Abstract
Background
The recommendations in guidelines are based on evidence; however, there is a gap between recommendations and clinical practice.
Objective
To describe the practice of prescribing evidence-based treatments for patients with acute coronary syndrome in Brazil.
Methods
This study carried out a subanalysis of the ACCEPT registry, assessing epidemiological data and the prescription rate of acetylsalicylic acid, p2y12 inhibitors, antithrombotic drugs, beta-blockers, angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers (IAT1RB), and statins. In addition, the quality of myocardial reperfusion in ST-segment elevation myocardial infarction was evaluated.
Results
This study assessed 2,453 patients. The prescription rates of acetylsalicylic acid, p2y12 inhibitors, antithrombotic drugs, beta-blockers, angiotensin-converting enzyme inhibitors/IAT1RB, and statins were as follows: in 24 hours - 97.6%, 89.5%, 89.1%, 80.2%, 67.9% and 90.6%; and at six months - 89.3%, 53.6%, 0%, 74.4%, 57.6% and 85.4%, respectively. Regarding ST-segment elevation myocardial infarction, only 35.9% and 25.3% of the patients underwent primary angioplasty and thrombolysis, respectively, within the recommended times.
Conclusion
This registry showed high initial prescription rates of antiplatelet drugs, antithrombotic drugs, and statins, and lower prescription rates of beta-blockers and angiotensin-converting enzyme inhibitors/IAT1RB. Independently of the class, the use of all drugs decreased by six months. Most patients with ST-segment elevation myocardial infarction did not undergo myocardial reperfusion within the time recommended.
Keywords: Evidence based practice, Acute coronary syndrome, Disease registries, Epidemiology
Introduction
In Brazil, cardiovascular diseases account for approximately 30% of the deaths of patients aged from 20 to 59 years1. In 2009, acute myocardial infarction (AMI) was the second major cause of death (96,386 individuals)2, representing an incidence of 48 deaths per 100,000 inhabitants1. In addition to the loss of lives, the social costs are worthy of note; for example, chest pain was the cause of approximately 100,000 visits to basic health care units1 and more than 200,000 hospitalizations in 20103. Those figures have increased over the years4.
Most deaths due to AMI have occurred outside the hospital, 80% of which within the first 24 hours5. In-hospital mortality has ranged from 3% to 20%5, and morbidity (post-AMI heart failure) has ranged from 5% to 15%1. That great variation in mortality is due to the quality of the health care provided1. Accurate early treatment improves survival and quality of life. The guidelines of the Brazilian Society of Cardiology5,6 (SBC) and of other international societies7,8 have aimed at guiding clinical practice, providing evidence-based recommendations supported by scientific rigor. That tool has proved to improve the quality of the health care provided9; in addition, centers implementing such recommendations have lower event rates. However, there is a gap between medical practice and guidelines. This study aimed at assessing the treatment provided in the Acute Coronary Care Evolution of Practice (ACCEPT) Registry and at comparing it with that in the Brazilian and North-American guidelines for acute coronary syndrome.
Methods
The ACCEPT Registry has been conceived by the SBC. Its methodology, organization and data collection have already been described in detail10. Briefly, 65 centers in Brazil have contributed to build the registry. Such centers were gathered according to two criteria: invitation and active search (via the SBC web page). The ACCEPT Registry was aimed to be as comprehensive as possible, regarding both the Brazilian territorial coverage and the profile of the patients cared for (public and private systems). Data were collected from January 2011 to December 2012. The 30-day results of the registry have been previously reported11.
This study is a subanalysis prespecified in that registry planning and included all patients of the registry, whose inclusion criteria were as follows: patients with acute coronary syndrome without ST-segment elevation [unstable angina and non-ST-segment elevation AMI (NSTEMI), the latter characterized by clinical findings and electrocardiographic (ECG) or cardiac enzyme changes]; and patients with ST-segment elevation AMI (STEMI), characterized by clinical findings and ECG changes of ST-segment elevation. Patients whose data were not complete were excluded.
The primary objective was to assess the prescription rate of drugs known to have an impact on cardiovascular events, such as: antiplatelet agents [acetylsalicylic acid (ASA) and p2y12 inhibitors]; beta-blockers; angiotensin-converting enzyme inhibitors (ACEI); angiotensin-receptor blockers (AT1RB); and statins. The primary objective was to assess the impact of that therapy on major cardiac events (death, AMI, cardiopulmonary arrest, stroke and major bleeding).
This study was approved by the committee on ethics and research of the Instituto de Ensino e Pesquisa of the Hospital do Coração of São Paulo (IEP/HCOR) (registry number 117/2010). All participants provided written informed consent, and the study abided by guidelines, Resolution 196/96 of the Brazilian Council of Health, good medical practices and the Declaration of Helsinki.
The ACCEPT Registry belongs to and was funded by the SBC. The IEP/HCOR was hired to build that registry under the SBC coordination.
Statistical analysis
The continuous variables were described as mean and standard deviation. The categorical variables were described as absolute and relative frequencies. For comparison, the chi-square test was used, except for the age means, for which the ANOVA F test was used. When comparing continuity of drug prescription over time, a model was adjusted for generalized estimating equations (GEE) for binary data to consider the dependence between the observations. The statistical program R 2.15.3 was used in the statistical analysis. A 5% significance level was considered.
Results
From August 2010 to December 2011, 2,584 patients were included, of whom, 2,453 completed a one-year follow-up and 40 were excluded due to incomplete follow-up, with a 2.6% loss.
Table 1 shows the epidemiological profile of the patients. Mean age ranged from 61 to 65 years. The male sex predominated in all three clinical conditions: 58.9%, 73.4% and 70% for unstable angina, NSTEMI and STEMI, respectively. The patients with unstable angina, as compared with the others, had a higher incidence of the risk factors dyslipidemia, hypertension, and smoking habit, and a higher prevalence of heart failure (HF) (67.3%, 84.1%, 30.4% and 15%, respectively). It is worth noting, in the NSTEMI group, the presence of lower rates of dyslipidemia (44.4%), of previous AMI (18.2%) and of diabetes mellitus (23.6%), and, in the STEMI group, a lower mean age (61 ± 12 years) and a high rate of diabetics (37.5%) and smokers (29.3%). The incidence of stroke was similar in the three clinical conditions.
Table 1.
Epidemiological profile
| Unstable angina (767) | NSTEMI (800) | STEMI (846) | p | |
|---|---|---|---|---|
| Age (mean ± SD) | 64 ± 12 | 65 ± 12 | 61 ± 12 | < 0.001 |
| Male sex, n (%) | 452 (58.9) | 587 (73.4) | 592 (70) | < 0.001 |
| Dyslipidemia, n (%) | 516 (67.3) | 355 (44.4) | 490 (57.9) | < 0.001 |
| Previous AMI, n (%) | 275 (35.9) | 146 (18.2) | 304 (35.9) | < 0.001 |
| SAH, n (%) | 645 (84.1) | 544 (68) | 66 (78.8) | < 0.001 |
| Diabetes mellitus, n (%) | 246 (32.1) | 189 (23.6) | 317 (37.5) | < 0.001 |
| Heart failure, n (%) | 119 (15.5) | 54 (6.8) | 92 (10.9) | < 0.001 |
| Obesity, n (%) | 272 (35.5) | 261 (32.6) | 270 (31.9) | 0.285 |
| Smoking, n (%) | 233 (30.4) | 199 (24.9) | 248 (29.3) | < 0.001 |
| Stroke, n (%) | 68 (8.9) | 53 (6.6) | 68 (8) | 0.247 |
NSTEMI: non-ST-segment elevation myocardial infarction; STEMI: ST-segment elevation myocardial infarction; SD: standard deviation; AMI: acute myocardial infarction; SAH: systemic arterial hypertension.
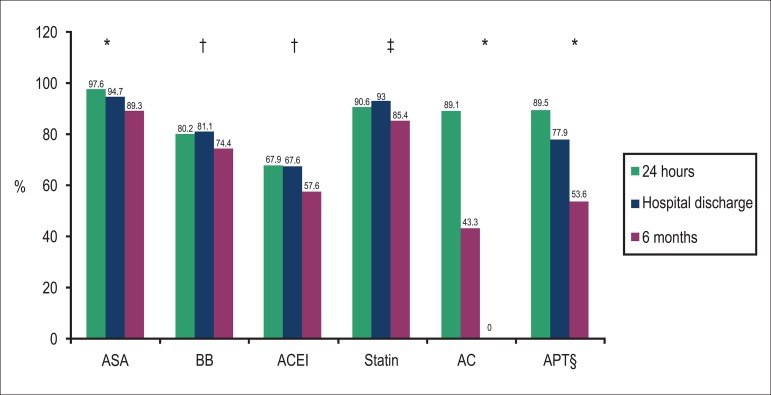
Of the drugs with an impact on acute coronary syndrome, ASA was the most often prescribed, with rates ranging from 97.6% on admission to 89.3% at six months (Figure 1). The prescription rate of statins on admission was also high (90.6%). However, analyzing beta-blockers, ACEI/AT1RB, antithrombotic agents (unfractionated heparin, low-molecular weight heparin and fondaparinux heparin) and p2y12 inhibitors, prescription rates below 90% on admission were observed (80.2%, 67.9%, 89.1% and 88.7%, respectively).
Figure 1.
Drug prescription rates in acute coronary syndrome within the first 24 hours, on hospital discharge, and at 6 months.
§ Except ASA; * significant reduction (p < 0.05) at all three specified times; † significant reduction only at 6 months; ‡ significant increase on hospital discharge compared to the first 24 hours and significant reduction at 6 months. ASA: acetylsalicylic acid; BB: beta-blocker; ACEI: angiotensin-converting enzyme inhibitor; AC: anticoagulants; APT: antiplatelet drug (p2y12 inhibitor).
Comparing the drug prescription rate on hospital discharge with that six months after the index event, a reduction was observed for all drugs, but more marked for ACEI/AT1RB, p2y12 inhibitors and beta-blockers [absolute reduction of 10% (67.6% to 57.6%), 24.5% (77.5% to 53%) and 6.7% (81.1% to 74.4%), respectively] (Figure 1).
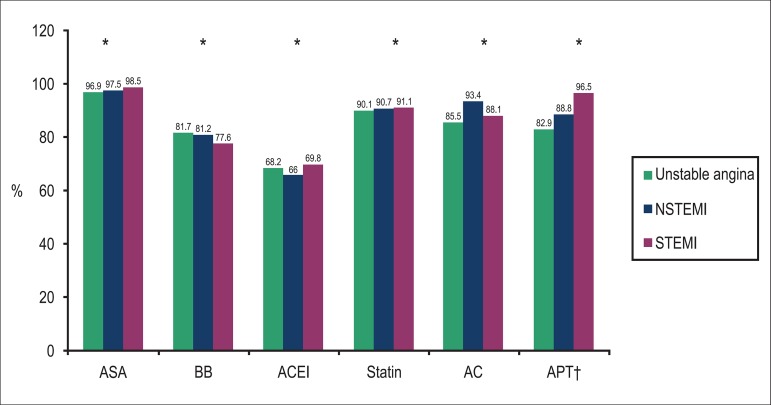
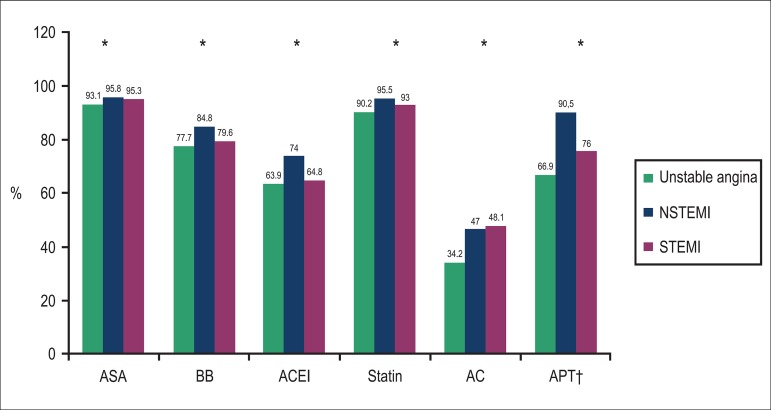
Assessing the drug prescription rate according to the clinical findings, antiplatelet drugs (p2y12 inhibitor) were more often prescribed in patients with STEMI, followed by patients with NSTEMI and unstable angina (96.5% vs. 88.5% vs. 82.9%, respectively). Antithrombotic drugs were more often used in patients with NSTEMI (93.4% vs. 88.1% vs. 85.5% for NSTEMI, STEMI and unstable angina, respectively). The prescription rates of the other drugs were similar in the three conditions (unstable angina, NSTEMI and STEMI) as follows: ASA, 96.9% vs. 97.5% vs. 98.5%; ACEI, 68.2% vs. 66% vs. 69.8%; beta-blocker, 81.7% vs. 81.2% vs. 77.6%; and statin, 90.1% vs. 90.7 vs. 91.1%, respectively. Only the prescription rates of ASA and statins were over 90% in the three different conditions (Figure 2). In general, the prescription rate of statin increased from 90.6% to 93% on hospital discharge (Figure 3). The ASA prescription rate remained stable, but the reductions in the prescription rates of ACEI and beta-blockers were greater in unstable angina, 4.3% and 3.4%, respectively.
Figure 2.
Drug prescription rates in acute coronary syndrome according to the clinical findings (unstable angina, NSTEMI and STEMI) on patient’s admission (24 hours).
† Except ASA; * p < 0.05. ASA: acetylsalicylic acid; BB: beta-blocker; ACEI: angiotensin-converting enzyme inhibitor; AC: anticoagulants; APT: antiplatelet drug (p2y12 inhibitor); NSTEMI: non-ST-segment elevation myocardial infarction; STEMI: ST-segment elevation myocardial infarction.
Figure 3.
Drug prescription rates in acute coronary syndrome according to the clinical findings (unstable angina, NSTEMI and STEMI) on hospital discharge.
† Except ASA; * p<0.05. ASA: acetylsalicylic acid; BB: beta-blocker; ACEI: angiotensin-converting enzyme inhibitor; AC: anticoagulants; APT: antiplatelet drug (p2y12 inhibitor); NSTEMI: non-ST-segment elevation myocardial infarction; STEMI: ST-segment elevation myocardial infarction.
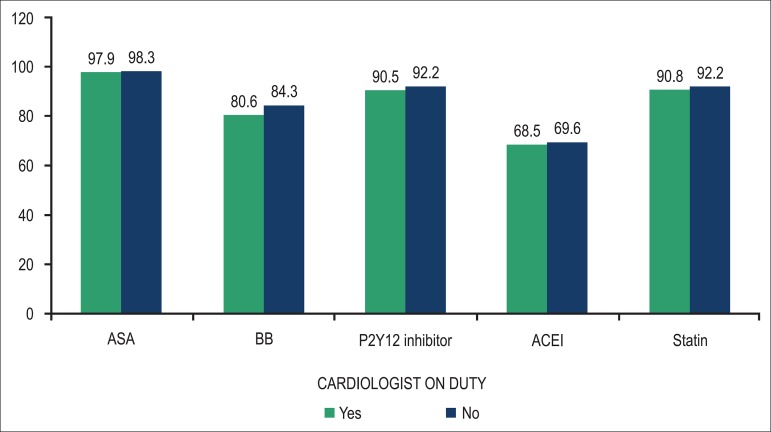
The presence of a cardiologist at the emergency room did not significantly increase evidence-based drug prescription rates, which were as follows according to the presence vs. absence of a cardiologist, respectively: ASA, 97.9% vs. 98.3%; beta-blocker, 80.6% vs. 84.3%; ACEI, 68.5% vs. 69.6%; statin, 90.8% vs. 92.2%; p2y12 inhibitor, 90.5% vs. 92.2% (Figure 4).
Figure 4.
Drug prescription rates in acute coronary syndrome according to the presence or absence of a cardiologist on duty on patient’s admission.
ASA: acetylsalicylic acid; BB: beta-blocker; ACEI: angiotensin-converting enzyme inhibitor.
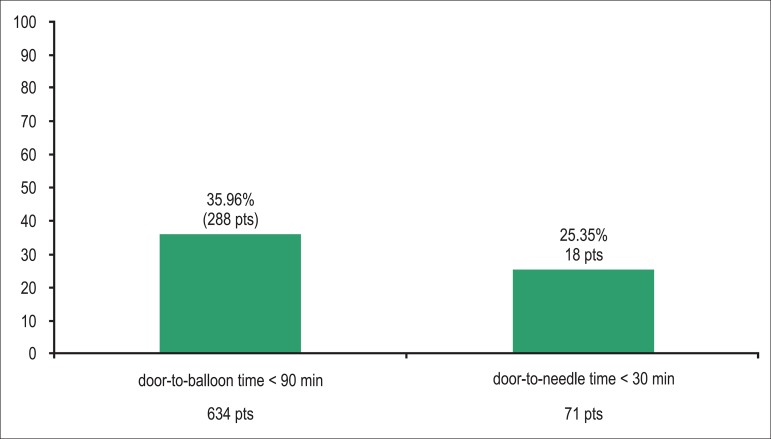
Of the 846 patients admitted with STEMI, 705 (83.3%) received reperfusion therapy as follows: 71 with thrombolytic agents and 643 with primary angioplasty. Of the patients undergoing primary angioplasty, only 35.96% (n = 288) had a door-to-balloon time < 90 minutes, while among those undergoing thrombolysis, that rate was even lower (n = 18; 25.35%) (Figure 5).
Figure 5.
Patients admitted with ST-segment elevation acute myocardial infarction, who met the requirements for myocardial reperfusion.
pt: patients; min: minutes.
The use of beta-blockers, ACEI/AT1RB and statins proved to impact the rate of major cardiac events already on admission, with reductions in the relative risk at 12 months of 46.3% (p = 0.016), 31.9% (p < 0.001) and 39.9% (p = 0.003), respectively (Table 2). The benefit of ASA became apparent only on the sixth month, an effect maintained in the long run, with a 38% relative reduction at 12 months (p = 0.013). The use of the p2y12 inhibitor reduced the cardiac event rate, but without statistical significance (p = 0.305).
Table 2.
Combined clinical events (death, reinfarction, cardiopulmonary arrest, stroke and severe bleeding) according to drug use
| 30 days n (%) | 6 months n (%) | 12 months n (%) | |
|---|---|---|---|
| ASA | |||
| Yes | 140 (6.1) | 225 (10.8) | 269 (14.8) |
| No | 12 (9.4) | 21 (18.4)* | 27 (23.9)* |
| Clopidogrel | |||
| Yes | 111 (5.9) | 183 (10.7) | 296 (14.8) |
| No | 41 (7.6) | 63 (13) | 75 (17) |
| Beta-blocker | |||
| Yes | 92 (4.7) | 160 (9.1) | 199 (12.9) |
| No | 58 (12.7)** | 83 (39)** | 94 (24.4)* |
| ACE/AT1RB | |||
| Yes | 79 (4.8) | 136 (9.2) | 169 (13.2) |
| No | 73 (9.3)** | 110 (15.6)** | 127 (19.4)** |
| Statin | |||
| Yes | 127 (5.7) | 214 (10.5) | 261 (14.6) |
| No | 25 (14.7)** | 32 (21.1)** | 35 (24.3)** |
p < 0.05;
p < 0.001.
ASA: acetylsalicylic acid; ACEI/AT1RB: angiotensin-converting enzyme inhibitors/angiotensin-receptor blocker
Discussion
The most important findings in our registry were as follows: high prescription rates of antiplatelet drugs and statin in the first 24 hours; lower prescription rates of beta-blockers and ACEI/AT1RB; a significant reduction in the number of patients on medication, especially p2y12 inhibitors, ACEI/AT1RB, and beta-blockers six months after the event; less than half of the patients underwent myocardial reperfusion within the time limits established in the guidelines.
Compared to the Global Registry of Acute Coronary Events (GRACE)12 and the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines) Initiative9, the prescription rates of the five major drugs were higher in this registry. However, the time period in which those data were collected should be considered, as well as the programs of disclosure and implementation of the guidelines conducted during such period1,13. The ACute Coronary Events - a multinational Survey of current management Strategies (ACCESS) registry14, carried out in developing countries, to which Brazil has also contributed, has an epidemiological profile similar to that of the ACCEPT registry. They have also reported lower prescription rates of beta-blockers and thienopyridines. When compared to two other Brazilian registries2,3 recently published, the drug prescription rates were higher in this registry, which can be explained by the method of selecting the centers and the profile of patients3.
Fermann et al.15 have reported that patients who received appropriate acute treatment upon hospital admission were more likely to be discharged on guideline-recommended therapy. However, in this study sample, the presence of a cardiologist at the emergency room on patient's admission did not increase the prescription rate of drugs that modify the natural history of acute coronary syndrome.
Usually, ASA is highly used in all Brazilian2,3 and international14,16 registries. In this study sample, a high initial prescription rate of p2y12 inhibitors was observed, and, as compared to those registries previously published, that occurred to the detriment of the use of glycoprotein (GP) IIb/IIIa inhibitors. Such result differs from that of the Acute Coronary Treatment and Intervention Outcomes Network (ACTION registry), which has reported higher prescription rates of GP IIb/IIIa inhibitors; despite the class I recommendation for clopidogrel, this drug was prescribed only to 59% of the patients, and, even more alarming, 28% of the patients received no double antiplatelet therapy17. The low prescription rate of GPIIb/IIIa inhibitors in this registry might result from an association between a reduction in the recommendation grade and their elevated cost. The use of new antiplatelet drugs, such as prasugrel and ticagrelor, in this registry is low, possibly because it was only recently that they began to be commercialized in Brazil, during the conduction of this registry.
Angiotensin-converting enzyme inhibitors and AT1RB belong to a well-established class of drugs for the treatment of patients with HF. The Heart Outcomes Prevention Evaluation Study Investigators (HOPE)18 has shown that patients at high cardiovascular risk, such as those with post-AMI diabetes mellitus, who do not necessarily have systolic ventricular dysfunction also derive great benefit from ACEI therapy. Bagnall et al.19 have reported that nonprovision of that class of drugs may be due to subjective underestimation of patient risk and, hence, likely treatment benefit.
It is worth noting that patients who would derive the greatest benefit from medication are precisely those who most seldom receive a prescription20 (risk-treatment paradox)19. That paradox was observed in the present registry. Considering the clinical conditions in decreasing grade of severity, that is STEMI, NSTEMI and unstable angina, the rate of treatment with ACEI and beta-blockers was not proportional to the severity of the clinical findings. Regarding beta-blockers, contraindications, such as bronchial asthma, chronic obstructive pulmonary disease, bradycardia, and shock, are causes of nonprovision of those drugs19; however, most of the time, the reason is not apparent20.
The delay to reperfusion in patients with STEMI has also been observed in other registries21. In the National Registry of Myocardial Infarction (NRMI), the percentage of patients reaching a door-to-balloon time under 90 minutes was only 29.3%22, and the mean door-to-needle time of 32 minutes21. Those figures have decreased over time, mainly due to the creation of registries, which are useful to assess the performance of the services participating in them21.
In the CRUSADE Initiative, the hospitals with the greatest adherence to guidelines, the parameters assessed including the prescription of antiplatelet drugs, beta-blockers, ACEI/AT1RB and statins on hospital discharge, have shown lower mortality, with a reduction from 6.31% to 4.15%9. Usually controlled clinical studies assess an isolated effect of a drug. Mukherjee et al.23 have shown the synergic effect of the combined use of the above-mentioned four classes of drugs in acute coronary syndrome, with an odds ratio of 0.36 for one drug, and of 0.10 for four drugs.
During hospitalization, the physician is responsible for drug prescription. In addition to assessing criteria for drug use, that professional has to consider contraindications and adverse effects of the drug in question. The lack of physicians' adherence to guidelines is multifactorial, ranging from considering that the guidelines interfere with their autonomy and recognizing the difficulty of acquiring new treatment methods15, until underestimating the disease's severity19. In addition to the factor 'physician', after hospital discharge, there is the variable 'patient', who does not use the drug prescribed due to the following reasons: drug cost; subjective perception that the drug does not improve symptoms; not understanding the benefit of treatment; fear of and difficulty in using several drugs19. The association of all those factors result in low adherence, which already begins on the first contact.
Limitations
This registry's great limitation is being a nonrandomized observational study, in which the causality between the facts observed and the clinical outcomes cannot be inferred. Another limitation is the profile of the centers contributing to the data bank, 90% of which are tertiary hospitals with hemodynamic laboratories11, known to have greater adherence to guidelines19,23. The contribution to the ACCEPT registry of centers with fewer resources is important to provide a real image of the quality of the care provided to the Brazilian population; thus, the implantation of new health care models, with draining systems from primary to more complex centers, in several Brazilian cities should be considered24,25.
Neither the reasons why physicians do not prescribe a certain drug nor the long-term adherence were assessed in this registry. In addition, the number of patients meeting the secondary prevention goals was not evaluated.
Conclusion
The quality of the care provided to patients with acute coronary syndrome in the ACCEPT registry, assessed by the percentage of patients on the drugs known to improve survival in that syndrome, is greater than that of other international registries. However, considering the ideal drug prescription rate as being close to 95%, there is still room for improvement4. The SBC initiative of promoting the creation of registries in several areas of cardiology, reflecting the health care provided to patients with cardiovascular disease, will allow the improvement of the quality of that care by both the SBC and the government.
Footnotes
Author contributions
Conception and design of the research: Santos ES, Piva e Mattos LA, Berwanger O, Andrade JP; Acquisition of data: Neuenschwander FC, Moreira CM, Santos ES, Reis HJL, Romano ER, Piva e Mattos LA, Berwanger O, Andrade JP; Statistical analysis and Analysis and interpretation of the data: Wang R, Piva e Mattos LA, Berwanger O; Obtaining funding: Piva e Mattos LA, Berwanger O, Andrade JP; Writing of the manuscript: Wang R, Neuenschwander FC, Lima Filho A, Moreira CM; Critical revision of the manuscript for intellectual content: Wang R, Neuenschwander FC, Lima Filho A, Moreira CM, Berwanger O.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Study Association
This study is not associated with any post-graduation program.
Sources of Funding
This study was funded by Sociedade Brasileira de Cardiologia.
References
- 1.Andrade JP, Piva e Mattos LA, Carvalho AC, Machado CA, Oliveira GM. National physician qualification program in cardiovascular disease prevention and integral care. Arq Bras Cardiol. 2013;100(3):203–211. doi: 10.5935/abc.20130061. [DOI] [PubMed] [Google Scholar]
- 2.Nicolau JC, Franken M, Lotufo PA, Carvalho AC, Marin JA, Neto, Lima FG, et al. Utilização de terapêuticas comprovadamente úteis no tratamento da coronariopatia aguda: comparação entre diferentes regiões brasileiras. Análise do registro brasileiro de síndromes coronarianas agudas (BRACE - Brazilian Registry on Acute Coronary Syndromes) . Arq Bras Cardiol. 2012;98(4):282–289. [Google Scholar]
- 3.Piegas LS, Avezum A, Guimaraes HP, Muniz AJ, Reis HJ, dos Santos ES, et al. Acute coronary syndrome behavior: results of a brazilian registry. Arq Bras Cardiol. 2013;100(6):502–510. doi: 10.5935/abc.20130101. [DOI] [PubMed] [Google Scholar]
- 4.Berwanger O, Piva e Mattos LA, Martin JF, Lopes RD, Figueiredo EL, Magnoni D, et al. Evidence-based therapy prescription in high-cardiovascular risk patients: the react study. Arq Bras Cardiol. 2013;100(3):212–220. doi: 10.5935/abc.20130062. [DOI] [PubMed] [Google Scholar]
- 5.Piegas LS, Feitosa G, Mattos LA, Nicolau JC, Rossi JM, Neto, Timerman A, et al. Sociedade Brasileira de Cardiologia Diretriz da Sociedade Brasileira de Cardiologia sobre tratamento do infarto agudo do miocárdio com supradesnível do segmento ST. Arq Bras Cardiol. 2009;93(6) supl.2:e179–e264. [PubMed] [Google Scholar]
- 6.Nicolau JC, Timerman A, Piegas LS, Marin-Neto JA, Rassi A., Jr Guidelines for unstable angina and non-ST-segment elevation myocardial infarction of the Brazilian Society of Cardiology (II Edition, 2007) Arq Bras Cardiol. 2007;89(4):e89–e131. doi: 10.1590/s0066-782x2007001600015. [DOI] [PubMed] [Google Scholar]
- 7.O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. American College of Emergency Physicians. Society for Cardiovascular Angiography and Interventions 2013 ACCF/AHA guideline for the management of st-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, et al. 2012 ACCF/AHA focused update incorporated into the accf/aha 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(23):e179–e347. doi: 10.1016/j.jacc.2013.01.014. Erratum in: J Am Coll Cardiol. 2013;62(11):1040-1. [DOI] [PubMed] [Google Scholar]
- 9.Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295(16):1912–1920. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]
- 10.Mattos LA. Rationality and methods of ACCEPT registry - Brazilian registry of clinical practice in acute coronary syndromes of the Brazilian Society of Cardiology. Arq Bras Cardiol. 2011;97(2):94–99. doi: 10.1590/s0066-782x2011005000064. [DOI] [PubMed] [Google Scholar]
- 11.Piva e Mattos LA, Berwanger O, dos Santos ES, Reis HJ, Romano ER, Petriz JL. Desfechos clínicos aos 30 dias do Registro Brasileiro das Síndromes Coronárias Agudas (ACCEPT) Arq Bras Cardiol. 2013;100(1):6–13. doi: 10.1590/s0066-782x2013000100003. [DOI] [PubMed] [Google Scholar]
- 12.Fox KA, Goodman SG, Klein W, Brieger D, Steg PG, Dabbous O, et al. Management of acute coronary syndromes: variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (grace) . Eur Heart J. 2002;23(15):1177–1189. doi: 10.1053/euhj.2001.3081. [DOI] [PubMed] [Google Scholar]
- 13.Gibler WB, Cannon CP, Blomkalns AL, Char DM, Drew BJ, Hollander JE, et al. American Heart Association Council on Clinical Cardiology . Council on Cardiovascular Nursing, and Quality of Care and Outcomes Research Interdisciplinary Working Group. Society of Chest Pain Centers Practical implementation of the guidelines for unstable angina/non-st-segment elevation myocardial infarction in the emergency department: a scientific statement from the American Heart Association Council on Clinical Cardiology (subcommittee on acute cardiac care), council on cardiovascular nursing, and quality of care and outcomes research interdisciplinary working group, in collaboration with the society of chest pain centers. Circulation. 2005;111(20):2699–2710. doi: 10.1161/01.CIR.0000165556.44271.BE. [DOI] [PubMed] [Google Scholar]
- 14.ACCESS Investigators Management of acute coronary syndromes in developing countries: acute coronary events - a multinational survey of current management strategies. Am Heart J. 2011;162(5):852–859. doi: 10.1016/j.ahj.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 15.Fermann GJ, Raja AS, Peterson ED, Roe MT, Hoekstra JW, Milford-Beland S, et al. Early treatment for non-ST-segment elevation acute coronary syndrome is associated with appropriate discharge care. Clin Cardiol. 2009;32(9):519–525. doi: 10.1002/clc.20629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steg PG, Goldberg RJ, Gore JM, Fox KA, Eagle KA, Flather MD, et al. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (Grace) Am J Cardiol. 2002;90(4):358–363. doi: 10.1016/s0002-9149(02)02489-x. [DOI] [PubMed] [Google Scholar]
- 17.Alexander JH. The current state of antiplatelet therapy in acute coronary syndromes: the data and the real world. Cleve Clin J Med. 2009;76(Suppl 1):S16–S23. doi: 10.3949/ccjm.76.s1.03. [DOI] [PubMed] [Google Scholar]
- 18.Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342(3):145–153. doi: 10.1056/NEJM200001203420301. Erratum in N Engl J Med. 2000;342(10):748; N Engl J Med. 2000;342(18):1376. [DOI] [PubMed] [Google Scholar]
- 19.Bagnall AJ, Yan AT, Yan RT, Lee CH, Tan M, Baer C, et al. Canadian Acute Coronary Syndromes Registry II Investigators Optimal medical therapy for non-ST-segment-elevation acute coronary syndromes: exploring why physicians do not prescribe evidence-based treatment and why patients discontinue medications after discharge. Circ Cardiovasc Qual Outcomes. 2010;3(5):530–537. doi: 10.1161/CIRCOUTCOMES.109.919415. [DOI] [PubMed] [Google Scholar]
- 20.Viskin S, Kitzis I, Lev E, Zak Z, Heller K, Villa Y, et al. Treatment with beta-adrenergic blocking agents after myocardial infarction: from randomized trials to clinical practice. J Am Coll Cardiol. 1995;25(6):1327–1332. doi: 10.1016/0735-1097(94)00552-2. [DOI] [PubMed] [Google Scholar]
- 21.Gibson CM. NRMI and current treatment patterns for ST-elevation myocardial infarction. Am Heart J. 2004;148(5) Suppl:S29–S33. doi: 10.1016/j.ahj.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 22.Moscucci M, Eagle KA. Door-to-balloon time in primary percutaneous coronary intervention: is the 90-minute gold standard an unreachable chimera? . Circulation. 2006;113(8):1048–1050. doi: 10.1161/CIRCULATIONAHA.105.606905. [DOI] [PubMed] [Google Scholar]
- 23.Mukherjee D, Fang J, Chetcuti S, Moscucci M, Kline-Rogers E, Eagle KA. Impact of combination evidence-based medical therapy on mortality in patients with acute coronary syndromes. Circulation. 2004;109(6):745–749. doi: 10.1161/01.CIR.0000112577.69066.CB. [DOI] [PubMed] [Google Scholar]
- 24.Caluza AC, Barbosa AH, Gonçalves I, Oliveira CA, Matos LN, Zeefried C, et al. Rede de infarto com supradesnivelamento de st: Sistematização em 205 casos diminui eventos clínicos na rede pública. Arq Bras Cardiol. 2012;99(5):1040–1048. doi: 10.1590/s0066-782x2012005000100. [DOI] [PubMed] [Google Scholar]
- 25.Marcolino MS, Brant LC, Araujo JG, Nascimento BR, Castro LR, Martins P, et al. Implantação da linha de cuidado do infarto agudo do miocárdio no município de belo horizonte. Arq Bras Cardiol. 2013;100(4):307–314. [PubMed] [Google Scholar]