Abstract
Most major decisions in the intensive care unit (ICU) regarding goals of care are shared by clinicians and someone other than the patient. Multicenter clinical trials focusing on improved communication between clinicians and these surrogate decision makers have not reported consistently improved outcomes. We suggest that acquired maladaptive reasoning may contribute importantly to failure of the intervention strategies tested to date. Surrogate decision makers often suffer significant psychological morbidity in the form of stress, anxiety, depression, and post-traumatic stress disorder. Family members in the ICU also suffer cognitive blunting and sleep deprivation. Their decision-making abilities are eroded by anticipatory grief and cognitive biases, while personal and family conflicts further impact their decision making. We propose recognizing a family ICU syndrome to describe the morbidity and associated decision-making impairment experienced by many family members of patients with acute critical illness (in the ICU) and chronic critical illness (in the long-term, acute care hospital). Research rigorously using models of compromised decision making may help elucidate both mechanisms of impairment and targets for intervention. Better quantifying compromised decision making and its relationship to poor outcomes will allow us to formulate and advance useful techniques. The use of decision aids and improving ICU design may provide benefit now and in the near future. In measuring interventions targeting cognitive barriers, clinically significant outcomes, such as time to decision, should be considered. Statistical approaches, such as survival models and rank statistic testing, will increase our power to detect differences in our interventions.
Keywords: intensive care units, end of life care, life support care, communication, caregivers
As intensive care unit (ICU) physicians, we have come to recognize that our patients’ surrogates are our partners in the collaborative process of clinical decision making, particularly regarding major goals of care (1). We rely on them to know, understand, and try to explain the patients’ wishes through the harrowing process of making the most difficult decisions. The data—and our experience of days filled with multiple family meetings—indicate that the overwhelming majority of end-of-life decisions are made by someone other than the patient (2, 3). As ICU use at the end of life increases (4), these family meetings focusing on the end of life may increase in frequency.
Clinically, a reality often missed in thinking about the family meeting is this: decision making is hard on these surrogates. Yet, as our sophistication in considering patient and family needs and preferences has grown, so too has the opportunity for a nuanced discussion of this reality. Most family members in the ICU suffer clinically significant depression (5). High levels of anxiety are common (6–8). Stress levels are high (8). Symptoms of anxiety and depression can persist long after the ICU (9, 10). Family members involved in the decision-making process are more likely to develop post-traumatic stress disorder (9), a condition that may begin even before their loved one is discharged from the ICU (11). Conflicts between health care team members and families occur frequently (12, 13).
Every ICU practitioner has experienced family members or emotionally involved surrogate decision makers who, despite frequent meetings with what we think is open and effective communication, simply will not reach decisions regarding care of their loved one, particularly near the end of life. Although some of these families may be invoking their interpretation of religious tenets (14), many or most are not. They are seemingly paralyzed in determining goals of care. Some may be distrustful or unwilling to decide. However, we are overlooking another etiology: a proportion of our patients’ families, and their decision makers, are cognitively overwhelmed. They are unable to decide.
We suggest that this disconnect—between the extraordinary demands we place on surrogates, and the limits of what they can actually provide—helps explain one of the fundamental challenges of the communication literature: that many of our most promising interventions do not work when rigorously tested at large scale. We have an observational literature rife with promising associations between aspects of good communication and good outcomes. Rigorous testing of empirically grounded interventions has yielded promising single-center studies (15, 16), but is negative when increased in scale (17–20). These studies all focused primarily on the provider side of the equation, with interventions directed toward our own dissemination and eliciting of information. We have focused on the transmitter, not the receiver.
Recognizing a Syndrome of Maladaptive Thinking and Behavior among Family Members
The evidence in the ICU and across a variety of spectrums indicates that family members, under the burden of critical illness and the illnesses that predisposed their loved ones to the ICU, suffer serious cognitive deficits. Anticipatory grief is associated with worsened problem solving in family caregivers of patients with dementia (21). Among mothers of children with newly diagnosed cancer, 57% suffer worsened problem solving, correlating with neurotic symptoms (22). For the 44% of family caregivers of stroke patients who are depressed, their low problem-solving capabilities correlated with worse Beck depressive inventory scores (23).
Cognitive behavioral therapy has characterized a condition known as “learned helplessness” that results in maladaptive reasoning after stress a person is unable to relieve. The classic example is of a father whose child has incurable leukemia (24). As nothing the father does improves his child’s health, he gives up trying, begins to manifest helpless behavior, and becomes depressed and withdrawn. Disengagement from decision making is one of the main results of learned helplessness, a behavior seen frequently in the ICU (25). A validated measure of learned helplessness was used to assess 499 family members, including 184 surrogate decision makers. Among all family members, including decision makers, more than half suffered significant learned helplessness (8). Their learned helplessness was similar in magnitude to alcoholics entering 12-step programs and unemployed patients with multiple sclerosis. The disengagement from decision making arising from learned helplessness may play a role in the desire of some family members to withdraw from or take a passive role in the decision-making process (26–28).
Family Members of Patients in the ICU Report Being Sleepy and Sleep Deprived (29–31). Because sleep deprivation results in cognitive deficits (32–34), this further threatens surrogate decision making. When these sleep-associated deficits are quantified, the results are startling (35). More than one-half have Epworth sleepiness scores consistent with significant daytime sleepiness, more than two-thirds have Functional Outcome of Sleep Questionnaire-10 scores indicating impairment of daily activities, and 15% of family members and 12% of surrogates have blunted cognition, as measured by psychomotor vigilance testing, consistent with being intoxicated with a blood alcohol content of 0.05–0.10% (36).
Methodical observations that people’s choices often deviate from those based on desirability and utility are not new (37, 38). We see this in the ICU daily. Decision makers for chronically ventilated patients themselves acknowledge the startling gulf between their best judgment and their decisions as surrogates, evidenced by the divergence of their wishes for their own care and the care they choose for their loved ones (39). Patient-designated and next-of-kin surrogates often incorrectly predict end-of-life treatment preferences (40). Decision makers struggle with highly charged personal and family conflicts, not wanting to feel responsible for their loved one’s death, and wishing to avoid family conflict (41). Their decisions are filled with conflict and regret (42).
These deviations from rational decision making may emerge from cognitive bias, common among family members in the ICU. They frequently misinterpret prognoses, unable to overcome optimistic biases (43). This is consistent with studies outside of the ICU, in which people frequently manifest unrealistic optimism regarding possible life events (44), and these expectations can contribute to systematic errors in decision making (45). An additional potential source of cognitive deviation may arise from the base rate bias (also known as the base rate fallacy), in which people may ignore base rates and concentrate on individual information (46). For example, although a particular metastatic malignancy may have a well known median survival, the family member may ignore these data and concentrate instead on their loved one’s perceived hardiness and survival, rather than attempting to integrate the information. Mood, too, can change both the recall and judgment of one’s perception of others (47). This effect of emotion on processing is termed an encoding bias. Multiple studies suggest that individuals are unable to reconcile their current feelings and preferences to those they would have in a different predicament (48).
Affect plays a pivotal role in decision making (45). The importance of this body of literature to decision making in the ICU has begun to be recognized (49, 50). Families’ judgments and decisions are critically influenced by the emotions they experience. Emotions, such as anger and fear, impact decision making (51, 52), and can be a source of systematic bias and reckless behavior in decision making (53, 54), as they relate to cognitive processing. High-intensity affect can also overwhelm cognitive processing or eliminate deliberate decision making altogether (45), potentially explaining some families’ passivity in decision making. In addition, affect may errantly influence families’ determinations of the probability of positive and negative outcomes, perhaps a factor in the discordance between physician and family expectations of ICU outcomes (50, 55). As encouraging individuals to attribute their present emotions to judgment-irrelevant situational factors reduces the tendency for affect to inform judgment (56), helping families acknowledge the causes and focus of their present emotions before making decisions may be beneficial during family meetings. Admittedly, in the highly charged environment of the ICU, strategies aimed at reducing high-intensity affect may be limited (45).
Naming This Syndrome
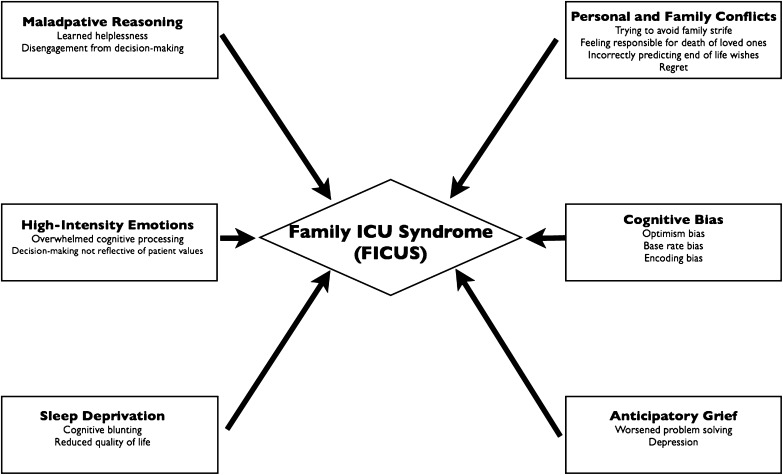
We need to recognize that we face a syndrome of injured and impaired family members. We have already recognized such a syndrome after ICU discharge with the Family Response to Critical Illness, the Post–ICU Syndrome Family (57). We must be cognizant that morbidity begins for many family members as they walk through the doors of the ICU. The family response to acute critical illness is just as real. We propose recognizing a Family ICU Syndrome (FICUS), to describe this syndrome of morbidity and impairment among family members of patients with acute critical illness (in the ICU) and chronic critical illness (in the long-term acute care hospital; Figure 1). The time has come to dispense with the notion that family members are not our patients and look past this (58). Not only are family members the crucial component of end-of-life decision making, they are key determinants of how our surviving patients will fare in the disablement process, whether maintaining independence or having functional limitations become disabilities (59).
Figure 1.
The family intensive care unit syndrome: potential mechanisms.
How Can We Better Study FICUS?
We are in the nascency of discovery, less than 2 decades after our realization that our communication with patients and their families at the end of life was inadequate (20). Giving a name to this syndrome will facilitate its study and characterization. Precisely defining it will be more difficult and require a multidisciplinary approach, including both health care and academic professionals. Some conditions, such as acute stress disorder, major depressive disorder, post-traumatic stress disorder, and complicated grief, are defined by the American Psychiatric Association’s Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (60), and have been previously incorporated into the working definition of the Post–ICU Syndrome Family (57). As such, the input of psychiatrists and psychologists will be essential in modeling the components of FICUS. Sleep medicine participation will be necessary to both characterize the extent of deficit as well as to design potential interventions to mitigate it. Nursing and social work will provide expertise in assessing family conflicts and their effects at the bedside. Defining and explicating cognitive barriers, including biases, maladaptive reasoning, and the effect of high-intensity emotion, will be more complex. Cognitive psychologists and behavioral economists have been studying and grappling with these issues for decades, working across methodological disciplines in doing so. Their intellectual structures, methods, and insights will be vital in developing a complete model of this syndrome. It is crucial that our efforts to delineate this syndrome be used for the benefit and well being of patients’ families to improve patient-centered care, and not usurp the central role of families in ICU decision making. The involvement of medical ethicists will be crucial in this regard.
As discussed previously here, mechanisms underlying cognitive compromise among decision makers are likely complex and multifactorial. We do not yet know exactly which model(s) are best suited to characterize them. Only research rigorously using models of compromised decision making will make this clear. Better quantifying compromised decision making and its relationship to poor outcomes will allow us to formulate and advance useful techniques. For example, the approach of the so-called problem solving intervention is built upon training cognitive appraisal and coping (61). Among caregivers of seriously ill (62, 63) and dying patients (64), this approach provides caregivers with coping skills, increases quality of life, and lowers anxiety. Applying this intervention to caregivers outside the ICU may even improve outcomes for the patients themselves (65). Might it offer similar benefits in the ICU? Other traditional cognitive behavioral theory approaches are labor and resource intensive, and may be difficult to implement in the ICU (66, 67); however, brief Web-based approaches may offer promise (68). Only careful and thoughtful research will determine which, or if any, of the cognitive–behavioral approaches will be effective in reaching this population.
In assessing the effectiveness of future interventions, we must advance our methodology and outcome metrics. Satisfaction is a common measure (69), but tells us little about the decision-making process and its impact on clinical care. From a patient- and family-centric perspective, a decisional conflict scale may tell us more about surrogates’ feelings regarding their choices (70). In addition to measuring patient-centered metrics, we must also evaluate objective clinical outcomes, to assess collaborative decision making with the health care team. Assessment of length of ICU stay and time on mechanical ventilation have previously been measured, but have limitations. These do not reflect the discrete amount of time eligible for intervention, which comes only after the recognition by the team of the need to direct care to comfort, and their communicating this to the family. This may comprise just a fraction of the total ICU length of stay. Including the entire length of stay erodes statistical power, as this decreases the relative effect size (71). This approach cannot distinguish between the death occurring 48 hours after a family meeting in which the decision maker opts for no further aggressive measures and the death that occurs with no limitations of care after 2 days. Time zero should be when the medical team deems limitations of care or changes in the goals of care appropriate, not ICU admission.
We have better statistical approaches—let’s use them. One example is the use of survival models, such as Cox proportional hazards model (72), assessing the time for decision makers to arrive at limitations of care. Survival analyses, including the Cox model, can reduce the number of subjects needed to detect a difference in therapies (73). Death without advance directives or consensus would be a competing outcome, using the statistical method of Fine and Gray (74). Another approach is rank statistic testing (75), which can capture and compare outcomes by desirability. In such an approach, consensus on the day of initial meeting would be the most desirable (i.e., Day 1 is ranked as “1”). Each day after this that is required to reach limitations of care/consensus would be less desirable (3 d until consensus = 3; 8 d until consensus = 8). Death without consensus or limitations on care would be the least desirable of all, and would be assigned a number such as 999. The distribution of these rankings would then be compared between the intervention and control arms. Not only does this approach capture the subtle gradations in outcomes from interventions, it also increases statistical efficiency markedly, and is less affected by extreme values (76).
What Do We Do Now?
Defining the FICUS is crucial, as it will allow identification of families in crisis and help the health care team direct treatments to ameliorate both its deleterious effects on decision making and the morbidity inflicted upon family members. Until we better understand mechanisms and treatments, we can start by simply acknowledging that the family member sitting with us is not only suffering great upheaval and turmoil, but may also be suffering from maladaptive reasoning and cognitive blunting. Doing so may reduce our countertransference associated with conflicts regarding end-of-life care, which are frequent and result in job strain (13).
We need to recognize just how complex the decision-making process is. Under dispassionate, controlled circumstances, it is clear that how we present choices impacts how people arrive at their decisions (77). As discussed previously here, multiple factors in the ICU superimpose on this milieu, making decision making even more problematic. We should recognize that we, as physicians, shape the decisions that these surrogates make. This is the case for the presentation of advanced directives to surrogates (78). Similarly, when patients with serious illness are shown end-of-life care options, they are more likely to choose comfort-oriented care when it is presented as a default choice (79). The use of decision aids may facilitate better decisions by pre-empting physician bias as well as patient barriers to effective decision making (80). This is possible in the ICU: a multicenter pilot study has evaluated the use of a decision aid incorporating graphic depictions of patients’ prognoses and case vignettes to illustrate decision options, along with prompts to assess surrogates’ preferences and understanding (81). Compared with controls, families enrolled in the intervention had lower rates of discordance with physicians, greater medical comprehension, and less decisional conflict. Hospital costs were also lower among the patients whose families participated. As our understanding of the FICUS increases, our knowledge will help refine best design for these decision aids, as well as their implementation.
ICUs need to be designed with families in mind. We know that dedicated meeting rooms reduce the anxiety of family members (82), and that families welcome open visitation policies (83). Current guidelines propose a “family support zone,” which can include foldout furniture for overnight guests (84). Given that sleep deprivation among families is well recognized (85), we should make explicit the need for rooms with a comfortable and clearly demarcated place for family members to sleep. Tertiary care centers should recognize that many of their patients’ families are far from home. These families may need a place to bathe themselves and to wash clothes.
As we build on this emerging foundational research, we can innovate and incorporate these early data and concepts into our practice. When rounding, we always try to remember how profoundly disempowering the ICU environment is to family members. We leave doors open and invite family members to join us on rounds. We show and share the radiographic imaging of their loved ones with them, bringing the adage that “a picture is worth a thousand words” to ICU communication. We ask families about whether they are getting enough sleep and if they have been able to get themselves meals. Looking into the room, we note whether it contains enough reclining chairs so that family members can steal away some sleep. When house officers bitterly lament loggerheads in goals of care with families, it is an opportunity to discuss the data presented here that quantify the immense pain and challenges these family members are confronting.
Conclusions
Our patients’ decision makers are an integral part of the ICU and the care we provide. In this role, they face tremendous burdens and cognitive challenges that can lead to maladaptive reasoning and impaired decision making. It is time to recognize this condition as FICUS. To get to the next level in collaborative decision making, in reaching all of our patients’ families and surrogates, we must identify, rigorously define, and methodically tackle the syndrome of suffering and impaired family members in the ICU. As our thinking and methods increase in sophistication, so should our metrics and statistical approaches. Perhaps by this approach we can substantially improve shared clinical decision making near the end of life in the ICU.
Footnotes
Supported by National Institutes of Health Clinical Research Career Development Award 5K12RR023250-03 (G.N.).
Author Contributions: G.N. and D.R.S. conceived and designed the study, and drafted, critically revised, and approved the manuscript.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Thompson BT, Cox PN, Antonelli M, Carlet JM, Cassell J, Hill NS, Hinds CJ, Pimentel JM, Reinhart K, Thijs LG American Thoracic Society; European Respiratory Society; European Society of Intensive Care Medicine; Society of Critical Care Medicine; Sociètède Rèanimation de Langue Française. Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: executive summary. Crit Care Med. 2004;32:1781–1784. doi: 10.1097/01.ccm.0000126895.66850.14. [DOI] [PubMed] [Google Scholar]
- 2.Smedira NG, Evans BH, Grais LS, Cohen NH, Lo B, Cooke M, Schecter WP, Fink C, Epstein-Jaffe E, May C, et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med. 1990;322:309–315. doi: 10.1056/NEJM199002013220506. [DOI] [PubMed] [Google Scholar]
- 3.Covinsky KE, Goldman L, Cook EF, Oye R, Desbiens N, Reding D, Fulkerson W, Connors AF, Jr, Lynn J, Phillips RS SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. The impact of serious illness on patients’ families. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 4.Teno JM, Gozalo PL, Bynum JP, Leland NE, Miller SC, Morden NE, Scupp T, Goodman DC, Mor V. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309:470–477. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi J, Sherwood PR, Schulz R, Ren D, Donahoe MP, Given B, Hoffman LA. Patterns of depressive symptoms in caregivers of mechanically ventilated critically ill adults from intensive care unit admission to 2 months postintensive care unit discharge: a pilot study. Crit Care Med. 2012;40:1546–1553. doi: 10.1097/CCM.0b013e3182451c58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pochard F, Darmon M, Fassier T, Bollaert PE, Cheval C, Coloigner M, Merouani A, Moulront S, Pigne E, Pingat J, et al. French FAMIREA study group. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death: a prospective multicenter study. J Crit Care. 2005;20:90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Delva D, Vanoost S, Bijttebier P, Lauwers P, Wilmer A. Needs and feelings of anxiety of relatives of patients hospitalized in intensive care units: implications for social work. Soc Work Health Care. 2002;35:21–40. doi: 10.1300/J010v35n04_02. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan DR, Liu X, Corwin DS, Verceles AC, McCurdy MT, Pate DA, Davis JM, Netzer G. Learned helplessness among families and surrogate decision-makers of patients admitted to medical, surgical, and trauma ICUs. Chest. 2012;142:1440–1446. doi: 10.1378/chest.12-0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, et al. FAMIREA Study Group. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171:987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 10.Jones C, Macmillan RR, Griffiths RD. Providing psychological support for patients after critical illness. Clin Intensive Care. 1994;5:176–179. [PubMed] [Google Scholar]
- 11.Paparrigopoulos T, Melissaki A, Efthymiou A, Tsekou H, Vadala C, Kribeni G, Pavlou E, Soldatos C. Short-term psychological impact on family members of intensive care unit patients. J Psychosom Res. 2006;61:719–722. doi: 10.1016/j.jpsychores.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 12.Asch DA, Hansen-Flaschen J, Lanken PN. Decisions to limit or continue life-sustaining treatment by critical care physicians in the United States: conflicts between physicians’ practices and patients’ wishes. Am J Respir Crit Care Med. 1995;151:288–292. doi: 10.1164/ajrccm.151.2.7842181. [DOI] [PubMed] [Google Scholar]
- 13.Azoulay E, Timsit JF, Sprung CL, Soares M, Rusinová K, Lafabrie A, Abizanda R, Svantesson M, Rubulotta F, Ricou B, et al. Conflicus Study Investigators and for the Ethics Section of the European Society of Intensive Care Medicine. Prevalence and factors of intensive care unit conflicts: the Conflicus Study. Am J Respir Crit Care Med. 2009;180:853–860. doi: 10.1164/rccm.200810-1614OC. [DOI] [PubMed] [Google Scholar]
- 14.Brett AS, Jersild P. “Inappropriate” treatment near the end of life: conflict between religious convictions and clinical judgment. Arch Intern Med. 2003;163:1645–1649. doi: 10.1001/archinte.163.14.1645. [DOI] [PubMed] [Google Scholar]
- 15.Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, Barnoud D, Bleichner G, Bruel C, Choukroun G, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356:469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 16.Lilly CM, De Meo DL, Sonna LA, Haley KJ, Massaro AF, Wallace RF, Cody S. An intensive communication intervention for the critically ill. Am J Med. 2000;109:469–475. doi: 10.1016/s0002-9343(00)00524-6. [DOI] [PubMed] [Google Scholar]
- 17.Burns JP, Mello MM, Studdert DM, Puopolo AL, Truog RD, Brennan TA. Results of a clinical trial on care improvement for the critically ill. Crit Care Med. 2003;31:2107–2117. doi: 10.1097/01.CCM.0000069732.65524.72. [DOI] [PubMed] [Google Scholar]
- 18.Curtis JR, Nielsen EL, Treece PD, Downey L, Dotolo D, Shannon SE, Back AL, Rubenfeld GD, Engelberg RA. Effect of a quality-improvement intervention on end-of-life care in the intensive care unit: a randomized trial. Am J Respir Crit Care Med. 2011;183:348–355. doi: 10.1164/rccm.201006-1004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daly BJ, Douglas SL, O’Toole E, Gordon NH, Hejal R, Peerless J, Rowbottom J, Garland A, Lilly C, Wiencek C, et al. Effectiveness trial of an intensive communication structure for families of long-stay ICU patients. Chest. 2010;138:1340–1348. doi: 10.1378/chest.10-0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 21.Fowler NR, Hansen AS, Barnato AE, Garand L. Association between anticipatory grief and problem solving among family caregivers of persons with cognitive impairment. J Aging Health. 2013;25:493–509. doi: 10.1177/0898264313477133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dolgin MJ, Phipps S, Fairclough DL, Sahler OJ, Askins M, Noll RB, Butler RW, Varni JW, Katz ER. Trajectories of adjustment in mothers of children with newly diagnosed cancer: a natural history investigation. J Pediatr Psychol. 2007;32:771–782. doi: 10.1093/jpepsy/jsm013. [DOI] [PubMed] [Google Scholar]
- 23.Shanmugham K, Cano MA, Elliott TR, Davis M. Social problem-solving abilities, relationship satisfaction and depression among family caregivers of stroke survivors. Brain Inj. 2009;23:92–100. doi: 10.1080/02699050802657020. [DOI] [PubMed] [Google Scholar]
- 24.Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: critique and reformulation. J Abnorm Psychol. 1978;87:49–74. [PubMed] [Google Scholar]
- 25.Azoulay E, Pochard F, Chevret S, Arich C, Brivet F, Brun F, Charles PE, Desmettre T, Dubois D, Galliot R, et al. French Famirea Group. Family participation in care to the critically ill: opinions of families and staff. Intensive Care Med. 2003;29:1498–1504. doi: 10.1007/s00134-003-1904-y. [DOI] [PubMed] [Google Scholar]
- 26.Azoulay E, Pochard F, Chevret S, Adrie C, Annane D, Bleichner G, Bornstain C, Bouffard Y, Cohen Y, Feissel M, et al. FAMIREA Study Group. Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Crit Care Med. 2004;32:1832–1838. doi: 10.1097/01.ccm.0000139693.88931.59. [DOI] [PubMed] [Google Scholar]
- 27.Anderson WG, Arnold RM, Angus DC, Bryce CL. Passive decision-making preference is associated with anxiety and depression in relatives of patients in the intensive care unit. J Crit Care. 2009;24:249–254. doi: 10.1016/j.jcrc.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 28.Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, Peters S, Tranmer JE, O’Callaghan CJ. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2003;29:75–82. doi: 10.1007/s00134-002-1569-y. [DOI] [PubMed] [Google Scholar]
- 29.Day A, Haj-Bakri S, Lubchansky S, Mehta S. Sleep, anxiety and fatigue in family members of patients admitted to the intensive care unit: a questionnaire study. Crit Care. 2013;17:R91. doi: 10.1186/cc12736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Horn E, Tesh A. The effect of critical care hospitalization on family members: stress and responses. Dimens Crit Care Nurs. 2000;19:40–49. doi: 10.1097/00003465-200019040-00014. [DOI] [PubMed] [Google Scholar]
- 31.Novaes MA, Knobel E, Bork AM, Pavão OF, Nogueira-Martins LA, Ferraz MB. Stressors in ICU: perception of the patient, relatives and health care team. Intensive Care Med. 1999;25:1421–1426. doi: 10.1007/s001340051091. [DOI] [PubMed] [Google Scholar]
- 32.Killgore WD. Effects of sleep deprivation on cognition. Prog Brain Res. 2010;185:105–129. doi: 10.1016/B978-0-444-53702-7.00007-5. [DOI] [PubMed] [Google Scholar]
- 33.Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res. 2011;191:75–89. doi: 10.1016/B978-0-444-53752-2.00012-6. [DOI] [PubMed] [Google Scholar]
- 34.Tucker AM, Stern Y, Basner RC, Rakitin BC. The prefrontal model revisited: double dissociations between young sleep deprived and elderly subjects on cognitive components of performance. Sleep. 2011;34:1039–1050. doi: 10.5665/SLEEP.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verceles A, Corwin D, Friedman E, Friedman E, McCurdy M, Shanholtz C, Netzer G.Sleepiness and cognitive impairment among family members of the critically ill [abstract]. Am J Respir Crit Care Med2012. 185:A1089 [Google Scholar]
- 36.Williamson AM, Feyer AM, Mattick RP, Friswell R, Finlay-Brown S. Developing measures of fatigue using an alcohol comparison to validate the effects of fatigue on performance. Accid Anal Prev. 2001;33:313–326. doi: 10.1016/s0001-4575(00)00045-2. [DOI] [PubMed] [Google Scholar]
- 37.Kahneman D, Tversky A. An analysis of decision under risk. Econometrica. 1979;47:263–292. [Google Scholar]
- 38.Kahneman D, Tversky A. Choices, values, and frames. Am Psychol. 1984;39:341–350. [Google Scholar]
- 39.Sviri S, Garb Y, Stav I, Rubinow A, Linton DM, Caine YG, Marcus EL. Contradictions in end-of-life decisions for self and other, expressed by relatives of chronically ventilated patients. J Crit Care. 2009;24:293–301. doi: 10.1016/j.jcrc.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 40.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision makers: a systematic review. Arch Intern Med. 2006;166:493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 41.Schenker Y, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM, White DB. I don’t want to be the one saying ‘we should just let him die’: intrapersonal tensions experienced by surrogate decision makers in the ICU. J Gen Intern Med. 2012;27:1657–1665. doi: 10.1007/s11606-012-2129-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hickman RL, Jr, Daly BJ, Lee E. Decisional conflict and regret: consequences of surrogate decision making for the chronically critically ill. Appl Nurs Res. 2012;25:271–275. doi: 10.1016/j.apnr.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers’ interpretation of prognostic information: a mixed-methods study. Ann Intern Med. 2012;156:360–366. doi: 10.1059/0003-4819-156-5-201203060-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weinstein ND. Unrealistic optimism about future life events. J Pers Soc Psychol. 1980;39:806–820. [Google Scholar]
- 45.Loewenstein G, Lerner J.The role of affect in decison makingAnonymous handbook of affective sciences. Oxford, UK: Oxford University Press; 2003. 619–642 [Google Scholar]
- 46.Bar-Hillel M. The base-rate fallacy in probability judgments. Acta Psychol (Amst) 1980;44:211–233. [Google Scholar]
- 47.Forgas JP. On being happy and mistaken: mood effects on the fundamental attribution error. J Pers Soc Psychol. 1998;75:318–331. doi: 10.1037//0022-3514.75.2.318. [DOI] [PubMed] [Google Scholar]
- 48.Van Boven L, Loewenstein G. Social projection of transient drive states. Pers Soc Psychol Bull. 2003;29:1159–1168. doi: 10.1177/0146167203254597. [DOI] [PubMed] [Google Scholar]
- 49.White DB. Rethinking interventions to improve surrogate decision making in intensive care units. Am J Crit Care. 2011;20:252–257. doi: 10.4037/ajcc2011106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.White DB, Cua SM, Walk R, Pollice L, Weissfeld L, Hong S, Landefeld CS, Arnold RM. Nurse-led intervention to improve surrogate decision making for patients with advanced critical illness. Am J Crit Care. 2012;21:396–409. doi: 10.4037/ajcc2012223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Smith CA, Ellsworth PC. Patterns of cognitive appraisal in emotion. J Pers Soc Psychol. 1985;48:813–838. [PubMed] [Google Scholar]
- 52.Ellsworth P, Scherer K.Appraisal processes in emotionDavidson RJ, Scherer KR, Goldsmith HH, editors. Handbook of affective sciences. New York: Oxford University Press; 2003. 572–595 [Google Scholar]
- 53.Averill JR. Studies on anger and aggression. Implications for theories of emotion. Am Psychol. 1983;38:1145–1160. doi: 10.1037//0003-066x.38.11.1145. [DOI] [PubMed] [Google Scholar]
- 54.Berkowitz L. On the formation and regulation of anger and aggression: a cognitive-neoassociationistic analysis. Am Psychol. 1990;45:494–503. doi: 10.1037//0003-066x.45.4.494. [DOI] [PubMed] [Google Scholar]
- 55.Berge KH, Maiers DR, Schreiner DP, Jewell SM, Bechtle PS, Schroeder DR, Stevens SR, Lanier WL. Resource utilization and outcome in gravely ill intensive care unit patients with predicted in-hospital mortality rates of 95% or higher by APACHE III scores: the relationship with physician and family expectations. Mayo Clin Proc. 2005;80:166–173. doi: 10.4065/80.2.166. [DOI] [PubMed] [Google Scholar]
- 56.Keltner D, Locke KD, Audrain PC. The influence of attributions on the relevance of negative feelings to personal satisfaction. Pers Soc Psychol Bull. 1993;19:21–29. [Google Scholar]
- 57.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome–family. Crit Care Med. 2012;40:618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 58.Davidson JE. Time for a formal assessment, treatment, and referral structure for families of intensive care unit patients. Crit Care Med. 2012;40:1675–1676. doi: 10.1097/CCM.0b013e318249594a. [DOI] [PubMed] [Google Scholar]
- 59.Iwashyna TJ, Netzer G. The burdens of survivorship: an approach to thinking about long-term outcomes after critical illness. Semin Respir Crit Care Med. 2012;33:327–338. doi: 10.1055/s-0032-1321982. [DOI] [PubMed] [Google Scholar]
- 60.American Psychiatric AssociationDiagnostic and statistical manual of mental disorders, 5th ed. Arlington, VA: American Psychiatric Association; 2013 [Google Scholar]
- 61.D’Zurilla T, Nezu A.Problem-solving therapy: a positive approach to clinical intervention. New York: Springer Publishing Co.; 2007 [Google Scholar]
- 62.Wade SL, Wolfe C, Brown TM, Pestian JP. Putting the pieces together: preliminary efficacy of a Web-based family intervention for children with traumatic brain injury. J Pediatr Psychol. 2005;30:437–442. doi: 10.1093/jpepsy/jsi067. [DOI] [PubMed] [Google Scholar]
- 63.Gallagher-Thompson D, Lovett S, Rose J, McKibbin C, Coon D, Futterman A, Thompson L.Impact of psychoeducational interventions on distressed family caregivers. J Clinical Geropsychology 2000691–110. [Google Scholar]
- 64.Demiris G, Oliver DP, Washington K, Fruehling LT, Haggarty-Robbins D, Doorenbos A, Wechkin H, Berry D. A problem solving intervention for hospice caregivers: a pilot study. J Palliat Med. 2010;13:1005–1011. doi: 10.1089/jpm.2010.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berry JW, Elliott TR, Grant JS, Edwards G, Fine PR. Does problem-solving training for family caregivers benefit their care recipients with severe disabilities? A latent growth model of the Project CLUES randomized clinical trial. Rehabil Psychol. 2012;57:98–112. doi: 10.1037/a0028229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smith BW, Shelley BM, Dalen J, Wiggins K, Tooley E, Bernard J. A pilot study comparing the effects of mindfulness-based and cognitive–behavioral stress reduction. J Altern Complement Med. 2008;14:251–258. doi: 10.1089/acm.2007.0641. [DOI] [PubMed] [Google Scholar]
- 67.Gross CR, Kreitzer MJ, Russas V, Treesak C, Frazier PA, Hertz MI. Mindfulness meditation to reduce symptoms after organ transplant: a pilot study. Adv Mind Body Med. 2004;20:20–29. [PubMed] [Google Scholar]
- 68.Gluck TM, Maercker A.A randomized controlled pilot study of a brief Web-based mindfulness training. BMC Psychiatry201111:175–244X–11–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Henrich NJ, Dodek P, Heyland D, Cook D, Rocker G, Kutsogiannis D, Dale C, Fowler R, Ayas N. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med. 2011;39:1000–1005. doi: 10.1097/CCM.0b013e31820a92fb. [DOI] [PubMed] [Google Scholar]
- 70.O’Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15:25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- 71.Woodward M.Epidemiology: study design and data analysis. Boca Raton: Chapman & Hall/CRC; 2005 [Google Scholar]
- 72.Cox DR. Regression models and life-tables. J R Stat Soc, B. 1972;34:187–220. [Google Scholar]
- 73.Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Peto J, Smith PG. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. I. Introduction and design. Br J Cancer. 1976;34:585–612. doi: 10.1038/bjc.1976.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fine J, Gray R. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 75.Conover W.Practical nonparametric statisticsAnonymous. New York: John Wiley; 1980. 213–343 [Google Scholar]
- 76.Charache S, Terrin ML, Moore RD, Dover GJ, Barton FB, Eckert SV, McMahon RP, Bonds DR Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia. Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. N Engl J Med. 1995;332:1317–1322. doi: 10.1056/NEJM199505183322001. [DOI] [PubMed] [Google Scholar]
- 77.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 78.Barnato AE, Arnold RM. The effect of emotion and physician communication behaviors on surrogates’ life-sustaining treatment decisions: a randomized simulation experiment. Crit Care Med. 2013;41:1686–1691. doi: 10.1097/CCM.0b013e31828a233d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Halpern SD, Loewenstein G, Volpp KG, Cooney E, Vranas K, Quill CM, McKenzie MS, Harhay MO, Gabler NB, Silva T, et al. Default options in advance directives influence how patients set goals for end-of-life care. Health Aff (Millwood) 2013;32:408–417. doi: 10.1377/hlthaff.2012.0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ubel P.Critical decisions: how you and your doctor can make the right medical choices together. New York: Harper Collins; 2012 [Google Scholar]
- 81.Cox CE, Lewis CL, Hanson LC, Hough CL, Kahn JM, White DB, Song MK, Tulsky JA, Carson SS. Development and pilot testing of a decision aid for surrogates of patients with prolonged mechanical ventilation. Crit Care Med. 2012;40:2327–2334. doi: 10.1097/CCM.0b013e3182536a63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, Grassin M, Zittoun R, le Gall JR, Dhainaut JF, et al. French FAMIREA Group. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29:1893–1897. doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 83.Schnell D, Abadie S, Toullic P, Chaize M, Souppart V, Poncet MC, Schlemmer B, Azoulay E. Open visitation policies in the ICU: experience from relatives and clinicians. Intensive Care Med. 2013;39:1873–1874. doi: 10.1007/s00134-013-2956-2. [DOI] [PubMed] [Google Scholar]
- 84.Thompson DR, Hamilton DK, Cadenhead CD, Swoboda SM, Schwindel SM, Anderson DC, Schmitz EV, St Andre AC, Axon DC, Harrell JW, et al. Guidelines for intensive care unit design. Crit Care Med. 2012;40:1586–1600. doi: 10.1097/CCM.0b013e3182413bb2. [DOI] [PubMed] [Google Scholar]
- 85.Schmidt M, Azoulay E. Sleepless nights in the ICU: the awaken family. Crit Care. 2013;17:1003. doi: 10.1186/cc12781. [DOI] [PMC free article] [PubMed] [Google Scholar]