Abstract
HIV/AIDS-related stigma and discrimination have a substantial impact on people living with HIV/AIDS (PLHA). The objectives of this study were: (1) to determine the associations of two constructs of HIV/AIDS-related stigma and discrimination (negative attitudes towards PLHA and perceived acts of discrimination towards PLHA) with previous history of HIV testing, knowledge of antiretroviral therapies (ARVs) and communication regarding HIV/AIDS and (2) to compare these two constructs across the five research sites with respect to differing levels of HIV prevalence and ARV coverage, using data presented from the baseline survey of U.S. National Institute of Mental Health (NIMH) Project Accept, a four-country HIV prevention trial in Sub-Saharan Africa (Tanzania, Zimbabwe and South Africa) and northern Thailand. A household probability sample of 14,203 participants completed a survey including a scale measuring HIV/AIDS-related stigma and discrimination. Logistic regression models determined the associations between negative attitudes and perceived discrimination with individual history of HIV testing, knowledge of ARVs and communication regarding HIV/AIDS. Spearman's correlation coefficients determined the relationships between negative attitudes and perceived discrimination and HIV prevalence and ARV coverage at the site-level. Negative attitudes were related to never having tested for HIV, lacking knowledge of ARVs, and never having discussed HIV/AIDS. More negative attitudes were found in sites with the lowest HIV prevalence (i.e., Tanzania and Thailand) and more perceived discrimination against PLHA was found in sites with the lowest ARV coverage (i.e., Tanzania and Zimbabwe). Programs that promote widespread HIV testing and discussion of HIV/AIDS, as well as education regarding and universal access to ARVs, may reduce HIV/AIDS-related stigma and discrimination.
Keywords: Sub-Saharan Africa, Thailand, HIV/AIDS, Stigma, Discrimination, Tanzania, Zimbabwe, South Africa
Introduction
Health-related stigma is defined by Weiss, Ramakrishna, and Somma (2006) as “a social process, experienced or anticipated, characterized by exclusion, rejection, blame or devaluation that results from experience, perception or reasonable anticipation of an adverse social judgment about a person or group” (Weiss et al., 2006). Historically, illnesses most likely to induce stigmatizing attitudes are those characterized as difficult to conceal, disruptive or intrusive to daily living, manifested with disfiguring or visibly displeasing qualities, incurable and progressive, and with a high propensity for transmission, qualities which to varying degrees describe the stages of HIV/AIDS (Herek, 1990). However, these characteristics are not necessary or sufficient to explain illness-related stigma, as in the case of epilepsy which is non-progressive and HIV which is almost entirely asymptomatic prior to the onset of AIDS.
HIV/AIDS-related stigma and discrimination have had a substantial impact on people living with HIV/AIDS (PLHA) and those at risk of HIV infection. HIV-related stigma has been shown to act as a barrier to HIV voluntary counseling and testing (VCT) as well as to the effectiveness of prevention and care services (Boer & Emons, 2004; Carr & Gramling, 2004; Doherty, Chopra, Nkonki, Jackson, & Greiner, 2006; Kalichman & Simbayi, 2003; Thomas et al., 2005; Turan, Miller, Bukusi, Sande, & Cohen, 2008). Often these barriers are most profound in settings with limited access to antiretroviral therapies (ARVs). Previous research demonstrated that access to ARVs reduces HIV/AIDS-related stigma (Abadia-Barrero & Castro, 2006; Castro & Farmer, 2005; Wolfe et al., 2008). As ARV programs continue to scale-up and access to therapies increases worldwide, it is crucial to consider the role of HIV/AIDS-related stigma in the design and implementation of effective prevention and treatment programs.
There has been substantial research on HIV-related stigma in settings with concentrated epidemics where layered stigma, that is, stigma compounded with other socially stigmatized conditions, has most often been observed. Layered stigma is prominent worldwide among men who have sex with men and injection drug users, compounding negative social norms surrounding behaviors linked with HIV infection (Herek, 1990; Nyblade, 2006). Less is known about the features of HIV-related stigma in generalized epidemics. While not as closely linked to the layered stigma observed in concentrated epidemics, HIV-related stigma may still be heightened in populations vulnerable to the historical and socioeconomic processes shaping the social inequalities fueling HIV/AIDS epidemics and influencing access to and use of prevention, treatment and care services (Castro & Farmer, 2005).
Several instruments have been developed to measure self-reported HIV/AIDS stigma among PLHA (Berger, Ferrans, & Lashley, 2001; Holzemer et al., 2007; Kalichman et al., 2009). However, measuring HIV/AIDS-related stigma from the perspective of the general population with survey methods has been a challenge to the scientific community, with only a few scales implemented across multiple contexts (Nyblade, 2006). In past quantitative studies of stigma in multiple settings, there have not been direct comparisons across epidemiologic or cultural contexts (Kalichman et al., 2005; Reidpath, Brijnath, & Chan, 2005). Although some authors have argued that HIV/AIDS-related stigma should be measured using scales designed specifically for a given culture (Weiss et al., 2006), this limits comparability across sites. Others have argued that stigma stems from a similar underlying construct and can, therefore, be measured across cultural contexts (Van Brakel, 2006).
Studies must consider the multi-faceted nature of HIV/AIDS-related stigma and attempt to measure the distinct components of stigma and their differential impacts. Recent arguments have been made to incorporate discrimination as a component of HIV/AIDS-related stigma (Mahajan et al., 2008; Maluwa, Aggleton, & Parker, 2002; Nyblade, 2006). Obermeyer and Osborn (2007) noted the difficulties associated with measuring self-reported discriminatory behaviors; this challenge may be addressed by assessing perceptions of discriminatory actions faced by PLHA in respondents' environments. Prior qualitative research in Sub-Saharan Africa has focused on HIV-related discrimination (Dlamini et al., 2007; Kohi et al., 2006), but to our knowledge there have been no efforts to quantitatively measure both HIV/AIDS-related stigmatizing attitudes and discrimination among the general population.
The data presented here are from U.S. National Institute of Mental Health (NIMH) Project Accept, a four-country HIV prevention trial in Tanzania, Zimbabwe, South Africa, and northern Thailand (Khumalo-Sakutukwa et al., 2008). The context of the HIV/AIDS epidemic is distinct in each of these settings. The epidemic in Thailand is primarily concentrated among sex workers, men who have sex with men and injection drug users (Chariyalertsak, Aramrattana, & Celentano, 2008), while in the Sub-Saharan African settings, the epidemic is generalized in the adult population and has been present much longer than it has been recognized as a public health problem (Beyrer, Davis, & Celentano, 2008). Further, while the HIV prevalence in Chiang Mai Province in 2005–2006 was estimated to be below 2%, there was a range of HIV prevalence in the African sites, from 7 to 10% in the Kisarawe District of Tanzania, to 15% in the Gauteng Province of South Africa, to between 18 and 20% in the Mutoko District of Zimbabwe, to a high of 39% among women attending antenatal care in the KwaZulu Natal Province of South Africa (Genberg, Kulich et al., 2008). Within the African sites, the resources devoted to stemming the epidemic varied substantially, with the greatest monetary resources and programmatic efforts mounted by South Africa, despite political debate surrounding the national response to HIV in this country (McIntyre, de Bruyn, & Gray, 2008), followed by Tanzania and trailed by Zimbabwe. In contrast, the Thai national response in terms of HIV prevention among sex workers and provision of ARVs has been substantial (Chariyalertsak et al., 2008). Finally, the study settings represent diverse population and cultural profiles, with four of the five study communities in rural or semi-rural areas (the exception being urban Soweto).
This paper presents an assessment of HIV/AIDS-related stigma and discrimination from household probability samples in these four countries. We analyzed two components of HIV-related stigma (negative attitudes and perceived acts of discrimination towards PLHA) by history of prior HIV testing, knowledge of ARVs, and communication regarding HIV/AIDS. We hypothesized a priori that individuals with no history of HIV testing, no knowledge of ARVs and no history of communication about HIV/AIDS would hold more negative attitudes towards PLHA. We further compared the distributions of these two components across the five research sites and hypothesized that the distinct epidemiologic contexts, combined with the varying availability resources across these five sites, would be associated with differences in the observed HIV/AIDS-related stigma and discrimination perceived and expressed by individuals living in these settings. Specifically, we hypothesized that individuals in sites with lower HIV prevalence would express higher levels of negative attitudes towards PLHA than those living in higher prevalence settings, while individuals living in areas with greater availability of resources would convey lower levels of perceived discrimination towards PLHA.
Methods
The methods of this survey have been reported in detail elsewhere (Genberg, Kulich et al., 2008). Briefly, the Project Accept baseline survey was conducted in 48 communities in 5 sites: Chiang Mai Province, Thailand (14 communities); Mutoko District, Mashonaland East Province, Zimbabwe (8 communities); Kisarawe District in the Pwani region of Tanzania (10 communities); Vulindlela, KwaZulu Natal Province (8 communities), and Soweto, Gauteng Province, South Africa (8 communities). Data were collected during 2005–2006.
The multi-stage sampling strategy yielded 14,367 individuals overall. Household enumerations were conducted from which random household probability samples were drawn. One eligible individual aged 18–32 from each household was randomly selected to participate. Interviewer-administered questionnaires measured demographic characteristics, sexual behaviors, communication regarding HIV/AIDS, attitudes and perceptions about HIV stigma and discrimination, HIV testing history and knowledge of ARVs. The survey was created in English and translated into Thai, Shona, Swahili, Zulu, Sotho and Tsonga. Surveys were back-translated, revised and pilot tested in all five sites.
Measurement of stigma and discrimination
Respondents were asked to respond to 22 statements about PLHA according to a 5-point Likert scale. The scale was developed in advance of the current study from two pilot investigations conducted in Thailand and Zimbabwe (Genberg, Kawichai et al., 2008). Briefly, this instrument measured three constructs of HIV-related stigma and discrimination. The first subscale measured negative attitudes and beliefs associated with PLHA, including blame on PLHA for their infection, and whether PLHA should be ashamed and isolated. This subscale also included items regarding negative feelings about PLHA (e.g., PLHA are disgusting). The second subscale focused on the respondents' perceptions of acts of discrimination faced by PLHA within their community. The third subscale included items focused on personal attitudes and beliefs related to fair treatment of PLHA in society. Respondents were asked their level of agreement with restrictive policies for PLHA and whether PLHA should have equal rights.
Exploratory factor analyses of the stigma constructs as specified a priori was conducted with R software (R Development Core Team, 2008) using the principal factors method and varimax rotation on the original 22 items from 14,203 respondents (164 respondents had missing data on stigma questions). Positively worded items were reverse-coded for consistency in meaning. We set the minimum factor loading to 0.40 as the threshold for scale inclusion. A three-factor solution emerged from the initial exploratory factor analysis of the scale items (data not shown), confirming the factor structure of the pilot study. The factors included eight, seven and four items accounting for 14.3%, 14.5% and 9% of the total variance, respectively. From this initial analysis, we observed minor changes to the original pilot scale which we incorporated into confirmatory analysis (Appendix 1).
Confirmatory factor analysis was conducted using LISREL with a structural equation model with a polychoric correlation matrix specifying a priori three correlated factors measured with 19 items on the total sample (Muthen & Kaplan, 1985; Muthen, 1984). Polychoric correlations are less biased when used with Likert scale variables (Jorsekog & Moustaki, 2001). We utilized the entire sample in order to define one scale to be used across multiple settings. The confirmatory factor analysis produced similar results to the exploratory analysis (Appendix 1). Overall, the internal consistency of the first two subscales was good (Appendix 2): Cronbach's alpha measures were 0.82 and 0.81 overall. The internal consistency of the third subscale was acceptable at 0.68 overall, however, since it was comparatively lower, the remaining analyses excluded this subscale.
We did not present a total stigma score (an overall score combining the two remaining subscales) since the components are related, but representing different aspects of HIV/AIDS-related stigma. While we would expect that individuals with negative attitudes towards PLHA would be more likely to report large amounts of discrimination, the two subscales could also be independent. The correlation between the two subscales from the structural equation model was low (Φ = 0.261) providing further evidence that the two factors required separate analyses.
Data analysis
The items in each subscale were summed and standardized by the number of items to create individual mean and median scores, with higher scores (from 0 to 4) indicating more negative attitudes or perceived discrimination. Descriptive statistics of the subscales were evaluated overall and by site. Crude logistic regression models examining the associations of history of HIV testing, knowledge of ARVs, and communication regarding HIV/AIDS, as well as models adjusted for sex, age and recent sexual behaviors, were estimated with a score in the top quartile of each of the factors as the outcome, stratified by site. The 75th percentile cut point was determined based on data from all five sites to enable comparisons of individuals in the top of the distribution of scores across the five sites. Data analysis was conducted using R software (R Development Core Team, 2008).
We examined the correlations between the proportions exceeding the 75th percentile for each factor within each site (n = 5 sites) and two macro-level factors: HIV prevalence and national ARV coverage, using Spearman's rank correlation tests. We used HIV prevalence estimates from those seeking VCT from the Project Accept mobile units in the intervention communities, where nearly 40% of the adult population aged 18–32 years has been tested to date (Khumalo-Sakutukwa et al., 2008). ARV coverage estimates, characterized as the proportion of individuals receiving treatment relative to those in need, were obtained from the World Health Organization's 3-by-5 Initiative as of June 2005 (World Health Organization, 2005).
Results
Sample demographic and behavioral characteristics
Table 1 presents the socio-demographic characteristics of the sample. The overall median age was 24 years and over 44% were male. Behaviors and knowledge related to HIV/AIDS varied across the five sites and were presented previously in detail (Genberg, Kulich et al., 2008). In all sites, 32.8% reported ever having been tested for HIV, ranging from 9.4% in Zimbabwe to 49.1% in Soweto. On average, 53.3% had heard of ARVs, ranging from 28.3% in Zimbabwe to 75.5% in Soweto. The majority (69%) had discussed HIV/AIDS, ranging from 51.2% in Tanzania to 88.7% in Soweto.
Table 1.
Socio-demographic characteristics and HIV/AIDS-related knowledge and behaviors, by site and overall.
| Thailand, N = 2997 |
Tanzania, N = 3073 |
Soweto, SA,a N = 2663 |
Zimbabwe, N = 2874 |
Vulindlela, SA,a N = 2596 |
Total, N = 14,203 |
|
|---|---|---|---|---|---|---|
| Age, median (interquartile range) | 26 (8) | 25 (9) | 24 (7) | 23 (8) | 23 (8) | 24 (9) |
| Male, % | 47.4 | 46.3 | 45.4 | 43.0 | 41.4 | 44.8 |
| Education, % | ||||||
| <5 years | 30.1 | 30.7 | 1.0 | 3.4 | 2.7 | 14.4 |
| 5–10 years | 45.8 | 64.8 | 20.2 | 48.1 | 34.2 | 43.5 |
| 11–12 years | 16.9 | 3.4 | 66.3 | 43.5 | 58.4 | 36.2 |
| 12 + years | 7.1 | 1.2 | 12.5 | 5.0 | 4.7 | 6.0 |
| Marital Status, % | ||||||
| Single | 33.9 | 45.3 | 88.4 | 42.5 | 95.7 | 59.6 |
| Married | 56.6 | 48.4 | 10.3 | 46.3 | 3.6 | 34.4 |
| Separated | 4.3 | 0.7 | 0.4 | 3.3 | 0.3 | 1.8 |
| Divorced | 0.4 | 1.1 | 0.3 | 0.4 | 0.1 | 0.5 |
| Widowed | 4.0 | 3.9 | 0.5 | 5.0 | 0.2 | 2.8 |
| Earned money for work,b % | 85.6 | 59.4 | 65.4 | 55.1 | 47.5 | 63.0 |
| Household socioeconomic status,c % | ||||||
| Low | 26.7 | 37.2 | 11.2 | 35.5 | 37.0 | 29.7 |
| Moderate | 30.4 | 54.9 | 61.2 | 51.5 | 50.0 | 49.4 |
| High | 43.0 | 7.9 | 27.5 | 13.0 | 13.0 | 20.9 |
| Ever had sex, % | 79.9 | 89.6 | 88.0 | 79.5 | 89.5 | 85.2 |
| Ever HIV test, % | 44.0 | 30.4 | 49.1 | 9.4 | 32.0 | 32.8 |
| Knowledge of ARVs, % | 55.5 | 41.7 | 75.0 | 28.3 | 69.8 | 53.3 |
| Ever talked about HIV/AIDS, % | 62.6 | 51.2 | 88.7 | 70.3 | 75.9 | 69.0 |
SA = South Africa.
Refers to respondent's earning money from a person, trade, organization or self-employment in the past twelve months.
These categories are determined by site-specific definitions of socioeconomic status, however, comparisons of within-site tertiles can still be made across sites.
HIV/AIDS-related stigma and discrimination
In all sites, never having had an HIV test was associated with negative attitudes towards PLHA compared to those who had ever been tested (Table 2), although the difference was statistically significant in Thailand only (OR = 1.68, 95% CI: 1.37, 2.04) after adjusting for age, sex and recent sexual behavior. No knowledge of ARVs was associated with negative attitudes towards PLHA when compared with those who had knowledge across all sites, a relationship that remained statistically significant after adjusting for age, sex and recent sexual behavior in all sites except Soweto (OR = 1.38, 95% CI: 0.92, 2.06). Never having talked about HIV/AIDS was also associated with negative attitudes towards PLHA compared with those who had ever talked, a difference that remained statistically significant across all five sites in models adjusted for age, sex and recent sexual behavior.
Table 2.
Mean and median negative attitude score, proportions above the upper quartile of the overall negative attitudes score, crude (OR) and adjusted odds ratios (AOR) and 95% confidence intervals (CI) of being in the upper quartilea by site, HIV testing history, knowledge of ARVs and communication about HIV/AIDS.
| Thailand | Tanzania | Soweto, SAb | Zimbabwe | Vulindlela, SAb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Meanc (SD) | 1.35 (0.49) | 1.66 (0.76) | 0.79 (0.53) | 1.23 (0.62) | 0.93 (0.40) | |||||
| Medianc (interquartile range) | 1.25 (0.62) | 1.50 (1.25) | 0.88 (0.75) | 1.12 (0.62) | 1.00 (0.38) | |||||
| % Above upper quartile | 25.4 OR (95% CI) |
AOR (95% CI) | 49.8 OR (95% CI) |
AOR (95% CI) | 6.1 OR (95% CI) |
AOR (95% CI) | 23.7 OR (95% CI) |
AOR (95% CI) | 3.9 OR (95% CI) |
AOR (95% CI) |
| No HIV test | 2.07 (1.74, 2.46) | 1.68 (1.37, 2.04) | 1.07 (0.92, 1.25) | 1.04 (0.88, 1.24) | 1.78 (1.23, 2.58) | 1.42 (0.93, 2.16) | 1.27 (0.93, 1.73) | 1.06 (0.77, 1.46) | 1.60 (1.00, 2.57) | 1.12 (0.65, 1.92) |
| No knowledge of ARVs | 4.45 (3.72, 5.32) | 3.33 (2.75, 4.05) | 1.79 (1.55, 2.07) | 1.51 (1.29, 1.76) | 1.75 (1.21, 2.53) | 1.38 (0.92, 2.06) | 1.94 (1.57, 2.40) | 1.77 (1.42, 2.21) | 2.12 (1.43, 3.17) | 1.75 (1.13, 2.69) |
| Never talked about HIV/AIDS | 2.73 (2.31, 3.23) | 1.64 (1.36, 1.98) | 2.53 (2.18, 2.92) | 2.32 (1.99, 2.70) | 2.52 (1.65, 3.87) | 1.81 (1.13, 2.90) | 1.64 (1.37, 1.97) | 1.52 (1.28, 1.82) | 2.28 (1.51, 3.43) | 2.10 (1.35, 3.27) |
Above the upper quartile of negative attitudes across all sites (1.50).
SA = South Africa; AORs adjusted for sex, age, sexual behavior in the previous six months and other factors included in the table; bolding indicates confidence interval does not cross 1.00.
4 = Strongly agree; 3 = agree; 2 = don't know; 1 = disagree; 0 = strongly disagree.
Never having had an HIV test was associated with higher perceived discrimination compared to those who had ever tested in Thailand only, a difference that was nearly statistically significant (OR = 1.96, 95% CI: 0.96, 4.00) after adjustment for age, sex and recent sexual behavior (Table 3). No knowledge of ARVs was significantly associated with lower perceived discrimination compared to those with knowledge of ARVs in Zimbabwe and the two South African sites (Table 2), but conversely, this relationship was associated with higher perceived discrimination in Thailand (OR = 3.97, 95% CI: 1.76, 8.95). Never talking about HIV/AIDS was associated with higher perceived discrimination compared to those who had ever talked about HIV/AIDS in Thailand and Tanzania, but was associated with lower perceived discrimination in Soweto after adjustment for age, sex and recent sexual behavior (OR = 0.71, 0.52, 0.95).
Table 3.
Mean and median perceived discrimination score, crude (OR) and adjusted odds ratios (AOR) with 95% confidence intervals (CI) of being in the upper quartilea by site, HIV testing history, knowledge of ARVs, and communication about HIV/AIDS.
| Thailand | Tanzania | Soweto, SAb | Zimbabwe | Vulindlela, SAb | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Meanc (SD) | 1.32 (0.45) | 2.04 (0.76) | 2.02 (0.77) | 2.32 (0.66) | 1.76 (0.67) | |||||
| Medianc (Interquartile range) | 1.29 (0.57) | 2.14 (1.29) | 2.00 (1.14) | 2.43 (0.86) | 1.71 (0.86) | |||||
| % Above upper quartile | 1.6 OR (95% CI) |
AOR (95% CI) | 31.5 OR (95% CI) |
AOR (95% CI) | 29.1 OR (95% CI) |
AOR (95% CI) | 41.5 OR (95% CI) |
AOR (95% CI) | 14.3 OR (95% CI) |
AOR 95% CI) |
| No HIV test | 2.60 (1.32, 5.13) | 1.96 (0.96, 4.00) | 1.12 (0.95, 1.33) | 1.05 (0.87, 1.26) | 0.92 (0.78, 1.08) | 1.03 (0.85, 1.24) | 0.89 (0.69, 1.15) | 0.96 (0.74, 1.24) | 0.80 (0.64, 1.01) | 0.91(0.71, 1.17) |
| No knowledge of ARVs | 6.24 (2.91, 13.40) | 3.97 (1.76, 8.95) | 1.11 (0.95, 1.30) | 1.02 (0.87, 1.20) | 0.64 (0.52, 0.78) | 0.68 (0.55, 0.84) | 0.78 (0.66, 0.92) | 0.82 (0.69, 0.97) | 0.70 (0.54, 0.91) | 0.74 (0.57, 0.97) |
| Never talked about HIV/AIDS | 3.30 (1.80, 6.06) | 1.88 (0.98, 3.59) | 1.56 (1.34, 1.82) | 1.61 (1.37, 1.89) | 0.64 (0.48, 0.85) | 0.71 (0.52, 0.95) | 0.93 (0.79, 1.09) | 0.99 (0.84, 1.18) | 1.02 (0.79, 1.32) | 1.13 (0.86, 1.49) |
Above the upper quartile of perceived discrimination across all sites (2.43).
SA = South Africa; AORs adjusted for sex, age, sexual behavior in the previous six months and other factors included in the table; bolding indicates confidence interval does not cross 1.00.
4 = Strongly agree; 3 = agree; 2 = don't know; 1 = disagree; 0 = strongly disagree.
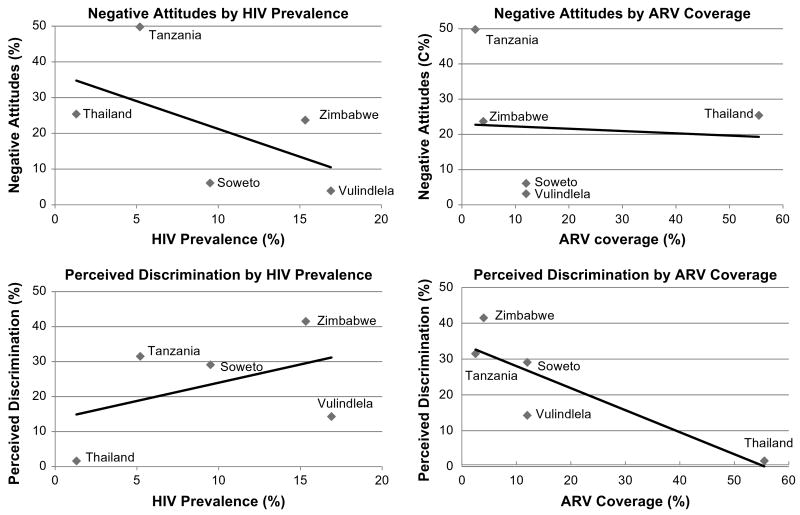
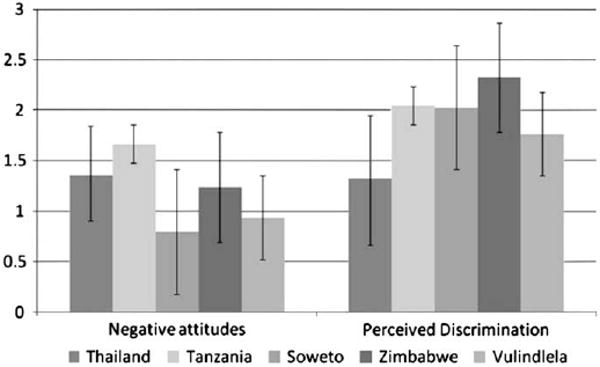
The mean scores for the two subscales are represented in Fig. 1, where the sites are arranged in order from lowest to highest HIV prevalence. The mean negative attitudes score was 1.20 (SD = 0.65) across sites, ranging from 0.79 in Soweto to 1.66 in Tanzania (Table 2). Very few respondents in both South African sites were classified within the upper quartile of negative attitudes scores (3.9% in Vulindlela and 6.1% in Soweto), while approximately one-quarter of participants in Thailand and Zimbabwe and nearly half in Tanzania exceeded the 75th percentile for this measure. Fig. 2 depicts the proportions of individuals with scores above the 75th percentile in each site for each factor by HIV prevalence and ARV coverage estimates. Negative attitudes towards PLHA were negatively correlated with HIV prevalence (rho = −0.60, p < 0.28), such that as HIV prevalence increased, the proportion expressing negative attitudes towards PLHA decreased (Fig. 2). There was a weaker negative correlation observed between ARV coverage and negative attitudes towards PLHA (rho = −0.36, p < 0.55).
Fig. 1.
Mean scores (and standard deviation bars) of negative attitudes and perceived discrimination towards PLHA by site.
Fig. 2.
Proportions above the overall 75th percentile of negative attitudes and perceived discrimination scores by site, HIV prevalence and ARV coverage.
The mean perceived discrimination score overall was 1.90 (SD = 0.75) across the five sites. The lowest mean score was in Thailand, 1.32, with the highest score found in Zimbabwe, 2.32 (Fig. 1). A very low percentage (1.6%) of the respondents in Thailand scored within the upper quartile of perceived discrimination scores (Table 3). The African sites had higher proportions within the upper quartile of perceived discrimination scores, ranging from moderate in South Africa (14.3% in Vulindlela and 29.1% in Soweto) and Tanzania (31.5%), to the highest in Zimbabwe (41.5%). We observed a weak positive correlation between HIV prevalence and the proportion of the sample in the upper quartile of perceived discrimination scores (rho = 0.30, p < 0.62) such that as prevalence increased, perceived discrimination also increased (Fig. 2). Finally, there was a strong statistically significant negative correlation between perceived discrimination towards PLHA and ARV coverage (rho = −0.87, p < 0.05).
Discussion
The findings address two components of HIV/AIDS-related stigma and discrimination in five distinct cultural and epidemiologic settings. The inclusion of perceived discrimination towards PLHA in this analysis fills a gap in the existing literature (Nyblade, 2006; Obermeyer & Osborn, 2007). The ecological analyses provided additional context for the interpretation of the results across the five research sites.
Despite the differences in negative attitudes towards PLHA and perceived discrimination of PLHA in the study settings, the overall levels observed were not high. However, using a common cut point to define individuals in the upper end of the distribution of score across the sites enabled us to explore the variations that exist in these settings and to make comparisons of HIV/AIDS-related stigma and discrimination across the study sites.
HIV testing
Previous research has suggested that fear of stigmatization and discrimination is a barrier to HIV testing in diverse settings (Day et al., 2003; Ma et al., 2007) and that individuals who had never been tested for HIV were more likely to express stigmatizing attitudes towards PLHA (Hutchinson & Mahlalela, 2006; Kalichman & Simbayi, 2003; Pulerwitz, Michaelis, Lippman, Chinaglia, & Diaz, 2008). The results of this study confirmed the association between negative attitudes towards PLHA and not having been tested for HIV, but the relationship was statistically significant in Thailand and borderline significant in Soweto. It is important to note that these two sites also reported the highest levels of HIV testing (44% in Thailand; 49% in Soweto), thus providing more variance for statistical purposes, and the greatest level of resources committed to HIV/AIDS prevention and care when compared to Zimbabwe and Tanzania. In Tanzania, HIV testing was four times as common among females as males (Genberg, Kulich et al., 2008), because women were often tested in the context of antenatal care. The literature suggests that women's experiences testing during pregnancy are very different from individuals who seek VCT (Medley, Garcia-Moreno, McGill, & Maman, 2004), which may account for why no statistical association was observed between testing and negative attitudes in Tanzania.
Knowledge of ARVs
In the current study, lack of knowledge of ARVs was associated with negative attitudes towards PLHA in all five settings. This finding confirms previous qualitative studies which showed that access to ARVs was related to HIV/AIDS-related stigma (Abadia-Barrero & Castro, 2006; Castro & Farmer, 2005), as well as a recent population-based study in Botswana which showed that perceived availability of ARVs was associated with reduced HIV-related stigma (Wolfe et al., 2008). Lacking knowledge of ARVs suggests that the individual is unaware that treatment is available for HIV, a belief known to be associated with stigmatizing attitudes (Herek, 1990). ARV programs accompanied by population-based educational campaigns may reduce negative attitudes towards PLHA.
Communication about HIV/AIDS
A recent study demonstrated that informal communication about HIV/AIDS was associated with lower HIV-related stigma (Hutchinson, Mahlalela, & Yukich, 2007). Our findings also demonstrate that individuals who had never talked about HIV/AIDS with anyone were more likely in all five sites to hold more negative attitudes about PLHA. These findings suggest that initiatives which increase discussion about HIV/AIDS in informal settings and within existing social networks may reduce negative attitudes towards PLHA (Campbell, Nair, Maimane, & Nicholson, 2007). Informal discussion about HIV/AIDS, a mechanism that has been suggested to have greater influence on personal knowledge of PLHA than the stage of the HIV epidemic in a region, may increase personal exposure to PLHA and as a result, decrease HIV-related stigma, and perhaps even risk behaviors related to HIV (Stoneburner & Low-Beer, 2004). HIV prevention efforts and stigma-reduction programs should incorporate novel approaches to foster discussion about HIV/AIDS in informal settings.
Perceived discrimination towards PLHA
In Thailand and Tanzania, lacking knowledge of ARVs and never having talked about HIV/AIDS were associated with increased perceived discrimination towards PLHA. It is possible that in low prevalence settings individuals lack personal experience with PLHA and may overestimate the amount of discrimination being experienced by PLHA in their communities. In Soweto, Vulindlela and Zimbabwe, individuals who had no knowledge of ARVs were significantly less likely than those with knowledge to perceive discrimination in their communities. This was also true for individuals who had never talked about HIV/AIDS in Soweto. Perhaps individuals living in high prevalence regions, who did not communicate about HIV and had no knowledge of treatment and prevention services, also remained unaware or in denial of the amount of discrimination experienced by PLHA. It is also possible that the types of discrimination assessed in the scale were not as relevant in these three sites. Further work on the relationships between knowledge of ARVs and perceived discrimination faced by PLHA living in high prevalence settings is needed.
HIV prevalence and ARV coverage
The three explanatory variables in this study may also be conceptualized as individual-level proxies for the availability and use of HIV treatment and prevention services at the broader community-level. We cannot make conclusive statements about the relationships observed in our ecological analyses due to the small number of sites, but the direction and magnitude of observed correlations suggest that negative attitudes and perceived discrimination expressed by individuals appeared to vary with the prevalence of HIV and the availability of HIV-related resources at the local level.
We observed a negative correlation between the proportion of individuals above the 75th percentile of negative attitudes scores and HIV prevalence. Individuals in higher prevalence regions have more opportunities than individuals in low prevalence regions to have personal contact and experiences with PLHA, or to be HIV-positive themselves, and this may have decreased fear, misunderstanding and blame directed towards PLHA. We previously demonstrated that in Thailand, a lower prevalence setting, individuals who knew someone living with HIV/AIDS were less likely to have negative attitudes towards PLHA (Genberg, Kawichai et al., 2008). It is also possible that in areas of higher HIV prevalence, increased exposure to PLHA and knowledge of PLHA who represent normative demographic and behavioral characteristics (i.e., heterosexual transmission routes) prompts further examination of higher levels of perceived personal risk of and vulnerability to HIV infection. This may promote greater compassion and decreased blame attributable to PLHA than would be observed in places with lower HIV prevalence and/or concentrated epidemics. It is also possible that in South Africa, there was greater exposure to HIV/AIDS health education and stigma-reduction programs which we would expect to reduce negative attitudes towards PLHA. In addition, while not addressed specifically in this scale, the layering of stigma may also partially account for the higher levels of negative attitudes towards PLHA observed in Thailand. Within a concentrated epidemic, there may be greater blame placed on PLHA for acquiring HIV through personal behaviors that are perceived as morally questionable or socially deviant (e.g., injection drug use or sex work) than would be observed in generalized epidemics (Herek, 1990).
The highest levels of perceived discrimination of PLHA were observed in sites with the least amount of support and care available to PLHA (i.e., Tanzania and Zimbabwe). It is possible that in settings lacking sufficient treatment and care for HIV/AIDS, the elements of the infection which are known to fuel stigma, specifically difficulty concealing the infection, disruption of daily life, disfiguring or visibly displeasing symptoms, and faster progression to severe illness or death, were more prominent and had more influence on how PLHA were perceived in the community. In addition, areas with little or no available resources for care and treatment may have had the highest level of burden on the family and community, which may foster resentment and discrimination, particularly in areas with little economic and social capital.
We must not interpret the findings of this study solely in light of HIV prevalence or ARV coverage. First, the ARV coverage variable, as a proxy for the availability of resources in the community, is incomplete and the lack of relationship between ARV coverage and negative attitudes may be related to the limited nature of this variable. Prevention resources, as well as care and support programs beyond ARV coverage, are also important to capture and should be investigated in future studies. Secondly, the two macro-level factors must be considered concurrently. While the negative attitudes towards PLHA in South Africa were lower compared to the other sites, the perceived discrimination scores were similar to the other sites in Sub-Saharan Africa, possibly indicating that living in a setting with high HIV prevalence may lead to fewer personal negative attitudes about PLHA, but insufficient ARV coverage and the lower availability of HIV preventive and treatment resources in a high prevalence setting may contribute to persistent discrimination towards PLHA. Treatment and other resources were available in South Africa at the time of this study; however, ARV coverage was quite low (just above 10%). Available resources were also least accessible to those with the lowest social and economic capital, creating additional burden on families and communities. We would expect increasing HIV prevalence in a low-resource community to increase strain on the community and thereby lead to greater discrimination.
Project Accept qualitative study
The qualitative analyses from Project Accept also presented in this issue (Maman et al., submitted for publication) compared HIV/AIDS-related discrimination in the five research sites with respect to resource availability. The qualitative findings provided additional support that perceived acts of discrimination may be negatively related to ARV coverage. Use of ARVs in sites where treatment was available was described as a means to avoid physical symptoms and stay healthy as well as decrease the burden on the family by avoiding illness and continuing to contribute economically. Further in sites with access to ARVs (South Africa and Thailand), there was no mention of HIV as an inevitable death sentence, a narrative which was more prevalent in Tanzania and Zimbabwe, where access to ARVs was very limited.
The qualitative findings were less consistent with our findings regarding the association between negative attitudes towards PLHA and ARV coverage. Qualitative analyses suggested that while there was compassion for individuals in high prevalence areas due to the recognition that the risk of HIV infection was widespread and indiscriminant, fear of HIV transmission and blame towards PLHA seemed more pronounced in settings with fewer resources to address the epidemic. They found little evidence of negative attitudes towards PLHA in Thailand, the site with the highest ARV coverage. However, while people were compassionate towards PLHA in Thailand in general, they blamed individuals who were engaging in behaviors that placed others at risk of acquiring HIV infection.
Limitations
This study had several limitations. The scales employed in this study may induce social desirability bias. Individuals may be unwilling to express negative attitudes towards PLHA or discuss discrimination that they perceive in their communities during face-to-face interviews. As a result, the estimates in the current study may underestimate the true levels of negative attitudes and acts of discrimination towards PLHA. In addition, the overall percentage of variance explained by our scale was approximately 40%, indicating that there are features of HIV/AIDS-related stigma not being captured by the current measure which ought to be investigated in future research. Finally, this is a cross-sectional study and as a result, we cannot make any causal conclusions based on the associations presented. For example, negative attitudes could result in avoidance of testing or avoidance could lead to negative attitudes.
HIV/AIDS-related stigma and discrimination are often measured at the individual-level, although many of the attitudes expressed by individuals result from contextual factors constructed at the societal level. Recently, there have been calls for the analysis of HIV/AIDS-related stigma within frameworks that emphasize the larger economic and social processes within which stigma is generated (Castro & Farmer, 2005; Parker & Aggleton, 2003). HIV-related stigma builds on existing social inequalities, exacerbating the social differences between those at increased risk of HIV infection or living with HIV and those perceived to be at low risk (Boer & Emons, 2004). While this paper reflects HIV/AIDS-related stigma and discrimination at the individual level, and HIV prevalence and ARV coverage at the ecological level, future analyses should focus on understanding how stigma and related constructs such as ARV programs, availability of preventive services, and HIV prevalence at the contextual level impact individual-level attitudes and behaviors.
The approach presented in this paper utilized a common cut point and compared individuals across the sites according to levels of negative attitudes and perceived discrimination; we acknowledge the possibility that these cut points may have varied meanings in different settings. As a result, the comparisons of individuals scoring above these cut points in Thailand and Sub-Saharan Africa may not reflect true differences in stigmatizing attitudes and perceived discrimination. However, the scale items are descriptive and not tied to any specific cultural attitudes or acts, and, therefore, well-suited to use across multiple cultural settings.
The results of this study showed that negative attitudes and perceived discrimination towards PLHA were related to lacking knowledge of ARVs, a lack of prior history of HIV testing, and not having discussed HIV/AIDS with anyone. We observed the highest negative attitudes towards PLHA in sites with the lowest HIV prevalence (i.e., Tanzania and Thailand) and the highest perceived discrimination of PLHA in sites with the least support and care available to PLHA (i.e., Tanzania and Zimbabwe). Universal access to treatment for HIV and widespread educational and prevention efforts that promote understanding of ARVs, adoption of HIV testing, and discussion of HIV/AIDS, may reduce HIV/AIDS-related stigma and discrimination.
Appendix 1
Factor loadings from confirmatory factor analysis of the HIV/AIDS-related stigma and discrimination scale.a
| Item | Negative attitudes | Perceived discrimination | Equity |
|---|---|---|---|
| Families of people living with HIV/AIDS should be ashamed. | 0.809 | ||
| People living with HIV/AIDS should be ashamed. | 0.636 | ||
| People who have HIV/AIDS are cursed. | 0.715 | ||
| People who have AIDS are disgusting. | 0.789 | ||
| People living with HIV/AIDS deserve to be punished. | 0.723 | ||
| It is reasonable for an employer to fire people who have AIDS. | 0.709 | ||
| People with AIDS should be isolated from other people. | 0.778 | ||
| People with HIV/AIDS should not have the same freedoms as other people.b | 0.602 | ||
| People living with HIV/AIDS in this community face rejection from their peers. | 0.775 | ||
| People who have HIV/AIDS in this community face verbal abuse or teasing. | 0.758 | ||
| People living with HIV/AIDS in this community face ejection from their homes by their families. | 0.726 | ||
| People living with HIV/AIDS in this community face neglect from their family. | 0.705 | ||
| People who are suspected of having HIV/AIDS lose respect in the community. | 0.656 | ||
| People living with HIV/AIDS in this community face physical abuse. | 0.641 | ||
| Most people would not buy vegetables from a shopkeeper or food seller that they knew had AIDS. | 0.572 | ||
| People with AIDS should be treated similarly by health care professionals as people with other illnesses. | 0.644 | ||
| People with HIV should be allowed to fully participate in social events in this community.c | 0.724 | ||
| A person with AIDS should be allowed to work with other people.c | 0.710 | ||
| People who have HIV/AIDS should be treated the same as everyone else. | 0.754 | ||
| Goodness of Fit Statistics | |||
| Chi-square (df = 149) | 2875.09 (p< 0.00) | ||
| Goodness of Fit Index (GFI) | 0.991 | ||
| Root mean square error of approximation (RMSEA) | 0.035 | ||
The following changes to the original scale from EFA were incorporated into the CFA: people who have HIV/AIDS deserve compassion (removed from factor 1); people want to be friends with someone who has HIV/AIDS (removed from factor 2); people with HIV/AIDS do not deserve any support (removed from factor 3); blank cells indicate loading was <0.4.
Previously loaded on factor 3.
Previously loaded on factor 1.
Appendix 2
Reliability coefficients (Cronbach's alpha) and standard error of measurementa (SEM) for three factors by site and overall.
| Negative attitudes | Perceived discrimination | Equity | |
|---|---|---|---|
| Thailand | |||
| Reliability | 0.73 | 0.69 | 0.64 |
| SEM | 0.25 | 0.25 | 0.31 |
| Tanzania | |||
| Reliability | 0.83 | 0.80 | 0.64 |
| SEM | 0.31 | 0.34 | 0.39 |
| Soweto | |||
| Reliability | 0.77 | 0.80 | 0.72 |
| SEM | 0.25 | 0.34 | 0.33 |
| Zimbabwe | |||
| Reliability | 0.76 | 0.73 | 0.60 |
| SEM | 0.30 | 0.34 | 0.36 |
| Vulindlela | |||
| Reliability | 0.66 | 0.78 | 0.69 |
| SEM | 0.23 | 0.31 | 0.27 |
| Overall | |||
| Reliability | 0.82 | 0.81 | 0.68 |
Standard error of measurement: √variance(factor) (1 – reliability).
Footnotes
We thank the communities that partnered with us in conducting this research, and all study participants for their contributions. We also thank the Project Accept (HIV Prevention Trials Network, protocol 043) Steering Committee (Tom Coates, Deborah Donnell, Glenda Gray, Michal Kulich, Steve Morin, Linda Richter, and Michael Sweat), project directors (Kathryn Curran, Surinda Kawichai, Alfred Timbe), study staff and volunteers at all participating institutions for their work and dedication.
References
- Abadia-Barrero CE, Castro A. Experiences of stigma and access to HAART in children and adolescents living with HIV/AIDS in Brazil. Social Science & Medicine. 2006;62(5):1219–1228. doi: 10.1016/j.socscimed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in Nursing & Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Beyrer C, Davis W, Celentano DD. The HIV/AIDS epidemics of Africa. In: Celentano DD, Beyrer C, editors. Public health aspects of HIV/AIDS in low and middle income countries. New York: Springer; 2008. pp. 187–194. [Google Scholar]
- Boer H, Emons PA. Accurate and inaccurate HIV transmission beliefs, stigmatizing and HIV protection motivation in northern Thailand. AIDS Care. 2004;16(2):167–176. doi: 10.1080/09540120410001641011. [DOI] [PubMed] [Google Scholar]
- Campbell C, Nair Y, Maimane S, Nicholson J. ‘Dying twice’: a multilevel model of the roots of AIDS stigma in two South African communities. Journal of Health Psychology. 2007;12(3):403–416. doi: 10.1177/1359105307076229. [DOI] [PubMed] [Google Scholar]
- Carr RL, Gramling LF. Stigma: a health barrier for women with HIV/AIDS. The Journal of the Association of Nurses in AIDS Care. 2004;15(5):30–39. doi: 10.1177/1055329003261981. [DOI] [PubMed] [Google Scholar]
- Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. American Journal of Public Health. 2005;95(1):53–59. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chariyalertsak S, Aramrattana A, Celentano DD. The HIV/AIDS epidemic in Thailand: the first two decades. In: Celentano DD, Beyrer C, editors. Public health aspects of HIV/AIDS in low and middle income countries. New York: Springer; 2008. pp. 401–432. [Google Scholar]
- Day JH, Miyamura K, Grant AD, Leeuw A, Munsamy J, Baggaley R, et al. Attitudes to HIV voluntary counselling and testing among mineworkers in South Africa: will availability of antiretroviral therapy encourage testing? AIDS Care. 2003;15(5):665–672. doi: 10.1080/0954012030001595140. [DOI] [PubMed] [Google Scholar]
- Dlamini PS, Kohi TW, Uys LR, Phetlhu RD, Chirwa ML, Naidoo JR, et al. Verbal and physical abuse and neglect as manifestations of HIV/AIDS stigma in five African countries. Public Health Nursing. 2007;24(5):389–399. doi: 10.1111/j.1525-1446.2007.00649.x. [DOI] [PubMed] [Google Scholar]
- Doherty T, Chopra M, Nkonki L, Jackson D, Greiner T. Effect of the HIV epidemic on infant feeding in South Africa: “when they see me coming with the tins they laugh at me”. Bulletin of the World Health Organization. 2006;84(2):90–96. doi: 10.2471/blt.04.019448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genberg BL, Kawichai S, Chingono A, Sendah M, Chariyalertsak S, Konda KA, et al. Assessing HIV/AIDS stigma and discrimination in developing countries. AIDS and Behavior. 2008;12(5):772–780. doi: 10.1007/s10461-007-9340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genberg BL, Kulich M, Kawichai S, Modiba P, Chingono A, Kilonzo GP, et al. HIV risk behaviors in Sub-Saharan Africa and northern Thailand: baseline behavioral data from Project Accept. Journal of the Acquired Immune Deficiency Syndrome. 2008;49(3):309–319. doi: 10.1097/QAI.0b013e3181893ed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM. Psychological aspects of serious illness. Washington, DC: American Psychological Association; 1990. Illness, stigma and AIDS. [Google Scholar]
- Holzemer WL, Uys LR, Chirwa ML, Greeff M, Makoae LN, Kohi TW, et al. Validation of the HIV/AIDS stigma instrument – PLWA (HASI-P) AIDS Care. 2007;19(8):1002–1012. doi: 10.1080/09540120701245999. [DOI] [PubMed] [Google Scholar]
- Hutchinson PL, Mahlalela X. Utilization of voluntary counseling and testing services in the eastern cape, South Africa. AIDS Care. 2006;18(5):446–455. doi: 10.1080/09540120500213511. [DOI] [PubMed] [Google Scholar]
- Hutchinson PL, Mahlalela X, Yukich J. Mass media, stigma, and disclosure of HIV test results: multilevel analysis in the eastern cape, South Africa. AIDS Education and Prevention. 2007;19(6):489–510. doi: 10.1521/aeap.2007.19.6.489. [DOI] [PubMed] [Google Scholar]
- Jorsekog KG, Moustaki I. Factor analysis of ordinal variables: a comparison of three approaches. Multivariate Behavioral Research. 2001;36(3):347–387. doi: 10.1207/S15327906347-387. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sexually Transmitted Infections. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the internalized AIDS-related stigma scale. AIDS Care. 2009;21(1):87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behavior. 2005;9(2):135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- Khumalo-Sakutukwa G, Morin SF, Fritz K, Charlebois ED, Van Rooyen H, Chingono A, et al. Project Accept (HPTN 043): a community-based intervention to reduce HIV incidence in populations at risk for HIV in Sub-Saharan Africa and Thailand. Journal of the Acquired Immune Deficiency Syndrome. 2008;49(4):422–431. doi: 10.1097/QAI.0b013e31818a6cb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohi TW, Makoae L, Chirwa M, Holzemer WL, Phetlhu DR, Uys L, et al. HIV and AIDS stigma violates human rights in five African countries. Nursing Ethics. 2006;13(4):404–415. doi: 10.1191/0969733006ne865oa. [DOI] [PubMed] [Google Scholar]
- Ma W, Detels R, Feng Y, Wu Z, Shen L, Li Y, et al. Acceptance of and barriers to voluntary HIV counselling and testing among adults in Guizhou province, China. AIDS. 2007;21(Suppl. 8):S129–S135. doi: 10.1097/01.aids.0000304708.64294.3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl. 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maluwa M, Aggleton P, Parker R. HIV- and AIDS-related stigma, discrimination, and human rights: a critical overview. Health and Human Rights. 2002;6(1):1–18. [Google Scholar]
- Maman S, et al. A comparison of HIV stigma and discrimination in five international sites: the influence of care and treatment resources in high prevalence settings. Social Science & Medicine. doi: 10.1016/j.socscimed.2009.04.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre J, de Bruyn G, Gray G. Southern Africa. In: Celentano DD, Beyer C, editors. Public health aspects of HIV/AIDS in low and middle income countries. New York: Springer; 2008. pp. 289–330. [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers, and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bulletin of the World Health Organization. 2004;82(4):299–307. [PMC free article] [PubMed] [Google Scholar]
- Muthen B, Kaplan D. A comparison of some methodologies for the factor analysis of non-normal likert variables. British Journal of Mathematical and Statistical Psychology. 1985;38:171–189. [Google Scholar]
- Muthen BO. A general structural equation model with dichotomous, ordered categorical and continuous latent indicators. Psychometrika. 1984;49:115–132. [Google Scholar]
- Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychology, Health & Medicine. 2006;11(3):335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. American Journal of Public Health. 2007;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Social Science & Medicine. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, Michaelis AP, Lippman SA, Chinaglia M, Diaz J. HIV-related stigma, service utilization, and status disclosure among truck drivers crossing the southern borders in Brazil. AIDS Care. 2008;20(7):764–770. doi: 10.1080/09540120701506796. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R Foundation for Statistical Computing; Vienna, Austria: 2008. R: A Language and Environment for Statistical Computing. http://www.R-project.org. [Google Scholar]
- Reidpath DD, Brijnath B, Chan KY. An Asia Pacific six-country study on HIV-related discrimination: introduction. AIDS Care. 2005;17(Suppl. 2):S117–S127. doi: 10.1080/09540120500120195. [DOI] [PubMed] [Google Scholar]
- Stoneburner RL, Low-Beer D. Population-level HIV declines and behavioral risk avoidance in Uganda. Science. 2004;304(5671):714–718. doi: 10.1126/science.1093166. [DOI] [PubMed] [Google Scholar]
- Thomas BE, Rehman F, Suryanarayanan D, Josephine K, Dilip M, Dorairaj VS, et al. How stigmatizing is stigma in the life of people living with HIV: a study on HIV positive individuals from Chennai, south India. AIDS Care. 2005;17(7):795–801. doi: 10.1080/09540120500099936. [DOI] [PubMed] [Google Scholar]
- Turan JM, Miller S, Bukusi EA, Sande J, Cohen CR. HIV/AIDS and maternity care in Kenya: how fears of stigma and discrimination affect uptake and provision of labor and delivery services. AIDS Care. 2008;20(8):938–945. doi: 10.1080/09540120701767224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Brakel WH. Measuring health-related stigma – a literature review. Psychology, Health & Medicine. 2006;11(3):307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- Weiss MG, Ramakrishna J, Somma D. Health-related stigma: rethinking concepts and interventions. Psychology, Health & Medicine. 2006;11(3):277–287. doi: 10.1080/13548500600595053. [DOI] [PubMed] [Google Scholar]
- Wolfe WR, Weiser SD, Leiter K, Steward WT, Percy-de Korte F, Phaladze N, et al. The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. American Journal of Public Health. 2008;98(10):1865–1871. doi: 10.2105/AJPH.2007.122044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Progress on global access to HIV antiretroviral therapy: An update on “3-by-5”. World Health Organization; 2005. [Google Scholar]