Abstract
Background
The prevalence of hypertension among children and adolescents is estimated to range between 1% and 13%. Excess weight and central obesity are related to blood pressure levels in adults, and may be important in the early pathogenesis of SH when present in childhood.
Objectives
To study the association between anthropometric variables and blood pressure levels in schoolchildren from the 5th and 8th grades, and to identify which parameter was more strongly correlated with blood pressure levels.
Methods
Contemporary cross-sectional study with probabilistic population-based cluster sampling of schoolchildren enrolled from the 5th to the 8th grades in public elementary schools of Porto Alegre. Data on familial risk factors and anthropometry were collected. Statistical analysis included correlations and cluster-adjusted confidence intervals.
Results
The mean age of participants was 12.57 (± 1.64) years, and 55.2% of them were females. Abnormal blood pressure levels were found in 11.3% of the sample and borderline values, in 16.2%. Among the anthropometric variables analyzed, hip circumference was the one with the strongest correlation with increased blood pressure (r = 0.462, p < 0.001), followed by waist circumference (r = 0.404, p < 0.001) and abdominal skinfold (r = 0.291, p < 0.001).
Conclusion
We observed an association of waist circumference and skinfolds with increased blood pressure levels in the schoolchildren of the sample. Therefore, it is of the utmost importance that early measurements of blood pressure, and waist and hip circumferences become a routine in health services in order to prevent this condition.
Keywords: Anthropometry, Body Weights and Measures, Child, Blood Pressure, Adolescents
Introduction
According to the World Health Organization (WHO), systemic hypertension (SH) is the major cause of cardiovascular diseases in adulthood, accounting for 62% of strokes and 49% of coronary artery diseases1. Approximately 30% of the worldwide adult population may be classified as hypertensive2; in Brazil, the prevalence of SH is of 22.3% to 43.9%3. Among children and adolescents, the prevalence of SH ranges from 1% to 13%4. SH found in adults may have started in childhood, and this is known as the tracking phenomenon4.
Lifestyles that lead to atherosclerosis may begin in childhood, and the prevalence of risk factors has increased in this age range5. If these conditions persist, it is likely that diseases previously observed only in elderly populations will become a cause of morbidity and mortality in young adults and adolescents5. Pathological changes resulting from atherosclerosis may be identified before the onset of clinical signs of the disease6; by the end of adolescence, approximately 61% of individuals show some type of atherosclerotic lesion in the coronary arteries. After 40 years of age, this figure reaches 95% of the population6.
Recent United States National Institutes of Health (NIH)'s guidelines for the treatment of obesity in adults stress the importance of recognizing excess body weight and central adiposity as health risks7. Body mass index (BMI) is used as a global excess weight indicator, whereas waist circumference (WC) has been advocated as a central obesity indicator8,9, and seems to be related to the development of cardiovascular diseases, type-2 diabetes mellitus, and premature death10,11. WC has been pointed as the best anthropometric predictor of cardiovascular risk factors among children and adolescents, including increased blood pressure levels12, sensitivity to insulin13, and metabolic syndrome14.
Therefore, the objective of this study is to identify the association between anthropometric variables and blood pressure levels among schoolchildren from the 5th to the 8th grades in the city of Porto Alegre. Additionally, we seek to evaluate which, among the variables studied, is the one with the strongest correlation with blood pressure levels. Thus, by means of its results, this study will contribute to the investigation of a more effective screening and an adequate planning of preventive measures.
Methods
This is a contemporary population-based cross-sectional study conducted by the research group of the Preventive Pediatric Cardiology Outpatient Clinic of the Institute of Cardiology and University Foundation of Cardiology of Rio Grande do Sul (IC-FUC) from 2004 to 2007. Its methodology has been described elsewhere5.
This project was approved by the Research Ethics Committees of IC-FUC and of the Federal University of Health Sciences Foundation of Porto Alegre (Fundação Universidade Federal de Ciências da Saúde de Porto Alegre - UFCSPA).
A population-based probabilistic cluster sample was selected by lot from a list of all public schools from the municipal, state and federal network of elementary school of Porto Alegre supplied by the State Board of Education. The schoolchildren assessed were attending from the 5th to the 8th grades of elementary school.
Individuals regularly enrolled in the participating schools were included; those with diseases or chronic conditions that prevented physical evaluation were excluded.
Data was collected as follows: first, the schools were contacted in relation to the project, receiving thorough information on the activities planned. After parents or guardians had given informed consent and the child had been included, the parents were sent a questionnaire on family history of cardiovascular diseases and another one addressing physical activity, exercise, and sedentary lifestyle. When the questionnaire was returned, physical evaluation of the children was performed in the schools, and included physical examination focused on the cardiovascular system, with cardiac auscultation and blood pressure measurement; anthropometric assessment; and skin folds, waist and hip measurement.
Aneroid blood pressure devices - manometer with scale from - 20 to 300 mmHg, were used for blood pressure measurement. Blood pressure levels were evaluated according to the "Report of the Fourth Task Force on Blood Pressure Control in Children"15.
Anthropometric assessment and measurements of skinfolds and circumferences followed the standards described below:
Weight: a Plena digital scale with 120-kg capacity and accuracy to 100 grams was used. The individuals were weighted without shoes and wearing as little clothes as possible. They should be still and have their feet centered on the scale platform.
Height: a metallic non-stretchable tape measure fixed to a plane surface and a set-square were used. The individuals should be have their heels, buttocks, back and head touching the wall, or as close to it as possible, and look straight forward. Height was measured at the end of inspiration.
Skinfolds: the folds were measured on the right side of the body. The mean value between three measurements was considered. The anatomical points were selected as follows: the triceps skinfold was measured halfway between the acromion and olecranon; the subscapular skinfold was measured two centimeters below the lower scapular border; and the abdominal skinfold was measured two centimeters lateral to the umbilicus.
Circumferences: waist circumference (WC) was measured at the mid-point between the last rib border and the iliac crest; hip circumference (HC) was measured at the largest point of the of the gluteal region.
Calculation of the body mass index (BMI): obtained by the ratio body mass to square height, expressed in kg/m2. The cut-off points for overweight (percentile > 85) and obesity (percentile > 97) were used for BMI values based on the WHO criteria16.
Statistical analysis: the analysis was carried out using the Statistical Package for the Social Sciences (SPSS) version 11.0 software program. Prevalences were described as proportions with respective 95% confidence intervals (CI). Continuous variables were described as means and standard deviations or medians and interquartile intervals. Differences between the groups with or without excess weight were assessed using the Student's t test or Mann Whitney test for continuous variables, and the chi square test or Fisher's exact test for categorical variables. Analysis of variance (ANOVA) was used for the variable BMI categorized in 3 groups (normal, obesity, and overweight). Pearson's correlation was used to analyze correlations. Poisson regression and correction were used for clusters. For all comparisons, the significance level was set at 5%.
Results
A total of 511 adolescents were studied in six schools. Their mean age was 12.57 years, and 55.2% (n = 282) were females. Table 1 shows the overall sample characteristics. The proportion of families with less than eight year of education was 47% for fathers and 52.4% for mothers.
Table 1.
Overall characteristics of the study population
| Variables | n (%) | |
|---|---|---|
| Schoolchildren | 511 (100) | |
| Male | 229 (44.8) | |
| Age up to13 years | 377 (73.8) | |
| > 14 years | 134 (26.2) | |
| Father's level of education | ||
| Incomplete elementary school | 240 (56.1) | |
| Incomplete highschool | 113 (26.4) | |
| Complete highschool or higher | 75 (17.5) | |
| Mother's level of education | ||
| Incomplete elementary school | 268 (57.5) | |
| Incomplete highschool | 127 (27.3) | |
| Complete highschool or higher | 71 (15.2) | |
| Number of siblings | ||
| Only child | 62 (12.7) | |
| With siblings | 425 (87.3) | |
| Obese 1st degree family member | 62 (12.7) | |
| Dyslipidemic 1st degree relative | 86 (16.8) | |
| Diabetic 1st degree relative | 34 (6.7) | |
| Hypertensive 1st degree relative | 143 (28) | |
| Heart disease/ischemia in 1st degree relative | 7(1.4) | |
| Smoker at home | 264 (54.2) | |
In relation to the history of cardiovascular risk factors in first-degree family members, the following percentages were observed: 28% hypertension; 12.6% obesity; 16.8% dyslipidemia; 6.7% diabetes; and 1.4% cardiovascular disease or ischemia. In relation to the mean number of family members with risk factors, 1.6 were obese; 1.6 hypertensive; 1.3 dyslipidemic; 1.3 diabetics; and 1.3 had already had a vascular or cardiac event. The mean BMI of parents was 26.5 ± 4.0 kg/m2 for fathers and 25.7 ± 5.8 kg/m2 for mothers.
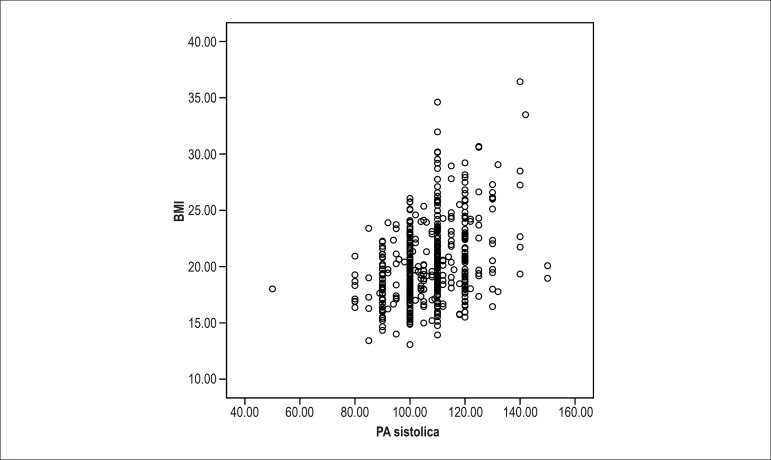
The prevalence of excess weight (BMI ≥ 85th percentile) among the schoolchildren was 27.6% (141 students, 95% CI: 23.9 - 31.6), of which 17.8% (91 students, 95% CI: 14.7 - 21.4) with overweight (BMI > 85th percentile) and 9.8% (50 students, 95% CI: 7.5 - 12.7) with obesity (BMI > 97th percentile). Overweight was more prevalent among females (19.9%), and obesity, among males (11.8%), as shown in Table 2. BMI classification and blood pressure levels are described in Table 3. Systolic blood pressure scattering in relation to BMI is shown in Figure 1.
Table 2.
Distribution of schoolchildren with excess weight according to gender
| Schoolchildren | Excess weight | Overweight | Obesity | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | CI* | N | % | CI* | N | % | CI* | |
| Male gender | 62 | 27.1 | 21.7-33.2 | 35 | 15.3 | 11.2-20.5 | 27 | 11.8 | 8.2-16.6 |
| Female gender | 79 | 28.0 | 23.1-33.5 | 56 | 19.9 | 15.6-24.9 | 23 | 8.2 | 5.5-11.9 |
| Total | 141 | 27.6 | 23.9-31.6 | 91 | 17.8 | 14.7-21.4 | 50 | 9.8 | 7.5-12.7 |
95% Confidence Interval
Table 3.
Classification of BMI percentile and blood pressure levels
| Proportion (n) | 95% CI | |
|---|---|---|
| BMI percentile by gender and age | ||
| Well-nourished | 0.758(318) | 0.713 - 0.802 |
| Overweight | 0.192 (153) | 0.151 - 0.232 |
| Obesity | 0.050 (40) | 0.030 - 0.070 |
| Blood pressure levels classification | ||
| Normal | 0.725(295) | 0.625 - 0.824 |
| Borderline | 0.162 (129) | 0.102 - 0.221 |
| Stage I SH | 0.084 (67) | 0.055 - 0.112 |
| Stage II SH | 0.029 (23) | 0.003 - 0.053 |
BMI: Body mass index; SH: Systemic hypertension
Figure 1.
Scatter-plot with relationship between systolic blood pressure levels and BMI.
Blood pressure levels were abnormal in 11.3% of the sample and borderline in 16.2%.
All anthropometric variables showed a direct and significant correlation with systolic (SBP) and diastolic blood pressure (DBP) levels (Table 4). Among the measurements analyzed, HC showed the strongest correlation with increased blood pressure levels (r = 0.462, p < 0.001), followed by WC (r = 0.404, p < 0.001) and abdominal skinfold (r = 0.291, p < 0.001).
Table 4.
Correlation between blood pressure levels and anthropometric variables
| Variable | r | p |
|---|---|---|
| BMI | 0.384 | <0.001 |
| Mother's BMI | 0.171 | <0.001 |
| Lowest waist circumference | 0.404 | <0.001 |
| Hip diameter | 0.462 | <0.001 |
| Abdominal skin fold | 0.291 | <0.001 |
| Sum of skinfolds | 0.293 | <0.001 |
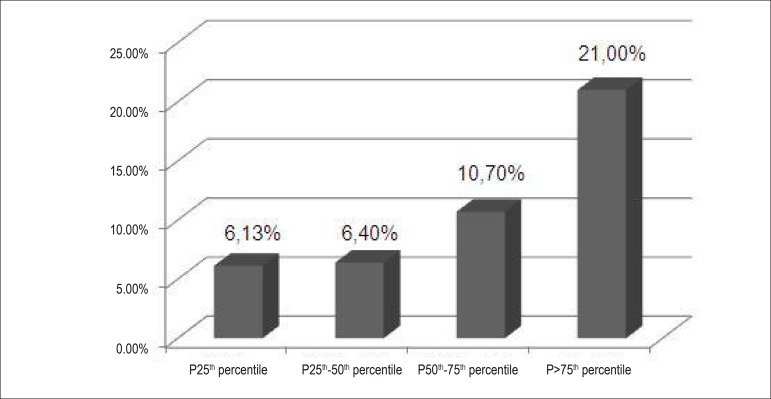
The mean WC was 74.54 ± 9.64 cm. WC percentiles were calculated for the sample, with values of 68 cm, 73 cm and 80 cm corresponding to the 25th, 50th, and 75th percentiles, respectively. Among individuals with measurements lower than the 25th percentile, 6.13% had abnormal blood pressure levels; this proportion increased to 6.4% for individuals between the 25-50th percentiles; to 10.7% for individuals between the 50 75th percentiles; and to 21% when the measurements were higher than the 75th percentile (p < 0.001) (Figure 2).
Figure 2.
Comparison between abdominal circumference percentiles.
The sum of the triceps and subscapular skinfolds (SF), according to the Lohman's nanogram was considered low in 9.1%; adequate in 41.9%; and high in 49% of the schoolchildren. In the first group, 19.4% had abnormal blood pressure levels, increasing to 20.9% and 34.5% in the other groups, respectively (p < 0.001). The percentage of individuals engaged in 2 or 3 physical activities per day was 74.7% in group low SF, 66.4% in group adequate SF, and 61.1% in group high SF (p < 0.001). Mothers' BMI (r = 0.171, p < 0.001) was also observed to be positively correlated to the presence of higher blood pressure levels.
Discussion
In this population-based study in schoolchildren of Porto Alegre, a high percentage of excess weight and abnormal blood pressure levels were observed.
According to the WHO's data, approximately 29% of deaths worldwide result from diseases of the circulatory system, such as coronary artery disease and cerebrovascular disease17. Approximately 80% of cardiovascular deaths in the world occur in developing countries18.
Previously, the cardiovascular risk factors were only known for the adult population. Sedentary lifestyle, sodium-rich diet and psychosocial factors such as stress are among the factors more extensively studied19. Among adolescents, this relationship has been recently demonstrated20. However, better knowledge of the relationship between obesity, as assessed by BMI, and health risks for the pediatric population is still necessary21.
In our study, we observed prevalences of 17.8% overweight, 9.8% obesity and 27.6% excess weight. These findings are similar to those of The Bogalusa Heart Study, in which, in a sample of 2597 schoolchildren aged between 5 and 18 years, a prevalence of 33% of overweight was observed21. In the present study, overweight was more prevalent among females (19.9%), and obesity, among males (11.8%). These data corroborate Ribeiro et al22 findings in the "The Three Cities Heart Study", a cross-sectional trial assessing 3,179 students aged between 6 and 18 years in three large Brazilian cities, where the prevalence of overweight, excess weight and obesity was 10%, 15% and 5%, respectively22. Likewise, Pinto et al3 evaluated 1131 individuals from 7 to 14 years of age and found 12.6% of overweight/obesity. Guimarães et al23, in turn, reported a prevalence of overweight of 36.9% and obesity of 23.5% in a schoolchildren sample aged between 11 and 18 years from public and private schools in Bahia. This fact consolidates that the prevalence of excess weight is increasing in Brazil and, apparently, is distributed in a similar fashion in the different regions of the country, thus making it necessary that programs for obesity prevention in the pediatric population are created.
We found 11.3% of the sample with abnormal blood pressure levels and 16.2% with borderline values, results which are similar to those of a study recently conducted in three large Brazilian cities that found a 12% prevalence of individuals with increased blood pressure levels22, like in other Brazilian studies3,23,24. Li et al25 found 16.2% of increased blood pressure levels in a sample of 1005 children and adolescents in China. On the other hand, a study conducted in Fortaleza (State of Ceará, Brazil), in a sample of 342 schoolchildren aged between 6 and 18 years, found a frequency of 44.7% of the sample with increased blood pressure26, and a study of 1239 Mexican children showed a 22.8% prevalence of hypertension27.
All anthropometric variables studies showed significant correlations, and this was also observed in Araújo et al26 study in schoolchildren in Maceió. Katzmarzyk et al21 advocate the clinical use of BMI and WC for the prediction of the increase in risk factors among children and adolescents. Choy et al13 believe that WC per se may be used as a predictor of increased blood pressure levels in prepubertal children and recommend the use of this variable together with BMI, thus increasing its power to predict SH.
In a sample of 1190 Australian schoolchildren, Gopinath et al12 demonstrated that WC was closely associated with DBP and SBP levels in both genders. According to the NIH guidelines for adults, WC higher than 102 for men and 88 for women are considered abdominal obesity and may be related to metabolic disorders in comparison to individuals with lower measurements7.
However, studies have demonstrated that these cut-off values are useful for the prediction of metabolic risks in adults28,29, but currently there is no guideline for the classification of overweight and health risks among children and adolescents using WC.
In the present study, HC showed the strongest direct correlation with blood pressure levels, followed by WC. Katzmarzyk et al21 advocate that WC may be used and is efficient for the clinical assessment of the presence or absence of increased cardiovascular risk factors in children and adolescents. This association was also demonstrated by other authors, pointing out the risk for cardiovascular diseases in children30,31. In a sample of schoolchildren aged between 10 and 14 years in Chipre, Savva et al32 reported that children with increased WC had significantly higher chances of developing increased blood pressure levels in relation to those with adequate WC32. An Italian study of children aged between 3 and 11 years demonstrated that children with increased WC have multiple risk factors for cardiovascular diseases in comparison with children with lower values32.
In this study, the mean WC was 74.54 ± 9.64 cm. When WC percentiles were calculated, we found that among individuals with measurements lower than the 25th percentile, 6.13% showed abnormal blood pressure levels. This proportion increased to 6.4% for individuals between the 25th and 50th percentiles; to 10.7% for those between the 50th and 75th percentiles; and to 21% for individuals with WC higher than the 75th percentile (p < 0.001). A study conducted in the State of Bahia with a sample of 536 schoolchildren aged between 11 and 18 years found 51.7% of the sample above the 75th percentile for WC23.
Ribeiro et al22 described that students with excess weight showed a 3.25 (2.38 - 4.45) higher chance of having elevated SBP and a 1.93 (1.36-2.75) higher chance of elevated DBP. Additionally, the authors reported that those enrolled in public schools had a 2.48 (1.75 - 3.54) higher chance of having elevated SBP in comparison to those in private schools22.
In a recent study, Ribeiro et al22 reported that schoolchildren deemed "less active than others" had a 2.36 (1.98 - 2.82) higher chance of having higher SSF in relation to students considered physically active, in addition to presenting a 1.97 (1.65-2.35) higher chance of having increased suprailiac skinfold thickness, and a 2.34 (1.92-2.85) higher chance of having increased sum of the skinfolds22. Mother's BMI was also observed to be positively correlated with the presence of higher blood pressure levels. This probably reflects the strong relationship between the child's and mother's BMI, and is possibly associated with environmental and genetic factors.
Some limitations of this study are worthy of consideration. Because it is a cross-sectional study, it was not possible to have a second view on the students assessed. Also, the questionnaires used in the research were not validated and blood pressure was measured at one single moment. Therefore, the values can only be used as a reference and not as diagnosis of SH. We should also point out that there is no single reference value internationally accepted for WC in children; however, several suggestions exist for isolated populations.
Nevertheless, our findings are important to emphasize the need for an early diagnosis of these alterations and the designing of proper preventive measures in the future.
Conclusion
We observed an association of WC and skinfolds with increased blood pressure levels in the schoolchildren of our sample. Considering the progressive increase in the prevalence of hypertension and obesity, which can start early in childhood, it is of the utmost importance that measurement of blood pressure and waist and hip circumferences be implemented in the routine assessment in health services. Thus, the early detection of risk factors will allow primary prevention strategies to be adopted.
Footnotes
Author contributions
Conception and design of the research: Schommer VA, Barbiero SM, Pellanda LC; Acquisition of data: Barbiero SM, Cesa CC, Oliveira R, Silva AD, Pellanda LC; Analysis and interpretation of the data: Schommer VA, Silva AD, Pellanda LC; Statistical analysis: Pellanda LC; Writing of the manuscript: Schommer VA; Critical revision of the manuscript for intellectual content: Barbiero SM, Cesa CC, Oliveira R, Pellanda LC.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
This study was funded by FAPICC.
Study Association
This article is part of the Master's Degree dissertation submitted by Sandra Mari Barbiero at Instituto de Cardiologia / Fundação Universitária de Cardiologia and Completion of coursework submitted by Vanya Ames Schommer, at Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA).
References
- 1.World Health Organization (WHO) World Health Report 2002: reducing risks, promoting healthy life. Geneva: 2002. [DOI] [PubMed] [Google Scholar]
- 2.Sociedade Brasileira de Cardiologia. Sociedade Brasileira de Hipertensão. Sociedade Brasileira de Nefrologia VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol. 2010;95(1) supl.1:1–51. [PubMed] [Google Scholar]
- 3.Pinto SL, Silva RC, Priore SE, Assis AM, Pinto EJ. Prevalência de pré-hipertensão e de hipertensão arterial e avaliação de fatores associados em crianças e adolescentes de escolas públicas de Salvador, Bahia, Brasil. Cad Saúde Pública. 2011;27(6):1065–1076. doi: 10.1590/s0102-311x2011000600004. [DOI] [PubMed] [Google Scholar]
- 4.Salgado CM, Carvalhes JT. Hipertensão arterial na infância. J Pediatr (Rio J) 2003;79(supl.1):S115–S124. doi: 10.2223/jped.1006. [DOI] [PubMed] [Google Scholar]
- 5.Barbiero SM, Pellanda LC, Cesa CC, Campagnolo P, Beltrami F, Abrantes CC. Overweight, obesity and other risk factors for IHD in Brazilian schoolchildren. Public Health Nutr. 2009;12(5):710–715. doi: 10.1017/S1368980008003200. [DOI] [PubMed] [Google Scholar]
- 6.Duncan BB, Schmidt MI, Giugliani ER, editors. Medicina ambulatorial: condutas de atenção primária baseadas em evidências. 3ª ed. Porto Alegre: Artmed; 2004. [Google Scholar]
- 7.National Institutes of Health (NIH) Clinical guidelines for the identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, MD: 1998. [PubMed] [Google Scholar]
- 8.Pouliot MC, Després JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73(7):460–468. doi: 10.1016/0002-9149(94)90676-9. [DOI] [PubMed] [Google Scholar]
- 9.Rankinen T, Kim SY, Perusse L, Despres JP, Bouchard C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int J Obes Relat Metab Disord. 1999;23(8):801–809. doi: 10.1038/sj.ijo.0800929. [DOI] [PubMed] [Google Scholar]
- 10.Rexrode KM, Buring JE, Manson JE. Abdominal and total adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord. 2001;25(7):1047–1056. doi: 10.1038/sj.ijo.0801615. [DOI] [PubMed] [Google Scholar]
- 11.Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong CP, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med. 2000;160(14):2117–2128. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 12.Gopinath B, Baur LA, Garnett S, Pfund N, Burlutsky G, Mitchell P. Body mass index and waist circumference are associated with blood pressure in preschool-aged children. Ann Epidemiol. 2011;21(5):351–357. doi: 10.1016/j.annepidem.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Choy SC, Chan WY, Chen TL, Shih CC, Wu LC, Liao CC. Waist circumference and risk of elevated blood pressure in children: a cross-sectional study. BMC Public Health. 2011;11:613–613. doi: 10.1186/1471-2458-11-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreno LA, Pineda I, Rodriguez G, Fleta J, Sarría A, Bueno M. Waist circumference for the screening of metabolic syndrome in children. ActaPaediatr. 2002;91(12):1307–1312. doi: 10.1080/08035250216112. [DOI] [PubMed] [Google Scholar]
- 15.Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pt 1Pediatrics. 1996;98(4):649–658. [PubMed] [Google Scholar]
- 16.World Health Organization (WHO) Diet, nutrition, and the prevention of chronic diseases. Geneva: 2003. [PubMed] [Google Scholar]
- 17.National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992;89(3):495–501. [PubMed] [Google Scholar]
- 18.World Health Organization (WHO) The world health report. Life in the 21st century: a vision for all. Geneva: 1998. [Google Scholar]
- 19.Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, et al. American Heart Association Atherosclerosis. Hypertension, and Obesity in Youth Committee Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52(3):433–451. doi: 10.1161/HYPERTENSIONAHA.108.190329. [DOI] [PubMed] [Google Scholar]
- 20.Katzmarzyk PT, Tremblay A, Perusse L, Despres JP, Bouchard C. The utility of the international child and adolescent overweight guidelines for predicting coronary heart disease risk factors. J Clin Epidemiol. 2003;56(5):456–462. doi: 10.1016/s0895-4356(02)00595-4. [DOI] [PubMed] [Google Scholar]
- 21.Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, Berenson GS. Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics. 2004;114(2):e198–e205. doi: 10.1542/peds.114.2.e198. [DOI] [PubMed] [Google Scholar]
- 22.Ribeiro RC, Coutinho M, Bramorski MA, Giuliano IC, Pavam J. Association of the waist-to-height ratio with cardiovascular risk factors in children and adolescents: the Three Cities Heart study. Int J Prev Med. 2010;1(1):39–49. [PMC free article] [PubMed] [Google Scholar]
- 23.Guimarães IC, de Almeida AM, Santos AS, Barbosa DBV, Guimarães AC. Blood pressure: effect of body mass index and of waist circumference on adolescents. Arq Bras Cardiol. 2008;90(6):393–399. [Google Scholar]
- 24.Rosa ML, Mesquita ET, da Rocha ER, Fonseca Vde M. Índice de massa corporal e circunferência da cintura como marcadores de hipertensão arterial em adolescentes. Arq Bras Cardiol. 2007;88(5):573–578. doi: 10.1590/s0066-782x2007000500012. [DOI] [PubMed] [Google Scholar]
- 25.Li L, Wang Y, Cao W, Xu F, Cao J. Longitudinal studies of blood pressure in children. Asia Pac J Public Health. 1995;8(2):130–133. doi: 10.1177/101053959500800213. [DOI] [PubMed] [Google Scholar]
- 26.de Araújo TL, Lopes MV, Cavalcante TF, Guedes NG, Moreira RP, Chaves ES, et al. Análise de indicadores de risco para hipertensão arterial em crianças e adolescentes. Rev Esc Enferm USP. 2008;42(1):120–126. doi: 10.1590/s0080-62342008000100016. [DOI] [PubMed] [Google Scholar]
- 27.Colín-Ramírez E, Castillo-Martínez L, Orea-Tejeda A, Villa Romero AR, Vergara Castañeda A, Asensio Lafuente E. Waist circumference and fat intake are associated with high blood pressure in Mexican children aged 8 to 10 years. J Am Diet Assoc. 2009;109(6):996–1003. doi: 10.1016/j.jada.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 28.Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162(18):2074–2079. doi: 10.1001/archinte.162.18.2074. [DOI] [PubMed] [Google Scholar]
- 29.Ardern CI, Katzmarzyk PT, Janssen I, Ross R. Discrimination of health risk by combined body mass index and waist circumference. Obes Res. 2003;11(1):135–142. doi: 10.1038/oby.2003.22. Erratum in Obes Res. 2003;11(3):491. [DOI] [PubMed] [Google Scholar]
- 30.Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart Study. Am J Clin Nutr. 1999;69(2):308–317. doi: 10.1093/ajcn/69.2.308. [DOI] [PubMed] [Google Scholar]
- 31.Maffeis C, Pietrobelli A, Grezzani A, Provera S, Tato L. Waist circumference and cardiovascular risk factors in prepubertal children. Obes Res. 2001;9(3):179–187. doi: 10.1038/oby.2001.19. [DOI] [PubMed] [Google Scholar]
- 32.Savva SC, Tornaritis M, Savva ME, Kourides Y, Panagi A, Silikiotou N, et al. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int J Obes Relat Metab Disord. 2000;24(11):1453–1458. doi: 10.1038/sj.ijo.0801401. [DOI] [PubMed] [Google Scholar]