics
Of the 108 EDs in Alberta, 72 administrators responded to the survey, resulting in an overall response rate of 67%; however, the proportion answered for each question varied. Both nursing and medical leads were contacted simultaneously; there was only one respondent per hospital ED. Both of Alberta’s paediatric EDs responded to the survey; the remainder of the responses (n=70) were from general EDs that treated both adults and children. Sixty-eight percent (47 of 69) of respondents had a background in nursing and 32% (22 of 69) had a background in medicine; three respondents did not report their background training. The demographic characteristics of the EDs are summarized in Table 1. The mean (± SD) annual patient census was 21,258±17,236. With the two paediatric EDs excluded, the mean paediatric census of general EDs was 21±9.2% of the total. EDs with a larger total patient census were less likely to have a policy for topical anesthetic use (P=0.006). Neither the total patient census nor the paediatric census was associated with the likelihood of pain measurement tool use (P=0.26 and P=0.14) or mandatory pain documentation (P=0.54 and P=0.26), respectively. However, the association between topical anesthetic use and paediatric census approached significance.
TABLE 1.
Emergency department demographic characteristics
| Characteristic | n (%) |
|---|---|
| Total patient census (n=57) | |
| ≤10,000 | 16 (28.1) |
| 10,000−19,999 | 17 (29.8) |
| 20,000−29,999 | 12 (21.1) |
| ≥30,000 | 12 (21.1) |
| Paediatric census (n=38) | |
| <2500 | 15 (39.5) |
| 2500−4999 | 9 (23.7) |
| 5000−9999 | 8 (21.1) |
| 10,000−14,999 | 4 (10.5) |
| ≥15,000 | 2 (5.3)* |
| Nursing staff composition of institutions (n=47) | |
| General emergency department | 32 (68.1) |
| Paediatric ambulatory | 4 (8.5) |
| Paediatric critical care | 4 (8.5) |
| Other | 7 (14.9) |
| Medical staff composition of institutions† (n=19) | |
| CCFP | 18 (94.7) |
| CCFP (EM) | 8 (42.1) |
| FRCPC (EM) | 4 (21.1) |
CCFP Certificant of the Canadian College of Family Physicians; CCFP (EM) CCFP (Emergency Medicine); FRCPC (EM) Fellow of the Royal College of Physicians and Surgeons of Canada (Emergency Medicine)
Represents the two paediatric emegency departments in Alberta;
Medical staff qualifications were only assessed in general emergency departments; categories were not mutually exclusive
Policies and procedures
Most respondents reported use of a pain measurement tool in the ED; the choice of tool is reported in Table 2. Fifty-four percent (22 of 42) of respondents reported that pain was documented more than one-half of the time in the ED. Twenty-nine percent (15 of 51) of respondents reported that the triage nurse was the first to provide analgesia in the ED; 37% reported that this was provided by the bedside nurse (19 of 51) and 29% by the treating ED physician (15 of 51).
TABLE 2.
Reported practice and policies for pain management
| Pain tools | n (%) |
|---|---|
| Use of a pain measurement tool (n=59) | |
| Yes | 42 (71.2) |
| No | 16 (27.1) |
| Unsure | 1 (1.7) |
| Types of pain tools used* (n=42) | |
| Faces Pain Scale | 30 (71.4) |
| Verbal numeric scale | 25 (59.5) |
| Face, Legs, Activity, Cry, Consolability scale | 5 (11.9) |
| Visual analogue scale | 4 (9.5) |
| Topical anesthetics | |
|
| |
| Policy for topical anesthetic use for IV insertion (n=59) | |
| Yes | 15 (25.4) |
| No | 39 (66.1) |
| Unsure | 5 (8.5) |
| Types of topical anesthetics used* (n=64) | |
| EMLA (AstraZeneca, United Kingdom) | 54 (84.4) |
| Ametop (Smith & Nephew, United Kingdom) | 11 (17.2) |
| Maxilene (RGR Pharma, Canada) | 5 (7.8) |
| Lidocaine, epinephrine, tetracaine | 10 (15.6) |
| None | 3 (4.7) |
| Procedural sedation | |
|
| |
| Policy for use of paediatric procedural sedation (n=50) | |
| Yes | 22 (44.0) |
| No | 24 (48.0) |
| Unsure | 4 (8.0) |
| Staff present for paediatric procedural sedation* (n=64) | |
| One staff emergency department medical doctor | 33 (51.6) |
| Two staff emergency department medical doctors | 21 (32.8) |
| Anesthesiologist | 13 (20.3) |
| Registered nurse | 39 (60.9) |
| Respiratory therapist | 9 (14.1) |
Categories were not mutually exclusive and each institution could report ≥1 response. Ametop Topical amethocaine; EMLA Eutectic mixture of local anesthetics; IV Intravenous; Maxilene Liposomal lidocaine
Sixteen percent (10 of 60) of respondents reported that their ED had orders for nurse-initiated paediatric pain management. One-quarter of respondents reported a policy for topical anesthetic use in intravenous line (IV) insertion. Table 2 reports the choice of topical anesthetic. Pain documentation was reported to be mandatory by 29.3% (17 of 58) of respondents and not mandatory by 67.2% (39 of 58); 3.4% (two of 58) were unsure whether such a policy existed.
Most (82.1% [46 of 56]) EDs performed paediatric procedural sedation, and one-half had a policy to guide this practice (Table 2). Eighty-six percent (42 of 49) of respondents reported that an ED physician ordered the paediatric procedural sedation.
Presenting pain management
Figure 1A presents respondents’ reports of ED management of acute otitis media-related pain. The likelihood of the ED treating pain associated with acute otitis media was not significantly associated with paediatric census (P=0.44), the presence of a pain measurement tool (P=1.00), or a policy requiring mandatory pain documentation (P=0.55). Figure 1B presents respondents’ reports of ED management of femur fracture pain in children. The likelihood of the ED treating children’s pain from femur fractures was not significantly associated with paediatric census (P=0.58), the presence of a pain measurement tool (P=1.00) or a policy requiring mandatory pain documentation (P=0.41).
Figure 1).
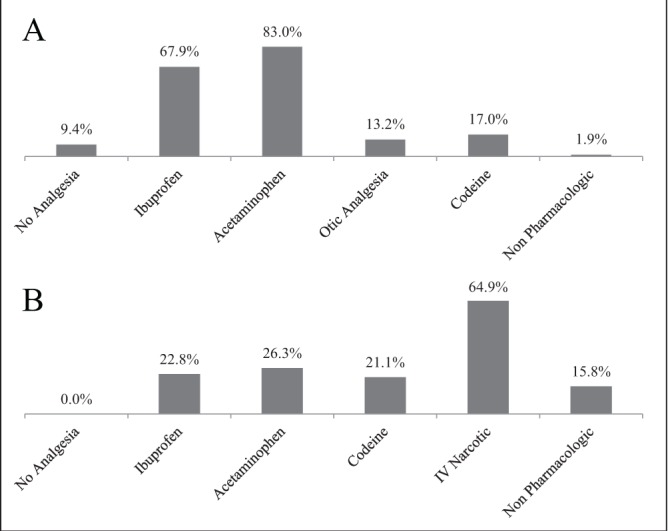
A Reported pain management practices for paediatric acute otitis media (n=53). B Reported pain management practices for paediatric femur fracture (n=57). Percentages refer to percentage of administrators who believed that the named intervention was used ‘often’ or ‘always’ in their emergency department. IV Intravenous
Procedural pain management
Figure 2 presents respondents’ reports of ED management of paediatric pain during urinary catheterization, IV insertion and lumbar puncture (LP). Neither paediatric census nor mandatory pain documentation were significantly associated with provision of analgesia for urinary catheterization (P=0.67 and P=0.46, respectively), IV insertion (P=0.28 and 0.74) or LP (P=0.47 and 0.37).
Figure 2).
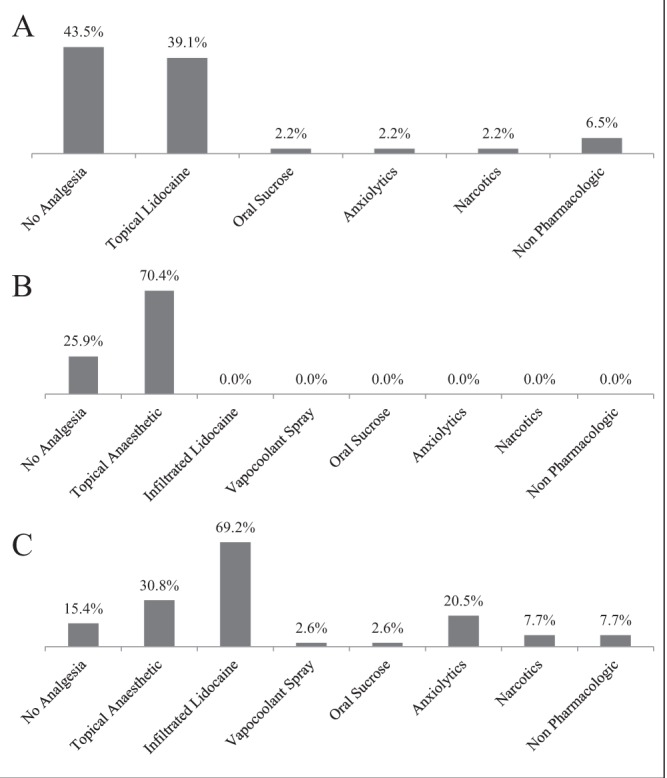
A Reported pain management practices for paediatric urinary catheterization (n=46). B Reported pain management practices for paediatric intravenous line insertion (n=54). C Reported pain management practices for paediatric lumbar puncture (n=39). Percentages refer to percentage of administrators who believed that the named intervention was used ‘often’ or ‘always’ in their emergency department
Nonpharmacological interventions
In children <12 months of age, 33.3% (18 of 54) of respondents reported that their ED allowed breastfeeding and 85.2% (46 of 54) reported use of pacifiers during venipuncture. For IV insertion, most (87.0% [47 of 54]) respondents reported that swaddling was used. When psychological interventions were used to manage needle-related pain, 100% of respondents reported that information (57 of 57) and parent presence/positioning (56 of 56) were used in their ED. Distraction was reported to be used by 98.2% (56 of 57) of respondents, and suggestion by 75.8% (25 of 33). All (57 of 57) respondents reported that parents were allowed to stay in the room during painful procedures.
Ninety-eight percent (56 of 57) of respondents reported that their department did not have a child-life specialist. Only one of the two paediatric EDs had a child-life specialist. Distraction kits were reported to be present in 31.6% (18 of 57) of EDs, while age-appropriate toys were available in 76.8% (43 of 56).
Perceived barriers and facilitators
Reported barriers to optimizing paediatric pain management, resources needed and education desired are reported in Table 3. Paediatric EDs and general EDs reported similar barriers and needs to optimizing analgesia (eg, difficulty in assessing young children’s pain).
TABLE 3.
Reported barriers, changes needed, required resources, and education requirements for optimal paediatric pain management
| Barriers (n=45) | n (%) |
|---|---|
| Education | 14 (31.1) |
| Inexperience/infrequently encountered issue | 12 (26.7) |
| Time constraints | 8 (17.8) |
| Staffing issues | 10 (22.2) |
| Lack of standing orders or policies | 6 (13.3) |
| Lack of treatment options | 4 (8.9) |
| Changes needed (n=37) | |
|
| |
| Additional policies/procedures | 13 (35.1) |
| More education | 10 (27.0) |
| Increased use of distraction techniques | 7 (18.9) |
| More treatment options available | 6 (16.2) |
| Increased focus on analgesia | 5 (13.5) |
| Required resources (n=37) | |
|
| |
| Continuing medical education | 20 (54.1) |
| Policies/protocols developed by experts | 13 (35.1) |
| Additional funding | 3 (8.1) |
| Parent education handouts | 2 (5.4) |
| “Anything available” | 2 (5.4) |
| Educational requirements (n=33) | |
|
| |
| New products/techniques | 14 (42.4) |
| Evidence based practice from other EDs | 11 (33.3) |
| “Anything available” | 4 (12.1) |
| Nonpharmacological interventions | 2 (6.1) |
ED Emergency department
DISCUSSION
To our knowledge, the present study was the first to focus on paediatric pain management in general EDs. In 2009, a multi-centre, prospective study assessing pain management practice in North American general EDs showed that 40% of patients experienced either no change or an increase in their pain during their ED visit (9). Unfortunately, paediatric patients were not analyzed separately from adults in this study. The Pain Management Practices in a Pediatric Emergency Room (PAMPER) study assessed analgesia in one Canadian paediatric ED; pain was documented 60% of the time, and analgesia was provided for only 27% of children (10).
The reported use of analgesia for paediatric patients in Alberta EDs was suboptimal compared with current recommendations from the AAP (2). Suboptimal pain management was particularly evident for procedural pain. Definitive evidence exists regarding the benefits of topical anesthetics in both IV insertion and LP, and the AAP recommends their use (2,15,22). Despite this, only one-quarter of EDs had a policy for topical anesthetic use before IV insertion. Although use of topical anesthetics was reported to be 70% for IV insertion and 30% for LPs, with such strong evidence for their efficacy, one would expect universal use (15,22). Furthermore, eutectic mixture of local anesthetics (AstraZeneca, United Kingdom) was used much more frequently than either amethocaine (Ametop; Smith & Nephew, United Kingdom) or liposomal lidocaine (Maxilene; RGR Pharma, Canada). Given the current evidence regarding efficacy and shortened time to onset, Maxilene or Ametop should be the first-line options for paediatric IV insertion in the ED, where time constraints are a significant issue (15). The barriers to using Maxilene and Ametop are unknown, but may include education, cost and availability.
Oral sucrose was also underutilized; <5% of EDs reported consistent use of oral sucrose for either urinary catheterization or LP. No respondent reported use of oral sucrose for IV insertion. AAP guidelines currently recommend the use of oral sucrose for procedural pain in infants younger than six months of age in the ED (2). A recent systematic review concluded that oral sucrose is both “safe and effective for reducing procedural pain from single events” in infants in the intensive-care setting; a second systematic review for children one to sixteen years of age was unable to draw conclusions on the utility of sucrose for older children due to a paucity of literature evidence (14,23).
Overall, reported pain management was more acceptable for presenting pain (eg, acute otitis media, femur fractures) because most patients received some form of analgesia. However, the choice of analgesia may not have been ideal in all scenarios; patients with a mid-shaft femur fracture were reported to be treated with IV opioids only 65% of the time. Given the severe pain associated with this injury, one would expect almost universal use of opioids. Our study demonstrates a likely knowledge-to-practice gap in the use of effective analgesics for paediatric patients in the ED setting.
Policies to optimize pain management were reportedly lacking. In our study, less than one-third of respondents reported having a policy for mandatory pain documentation. Only one-half reported that pain was frequently documented. This is despite published guidelines and Canadian Triage and Acuity Scale (CTAS) software that mandate universal paediatric pain documentation in the ED (2). In addition, only one-half of EDs reported having a pain tool available at triage, the first point of patient contact and when the AAP recommends initial pain assessment occur (2).
Similarly, although the majority of respondents reported that their ED performed procedural sedation, less than one-half had a policy to undertake this. Despite strong expert recommendations that institutions implement and enforce guidelines when undertaking procedural sedation, it is alarming that so few EDs reported a procedural sedation policy or protocol (24,25). Children are at high risk for complications from procedural sedation, including airway obstruction and apnea (24), and both the AAP and the American Society of Anesthesiologists recommend that an individual trained in advanced management of the paediatric airway be present during sedation in the ED (24,25).
Implementation of pain management policies and procedures can contribute to improved analgesia in both paediatric and general EDs (10,26–28). Although the present study was not primarily designed to demonstrate an association between policies and the likelihood of providing analgesia, this has been previously demonstrated in multiple studies. For example, Corwin et al (26) developed a multistep intervention to improve paediatric analgesia in the ED. Following implementation of this intervention, this group documented a 16% increase in patients receiving analgesia, a 70% increase in pain reassessment by physicians and a 52% increase in the rates of procedural analgesia. Interventions on a smaller scale have also been shown to improve pain management practice. A nurse-directed educational intervention led to a 30% improvement in pain documentation and a 15% increase in the use of nonpharmacological interventions six months after the education (10). Kaplan et al (29) found that including a validated pain scale in the ED electronic medical record improved pain documentation by 30%. This is a key observation, given that other studies have shown that improved pain scoring and documentation naturally leads to increased analgesia use (7,30,31).
Administrators in Alberta were aware that implementing policies and procedures for paediatric pain management could promote optimal care. The most common reported barrier to adequate paediatric analgesia was a lack of education and, accordingly, Alberta administrators expressed a desire for more pain management education for staff. Greater access to policies and protocols for paediatric analgesia was also desired for use in their ED. Interestingly, paediatric EDs indicated similar needs.
The vast majority of children with acute illness and injury are seen outside of paediatric centres (18,19); therefore, paediatricians need to engage community medical leaders and ED administrators to recognize and optimally address paediatric pain. While ED knowledge translation has traditionally been focused within academic centres, recent work by groups such as Translating Emergency Knowledge for Kids (TREKK) (http://trekk.ca) are working to change this by involving community ED practitioners in their efforts.
Limitations
There were several limitations to the present study. Although the overall response rate was acceptable, our survey allowed respondents to leave questions unanswered. This led to smaller response rates for some individual questions and, as such, may have affected our assessments of relationships between groups. Data related to sucrose use were not explicitly limited to the infant age group; therefore, under-reporting may have occurred if respondents considered all children when formulating their response. Demographic data regarding non-respondents were not collected; it is, therefore, possible that they differed from the respondents. However, we are confident that our participating EDs were representative of the entire geographical area that constitutes Alberta. As with all survey studies, selection bias may have led administrators with a greater interest in research to respond; data collected by self-report also carries a risk of both reporting and recall bias. Finally, because the present study was conducted within Alberta, it is unclear whether these results can be extrapolated to other provinces or countries.
CONCLUSION
Children remain at high risk for oligoanalgesia, and our study indicates that their pain is likely undertreated in the acute care setting. Policies and procedures to promote optimal pain management could be implemented, and administrators have identified more education and access to expert-designed policies as key requirements to improve paediatric analgesia practices. As paediatricians, the onus is on us to raise provincial and national awareness of this problem, and partner with policy makers and medical leaders to advocate for consistent, optimal analgesia for children in Canada.
Acknowledgments
The authors thank Ms Yvonne Klatt and Ms Erin Logue for their data entry and cleansing, and Mrs Janie Williamson for coordinating the telephone interviews.
Footnotes
DISCLOSURES: The authors have no financial or other conflicts of interest to disclose. Dr Newton is supported by a Canadian Institutes of Health Research (CIHR) New Investigator Award.
REFERENCES
- 1.Stinson JN, McGrath P. No pain – all gain: Advocating for improved paediatric pain management. Paediatr Child Health. 2007;12:93–4. [PMC free article] [PubMed] [Google Scholar]
- 2.Fein JA, Zempsky WT, Cravero JP, American Academy of Pediatrics, Committee on Pediatric Emergency Medicine and Section on Anesthesiology and Pain Medicine Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics. 2012;130:e1391–405. doi: 10.1542/peds.2012-2536. [DOI] [PubMed] [Google Scholar]
- 3.Anand KJ, International Evidence-Based Group for Neonatal Pain Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med. 2001;155:173–80. doi: 10.1001/archpedi.155.2.173. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy RM, Luhmann J, Zempsky WT. Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics. 2008;122(Suppl 3):S130–3. doi: 10.1542/peds.2008-1055e. [DOI] [PubMed] [Google Scholar]
- 5.Petrack EM, Christopher NC, Kriwinsky J. Pain management in the emergency department: Patterns of analgesic utilization. Pediatrics. 1997;99:711–4. doi: 10.1542/peds.99.5.711. [DOI] [PubMed] [Google Scholar]
- 6.Beattie TF. Pain in the paediatric emergency department. Eur J Emerg Med. 2003;10:255–6. doi: 10.1097/00063110-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Drendel AL, Brousseau DC, Gorelick MH. Pain assessment for pediatric patients in the emergency department. Pediatrics. 2006;117:1511–8. doi: 10.1542/peds.2005-2046. [DOI] [PubMed] [Google Scholar]
- 8.Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20:165–9. doi: 10.1053/ajem.2002.32643. [DOI] [PubMed] [Google Scholar]
- 9.Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: Results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8:460–6. doi: 10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Le May S, Johnston CC, Choiniere M, et al. Pain management practices in a pediatric emergency room (PAMPER) study: Interventions with nurses. Pediatr Emerg Care. 2009;25:498–503. doi: 10.1097/PEC.0b013e3181b0a0af. [DOI] [PubMed] [Google Scholar]
- 11.Alexander J, Manno M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Ann Emerg Med. 2003;41:617–22. doi: 10.1067/mem.2003.138. [DOI] [PubMed] [Google Scholar]
- 12.Dong L, Donaldson A, Metzger R, Keenan H. Analgesic administration in the emergency department for children requiring hospitalization for long-bone fracture. Pediatr Emerg Care. 2012;28:109–14. doi: 10.1097/PEC.0b013e3182442c25. [DOI] [PubMed] [Google Scholar]
- 13.Uman LS, Chambers CT, McGrath PJ, Kisely S. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2006;(4):CD005179. doi: 10.1002/14651858.CD005179.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Stevens B, Yamada J, Lee GY, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2013;(1):CD001069. doi: 10.1002/14651858.CD001069.pub4. [DOI] [PubMed] [Google Scholar]
- 15.Lander JA, Weltman BJ, So SS. EMLA and amethocaine for reduction of children’s pain associated with needle insertion. Cochrane Database Syst Rev. 2006;(3):CD004236. doi: 10.1002/14651858.CD004236.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Stevens B. Challenges in knowledge translation: Integrating evidence on pain in children into practice. Can J Nurs Res. 2009;41:109–14. [PubMed] [Google Scholar]
- 17.MacLean S, Obispo J, Young KD. The gap between pediatric emergency department procedural pain management treatments available and actual practice. Pediatr Emerg Care. 2007;23:87–93. doi: 10.1097/PEC.0b013e31803. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Institute for Health Information. Emergency departments and children in Ontario. 2013. < https://secure.cihi.ca/free_products/aib_apr24_08_en.pdf> (Accessed December 16, 2013).
- 19.Canadian Association of Emergency Physicians Working Group on the Future of Emergency Medicine in Canada The future of emergency medicine in Canada: Submission from CAEP to the Romanow Commission. Part 1. CJEM. 2002;4:359–68. [PubMed] [Google Scholar]
- 20.Johnson DW, Craig W, Brant R, Mitton C, Svenson L, Klassen TP. A cluster randomized controlled trial comparing three methods of disseminating practice guidelines for children with croup [ISRCTN73394937] Implement Sci. 2006;1:10. doi: 10.1186/1748-5908-1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–52. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaur G, Gupta P, Kumar A. A randomized trial of eutectic mixture of local anesthetics during lumbar puncture in newborns. Arch Pediatr Adolesc Med. 2003;157:1065–70. doi: 10.1001/archpedi.157.11.1065. [DOI] [PubMed] [Google Scholar]
- 23.Harrison D, Yamada J, Adams-Webber T, Ohlsson A, Beyene J, Stevens B. Sweet tasting solutions for reduction of needle-related procedural pain in children aged one to 16 years. Cochrane Database Syst Rev. 2011;(10):CD008408. doi: 10.1002/14651858.CD008408.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Cote CJ, Wilson S, American Academy of Pediatrics, American Academy of Pediatric Dentistry, Work Group on Sedation Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: An update. Pediatrics. 2006;118:2587–602. doi: 10.1542/peds.2006-2780. [DOI] [PubMed] [Google Scholar]
- 25.American Society of Anesthesiologists, Task Force on Sedation and Analgesia by Non-Anesthesiologists Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–17. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 26.Corwin DJ, Kessler DO, Auerbach M, Liang A, Kristinsson G. An intervention to improve pain management in the pediatric emergency department. Pediatr Emerg Care. 2012;28:524–8. doi: 10.1097/PEC.0b013e3182587d27. [DOI] [PubMed] [Google Scholar]
- 27.Yanuka M, Soffer D, Halpern P. An interventional study to improve the quality of analgesia in the emergency department. CJEM. 2008;10:435–9. doi: 10.1017/s1481803500010526. [DOI] [PubMed] [Google Scholar]
- 28.Decosterd I, Hugli O, Tamches E, et al. Oligoanalgesia in the emergency department: Short-term beneficial effects of an education program on acute pain. Ann Emerg Med. 2007;50:462–71. doi: 10.1016/j.annemergmed.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 29.Kaplan CP, Sison C, Platt SL. Does a pain scale improve pain assessment in the pediatric emergency department? Pediatr Emerg Care. 2008;24:605–8. doi: 10.1097/PEC.0b013e3181850c1c. [DOI] [PubMed] [Google Scholar]
- 30.Kellogg KM, Fairbanks RJ, O’Connor AB, Davis CO, Shah MN. Association of pain score documentation and analgesic use in a pediatric emergency department. Pediatr Emerg Care. 2012;28:1287–92. doi: 10.1097/PEC.0b013e31827687e6. [DOI] [PubMed] [Google Scholar]
- 31.Silka PA, Roth MM, Moreno G, Merrill L, Geiderman JM. Pain scores improve analgesic administration patterns for trauma patients in the emergency department. Acad Emerg Med. 2004;11:264–70. doi: 10.1111/j.1553-2712.2004.tb02207.x. [DOI] [PubMed] [Google Scholar]


