Abstract
Objectives
A thorough examination of the relationship of asthma severity and control with symptoms of depression is needed to identify groups of asthmatics at high risk for poor disease control outcomes. This study examines the relationship of symptoms of depression with severity and control in a well characterized cohort of asthmatics and healthy controls.
Methods
Depressive symptoms and quality of life were assessed using the Beck Depression Inventory. Disease control was measured by a composite index incorporating symptoms, activity limitation, and rescue medication use.
Results
Individuals with asthma (n=91) reported more symptoms of depression than controls (n=36; p<0.001). Those with Severe asthma (n=49) reported more symptoms of depression (p=0.002) and poorer asthma control (p<0.0001) than those with Not Severe asthma. Worse asthma control was associated with more depressive symptoms in Severe (r=0.46, p=0.002) but not in Not Severe (r=0.13, p=0.40) asthmatics. The relationship of symptoms of depression among Severe asthmatics was attenuated by disease control. Exploratory analyses identified specific disease symptom characteristics, as opposed to exacerbations, as associated with symptoms of depression.
Conclusions
Among individuals with severe asthma, increased symptom burden is positively associated with risk for co-morbid depression. These findings point to a need for regular mood disorder screenings and treatment referrals among this group. Further research is warranted to examine whether treatment of comorbid depression improves treatment adherence and asthma-related quality of life.
Keywords: severe asthma, depression, asthma control
INTRODUCTION
Although asthma has long been associated with symptoms of depression, the relationship between these two complex diseases remains unclear (1). When compared to the general population, individuals with asthma are at increased risk for depressive symptoms, including decreased ability to perform daily activities, agitation and even suicide (2–6). Depressive symptoms have also been associated with greater asthma symptoms, functional limitations, healthcare utilization, worse asthma quality of life (QOL) as well as decreased medication and treatment adherence (3, 4, 7–15). However, relationships between depression and asthma severity and control across a wide range of well characterized asthma patients remains poorly understood.
Asthma severity and control have recently been defined and, to some degree, separated (16–18). Severity generally defines an underlying feature of the disease that contributes to level of difficulty achieving symptom relief and normal lung function. Guidelines suggest that “asthma control” can be assessed by symptom frequency and intensity, rescue medication use and number of exacerbations, with or without the addition of lung function changes. In general, increasing asthma severity implies more poorly controlled asthma, although severe asthma definitions allow inclusion of patients on high doses of inhaled and oral corticosteroids (CSs) who are well controlled by National Asthma Education and Prevention Program (NAEPP), Global Initiative for Asthma (GINA) guidelines and ATS Refractory Asthma definitions (17–19).
Many individuals with asthma remain poorly controlled despite advances in treatment. Growing evidence suggests that poor disease control, as compared to disease severity, plays a greater contribution to symptoms of depression (8, 14, 20–23). However, no studies have included a large enough proportion of well-characterized severe asthma patients to fully understand the overlapping associations of asthma severity and control in the prediction of emotional function. Additionally, little is known about the impact of particular elements of disease control (e.g., symptoms, exacerbation) and their relationship to depression (24). Understanding these relationships could lead to improvements in clinical care (15, 25).
In the current study, we examined associations between asthma severity and disease control and symptoms of depression among individuals with well-characterized asthma who were recruited as part of the National Heart Lung and Blood Institute’s Severe Asthma Research Program (SARP). We hypothesized that: 1) depression would be significantly worse among severe asthmatics as compared to those with less severe asthma, and 2) lower levels of asthma control would explain the greater degree of depressive symptoms in severe asthma.
METHODS
Participants
Individuals were recruited from the larger parent multicenter SARP network in a sub-study conducted at the University of Pittsburgh (and earlier at National Jewish Health) site. Participants were ≥18 years of age, non-smokers for the past year with < 5 pack/year history of tobacco use, and either met the American Thoracic Society (ATS) criteria for a diagnosis of asthma or were healthy controls (26). Severe asthma was defined by the ATS Refractory Asthma Definition, including use of high dose inhaled CSs or oral CSs for >50% of the previous year as major criteria. Participants on these medications could be identified as severe asthmatics if they either required these medications to achieve a level of symptom, exacerbation and lung function control or if they did not achieve control despite these medications. “Not severe” asthmatics included all other individuals with asthma without regard to level of control (26). Normal Control participants were healthy atopic or non-atopic individuals with normal lung function and without a history of chronic respiratory conditions. Participants with asthma were recruited using flyers and public postings within the hospital and university clinic settings; they were not recruited following any specific health or asthma exacerbation events. Control participants were recruited using the same procedures including flyers and public postings within the hospital and clinic settings. The inclusion criteria and study procedures have been described in detail in a prior publication (26).
All participants gave informed consent, which was approved by the Institutional Review Boards of both the University of Pittsburgh, PA and the National Jewish Medical and Research Center (National Jewish Health) Denver, CO.
Measures
Participants underwent clinical testing and provided questionnaire data as previously described (26). Basic demographics, years of education, body mass index (BMI), pulmonary function testing and years since asthma onset were included.
Measure of Depression
Symptoms of depression were assessed using the Beck Depression Inventory (BDI-II), which includes 21 items that assess affective symptoms (e.g., sadness, irritability, and hopelessness), cognitive symptoms (e.g., guilt or feelings of being punished), and somatic symptoms (e.g., fatigue, sleep disruption, and weight change) of depression (27, 28). Each item assesses symptom severity on a scale of 0–3. Total scores on this measure range from 0 to 63, with scores of 16 or higher associated with clinical depression (27, 28). In addition to the full scale measure, we constructed a modified 17-item BDI (mBDI) excluding items that assess somatic symptoms that may also reflect symptoms associated with asthma morbidity (items 14–21, e.g., agitation, sleep disturbance) (29–31). The total scores on the modified scale ranged from 0 to 51, with a higher score reflecting greater depressive symptomatology. This modified BDI-II was used in sensitivity analyses to confirm that results from the original BDI were not being driven by asthma-related morbidity. The BDI was analyzed both as a continuous measure of depressive symptoms as well as a categorical variable examining BDI-II scores > or < 16, an accepted cut-off to screen for clinical depression (27, 32).
Asthma Control Index
While validated and accepted measures of disease control now exist (e.g., Asthma Control Test (ACT); Asthma Control Questionnaire (ACQ)), none were used in the original SARP dataset (34, 35). Thus, for this study, we developed a measure of asthma control modeled on the National Asthma Education Prevention Program (NAEPP) guidelines using data collected in SARP (17). A composite index was developed to assess asthma control in the past 2 weeks to 3 months using factors consistent with standardized measures of control in the NAEPP Guidelines (17). This composite measure included:
nocturnal awakenings (previous 3 months): 1 (never) to 6 (2 or more times a night)
shortness of breath (previous 3 months): 1 (never) to 6 (2 or more times a day)
chest tightness (previous 3 months): 1 (never) to 6 (2 or more times a day)
wheeze (previous 3 months):1 (never) to 6 (2 or more times a day)
interferes with daily activity (previous 2 weeks, as measured by the AQLQ activity domain. This score was reverse coded within the Asthma Control Index only, to be consistent with direction of association of the other continuous measures):1(least activity limitation) to 7 (most disrupted) [33]
short-acting metered dose inhaler and nebulized beta-agonist use (previous 3 months, retrieved from medication use questionnaire): 1 (never) to 6 (2 or more times a day).
A continuous score adding each patient’s asthma control characteristics was developed ranging from 7 to 43, with higher values representing worse disease control. The results were reported as a continuous scale, without cut-points for well, not-well or poorly controlled asthma.
Statistical Analysis
We first compared demographic variables and clinical measures between participants with asthma and controls and second, between participants with severe asthma and non-severe asthma. Continuous variables were compared using two-sample t-tests. Categorical variables were compared using Chi-squared tests or Fisher’s exact test. All tests were two tailed and conducted at α=0.05. We calculated Spearman’s correlation statistics to assess the strength of linear associations among depression and disease control. We used general linear regression models to compare mean BDI-II between participants with severe and mild asthma. We compared crude unadjusted models to models controlling for key covariates of gender, age, BMI, education, race, FEV1, and length of disease by age of onset.
To assess the possibility that asthma control contributes to the association between asthma severity and depression, we examined the magnitude, direction and significance of the primary model estimates after adjusting for asthma control. Logistic regression was used to assess differences in the proportion of individuals with BDI-II > or < 16, the cut-off for clinical depression. Here, we present crude and adjusted odds ratios and 95% CIs analogous to the general linear model results. All analyses were conducted using SAS software version 9.2; SAS Institute. Cary, NC. Exploratory analyses compared specific elements of disease control (e.g., nocturnal awakenings, asthma symptoms [wheeze, shortness of breath and chest tightness and interference with activity, metered-dose and nebulized beta-agonist use]) and exacerbation-related factors (e.g., emergency room visit and hospitalization) among individuals above and below the clinical cut off on the BDI-ll. Chi -square tests (two-sided Fisher’s exact test) were used for these analyses. In addition, Spearman’s correlation statistics were used to assess the linear association of the continuous BDI-II score with the various categorical measures of disease control.
RESULTS
Demographics
Compared to normal controls (n=36), individuals with asthma (n=91) were older (p<0.0001) and had higher body mass index (p=0.0007) (Table 1). Individuals with severe asthma were older than those with milder disease (p<0.0001), but did not differ by race, ethnicity, gender or BMI compared to individuals with milder disease. About 80% of patients with severe asthma were on oral CSs for > 50 % of the previous year compared to none in the not severe asthma group (p<0.0001).
TABLE 1.
Demographics and Sample Descriptive, (1) Asthma Compared with Normal Control and (2) Severe with Not severe Asthma Severity.
| Normal Controls (n=36) | Asthma (n=91) | Normal controls vs. Asthma (p-value) | Not severe (n=42) | Severe asthma (n=49) | Not severe vs. Severe Asthma (p-value) | |
|---|---|---|---|---|---|---|
|
| ||||||
| Age, mean (SD) | 29.74 (9.64) | 39.09 (13.68) | <.0001 | 31.83 (11.32) | 45.32 (12.48) | <.0001 |
|
| ||||||
| Female (%) | 18 (50.00) | 62 (68.13) | 0.07 | 29 (69.05) | 33 (67.35) | 0.86 |
|
| ||||||
| Ethnicity (%) | ||||||
| Hispanic/Latino | 2 (5.56) | 3 (3.30) | 2 (4.76) | 1 (2.04) | ||
| Not Hispanic/Latino | 34 (94.44) | 88 (96.70) | 0.62 | 40 (95.24) | 48 (97.96) | 0.59 |
|
| ||||||
| Race (%) | ||||||
| White | 29 (80.56) | 67 (73.63) | 28 (66.67) | 39 (79.59) | 0.24 | |
| Black | 3 (8.33) | 14 (15.38) | 0.63 | 7 (16.67) | 7 (14.29) | |
| Other | 4 (11.11) | 10 (10.99) | 7 (16.67) | 3 (6.12) | ||
|
| ||||||
| BMI, mean (SD) | 25.51 (4.54) | 29.14 (6.75) | 0.0007 | 28.51 (6.98) | 29.69 (6.57) | 0.41 |
|
| ||||||
| Education, (%) | ||||||
| <College | 1 (3.23) | 15 (16.67) | 4 (9.52) | 11 (22.92) | 0.10 | |
| ≥College | 30 (96.77) | 70 (77.78) | 0.05 | 37 (88.10) | 33 (68.75) | |
| Other | 0 | 5 (5.56) | 1 (2.38) | 4 (8.33) | ||
|
| ||||||
| Baseline FEV1 (mean (SD)) | 99.25 (8.87) | 70.99 (24.50) | <.0001 | 86.83 (17.03) | 57.41 (21.67) | <.0001 |
|
| ||||||
| Disease Control (mean (SD)) | N/A | N/A | N/A | 17.24 (5.70) | 28.05 (8.87) | <.0001 |
|
| ||||||
| Asthma Onset (mean (SD)) | N/A | N/A | N/A | 12.67 (12.41) | 19.96 (18.62) | 0.03 |
|
| ||||||
| OCS steroid use (%) | ||||||
| No | N/A | N/A | N/A | 42 (100) | 10 (20.41) | <.0001 |
| Yes | 0 | 39 (79.59) | ||||
Depression and Asthma Control in relation to Asthma Severity
Individuals with asthma reported significantly more symptoms of depression than normal controls on the standard BDI-II (Mean (SD) = 9.45 (9.48) vs. 1.53 (2.86), p<0.0001). The depression score measured by the standard BDI-II was twice as high in Severe (12.29[10.61], mean [SD]) as in Not Severe asthma (6.14[6.69], p =0.002) (Table 2). When somatic items were excluded and the mBDI compared, the differences remained and were marginally greater than the standard BDI-II [Not Severe=3.67(4.38) vs. Severe-8.31(8.37), p=0.001)] (Table 2). Given the modest difference in the outcomes, the validated standard BDI-II results were used for all subsequent analyses. As expected, asthma control differed by asthma severity, with over 50% worse control reported among the Severe asthma participants than the Not Severe participants (Table 1). Symptoms of depression correlated with poor asthma control across all individuals with asthma (0.43 p<0.001). However, when the asthma severity groups were examined separately, significant correlations only existed in those individuals with severe asthma (r=0.46, p=0.002), and not in those with milder disease (r=0.13, p=0.40) (Figure 1).
Table 2.
| Normal Controls (n=36) | Asthma (n=91) | Normal controls vs. Asthma (wilcoxon p-value) | Not severe (n=42) | Severe asthma (n=49) | Not severe vs. Severe Asthma (Wilcoxon p-value) | |
|---|---|---|---|---|---|---|
|
| ||||||
| Standard BDI-II (mean, SD) | 1.53 (2.86) | 9.45 (9.48) | <.0001 | 6.14 (6.69) | 12.29 (10.61) | 0.002 |
| Median | 0 | 7.0 | 4.5 | 9.0 | ||
|
| ||||||
| Modified BDI-II (mBDI) (mean (SD) | 1.03 (2.08) | 6.16 (7.18) | <.0001 | 3.67 (4.38) | 8.31 (8.37) | 0.001 |
| Median | 0 | 4.0 | 2.0 | 5.0 | ||
Figure 1.
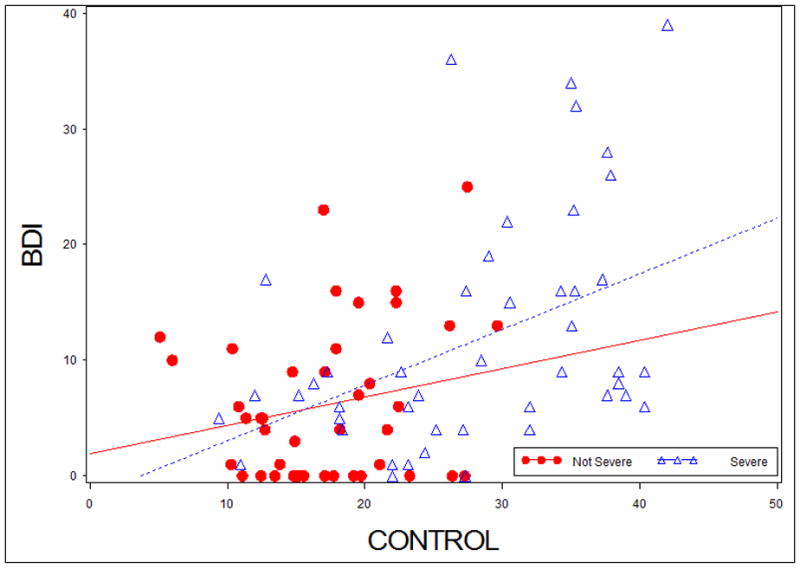
Scatterplot of the Disease Control Measure vs. symptoms of depression (BDI-II) for individuals with asthmaa.
a Not Severe Asthma (r= 0.13, p=0.40) vs. Severe Asthma (r=0.46, p=0.001)
Multivariable Analyses for Factors Associated with Depression
Symptoms of depression were higher among severe compared to milder asthmatics in unadjusted and adjusted analyses that controlled for key covariates (i.e., sex, age, BMI, education and length of disease) (β −7.67, t-statistic −3.47, p=0.0008). There was no significant interaction of severity with asthma control in the prediction of depression (p=.31) However, the difference in BDI scores between severity groups was attenuated and became non-significant when disease control was added to the model (β −2.85, t-statistic −1.15, p= 0.25) (Table 3), consistent with the hypothesis that the relationship between depression and asthma “severity” is related to level of disease control.
Table 3.
Multivariable Regression Analyses for Depression.
| BDI (continuous) Adj Δ (95% CI) p-value | BDI>16 OR (95% CI) | |
|---|---|---|
| ASTHMA (Severe vs. Not Severe) | 6.14 (9.91, 2.37), 0.002 | 4.19 (1.27, 13.86) |
|
ASTHMA (Severe vs. Not Severe) *Adjusted for Significant Covariates (Sex/Gender, Age of onset, Education, BMI, Age) |
7.67 (12.08, 3.28) 0.0008 |
5.00 (1.31, 19.19) |
|
ASTHMA (Severe vs. Not Severe) *Adjusted Covariates *Adjusted for Disease Control |
2.85 (7.78, 2.09), 0.25 | 1.59 (0.31, 8.28) |
More participants in the Severe asthma group fell above the clinical cut-off for depression (BDI-II>16) than those in the Not Severe group (30.61% as compared with 9.52%, χ2 = 6.09, p=0.014). Logistic regression models that controlled for key covariates showed a 5-fold increase in the odds of falling above the clinical cutoff for depression among Severe compared to Not Severe asthmatics (OR = 5.00, 95% CI [1.31, 19.19]). When disease control was added to the model, this relationship was also no longer significant (1.59 [0.31, 8.28]) (Table 3).
Exploratory analyses examining components of disease control in relation to symptoms of depression
Our composite measure of recent disease control included assessments of nocturnal awakenings, asthma symptoms (e.g., wheeze, shortness of breath and chest tightness), interference with activity, and short acting beta-agonist use. In addition, we had data on systemic CS use, emergency room (ER) visits as well as hospitalizations in the previous year. To better understand the relationship between disease control and depression among severe asthmatics, specific elements of the disease control index, as well as exacerbations and systemic CS use were individually analyzed in relation to symptoms of depression. In exploratory analyses, symptoms of depression correlated positively with activity limitation (rs=−0.52, p <0.0001), nighttime awakenings (rs=0.43, p<0.002), shortness of breath (rs=0.37, p=0.009), chest tightness (rs=0.38, p=0.007) and short-acting β-agonist use (rs=0.39, p=0.006). There was no correlation with wheeze (rs=0.097, p=0.50). When compared to individuals with severe asthma who fell below the cut off for clinically significant depression, those above the cut off reported more nocturnal awakenings (BDI-II <16: 3.5 [2,5] vs. ≥ 16: 5[5,6], p=0.007), shortness of breath (< 16: 4.5[3,6] vs. ≥ 16: 6[5,6], p=0.027), chest tightness (<16: 4[2,5] vs. ≥16: 5[5,6], p=0.027) and activity limitation (lower score is worse) (<16: 4.2 [3.6–4.8] vs. ≥16: 3.0 [2.6,4.0], p=0.005). The groups did not differ in Wheeze (<16: 5[2, 6] vs. ≥16: 4[3, 6], p=0.592), β-agonist use (<16: 2[1,6] vs. ≥16: 4[2,5], p=0.290), ER visits (χ2=0.183, p=0.67), hospitalizations in the last 12 months (χ2=2.42, p=0.119), and need for 3 or more OCS (χ2=0.67, p=0.41).
DISCUSSION
The results from the current study indicate that individuals with a broad range of asthma severity have increased symptoms of depression when compared with matched healthy controls (7, 8, 14, 20, 37, 38). Further, asthmatics meeting the rigid ATS definition of severe asthma had twice the level of depressive symptoms compared to those with milder asthma and were more likely to fall above the pre-defined cut-off for clinical depression even after controlling for key covariates of sex, age, BMI, and asthma duration. The relationship between depression and severity was related to level of asthma control, with better asthma control being associated with less depressive symptomatology among the severe, but not the milder, asthma group. This suggests that asthma severity itself may not be the determinant of the level of depressive symptoms. However, the absence of an association of control with symptoms of depression among individuals with milder asthma suggests that severity and control are tightly interconnected in their relationship with symptoms of depression.
Previous studies examining the association between asthma severity and depression have yielded mixed results with some finding a positive association while others have not (14, 39–42). However, important differences exist between the current study and previous studies which may explain some of the inconsistencies. Our study is the first study to evaluate depression using a standardized instrument in a sample with a broad range of asthma severity and control that was rigorously assessed. We also confirmed that the relationship of asthma severity to depressive symptoms was not a function of shared somatic symptoms. This raises the strong possibility that individuals with severe asthma who also have heightened levels of chronic symptom burden are at increased clinical risk and should be regularly screened and referred for treatment of depression. In sum, our well characterized sample provides further support for an association of asthma severity with symptoms of depression, and suggests that level of disease control may contribute to this association.
Participants in the current study were a local subset of the larger SARP cohort, a well characterized group of asthmatic and healthy control participants in whom severity was rigidly defined by the ATS criteria and in whom poor control was not a specific criterion for severe asthma. While there is conceptual overlap between the definitions of asthma severity and disease control, it is generally acknowledged that recent control can be independent of more longstanding determinations related to asthma severity. Unfortunately, the SARP cohort was initiated before the widespread use of standardized disease control questionnaires. Therefore, we developed a composite index of control incorporating asthma symptoms and medication use from questions asked in SARP and modeled after the NAEPP Guidelines (17). Our control index did not include lung function, which is included in some but not all control questionnaires, as we believed that FEV1 % predicted data would skew the control index to severe asthma. Of note, there were differences in the control criteria recall periods (i.e., ranging from 2 weeks for activity limitation to 3 months for symptoms), which may have impacted the index, with scores likely more reliable over shorter time frames. Despite the limitations of this new control index, there were marked differences in asthma control in individuals with Severe versus Not Severe asthma. When adjusting for asthma control using this index, the differences in depression between Not Severe and Severe Asthma became non-significant.
When the asthma severity groups were examined separately, the association between disease control and depression was only significant for the severe asthma group. This implies that not only is the relationship between depression and asthma severity modified by disease control, but also that the relationship between asthma control and depressive symptoms is modified by asthma severity. These intersecting relationships are maintained even when controlling for key demographic factors. The current study is cross-sectional, which precludes causal interpretations. However, it is conceivable that a “threshold” loss of control or overall burden of disease is required before depressive symptoms increase in relation to control. The substantially and significantly worse asthma control score for those in the Severe Asthma subgroup supports this possibility. Alternatively, the relationship could be stronger in for individuals with severe asthma due to factors not measured in this study, including complexity of medication regimens, lack of response to medications, such as inhaled CSs which are effective in milder asthma and poorly understood participant behaviors which could also influence disease severity. The current findings complement the findings of Lavoie et al. who identified asthmatics who met criteria for depression and then examined their clinical asthma characteristics (20). In this study, asthma severity was not associated with depression; however, asthma control was. The populations examined in the two studies differ in a number of ways. The Lavoie et al. study only recruited individuals with depression whereas the current study included individuals with a range of asthma severity (20). Interestingly, both studies found an inverse association of asthma control with symptoms of depression
To examine the relationship between specific disease control characteristics and clinically significant depression, our exploratory analysis identified only nocturnal awakenings, shortness of breath, chest tightness and limitation of activity as covarying with symptoms of depression. Interestingly, asthma exacerbations (e.g., emergency room visits, hospitalization or OC use) were not associated with symptoms of clinical depression. The most strongly associated control features were activity limitation and nocturnal awakenings. The association with activity limitation is not surprising given its likely impact on overall lifestyle and asthma-related quality of life. Similarly, sleep disturbance, nighttime awakenings and poor sleep quality are common among individuals with both depression and poorly controlled asthma, creating a potential cycle of disruptive sleep disturbance (43–45). Understanding the causal direction of these associations is critical to determining whether interventions to improve sleep (or depression) will improve indices of asthma control. The present study indicates that both disease severity and control contribute to symptoms of depression. Psychological and psychiatric morbidity, such as depression, have been associated with increased asthma severity through biological and psychophysiological mechanisms such as non-adherence with medications and treatment, exposure to asthma triggers, and reduced perception of asthma symptoms (46). Therefore, prospective studies of individuals with severe asthma are needed to better characterize the direction and causal association of the asthma and depressive symptoms.
There are a number of strengths and limitations of the presented work. First, the association between symptoms of depression and asthma severity was observed using both the standard BDI-II and a modified version of the BDI-II that excluded somatic items (such as sleep disturbance and agitation) that accompany both depression and asthma. These results confirm that the positive relationship between asthma severity and symptoms of depression is not solely a function of shared somatic symptoms, but reflects mood disruption. Limitations of this study include the lack of a standardized asthma control questionnaire, reliance on questions with differing recall periods, and the lack of an ability to determine cause verses effect. In addition, the contribution of anxiety to depression was not analyzed in this study as no measure of anxiety was collected in the SARP study (2, 3, 14, 20, 47). Despite these limitations, this study supports a strong relationship of asthma severity with symptoms of depression that was partially accounted for by level of asthma control.
Conclusion
Our findings extend prior research by further examining associations between asthma severity and control and symptoms of depression among a well characterized sample. Individuals with severe asthma endorsed more symptoms of depression than those with milder asthma, with the severe asthmatics who endorsed poor asthma control being at particularly heightened risk. As reported earlier, given that psychological morbidity has been associated with increases in asthma severity, routine screening for depression among patients with severe asthma may result in the opportunity to tailor patient-centered clinical asthma management efforts resulting in improved disease management and control. Exploratory analyses show that activity limitation and nocturnal awakenings show the strongest association with depressive symptoms among those with severe disease and may be useful in the identification of individuals at increased risk for mood disorder. Studies are needed to determine whether interventions designed to improve sleep or increase levels of physical activity can prevent depression, and whether treatment of depression is associated with improved control of asthma or vice versa.
Clinical Implications
Individuals with severe asthma are at increased risk for clinical depression. The current study shows that this is particularly the case for individuals who experience increased asthma symptom burden, including disrupted sleep and limited levels of physical activity. The depression that accompanies severe asthma is not solely a function of shared somatic symptoms and likely reflects mood disruption that may negatively impact treatment adherence and quality of life. The current findings point to a need for regular mood disorder screenings and treatment referrals among severe asthmatics, particularly those with higher symptom burden. The possibility that interventions designed to improve sleep and increase physical activity may result in improved quality of life is also worth consideration.
Acknowledgments
Declaration of Sources of Funding:
Source 1 (SARP): NIH #HL069174
Source 2: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number KL2TR000146.
Abbreviations
- BDI-II
Beck Depression Inventory-II
- mBDI
Modified-Beck Depression Inventory
- BMI
Body Mass Index
- ATS
American Thoracic Society
- SARP
Severe Asthma Research Network
- CS
Corticosteroid
- OCS
Oral Corticosteroid
- NAEPP
National Asthma Education and Prevention Program
- GINA
Global Initiative for Asthma
Footnotes
Declaration of Interest:
The authors report no conflicts of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health Scientific overlap with RR024153
References
- 1.Di Marco F, Santus P, Centanni S. Anxiety and depression in asthma. Current Opinion in Pulmonary Medicine. 2011;17(1):39–44. doi: 10.1097/MCP.0b013e328341005f. [DOI] [PubMed] [Google Scholar]
- 2.Lavoie KL, Bouthillier D, Bacon SL, Lemière C, Martin J, Hamid Q, et al. Psychologic Distress and Maladaptive Coping Styles in Patients With Severe vs Moderate Asthma. CHEST Journal. 2010;137(6):1324–31. doi: 10.1378/chest.09-1979. [DOI] [PubMed] [Google Scholar]
- 3.Lavoie KL, Cartier A, Labrecque M, Bacon SL, Lemière C, Malo J-L, et al. Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respiratory medicine. 2005;99(10):1249–57. doi: 10.1016/j.rmed.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Goldney RD, Ruffin R, Wilson DH, Fisher LJ. Asthma symptoms associated with depression and lower quality of life: a population survey. Medical Journal of Australia. 2003;178(9):437–41. doi: 10.5694/j.1326-5377.2003.tb05408.x. [DOI] [PubMed] [Google Scholar]
- 5.Kuo C-J, Ko Y-C, Chen VC-H, Lee W-C, Chen WJ, Ferri CP, et al. Asthma and suicide mortality in young people: a 12-year follow-up study. The American journal of psychiatry. 2010;167(9):1092–9. doi: 10.1176/appi.ajp.2010.09101455. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin RD, Eaton WW. Asthma, Suicidal Ideation, and Suicide Attempts: Findings From the Baltimore Epidemiologic Catchment Area Follow-Up. American journal of public health. 2005;95(4):717–22. doi: 10.2105/AJPH.2003.019109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cluley S, Cochrane GM. Psychological disorder in asthma is associated with poor control and poor adherence to inhaled steroids. Respiratory medicine. 2001;95(1):37–9. doi: 10.1053/rmed.2000.0968. [DOI] [PubMed] [Google Scholar]
- 8.ten Brinke A, Ouwerkerk ME, Zwinderman AH, Spinhoven P, Bel EH. Psychopathology in Patients with Severe Asthma Is Associated with Increased Health Care Utilization. American Journal of Respiratory and Critical Care Medicine. 2001;163(5):1093–6. doi: 10.1164/ajrccm.163.5.2004020. [DOI] [PubMed] [Google Scholar]
- 9.McCauley E, Katon W, Russo J, Richardson L, Lozano P. Impact of anxiety and depression on functional impairment in adolescents with asthma. General hospital psychiatry. 2007;29(3):214–22. doi: 10.1016/j.genhosppsych.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kullowatz A, Kanniess F, Dahme B, Magnussen H, Ritz T. Association of depression and anxiety with health care use and quality of life in asthma patients. Respiratory medicine. 2007;101(3):638–44. doi: 10.1016/j.rmed.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Black SA, Goodwin JS, Markides KS. The Association Between Chronic Diseases and Depressive Symptomatology in Older Mexican Americans. The Journals of Gerontology. 1998;53A(3):M188–M94. doi: 10.1093/gerona/53a.3.m188. [DOI] [PubMed] [Google Scholar]
- 12.Goodwin RD, Olfson M, Shea S, Lantigua RA, Carrasquilo O, Gameroff MJ, et al. Asthma and mental disorders in primary care. General hospital psychiatry. 2003;25(6):479–83. doi: 10.1016/s0163-8343(03)00071-9. [DOI] [PubMed] [Google Scholar]
- 13.Nascimento I, Nardi AE, Valença AM, Lopes FL, Mezzasalma MA, Nascentes R, et al. Psychiatric disorders in asthmatic outpatients. Psychiatry research. 2002;110(1):73–80. doi: 10.1016/s0165-1781(02)00029-x. [DOI] [PubMed] [Google Scholar]
- 14.Janson C, Bjornsson E, Hetta J, Boman G. Anxiety and depression in relation to respiratory symptoms and asthma. American Journal of Respiratory and Critical Care Medicine. 1994;149(4):930–4. doi: 10.1164/ajrccm.149.4.8143058. [DOI] [PubMed] [Google Scholar]
- 15.Mancuso CA, Wenderoth S, Westermann H, Choi TN, Briggs WM, Charlson ME. Patient-Reported and Physician-Reported Depressive Conditions in Relation to Asthma Severity and Control. Chest. 2008;133(5):1142–8. doi: 10.1378/chest.07-2243. [DOI] [PubMed] [Google Scholar]
- 16.Reddel HK, Taylor DR, Bateman ED, Boulet L-P, Boushey HA, Busse WW, et al. An Official American Thoracic Society/European Respiratory Society Statement: Asthma Control and Exacerbations: Standardizing Endpoints for Clinical Asthma Trials and Clinical Practice. American Journal of Respiratory and Critical Care Medicine. 2009;180(1):59–99. doi: 10.1164/rccm.200801-060ST. [DOI] [PubMed] [Google Scholar]
- 17.GINA. The Global Initiative for Asthma (GINA): The Global Initiative for Asthma. 2011 [cited 2012 December 20]. Available from: http://www.ginasthma.org/
- 18.National Heart, Lung, and Blood Institute,, National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. U.S. Department of Health and Human Services: National Institutes of Health; National Heart, Lung, and Blood Institute; 2007. [cited 2012 December 6]. Available from: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. [Google Scholar]
- 19.Proceedings of the ATS Workshop on Refractory Asthma. Current Understanding, Recommendations, and Unanswered Questions. American Journal of Respiratory and Critical Care Medicine. 2000;162(6):2341–51. doi: 10.1164/ajrccm.162.6.ats9-00. [DOI] [PubMed] [Google Scholar]
- 20.Lavoie KL, Bacon SL, Barone S, Cartier A, Ditto B, Labrecque M. What Is Worse for Asthma Control and Quality of Life: Depressive Disorders, Anxiety Disorders, or Both? Chest. 2006;130(4):1039–47. doi: 10.1378/chest.130.4.1039. [DOI] [PubMed] [Google Scholar]
- 21.Chapman KR, Patel P, D’Urzo AD, Alexander M, Mehra S, Oedekoven C, et al. Maintenance of asthma control by once-daily inhaled ciclesonide in adults with persistent asthma. Allergy. 2005;60(3):330–7. doi: 10.1111/j.1398-9995.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- 22.Clark NM. Community-Based Approaches to Controlling Childhood Asthma. Annual Review of Public Health. 2012;33(1):193–208. doi: 10.1146/annurev-publhealth-031811-124532. [DOI] [PubMed] [Google Scholar]
- 23.Mancuso CA, Peterson MGE, Charlson ME. Effects of Depressive Symptoms on Health-related Quality of Life in Asthma Patients. JGIM: Journal of General Internal Medicine. 2000;15(5):301. doi: 10.1046/j.1525-1497.2000.07006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katz PP, Morris A, Julian L, Omachi T, Yelin EH, Eisner MD, et al. Onset of depressive symptoms among adults with asthma: results from a longitudinal observational cohort. Primary Care Respiratory Journal. 2010;19(3):223–30. doi: 10.4104/pcrj.2010.00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cockcroft DW, Swystun VA. Asthma control versus asthma severity. The Journal of allergy and clinical immunology. 1996;98(6):1016–8. doi: 10.1016/s0091-6749(96)80185-0. [DOI] [PubMed] [Google Scholar]
- 26.Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. Journal of Allergy and Clinical Immunology. 2007;119(2):405–13. doi: 10.1016/j.jaci.2006.11.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An Inventory for Measuring Depression. Archives of General Psychiatry. 1961;4(6):561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Alford BA. Depression Causes and Treatment. Philadelphia: University of Pennsylvania Press; 2009. [Google Scholar]
- 29.Cavanaugh S, Clark DC, Gibbons RD. Diagnosing depression in the hospitalized medically ill. Psychosomatics. 1983;24(9):809–15. doi: 10.1016/S0033-3182(83)73151-8. [DOI] [PubMed] [Google Scholar]
- 30.Suárez-Mendoza AA, Cardiel MH, Caballero-Uribe CV, Ortega-Soto HA, Márquez-Marin M. Measurement of depression in mexican patients with rheumatoid arthritis: Validity of the beck depression inventory. Arthritis & Rheumatism. 1997;10(3):194–9. doi: 10.1002/art.1790100307. [DOI] [PubMed] [Google Scholar]
- 31.Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 32.Craven J, Rodin G, Littlefield C. The Beck Depression Inventory as a Screening Device for Major Depression in Renal Dialysis Patients. The International Journal of Psychiatry in Medicine. 1988;18(4):365–74. doi: 10.2190/m1tx-v1ej-e43l-rklf. [DOI] [PubMed] [Google Scholar]
- 33.Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax. 1992;47(2):76–83. doi: 10.1136/thx.47.2.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: Reliability, validity, and responsiveness in patients not previously followed by asthma specialists. Journal of Allergy and Clinical Immunology. 2006;117(3):549–56. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 35.Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. European Respiratory Journal. 1999;14(4):902–7. doi: 10.1034/j.1399-3003.1999.14d29.x. [DOI] [PubMed] [Google Scholar]
- 36.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. Journal of clinical epidemiology. 1994;47(1):81–7. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 37.Perna G, Bertani A, Politi E, Colombo G, Bellodi L. Asthma and panic attacks. Biological psychiatry. 1997;42(7):625–30. doi: 10.1016/S0006-3223(96)00436-2. [DOI] [PubMed] [Google Scholar]
- 38.Katon WJ, Richardson L, Lozano P, McCauley E. The Relationship of Asthma and Anxiety Disorders. Psychosomatic medicine. 2004;66(3):349–55. doi: 10.1097/01.psy.0000126202.89941.ea. [DOI] [PubMed] [Google Scholar]
- 39.Afari N, Schmaling KB, Barnhart S, Buchwald D. Psychiatric Comorbidity and Functional Status in Adult Patients with Asthma. Journal of Clinical Psychology in Medical Settings. 2001;8(4):245–52. [Google Scholar]
- 40.Kovács M, Stauder A, Szedmák S. Severity of allergic complaints: The importance of depressed mood. Journal of psychosomatic research. 2003;54(6):549–57. doi: 10.1016/s0022-3999(02)00477-4. [DOI] [PubMed] [Google Scholar]
- 41.Opolski M, Wilson I. Asthma and depression: a pragmatic review of the literature and recommendations for future research. Clinical Practice and Epidemiology in Mental Health. 2005;1(1):18. doi: 10.1186/1745-0179-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Janson-Bjerklie S, Ferketich S, Benner P, Becker G. Clinical Markers of Asthma Severity and Risk - Importance of Subjective as well as Objective Factors. Heart & lung. 1992;21(3):265–72. [PubMed] [Google Scholar]
- 43.Goral A, Lipsitz JD, Muhsen K, Gross R. Depressive symptoms, risk factors and sleep in asthma: results from a national Israeli health survey. General hospital psychiatry. 2012;34(1):17–23. doi: 10.1016/j.genhosppsych.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 44.Mastronarde JG, Wise RA, Shade DM, Olopade CO, Scharf SM. Sleep Quality in Asthma: Results of a Large Prospective Clinical Trial. Journal of Asthma. 2008;45(3):183–9. doi: 10.1080/02770900801890224. [DOI] [PubMed] [Google Scholar]
- 45.Parish JM. Sleep-Related Problems in Common Medical Conditions. Chest. 2009;135(2):563–72. doi: 10.1378/chest.08-0934. [DOI] [PubMed] [Google Scholar]
- 46.Holgate ST, Polosa R. The Mechanisms, diagnosis and management of severe asthma in adults. Lancet. 2006;368:780–93. doi: 10.1016/S0140-6736(06)69288-X. [DOI] [PubMed] [Google Scholar]
- 47.Dahlén I, Janson C. Anxiety and Depression Are Related to the Outcome of Emergency Treatment in Patients With Obstructive Pulmonary Disease. Chest. 2002;122(5):1633. doi: 10.1378/chest.122.5.1633. [DOI] [PubMed] [Google Scholar]


