Abstract
Hyperreactio luteinalis is a rare entity in which there is bilateral, benign, functional multicystic ovarian enlargement during pregnancy, which is most commonly seen in third trimester. This condition is usually innocuous and does not need any specific treatment. However, many a times, it is mistaken for ovarian malignancy and inadvertently operated upon. This is a case report of a 24-year-old female with a partial molar pregnancy associated with hyperreactio luteinalis who was followed up for regression of the same and normalization of beta human chorionic gonadotropin (hCG) levels.
Keywords: Beta human chorionic gonadotropin, hyper reactio luteinalis, ovarian hyperstimulation syndrome
Introduction
Hyperreactio luteinalis, a rare condition occurring where there are elevated levels of beta human chorionic gonadotropin. It is characterized by benign enlargement of bilateral ovaries with presence of many thin walled cysts. These are often mistaken for malignant pathologies and hence should be borne in mind.
Case Report
A 24-year-old G2 P2 L1 female came for a regular antenatal scan at menstrual age of 13 weeks and 3 days. The scan revealed a missed abortion dated 7 weeks [Figure 1]. Bilateral ovaries were enlarged: Right ovary, 140 × 102 mm and left ovary, 107 × 66.9 mm [Figures 2 and 3]. There were multiple thin-walled cysts with clear contents in bilateral ovaries, the largest one being about 6.6 cm. There was no solid component and no areas of calcification. Vascularity in both adnexae was preserved. There was no ascites or pleural effusion. Based on this USG, provisional diagnosis of hyperreactio luteinalis (HL) was put forth.
Figure 1.
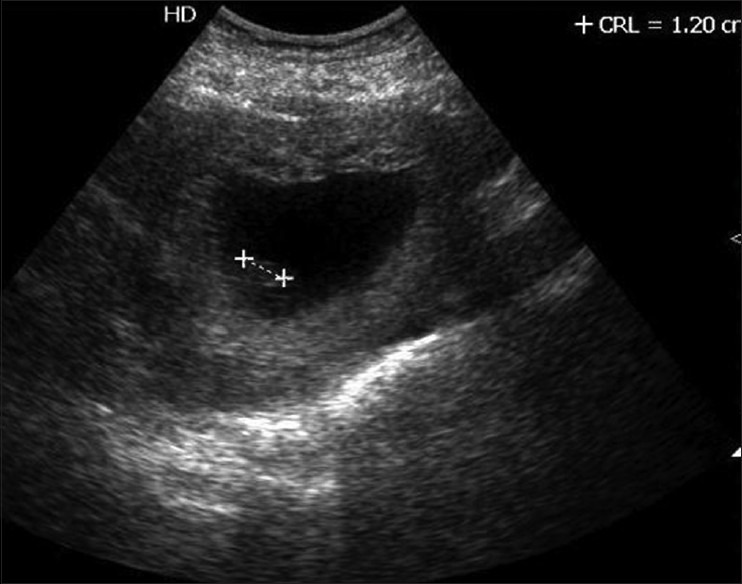
Gravid uterus with a fetal pole corresponding to about 7 weeks
Figure 2.
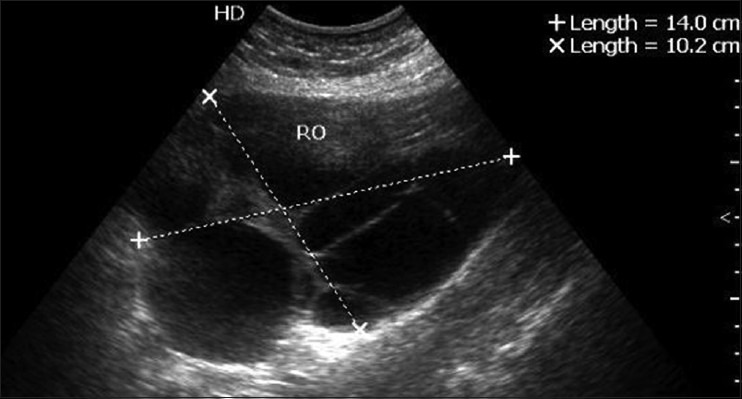
Enlarged right ovary measuring about 140 × 102 mm, with multiple thin-walled, clear cysts
Figure 3.
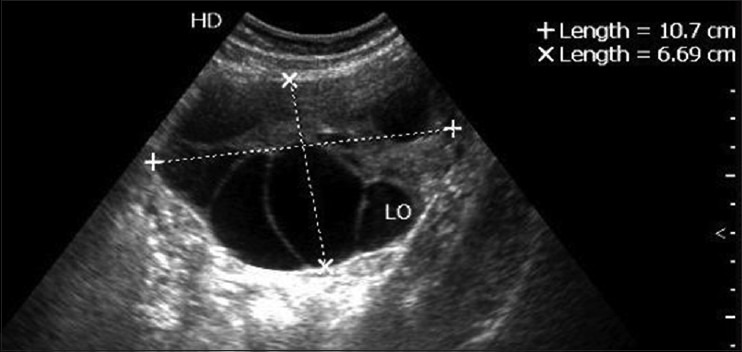
Left ovary measures 107 × 66.9 mm with multiple thin-walled cysts having clear contents
Following this, serum beta human chorionic gonadotropin (β HCG) was estimated which was 74,780 mIU/ml corresponding to about 10th-13th weeks of gestation. This confirmed the diagnosis of HL. The patient was fully evaluated and her history reviewed. She was not suffering from hypothyroidism, polycystic ovarian disease (PCOD), and not undergoing any infertility treatment. This had been a spontaneously conceived pregnancy.
In view of missed abortion, the patient underwent dilatation and evacuation. Histopathologic analysis revealed a partial molar pregnancy. The patient was followed up for 3 months till the β hCG values normalized to 4.7 mIU/ml. The patient also underwent serial USG scans which showed that post-evacuation, the ovaries reduced in size to; right ovary 90 × 38 mm and left ovary 48 × 36 mm at the end of 1 month [Figures 4 and 5] and at the end of second month were right ovary 40 × 26.6 mm and left ovary 32 × 31 mm. This patient is placed on a monthly follow-up with estimation of serum β hCG levels.
Figure 4.
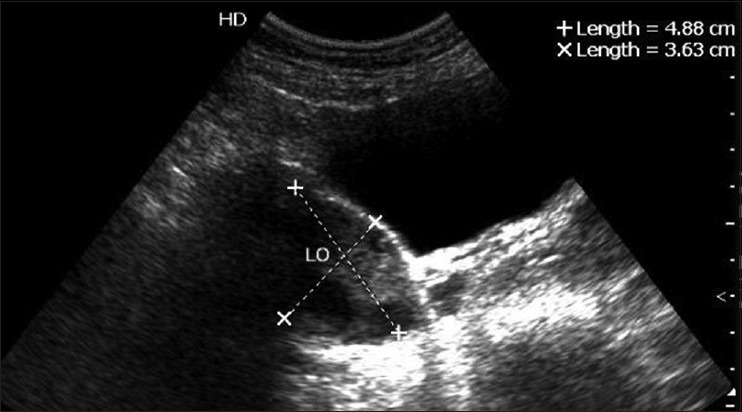
Follow-up USG after 1 month shows reduction in size of right ovary, measuring 9 × 3.8 cms
Figure 5.
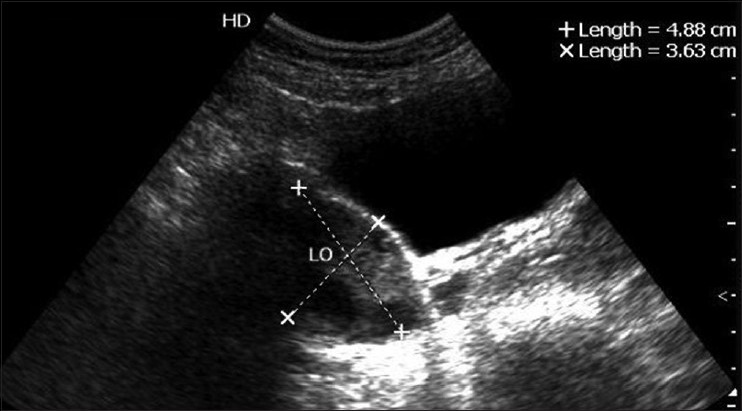
Follow-up USG after 1 month showing reduction in size of left ovary, which measured 4.8 × 3.6 cms
Discussion
HL is a rare condition observed in cases where there is elevated level of β HCG, like in gestational trophoblastic disease, multiple pregnancies, and hydrops fetalis.[1] It is seen in approximately 25% of molar pregnancy and 10% of choriocarcinoma.[2]
This condition is also seen in patients with PCOD due to an increased sensitivity of the ovarian stroma to β hCG.[3] It has also been seen in association with diabetes mellitus complicated pregnancy, ovulation induction, and clomiphene intake.[2] Our patient had no comorbidity and it had normally conceived pregnancy. These cysts are rarely seen in the first trimester of molar pregnancy and are even more rarely seen in association with partial mole due to insufficient amount of β hCG,[2] making our case a rarity among rarities.
HL cysts are characteristically enlarged ovaries, with multiple thin-walled clear theca leutein cysts within them.[2] Pathophysiology of the cysts is similar to ovarian hyperstimulation syndrome (OHSS); however, they can be differentiated by the fact that OHSS is iatrogenic whereas HL is a spontaneous occurrence.[4] HL is mostly seen in the third trimester and OHSS in the first trimester. However, our case presented in the first trimester. HL tends to be asymptomatic, whereas OHSS presents with symptoms of acute fluid imbalance. HL can also mimic ovarian malignancies like mucinous borderline tumor of intestinal type;[5] however, they are differentiated by the fact that they have smaller thin-walled cysts and not as much solid component as seen in HL.[6] They can be differentiated from the same based on β hCG levels, ovarian tumor markers, and imaging modality correlation like USG and magnetic resonance imaging (MRI).[7,8]
Most of these patients are asymptomatic. This condition, being self-limiting in course, most often does not need any intervention/medications.[9] Based on the size of these multicystic ovaries, the patients may have pain or may undergo torsion, cyst rupture, or pelvic entrapment of enlarged ovary, which then becomes a surgical emergency.[10] These patients may develop hyperandrogenism due to elevated β hCG levels[6] and require appropriate management.
Conclusion
The importance of knowing this entity is that it is a benign, self-limiting ovarian pathology which does not need any specific treatment except in cases of surgical emergencies like ovarian torsion. The self-limiting nature of this condition advocates a conservative management and necessitates differentiation from other malignant mimics.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Haq AN. Hyperreatio luteinalis assoicated with pregnancy induced hypertension. J Coll Physicians Surg Pak. 2010;20:137–9. [PubMed] [Google Scholar]
- 2.Hashmi HA, Tufail A. Hyperreatio luteinalis in association with molar pregnancy. Pak J Surg. 2008;24:140–2. [Google Scholar]
- 3.Mittal N, Mittal S, Dhadwal V, Swarupa PV. Hyper-reactio luteinalis associated with hypothyroidism. JK Science. 2005;7:104–6. [Google Scholar]
- 4.Foulk Ra, Martin MC, Jerkins GL, Laros RK. Hyperreactio luteinalis differentiated from severe ovarian hyperstimulation syndrome in a spontaneously conceived pregnancy. Am J Obstet Gynecol. 1997;176:1300–2. doi: 10.1016/s0002-9378(97)70349-1. [DOI] [PubMed] [Google Scholar]
- 5.Simsek Y, Celen S, Ustun Y, Danisman N, Bayramoglu H. Severe preeclampsia and fetal virilization in a spontaneous singleton pregnancy complicated by hyperreactio luteinalis. Eur Rev Med Pharmacol Sci. 2012;16:118–21. Eur Rev Med Pharmacol Sci 2012 Jan; 16 (1):118-21. [PubMed] [Google Scholar]
- 6.Van Holsbeke C, Amant F, Veldman J, De Boodt A, Moerman P, Timmerman D. Hyperreactio luteinalis in a spontaneously conceived singleton pregnancy. Ultrasound Obstet Gynecol. 2009;33:371–3. doi: 10.1002/uog.6325. [DOI] [PubMed] [Google Scholar]
- 7.Abe T, Ono S, Igarashi M, Akira S, Watanabe A, Takeshita T. Conservative management of hyperreactio luteinalis: A case report. J Nippon Med Sch. 2011;78:241–5. doi: 10.1272/jnms.78.241. [DOI] [PubMed] [Google Scholar]
- 8.Takeuchi M, Matsuzaki K, Nishitani H. MR manifestations of hyperreactio luteinalis: Value of diffusion-weighted imaging in the differentiation from neoplastic lesions. Proc Intl Soc Mag Reson Med. 2009;17:4143. [Google Scholar]
- 9.Cho AR, Song TB, Kim HJ, Kim YH, Kim JW. Vaginal delivery in a spontaneously conceived singleton pregnancy complicated with hyperreactio luteinalis: A case report. J Womens Med. 2011;4:53–6. [Google Scholar]
- 10.Lynn KN, Steinkeler JA, Wilkins-Haug LE, Benson CB. Hyperreactio luteinalis (enlarged ovaries) during the second and third trimesters of pregnancy: Common clinical associations. J Ultrasound Med. 2013;32:1285–9. doi: 10.7863/ultra.32.7.1285. [DOI] [PubMed] [Google Scholar]


