Abstract
Lichen planus pigmentosus (LPP) is a distinct clinical entity commonly encountered in the Indian population. It is considered a variant of lichen planus (LP). A 40-year-old male presented with asymptomatic hyperpigmented macules in a segmental distribution since 10 years that were clinically and histopathologically suggestive of LPP. We propose the terminology “segmental lichen planus pigmentosus” and report this unusual presentation.
Keywords: Lichen planus pigmentosus, segmental, unusual presentation
INTRODUCTION
Lichen planus pigmentosus (LPP) is a chronic pigmentary disorder of unknown etiology. It was first described by Bhutani et al.[1] It may be diffuse, reticular, blotchy, or linear. The face, neck, upper part of back, trunk, and extremities are common sites of involvement, whereas flexural areas are infrequently involved.[2] We herein report an unusual case of LPP in a segmental distribution.
CASE REPORT
A 40-year-old male presented at our outpatient department with complaints of hyperpigmented lesions over the left side of the abdomen since 10 years. He gave no history of itching, and the lesions were relatively asymptomatic since the beginning. The lesions started over the abdomen and gradually enlarged to attain the present size. There was no history of friction prior to the onset of the lesions, and his occupation did not involve any trauma at that site. The lesion showed gradual darkening in color over the years. There was no history of any drug intake, surgical intervention in the area, history of herpes zoster, or similar complaints among the family members. Cutaneous examination revealed a unilaterally distributed well-demarcated band-like rectilinear pigmentation on the left side of the lower abdomen. There was non-scaly, non-atrophic, bluish-black pigmentation, continuous and extending from the midline below the umbilicus upto the left flank corresponding to T11 and 12 dermatomes [Figure 1]. There were no similar lesions in other parts. Examination of palms and soles, hair, nails, and mucous membranes was normal. We considered LPP, erythema dyschromicum perstans (ashy dermatosis), linear epidermal nevus, macular amyloidosis, linear lichen planus (LP), and postinflammatory hyperpigmentation (PIH) in the differential diagnosis and took an elliptical skin biopsy from a representative site.
Figure 1.

Band-like hyperpigmented confluent patch, bluish-black pigmentation continuous on the left side of the lower abdomen extending from midline below the umbilicus upto the left flank attributing to T11 and 12 dermatomes
Routine investigations were within normal limits. HIV and Venereal Disease Research Laboratory (VDRL) tests were nonreactive. Histopathological examination of the section studied under hematoxylin and eosin staining showed epidermis with hyperkeratosis, extensive vacuolar change, and basal cell degeneration. There was melanin incontinence with numerous melanophages and perivascular and periadnexal chronic inflammation [Figure 2]. There was no deposition of amyloid-like substance. These histopathological findings were suggestive of LPP, and a final diagnosis of segmental pattern of LPP was made.
Figure 2.
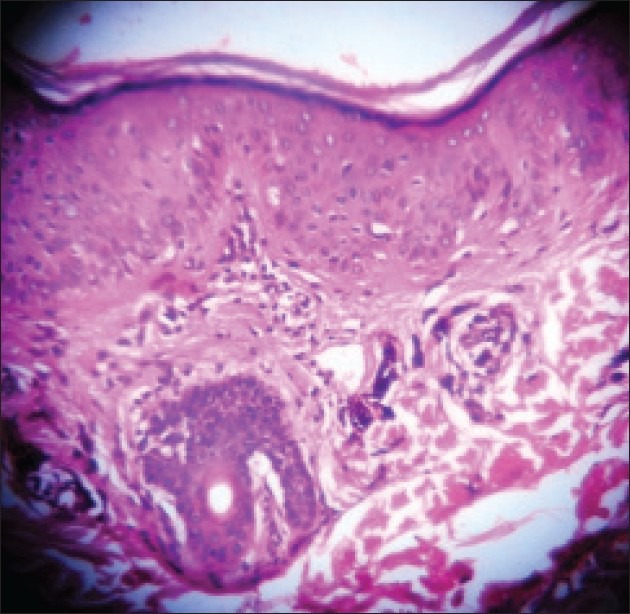
Histopathological examination of the section showed epidermis with hyperkeratosis, extensive vacuolar change, and basal cell degeneration. There was melanin incontinence with numerous melanophages and perivascular and periadnexal chronic inflammation (H and E, ×10)
The patient was counseled regarding the disease nature, and the prognosis was explained. He was advised topical mometasone and tacrolimus ointments for four weeks initially, followed by hydroquinone cream for lightening the pigmentation. The lesions responded well with significant pigment reduction.
DISCUSSION
LPP, first described by Bhutani et al.[1] is a fairly frequently encountered disorder of hyperpigmentation in Indians. Although initially described in Indians, this disorder has subsequently been seen in other racial and ethnic groups.[2,3] Several pigmentary disorders with similar features have been reported in the literature under various names such as ashy dermatosis,[4] erythema dyschromicum perstans,[5] lichen pigmentosus, and “lichen invisible pigmentogene,”[6] with some clinical overlap.[7,8,9,10,11] LPP differs clinically from classical LP by exhibiting dark brown macules and/or papules and a longer clinical course without pruritus, scalp, nail, or mucosal involvement. LPP is most common over the sun-exposed areas such as the face, neck, and flexural folds including the axillary, inguinal, and submammary regions.[1,2,3] Rarely, involvement can be generalized. Palms, soles, and nails are not affected, and involvement of the oral mucosa is infrequent. The disease is insidious in onset and has a chronic course. The patient may continue to develop new lesions, whereas old ones enlarge with gradual extension in size and deepening in color. Although lesions are generally asymptomatic, mild pruritus and burning sensation are present in about one-third of the patients. In an earlier reported series, pruritus was present in 50% to 62%[1,4] of the patients. Less common presentations include a zosteriform pattern on the trunk and involvement of unexposed areas such as the thigh.[9,10] In the Korean dermatologic literature, Hong and colleagues reported two cases of LPP presenting with a linear pattern over the extremities.[8] They presumed that the linearity of the lesions was probably related to Blaschko's lines, which suggests that predisposition to LPP might be determined during embryogenesis. In our case, the lesion did not follow the typical Blaschko's lines over the abdomen to consider it as a linear variety nor did it fulfill a characteristic zosteriform/dermatomal presentation involving the complete left half of the girdle, as the lesion involved only the left half of the abdomen involving the T11 and 12 segments extending up to the flank and sparing the posterior half. Hence, we propose the term segmental LPP and report this as a rare presentation. The etiology of LPP is not clear. No definite precipitating factors could be identified in the literature in any of the patients with LPP. Fragrances present in commercially available preparations could possibly precipitate LPP. Considering this and the fact that sun-exposed sites are frequently the first to be involved, sunlight probably plays a role in inciting LPP.[3] Further studies are required to ascertain the etiological factors.
The histopathological changes consist of vacuolar degeneration of the basal layer in the epidermis. In the dermis, a perivascular lymphohistiocytic infiltrate and the presence of melanophages are the predominant changes noted. LPP thus follows the typical changes seen in LP, but with thinning of the epidermis. A band-like infiltrate of lymphocytes is usually found at the dermo epidermal junction. Other salient features include hyperkeratosis, wedge-shaped hypergranulosis, acanthosis with saw-toothed rete ridges, and vacuolar degeneration of the basal layer. Civatte bodies (colloid or cytoid bodies) may be present at the dermal–epidermal junction and in the papillary dermis. The presence of these findings in skin biopsies suggests that LPP probably represents a lichenoid reaction to an unknown agent or stimulus and that a histopathological similarity exists between LPP and LP.[1,2,3] In PIH, the histological features include basket-weave horn, slight effacement of the rete ridge pattern, papillary dermis thickened by fibrosis, sparse superficial perivascular lymphohistiocytic infiltrate, and many melanophages in the papillary dermis.[1,2,3]
LPP is an uncommon variant of LP, for which no effective treatment is available. In the literature, tacrolimus ointment is suggested to have a beneficial role in the treatment of LPP.[11] The treatment of facial LPP includes the removal of aggravating factors, vigorous photoprotection, and some form of active pigment reduction. Topical agents include hydroquinone, which is the most commonly used agent, often in combination with retinoic acid, corticosteroids, azelaic acid, kojic acid, and glycolic acid.[3,11] Our patient was placed on topical mometasone and tacrolimus ointments initially, and got scant improvement of the symptoms at one month of follow-up. Upon application of hydroquinone cream for another month, there was significant reduction in the pigmentation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Bhutani LK, Bedi TR, Pandhi RK, Nayak NC. Lichen planus pigmentosus. Dermatologica. 1974;149:43–50. doi: 10.1159/000251470. [DOI] [PubMed] [Google Scholar]
- 2.Kanwar AJ, Kaur S. Lichen planus pigmentosus. J Am Acad Dermatol. 1989;21:815. doi: 10.1016/s0190-9622(89)80291-9. [DOI] [PubMed] [Google Scholar]
- 3.Kanwar AJ, Dogra S, Handa S, Parsad D, Radotra BD. A study of 124 Indian patients with lichen planus pigmentosus. Clin Exp Dermatol. 2003;28:481–5. doi: 10.1046/j.1365-2230.2003.01367.x. [DOI] [PubMed] [Google Scholar]
- 4.Vega ME, Waxtein L, Arenas R, Hojyo T, Dominguez-Soto L. Ashy dermatosis versus lichen planus pigmentosus: A controversial matter. Int J Dermatol. 1992;31:87–8. doi: 10.1111/j.1365-4362.1992.tb03242.x. [DOI] [PubMed] [Google Scholar]
- 5.Berger RS, Hayes TJ, Dixon SL. Erythema dyschromicum perstans and lichen planus. Are they related? J Am Acad Dermatol. 1989;21:438–42. doi: 10.1016/s0190-9622(89)80055-6. [DOI] [PubMed] [Google Scholar]
- 6.Gougerot MH. Lichen atypiques invisible pigmentogenes. Bull Soc Dermatol Syphiligr. 1935;42:894–8. [Google Scholar]
- 7.Jung YJ, Lee YH, Lee SY, Lee WS. A Case of Lichen Planus Pigmentosus-inversus in a Korean Patient. Ann Dermatol. 2011;23:61–3. doi: 10.5021/ad.2011.23.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong S, Shin JH, Kang HY. Two cases of lichen planus pigmentosus presenting with a linear pattern. J Korean Med Sci. 2004;19:152–4. doi: 10.3346/jkms.2004.19.1.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho S, Whang KK. Lichen planus pigmentosus presenting in zosteriform pattern. J Dermatol. 1997;24:193–7. doi: 10.1111/j.1346-8138.1997.tb02771.x. [DOI] [PubMed] [Google Scholar]
- 10.Kim KJ, Bae GY, Choi JH, Sung KJ, Moon KC, Koh JK. A case of localized lichen planus pigmentosus on the thigh. J Dermatol. 2002;29:242–3. doi: 10.1111/j.1346-8138.2002.tb00258.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Mutairi N, El-Khalawany M. Clinicopathological characteristics of lichen planus pigmentosus and its response to tacrolimus ointment: An open label, non-randomized, prospective study. J Eur Acad Dermatol Venereol. 2010;24:535–40. doi: 10.1111/j.1468-3083.2009.03460.x. [DOI] [PubMed] [Google Scholar]


