Abstract
This study documents the mortality, chronic morbidity and physical functioning experiences of U.S. Hispanics, non-Hispanic whites, and non-Hispanic blacks 50 years of age and older in the United States. Hispanics are classified by nativity to better assess an important source of heterogeneity in population health within that population. Drawing on mortality and morbidity data from the National Health Interview Survey, demographic models of healthy life expectancy are used to derive estimates of life expectancy, life expectancy with and without chronic morbidity conditions, and life expectancy with and without functional limitations. The results not only highlight the mortality advantages of foreign-born Hispanics, but also document their health advantages in terms of morbidity and physical functioning beyond age 50. Nativity is a highly important factor differentiating the health and mortality experiences of Hispanics: U.S.-born Hispanics have a health profile more indicative of their minority status while foreign-born Hispanics have much more favorable mortality and health profiles. Differences in smoking across racial/ethnic/nativity groups is suggested as an important reason behind the apparent health advantages of foreign-born Hispanics relative to whites as well as relative to their U.S.-born counterparts.
Keywords: Hispanic health paradox, smoking, functional limitations, chronic morbidity, nativity
Overview
This study documents the mortality, physical functioning, and chronic disease morbidity experiences of Hispanics, non-Hispanic whites, and non-Hispanic blacks 50 years of age and older in the United States in order to examine the role of health status in addition to longevity in the Hispanic paradox. Foreign-born Hispanics are differentiated from U.S.-born Hispanics to better assess the role of nativity as a source of heterogeneity in the health and mortality of the U.S. Hispanic population. We also take into account racial/ethnic/nativity differences in smoking behavior, since recent evidence points to the importance of these differences for the surprisingly low levels of mortality among older Hispanics compared to U.S.-born whites (Blue and Fenelon 2011). Demographic models are used to investigate whether the Hispanic paradox in mortality (i.e., relatively lengthy life expectancy) extends to other important health domains. These models are used to generate estimates of total life expectancy at age 50, life expectancy with and without physical functioning problems at age 50, and life expectancy with and without major chronic disease morbidity at age 50. Measures of physical functioning and chronic disease morbidity allow us to capture more innate forms of morbidity (i.e., health problems arising from within individuals, such as disease or physiological capacity), which are important in assessing whether racial/ethnic differences in mortality (e.g., life expectancy) are mirrored in differences in morbidity experiences (healthy life expectancy). These life tables will significantly expand what is known about how morbidity for racial/ethnic groups combines with their mortality to produce racial/ethnic differences in healthy and unhealthy life expectancy in the older American population.
Background
Growing evidence supports the idea that the Hispanic paradox among older Americans is not a methodological artifact but reflects the actual mortality experiences of Hispanics in the United States (Arias 2010; Arias et al. 2010; Eschbach, Kuo and Goodwin 2006a; Eschbach, Kuo and Goodwin 2006b; Hummer et al. 2000; Markides and Eschbach 2005, 2011; Turra and Elo 2008). Despite low levels of education and income, Hispanic mortality rates are comparable to – and often lower than – the more socioeconomically advantaged adult white population; hence, the characterization of this pattern as a paradox. This body of evidence is based on data from a variety of sources including vital registration data, Social Security Administration data, and nationally representative surveys such as the National Health Interview Survey Linked Mortality Files. Recent evidence also points to the importance of nativity in understanding this paradox. Hummer, Lariscy, and Hayward (2011), for example, reported that life expectancy at age 50 for the foreign-born Mexican American and Other Hispanic populations substantially exceeded that for U.S.-born white Americans as well as that of their U.S.-born co-ethnics. In other words, the Hispanic paradox in mortality is very much a story about nativity.
Recent evidence also suggests that Hispanics' mortality advantages relative to whites are not mirrored in their disability experience – where disability is measured in terms of health limiting various types of basic self care and social activities (Hayward et al. 2011). Markides and colleagues (2007), for example, used 2000 U.S. Census data to document the substantially higher disability rates of Hispanics aged 65 years and older, especially women, compared to non-Hispanic whites. Drawing on the Hispanic Established Population for Epidemiological Studies (HEPESE), Eschbach and colleagues (2007) also showed that foreign-born Mexican Origin adults aged 65 years and older not only had a total life expectancy that was greater than U.S.-born older Mexican Americans but they also spent more years disabled. Using the Health and Retirement Study, Hayward and colleagues (2011) recently documented that relative to other racial/ethnic groups, foreign-born Hispanics (especially women) experience a highly protracted period of lifetime disability, even though their life expectancies exceed those of U.S.-born whites. Similar to the Hispanic paradox story with regard to mortality, nativity appears to play a critical role with respect to disability, although in this case being foreign-born foretells a lengthy period at older ages beset with significant disability problems compared to all other racial/ethnic groups. From a “population health” perspective, then, foreign-born Hispanics' mortality advantage thus is potentially a double-edged sword. Extended life appears to be accompanied by extended disability. This pattern sharpens the idea that longer life is not necessarily accompanied by the compression of disability. It also raises the specter that the etiologies of mortality and disability are much less tightly coupled for foreign-born Hispanics than for other groups. Stated more bluntly, for foreign-born Hispanics “the factors that kill are not necessarily the same as those that disable.”
Disability, however, is only one aspect of health. Typically measured by limitations in activities of daily living (ADLs), disability reflects the intersection of physiological functioning or capacity combined with environmental challenges. Two individuals, for example, may have comparable physical functional abilities, but differences in environmental challenges may result in one person being disabled while the other is not. Similarly, morbidity for one person (e.g., a heart attack) may be less disabling than for another person because of differences in treatment and disease management. In the case of racial/ethnic differences in healthy and unhealthy life expectancy based on disability, it is likely that these patterns reflect both differences in chronic disease morbidity, physiological functioning and environmental challenges. A plausible hypothesis is that minority groups may encounter greater environmental challenges which then contribute in important ways to racial/ethnic differences in disability and the extent of life disabled. Compared to disability, evidence on how racial/ethnic groups differ in physiological functioning and chronic disease morbidity, however, is much less clear.
What, then, should we expect in terms of racial/ethnic differences in the years of life with and without chronic disease morbidity and physical functioning problems? Based on data from the Health and Retirement Survey (HRS), Zhang, Hayward, and Lu (Zhang, Hayward and Lu 2012) documented that foreign-born Hispanics aged 53 years and older reported lower rates of heart disease, cancer, and chronic lung disease (and higher rates of diabetes) compared with U.S.-born whites, controlling for age and sex. Heart disease, cancer, and chronic lung disease are the top three causes of death in the United States, while diabetes ranks seventh. Although racial/ethnic differentials in self-reported chronic disease morbidity are somewhat sensitive to the source of data and age group (Crimmins, Hayward and Seeman 2004), the racial/ethnic/nativity differentials identified by Zhang et al. (2012) are mirrored in U.S. cause-specific mortality data. Hummer, Lariscy, and Hayward (2011) report, for example, that mortality from heart disease, lung and other cancers, respiratory diseases, and cerebrovascular diseases are drastically lower among older foreign-born Hispanic men and women compared to U.S.-born whites. In addition, the self-reported morbidity differences reported by Zhang et al. (2012) are highly consistent with evidence of how racial/ethnic differences in lifetime smoking experience might be contributing to the Hispanic foreign-born mortality advantage (Blue and Fenelon 2011; Hummer, Lariscy, and Hayward 2011); foreign-born Hispanics are much less likely to have ever smoked than U.S.-born whites and this is especially the case among women. For example, Hummer and colleagues reported that lower levels of self-reported smoking (e.g., a greater prevalence of “never smoked”) was a major contributor to lower mortality rates for foreign-born Hispanics compared to U.S.-born whites. Elsewhere Blue and Fenelon (2011), using an indirect estimation approach, showed that a significant proportion of the difference in life expectancy (at age 50) between U.S. Hispanics and non-Hispanic whites is attributable to smoking history. These patterns suggest, therefore, that Hispanics – particularly foreign-born Hispanics – are likely to experience a relatively compressed period of life with major disease morbidity conditions – perhaps akin to that for U.S.-born whites.
The analysis below sheds light on these issues in a number of new ways. First, we offer more refined racial/ethnic differences in lifetime chronic disease morbidity, physical functioning and mortality than have heretofore been possible. As noted earlier, we estimate healthy life expectancy in terms of two types of morbidity – chronic disease morbidity and physiological functioning. These are important types of morbidity that arise within individuals and that are part of the health process that can result in death (Crimmins and Beltran-Sanchez 2010). We do so for both the foreign-born and U.S.-born Hispanic population, as well as for U.S.-born non-Hispanic whites and blacks. Second, we integrate for the first time information on how chronic morbidity, physical functioning problems, and mortality intersect to define life expectancy, and the years of life spent with and without major chronic morbidity conditions and functional problems. As noted above, prior studies have largely attended only to life expectancy and disabled life expectancy. Thus, we extend this line of inquiry to include other important domains of health. The choice to use these two types of morbidity also allows us to overcome limitations associated with disability analysis, namely the socially constructed nature of disability. By focusing on chronic disease morbidity and physical functioning, our analysis allows us to more directly align the morbidity and mortality experiences of racial/ethnic groups. Third, we introduce a simulation approach to assess racial/ethnic differentials in healthy life expectancy for a population that has never smoked. Because lifetime patterns of smoking appear to play a major role in racial/ethnic differentials in life expectancy, it is important to clarify how differences in smoking play out for differences in lifetime experiences with physical functioning and chronic disease morbidity across groups.
Data, Measures, and Approach
We integrate information on mortality incidence with information on the prevalence of physical functioning problems and chronic disease morbidity to calculate Sullivan-based multistate life table models of healthy (and unhealthy) life expectancy for the major racial/ethnic groups in the United States (Sullivan 1971). The Sullivan health expectancy reflects the current health of the population (or population subgroup) adjusted for mortality levels and independent of age structure. It is a very useful means to compare the health of population groups despite differences in age composition (Jagger et al. 2006). In this framework, total life expectancy for persons of a given age is divided into the number of years with and without a health problem – in this case, physical functioning problems or chronic disease morbidity.
Unhealthy life expectancy is an important measure of population health because it quantifies the number of years an average individual in the population is expected to manage or cope with various health problems. With respect to the question of whether Hispanic advantages in mortality carry over to functioning and chronic morbidity, we expect that the longer life expectancies of Hispanics will be mirrored in longer life expectancies free of chronic disease morbidity and physical functioning problems, and that the expected years lived with chronic disease morbidity and physical functioning problems will be compressed for Hispanics – especially foreign-born Hispanics -- relative to the other racial/ethnic groups. The integration of mortality with health in these life table models is thus a useful way to assess whether Hispanics' mortality advantages carry over to other domains of health.
Our life table results are representative of the civilian, non-institutionalized population 50 years of age and older in the United States. Hispanics are differentiated by nativity status, i.e., where a person was born. Only U.S.-born whites and blacks are considered for comparison as there are too few foreign-born whites and blacks to be included as separate groups in the analysis. Further parsing of Hispanic subgroups into, say Mexican Americans or Puerto Ricans, is also not possible given data density issues. Throughout the analysis, we stratify by sex, as it is evident that the magnitude of racial/ethnic differentials in life expectancy and lifetime health differ dramatically for men and women. We also differentiate each subpopulation by smoking status, as previous research has shown that a significant proportion of the Hispanic health advantage in life expectancy is associated with lower rates of smoking.
Data
We draw on the National Health Interview Survey as the source of all of the data used to document the racial/ethnic differentials in mortality, functional limitations and chronic morbidity conditions. We make use of the National Health Interview Survey Linked Mortality Files (NHIS-LMF) to estimate mortality incidence, while chronic morbidity and functional status are identified using the annual NHIS surveys; the NHIS-LMF provides mortality follow-up data for the annual NHIS cross-sectional surveys. Mortality follow-up in the NHIS-LMF is based primarily on a probabilistic match to National Death Index (NDI) death certificate records, although other sources (e.g., Social Security records) were also used to determine vital status. Lariscy (2011) investigated the implications of altering the match criteria to the NDI. Although the matches for foreign-born Hispanics were more sensitive to the match criteria, Hispanics' relative mortality advantages (compared to whites) remained among older adults regardless of the criteria.
Because of the need to obtain incidence and prevalence estimates for refined subgroups of the population, we pool waves across survey years. Mortality incidence is based on NHIS-LMF for the NHIS years 1990-1995 and 1997-2004, with the mortality follow up period ranging from the date of the interview until December 31 2006. We omit the 1996 NHIS wave because information is not available for smoking status in that year. Prevalence estimates for functional problems and chronic morbidity are based on NHIS cross-sectional surveys for the 1997-2006 period. The difference in observation periods for the incidence and prevalence rates stems from the need to draw on the most complete data available for mortality to obtain reliable estimates for the racial/ethnic subgroups.
Measures
Respondents' physiological functioning is assessed using the NAGI functioning items. We use a composite measure combining upper and lower body limitations. If a person reports having difficulty with one or more of 9 NAGI items (carry 10 pounds, grasp objects, reach over head, push large objects, walk up 10 steps, sit 2 hours, stand 2 hours, stoop/bend/kneel, and walk 1/4 mile), they are classified as having a functional limitation. Difficulty is defined as responding to the question “By yourself, and without the use of any special equipment, how difficult is it for you to….”; those who responded very difficult or cannot do at all are consider to have a functional limitation. We also assessed racial/ethnic differences in only lower body functional limitations but the substantive results did not differ in any appreciable way from the total composite measure.
The chronic morbidity measure we use is a composite of four different conditions: coronary heart disease, stroke, diabetes, and cancer (excluding non-melanoma skin cancer) that are highly related to the most prevalent causes of death in the United States. Respondents are asked “have you ever been told by a doctor or other health professional that you have (heart disease, diabetes, stroke, cancer)?”. Respondents reporting one or more conditions are coded as having a chronic morbidity condition.
The segment of the population who never smoked is based on the response “no” to a question asking whether they had ever smoked 100 cigarettes in their entire lifetime.
Approach
The Sullivan-based multistate life tables for each racial/ethnic group by sex depend on racial/ethnic/sex-specific age schedules of mortality incidence and the age-schedules of chronic morbidity or functional limitation prevalence. The age schedules of mortality incidence determine the calculation of the life expectancies, while the age schedules of chronic morbidity conditions or functional limitation prevalence determine the distribution of survivors at each age in the health states. The prevalence rates of health status are then used to partition the person-years lived at each age, and the healthy and unhealthy life expectancies are calculated as the sum of person-years lived in each state from that age onward divided by the number of survivors at that age (Jagger et al. 2006).
Pooled NHIS waves are used to estimate statistical models of mortality incidence and morbidity prevalence separately for men and women. For the mortality models, the log of the risk of death was estimated as function of age – a classic Gompertz mortality model – and race/ethnicity was entered as a covariate. The parameter estimates from the model were then used to calculate predicted racial/ethnic specific mortality rates (Teachman and Hayward 1993). Chronic morbidity and functional limitation prevalence rates were estimated within each racial/ethnic group where the log odds of having a chronic morbidity conditions or functional limitations were estimated as a function of age and age squared to capture non-linearities in functional form. Again, the parameter estimates from the statistical models were used to calculate predicted age-specific rates within each racial/ethnic group by sex. The age-specific mortality incidence and chronic morbidity/functional limitation prevalence rates are the inputs for the life table models.
We estimated confidence intervals for the life table models in order to formally test whether group differences in the expectancies are statistically different. We use a bootstrapping approach to derive the confidence intervals. The approach involves drawing 300 bootstrap samples on which the procedures outlined earlier (i.e., the derivation of mortality and morbidity/functional impairment prevalence) was carried out for each bootstrap sample. The bootstrap samples are generated at the primary sampling unit (PSU) level. For example, if there are k PSUs (say, ABCD) in a stratum, we draw k-1 PSU samples for the stratum “with ”replacement. Once a PSU is selected, all sampled persons in that PSU are included in the bootstrap sample and their weights are recalculated by the number of time their PSUs are selected. This approach produced 300 life tables (and expectancies) for each subgroup. The confidence intervals reported below reflect a 95% confidence interval where the upper and lower values reflect those at 2.5% in the expectancy distributions' tails.
Results
Descriptive Results
Table 1 shows the characteristics of our sample. By pooling data from multiple years of the NHIS we created a data set that has sufficient numbers of individuals and deaths in each subpopulation so that we can carry out our life table approach. Both foreign- and U.S.-born Hispanics were less likely to die during the follow-up period compared to whites; this pattern was exhibited for both men and women. Foreign-born Hispanic males and females above age 50 also have a lower prevalence of chronic morbidity and functional limitations compared to whites. Conversely, U.S.-born Hispanics have higher proportions of men and women with chronic morbidity conditions and functional limitations compared to whites. Never smoking is higher among both foreign- and U.S.-born Hispanics compared to whites. These measures of mortality and morbidity prevalence are not sufficient to adequately answer the question of whether or not the Hispanic paradox for mortality extends to morbidity and functioning, as they do not allow us to take into account mortality schedules or age differences in prevalence rates. For these reasons we next model prevalence of chronic morbidity conditions and functional limitations as quadratic functions of age by race and gender.
Table 1. Frequency and Percentages of Mortality, Chronic Morbidity Conditions, and Functional Limitations by Race/Ethnicity and Sex, Persons Aged 50 and Above in the Civilian Non-institutionalized Population.
| Native Born Whites | Native-Born Blacks | Native-Born Hispanics | Foreign-Born Hispanics | |
|---|---|---|---|---|
| Males | N=66,150 | N=9,781 | N=3,484 | N=5,063 |
|
| ||||
| Number of deaths | 11,434 | 1,939 | 417 | 424 |
| 17% | 20% | 12% | 8% | |
| Number of chronic morbidity conditions | 12,731 | 2,082 | 872 | 996 |
| 30% | 31% | 31% | 24% | |
| Number of functional limitations | 4,725 | 1,051 | 382 | 391 |
| 11% | 17% | 14% | 9% | |
| Number of never smokers | 22,039 | 3,290 | 1,358 | 2,378 |
| 33% | 34% | 39% | 47% | |
|
| ||||
| Females | N=88,293 | N=16,083 | N=4,815 | N=7,042 |
|
| ||||
| Number of deaths | 13,852 | 2,467 | 433 | 434 |
| 16% | 15% | 9% | 6% | |
| Number of chronic morbidity conditions | 14,907 | 3,417 | 1155 | 1455 |
| 27% | 33% | 31% | 25% | |
| Number of functional limitations | 10,453 | 2,598 | 848 | 968 |
| 20% | 26% | 24% | 17% | |
| Number of never smokers | 47,405 | 9,114 | 3,039 | 5,332 |
| 54% | 57% | 63% | 76% | |
The age patterning of men's chronic morbidity prevalence by race/ethnicity/nativity is shown in Figure 1a. As is evident, foreign-born Hispanic men report the lowest level of chronic morbidity for the bulk of the age range. In contrast, U.S.-born Hispanic men report quite high levels of chronic morbidity relative to foreign-born Hispanic men, higher levels compared to whites until about age 75, and similar levels compared to blacks until age 75, after which their levels diverge and U.S.-born Hispanics have a slight advantage. Overall, U.S.-born and foreign-born Hispanic men roughly bracket blacks and whites in terms of chronic morbidity prevalence. Women exhibit a somewhat similar pattern with respect to racial/ethnic differences (see Figure 1b). Moreover, the results shown for functional limitations in Figures 2a and 2b tell a similar story: foreign-born Hispanics generally have the lowest prevalence while U.S.-born Hispanics have higher levels that are in-between those of whites and blacks. At least from the standpoint of two major forms of morbidity, U.S.-born Hispanic men and women are fairly similar to blacks and highly dissimilar to foreign-born Hispanics. The morbidity patterns for foreign-born Hispanics tend to parallel those for non-Hispanic whites.
Figure 1.
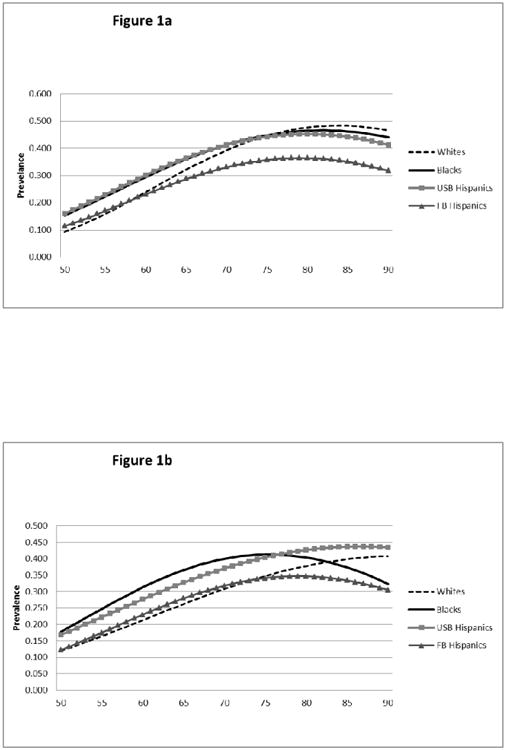
a. Chronic Morbidity Prevalence by Race/ethnicity/nativity for Men Ages 50 and Above
b. Chronic Morbidity Prevalence by Race/ethnicity/nativity for Women Ages 50 and Above
Figure 2.
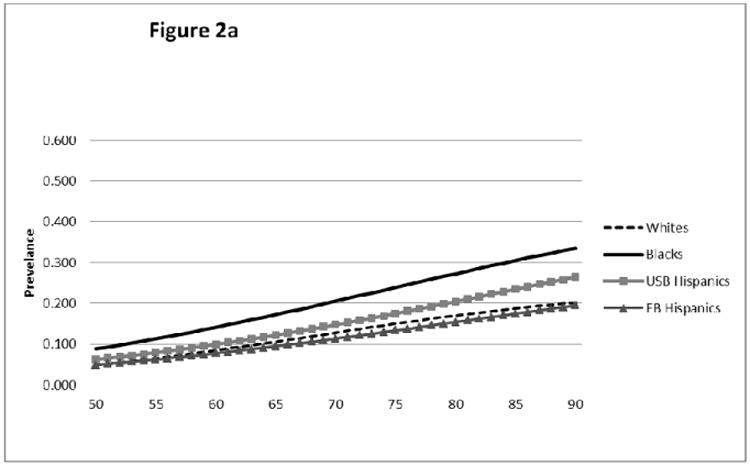
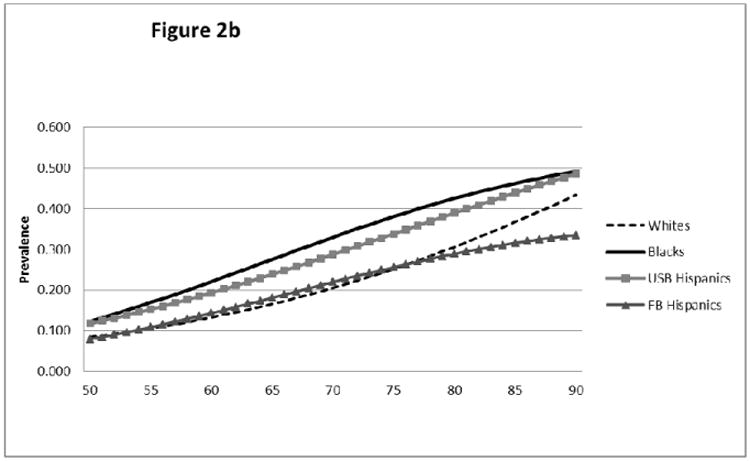
a. Functional Limitation Prevalence by Race/ethnicity/nativity for Men Ages 50 and Above
b. Functional Limitation Prevalence by Race/ethnicity/nativity for Women Ages 50 and Above
Life Table Results
As is evident in Table 2, foreign-born Hispanics have the longest estimated life expectancies at age 50: 31.67 years for men and 35.77 years for women. Foreign-born Hispanic men's life expectancy in the total population (smokers as well as never smokers) exceeds that for U.S.-born whites by about 2.8 years and is statistically significant. The gap for women in the total population is about 2.7 years and is also statistically significant. Life expectancy for U.S.-born Hispanic men and women is roughly comparable to that for whites, and black life expectancy lags significantly behind all other racial/ethnic groups. Note that these estimates differ slightly in magnitude from those reported by Hummer et al. (2011) due to differences in the years of the NHIS-LMF used to estimate mortality. However, the racial/ethnic differentials are very similar to those reported by Hummer and colleagues.
Table 2. Total Life Expectancy and Life Expectancy with and without Chronic Morbidity Conditions by Race/Ethnicity and Sex.
| Total Population | Never Smokers | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Sex | Race/Ethnicity | TLE | xMLE | MLE | TLE | xMLE | MLE |
| Male | NH Whites | 28.9 | 17.69 | 11.21 | 32.67 | 20.85 | 11.82 |
| NH Blacks | 25.57* | 15.76* | 9.81* | 28.81* | 18.95* | 9.85* | |
| NB Hispanics | 28.81 | 16.72 | 12.08 | 30.54 | 19.28 | 11.27 | |
| FB Hispanics | 31.67* | 20.52* | 11.15 | 34.11 | 22.74 | 11.38 | |
|
| |||||||
| Female | NH Whites | 33.1 | 22.33 | 10.76 | 35.59 | 24.46 | 11.13 |
| NH Blacks | 30.95* | 18.84* | 12.11* | 33.2* | 20.68* | 12.52* | |
| NB Hispanics | 33.63 | 20.4* | 13.24* | 34.85 | 21.3* | 13.55* | |
| FB Hispanics | 35.77* | 23.62* | 12.15* | 36 | 24.29 | 11.71 | |
Note: xMLE = Life expectancy without any Chronic Morbidity Conditions.
MLE = Life expectancy with one or more Chronic Morbidity Conditions.
indicates a statistically significant difference (p<0.05) from non-Hispanic whites.
The life expectancy results for never smokers reveal that while foreign-born Hispanic life expectancy continues to exceed that for whites, the gap narrows considerably – down to 1.4 years for men and only .4 years for women – and the differences are no longer statistically significant. This narrowing of the gap is due largely to the greater gains in life expectancy for whites compared to foreign-born Hispanics once smoking is controlled. In addition, although life expectancy is comparable for whites and U.S.-born Hispanics in the total population, life expectancy for whites actually exceeds that for U.S.–born Hispanics among never smokers. Among never smokers, the life expectancy difference between white men and U.S.-born Hispanics is 2.1 years; this difference is not statistically significant at the 95% level, but the confidence intervals only overlap by .02 years (not shown). The disadvantage for U.S.-born Hispanic women is considerably less, only .7 years, and does not reach a conventional level of statistical significance.
Part of the story behind the Hispanic paradox in mortality thus reflects the higher smoking rates among whites compared to foreign-born Hispanics as argued by Blue and Fenelon (2011) and Hummer and colleagues (2011). As well as narrowing the gap in life expectancy between whites and foreign-born Hispanics, controlling for smoking also increases the difference between whites and U.S.-born Hispanics. Although racial/ethnic differences in smoking are rarely discussed as a possible explanation for the paradox, our analysis falls in line with the two recent studies that show that smoking is important for understanding racial/ethnic/nativity differences in life expectancy.
Chronic Morbidity
Table 2 further shows that, in the total population, foreign-born Hispanic men and white men can expect to spend about 11.2 years with at least one chronic morbidity condition. The two groups differ, however, in their years of life without a chronic morbidity condition, with whites living 17.69 years free of chronic morbidity conditions compared to 20.52 years for foreign-born Hispanics. The difference of 2.8 years is statistically significant. U.S.-born Hispanic men live the most years with conditions – 12.1 years. Thus, although the life expectancy of U.S.-born Hispanic men is comparable to that for whites, U.S.-born Hispanics live more years with a chronic morbidity condition. When smoking is taken into account, foreign-born Hispanics and whites become more similar in their expectations of life without a morbidity condition: the difference narrows to a 1.9 year advantage for foreign-born Hispanics. The gap in life expectancy with a chronic morbidity condition for whites and foreign-born Hispanics expands to give foreign-born Hispanics a .4 fewer year advantage. In the total population and the nonsmoking population, U.S-born Hispanic men spend the highest percentage of their life with chronic morbidity conditions compared to the other groups, but the magnitude of their disadvantage is much smaller in the non-smoking population. In the total population U.S.-born Hispanics spend 42% of their life expectancy with a chronic morbidity condition compared to 39% for whites and 35% for foreign-born Hispanics. In the nonsmoking population 37% of U.S.-born Hispanic men's life expectancy is spent with a chronic morbidity condition compared to 36% for whites and 33% for foreign-born Hispanics. Interesting to note is the finding that black men spend the fewest years with a morbidity condition, but this is largely a consequence of their shorter life expectancy; the proportion of life with a morbidity condition is not significantly smaller.
For women, longer foreign-born Hispanics' life expectancy relative to whites life is equally split between the greater number of years that foreign-born Hispanics live with and without chronic morbidities; while foreign-born Hispanics live a statistically significant extra 1.3 years without a morbidity condition compared to white women, and they also live a statistically significant extra 1.4 years with a chronic morbidity condition. Again, U.S.-born Hispanic women's morbidity experience is very different than the experience for foreign-born women. U.S.-born Hispanic women live both fewer years free of a morbidity condition and more years with a morbidity condition when compared to whites and these differences are statistically significant. U.S.-born Hispanic women appear to be disadvantaged relative to foreign-born Hispanics (and whites) in their chronic morbidity experience. Looking at never smokers again highlights the important role that smoking plays in differentiating the health of Hispanics from whites. Among never smokers, the patterns of life expectancy, and life expectancy with and without chronic morbidity are highly similar for foreign-born Hispanics and whites. Moreover, U.S.-born Hispanic women who are never smokers appear to be even more disadvantaged in their mortality and morbidity experiences compared to foreign-born Hispanics and whites.
Functional Limitations
The general patterns reported above with respect to chronic morbidity in the total population also characterize racial/ethnic differences with respect to functional limitations. In the total population foreign-born Hispanic men and women live more years than whites free of functional limitations. U.S.-born Hispanics appear to be disadvantaged relative to whites and foreign-born Hispanics both in terms of the years of life free of functional limitations and more years with functional limitations.
The gains in men's life expectancy for never smokers compared to the total population are generally paralleled by gains in life free of functional limitations. The expected years of life with a functional limitation either declines somewhat when smoking is controlled or remains relatively stable. Thus, regardless of race/ethnicity, most of men's gains in life expectancy from not smoking contribute to extending life without a functional limitation. The greatest absolute gain in the expectation of life free of functional limitations is observed for white men who shift from 24.62 years of life without a functional limitation to 28.8 years – a gain of over 4 years. We observe less of a gain in the expected years free of functional limitations for foreign-born men (27.02 years in the total population compared to 29.08 years among never smokers), partly because of the already lower levels of smoking among foreign-born Hispanic men on the whole.
Note that among never smokers, U.S.-born Hispanic men's life expectancy falls between whites and blacks and that their expected years of life free of functional limitations is significantly lower than that for whites. That is also the case for blacks. To some extent among the never smoking population, U.S.-born Hispanic men appear to occupy a middle-ground between blacks and whites both with respect to mortality and the years of life free of functional limitations.
As is expected, the expected years of life with functional limitations is substantially higher among women compared to men. Gender differences in chronic morbidity expectancies described earlier were less evident. In the total population foreign-born Hispanic women have a significantly longer life expectancy without functional limitations by 1.8 years compared to whites (26.5 years for foreign-born Hispanics compared to 24.7 years for whites), but the gap is no longer significant when smoking was controlled. This is also the case with respect to the gap in life expectancy with functional limitations, when controlling for smoking. Similar to U.S.-born Hispanic men, U.S.-born Hispanic women also appear to occupy a middle ground in terms of mortality and functional limitations compared to blacks and whites. Among the never smokers, both black and U.S.-born Hispanic women's expected years free of life expectancy significantly falls below whites while their expected years of life with functional limitations are significantly higher.
Life table survival curves that link mortality, chronic morbidity conditions, and functional limitations are shown in Figure 3 (for men) and Figure 4 (for women), respectively. Curves are displayed for whites and foreign-born Hispanics – the two most advantaged groups. The curves allow us to assess age-related change in survival and healthy survival (the areas under the curves), and the differences between groups. The survival values indicate the number of persons in a life table population of 100,000 at age 50 who are alive at each age and who have no functional and chronic morbidity problems, respectively.
Figure 3.
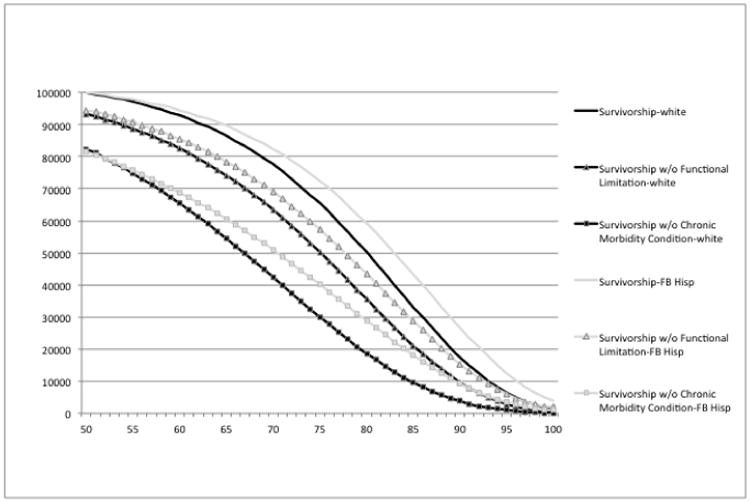
Survival with and without Chronic Morbidity Conditions and Functional Limitations Non-Hispanic Whilst and Foreign-Born Hispanies, Men, Total Population.
Figure 4.
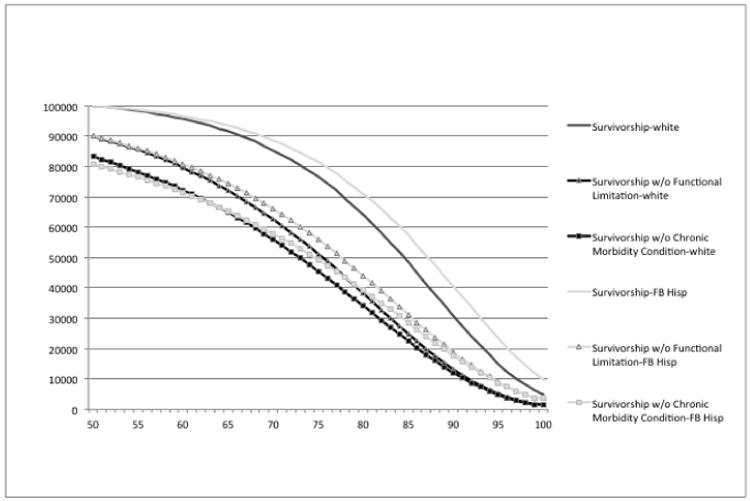
Survival with and without Chronic Morbidity Commons and Functional Limitations, Non-His-panit Whites and Foreign-Born Hispanic, Women, Total Population.
As is evident from both Figures 3 and 4, foreign-born Hispanics have a more rectangular survival curve than whites; more deaths are postponed to later ages. The same is also the case for survivorship free of functional limitations. The drop in survivorship free of chronic morbidity conditions occurs faster among whites than among foreign-born Hispanics. However, the drop is relatively linear for both groups compared to the overall survival curve and the survival curve for functional limitations. The key point is there does not appear to be a “dose-response” relationship between chronic morbidity, functioning and mortality with age for either group.
Limitations
Although the analysis advances what is known about the health and mortality of older Hispanics, Hispanics are a highly heterogenous group. The Hispanic paradox originally was conceptualized to speak to Mexican American health; however, Mexican Americans are not sufficiently represented in our data to support such an analysis at this time. The addition of more years of NHIS data, however, should permit a finer parsing of Hispanics by national origin in future studies.
In addition, it is important to acknowledge that the paradox is very likely a story about selection processes – a story that cannot be directly addressed here. At the very least, a two-stage selection process is likely at work. First, Hispanic immigrants to the United States are highly selected from the origin population – especially the birth cohorts represented in these data (Feliciano 2005). Second, there is some return migration from the United States to Mexico, for example, and these emigrants have been shown to exhibit higher mortality than foreign-born counterparts who remain in the United States (Turra and Elo 2008).
Our approach to control the effects of smoking is also limited. In essence, we have constructed a hypothetical scenario that ignores unobserved factors that might influence racial/ethnic groups' dispositions to ever smoke and which are also related to health and mortality. Thus, our analysis of never smokers in comparison to the total population should be seen as a first approximation of the effects of smoking on racial/ethnic differentials in healthy life expectancy.
Being mindful of these limitations, our analysis documents that the Hispanic paradox in mortality clearly extends to morbidity in the forms of major chronic conditions and functional limitations. However, we have not included ADL disability as part of the current analysis to see whether the paradox extends to disablement. As noted earlier, however, recent research provides evidence that the paradox does not extend to disablement (e.g., Hayward et al. 2011), and that foreign-born Hispanics – especially women – have higher disability rates across much of the older age range. Why this is so must await future research.
Conclusions
Foreign-born Hispanics' life expectancy exceeded that of whites,and, similarly, there are striking parallels in their mortality, chronic morbidity, and functioning experiences in the total population. However, U.S.-born Hispanics do not generally share the same health advantages of their foreign-born counterparts. They live fewer years, they are healthy fewer years and they live more years with chronic morbidity conditions and functional limitations.
Among never smokers, foreign-born Hispanics lose a substantial fraction of their health advantage relative to whites. The reason is that whites' higher rates of smoking takes its toll with regard to whites' mortality, chronic morbidity and functional limitations – despite whites' greater socioeconomic resources. Explanations for the Hispanic paradox have often focused on health selection, social networks, cultural factors, and the like to explain Hispanics' lower mortality, with the presumption that whites are uniformly advantaged due to greater socioeconomic resources. It is evident that whites are not uniformly advantaged when it comes to health behaviors such as smoking. Indeed, the comparable life expectancies of whites and U.S.-born Hispanics diverged among never smokers, with U.S.-born Hispanics having lower life expectancies and often worse health expectancies. The pattern for U.S.-born Hispanic never smokers was more akin to their minority status than to a “paradox”; exhibiting both lower life expectancy, fewer years of life free of health problems and more years of life with health problems compared to whites. It is evident that foreign-born and U.S.-born older Hispanics have highly divergent health experiences of a magnitude similar to the black-white gap in mortality, chronic morbidity, and functioning. Nativity, at least for the birth cohorts represented here, is an important divide in Hispanic older adults' health and mortality experiences.
The Hispanic paradox story, at least in terms of the evidence reported here, is not simply a story about mortality, but it also is a story about the morbidity process encompassing important chronic diseases and physiological capacity from which death arises. These results stand in contrast to those studies suggesting that the Hispanic paradox may not extend to disablement. It is unclear from available evidence why this is the case, but one possibility is that the factors giving rise to low rates of chronic disease, functional impairment, and mortality among foreign-born Hispanics may differ from those factors giving rise to disability. Typically, researchers often assume shared etiologies, but at least in the case of foreign-born Hispanics, this may not be the case. In particular, the types of work in which foreign-born Hispanics are employed may be highly disabling in terms of musceloskeletal impairments, but less harmful or even potentially beneficial in terms of morbidity and longevity. In addition, the types of environmental factors that contribute to making functional problems disabling may be more prevalent or have a greater impact among foreign-born Hispanics compared to other groups. These issues warrant careful attention in future research.
Even though smoking was implicated in this study and other recent research as an important explanation for the Hispanic paradox, it is important to note that even among never smokers in this study, foreign-born Hispanics still remain highly comparable to whites in terms of life expectancy and healthy life expectancy. Thus, the reasons for the Hispanic paradox should be seen as multifactorial and not simply due to smoking differences. Health selection processes – though unobserved here – very likely play important roles. Older Hispanic immigrants are highly select compared to the origin population, and it is likely that unhealthy migrants may return to their countries of origin throughout the adult age range (not simply the age range considered in this analysis). In addition, dietary practices, social relationships, and even intergenerational transfers from offspring to elders may also be consequential for the health of older foreign-born Hispanics. The relative importance of these types of selection processes and exposures as explanations for the Hispanic paradox will undoubtedly attract considerable attention in future research as better data on the United States' largest minority group becomes available.
Table 3. Total Life Expectancy and Life Expectancy with and without Functional Limitations by Race/Ethnicity and Sex.
| Total Population | Never Smokers | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Sex | Race | TLE | xFLE | FLE | TLE | xFLE | FLE |
| Male | NH Whites | 28.9 | 24.62 | 4.28 | 32.67 | 28.8 | 3.87 |
| NH Blacks | 25.57* | 20.22* | 5.34* | 28.81* | 23.44* | 5.36* | |
| NB Hispanics | 28.81 | 23.32* | 5.49* | 30.54 | 25.52* | 5.02 | |
| FB Hispanics | 31.67* | 27.02* | 4.65 | 34.11 | 29.08 | 5.03 | |
|
| |||||||
| Female | NH Whites | 33.1 | 24.68 | 8.41 | 35.59 | 27.14 | 8.45 |
| NH Blacks | 30.95* | 20.28* | 10.67* | 33.2* | 22.17* | 11.04* | |
| NB Hispanics | 33.63 | 22.65* | 10.99* | 34.85 | 24.17* | 10.68* | |
| FB Hispanics | 35.77* | 26.5* | 9.27 | 36 | 27.06 | 8.94 | |
Note: xFLE = Life expectancy without any Functional Limitations.
FLE = Life expectancy with one or more Function Limitations.
indicates a statistically significant difference (p<0.05) from non-Hispanic whites.
Acknowledgments
Funding for this research was provided by the MacArthur Foundation Research Network on an Aging Society: John W. Rowe, Columbia University (Chair). This research has received support from the grant, 5 T32 HD007081, Training Program in Population Studies, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development and from grant, 5 R24 HD042849, Population Research Center, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. We would like to thank the members of the Population Health Lab at the Population Research Center for their helpful comments and suggestions.
References
- Arias E. In: United States Life Tables by Hispanic Origin. Statistics VaH., editor. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- Arias E, Eschbach K, Schauman WS, Backlund EL, Sorlie PD. The Hispanic mortality advantage and ethnic misclassification on US death certificates. American Journal of Public Health. 2010;100(S1):171–177. doi: 10.2105/AJPH.2008.135863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blue L, Fenelon A. Explaining low mortality among US immigrants relative to native-born Americans: the role of smoking. International Journal of Epidemiology. 2011;40(3):786–793. doi: 10.1093/ije/dyr011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Hayward MD, Seeman T. Race/Ethnicity, Socioeconomic Status and Health. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Later Life. Washington, DC: National Academy Press; 2004. pp. 310–352. [PubMed] [Google Scholar]
- Eschbach K, Kuo YF, Goodwin JS. Ascertainment of Hispanic Ethnicity on California Death Certificates: Implications for the Explanation of the Hispanic Mortality Advantage. American Journal of Public Health. 2006a;96(12):2209–2215. doi: 10.2105/AJPH.2005.080721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eschbach K, Kuo YF, Goodwin JS. Ascertainment of Hispanic ethnicity on California death certificates: implications for the explanation of the Hispanic mortality advantage. American Jouurnal of Public Health. 2006b;96(12):2209–2215. doi: 10.2105/AJPH.2005.080721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eschbach K, Al-Snih S, Markides KS, Goodwin JS. Disability and Active Life Expectancy of Older U.S.-and Foreign-Born Mexican Americans. In: Angel Jacqueline L, Whitfield Keith E., editors. The Health of Aging Hispanics. New York: Springer; 2007. pp. 40–49. [Google Scholar]
- Feliciano C. Educational selectivity in US immigration: How do immigrants compare to those left behind? Demography. 2005;42(1):131–152. doi: 10.1353/dem.2005.0001. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Hummer RA, Chiu CT, Gonzalez C, Wong R. Does the Hispanic Paradox in Mortality Extend to Disability?; Presented at MacArthur Foundation Research Network on an Aging Society; Palo Alto, CA. 2011. [Google Scholar]
- Hummer RA, Lariscy JT, Hayward MD. Hispanic Adult Mortality in the United States: A Review, New Estimates, and Comparisons to Other Population Groups; Presented at MacArthur Foundation Research Network on an Aging Society; Palo Alto, CA. 2011. [Google Scholar]
- Hummer RA, Rogers RG, Amir SH, Forbes D, Frisbie WP. Adult Mortality Differentials Among Hispanic Subgroups and Non-Hispanic Whites. Social Science Quarterly. 2000;81:459–476. [PubMed] [Google Scholar]
- Jagger C, Cox B, Roy Le EHEMU. EHEMU Technical Report. Third. Sep, 2006. Health Expectancy Calculation by the Sullivan Method. [Google Scholar]
- Lariscy JT. Differential Record Linkage by Hispanic Ethnicity and Age in Linked Mortality Studies: Implications for the Epidemiologic Paradox. Journal of Aging and Health. 2011;23(8):1263–1284. doi: 10.1177/0898264311421369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, Migration, and Mortality: Current Status of Research on the Hispanic paradox. Journals of Gerontology: Social Sciences. 2005;60 Spec No 2:68–75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Hispanic Paradox in Adult Mortality in the United States. In: Rogers RG, Crimmins EM, editors. International Handbook of Adult Mortality. New York: Springer Press; 2011. pp. 227–240. [Google Scholar]
- Markides KS, Eschbach K, Ray LA, Kristen Peek M. Census Disability Rates among Older People by Race/Ethnicity and Type of Hispanic Origin. In: Angel Jacqueline L, Whitfield Keith E., editors. The Health of Aging Hispanics. New York: Springer; 2007. pp. 26–39. [Google Scholar]
- Sullivan DF. A Single Index of Mortality and Morbidity. HSMHA Health Reports. 1971;86(4):347–354. [PMC free article] [PubMed] [Google Scholar]
- Teachman JD, Hayward MD. Interpreting Hazard Rate Models. Sociological Methods and Research. 1993;21:340–371. [Google Scholar]
- Turra CM, Elo IT. The Impact of Salmon Bias on Hispanic Mortality Advantage: New Evidence from Social Security Data. Population Research and Policy Review. 2008;27(5):515–530. doi: 10.1007/s11113-008-9087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Hayward MD, Lu C. Is There a Hispanic Epidemiologic Paradox in Later Life? A Closer Look at Chronic Morbidity. Research on Aging. 2012;34:548–571. [Google Scholar]


