Abstract
Pseudoxanthoma elasticum (PXE) is an inherited disorder characterized by generalized fragmentation and progressive calcification of elastic tissue. We report two sporadic cases of PXE, both of whom presented with asymptomatic yellowish papules over the flexural sites for cosmetic reasons. Histopathological findings on hematoxylin and eosin and Verhoeff-Van Gieson (VVG) staining were classical of PXE. In addition to this, renal calcification was documented on plain radiography of kidneys, ureters, and bladder (KUB) in both the cases. Paucity of literature describing the association of nephrocalcinosis with PXE prompted the present report.
Keywords: Association, nephrocalcinosis, pseudoxanthoma elasticum
INTRODUCTION
PXE affects the connective tissue of the skin, eyes, and cardiovascular system. Many cases appear to be sporadic. In familial cases, both a recessive and dominant inheritance pattern have been reported, with the recessive form apparently being more common.[1] Lung involvement is seen, but rarely. Involvement of urinary tract in the form of asymptomatic nephrocalcinosis and bilateral obstructive uropathy with resultant frank hematuria or azotemia is an extremely rare presentation. We hereby, report two such cases of PXE and asymptomatic nephrocalcinosis.
CASE REPORTS
Case 1
A 35-year-old woman presented with a 20-year history of an asymptomatic eruption over her neck [Figures 1a and b]. She did not give any history of prominent exposure to sunlight. Physical examination revealed multiple firm, round to oval, yellow-colored, non-follicular papules, 2-5 mm in diameter, coalescing into plaques. In addition to this, skin laxity was noted. Routine laboratory investigations including serum calcium were within normal limits. Electrocardiography (ECG) and radiography of the chest were normal. Ophthalmic examination did not reveal any abnormality. There was no family history of similar lesions among first-degree relatives.
Figure 1.
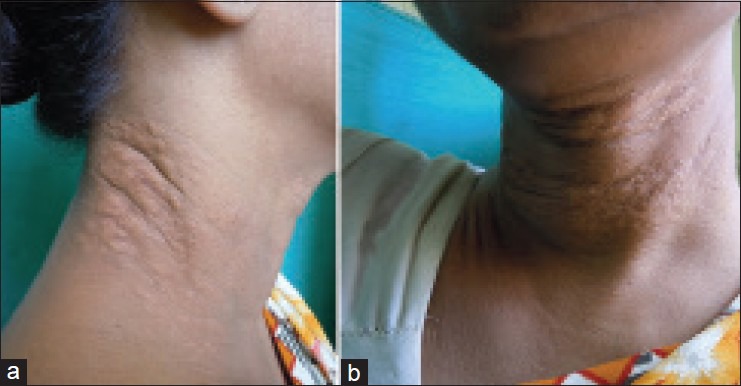
(a and b) Yellow-colored papules coalescing into plaques on the neck in case 1
Case 2
A 27-year-old female presented with a non-pruritic eruption over her neck since eight years. Onset of the eruption was insidious, commencing over the sides of the neck with an alteration in texture [Figures 2a and b]. It was not preceded by trauma or any constitutional symptoms. Her family history was not contributory. Her systemic examination was unremarkable; blood pressure and other vital signs were normal. Cutaneous examination revealed numerous yellowish papules symmetrically distributed over the front and sides of the neck. The skin over the area was soft, lax, and wrinkled. Ocular examination did not reveal any abnormality. The routine hemogram and biochemical parameters including serum calcium, chest X-ray, and ECG were also normal.
Figure 2.

(a and b) Numerous yellowish papules distributed over the neck in case 2
Plain X-ray KUB in the first case revealed three well-defined rounded and oval-shaped radio-opacities in the right renal region, suggestive of renal calculi [Figure 3a]. In the second case, straight X-ray KUB revealed a single, well-defined, rounded radio-opacity in the left renal region, suggestive of a renal calculus [Figure 3b].
Figure 3.

(a) Straight X-ray showing three well-defined rounded and oval-shaped radio-opacities in the right renal region in case 1, (b) A single well-defined rounded radio-opacity in the left renal region in case 2
In both the cases, examination of a skin biopsy specimen from neck, stained with hematoxylin and eosin and Verhoeff-Van Gieson (VVG) stains showed fragmented and calcified elastic fibers in the mid-dermis [Figures 4 and 5].
Figure 4.
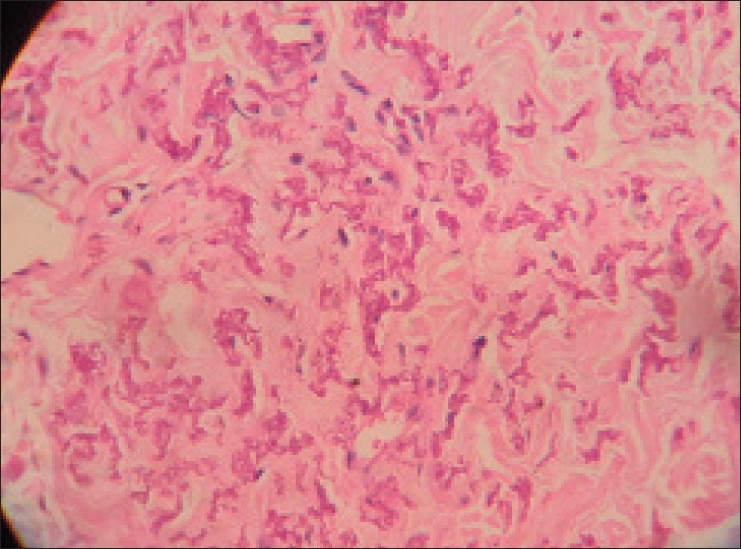
Fragmented, irregularly clumped, and calcified elastic fibers in the mid-dermis (H and E, ×40)
Figure 5.
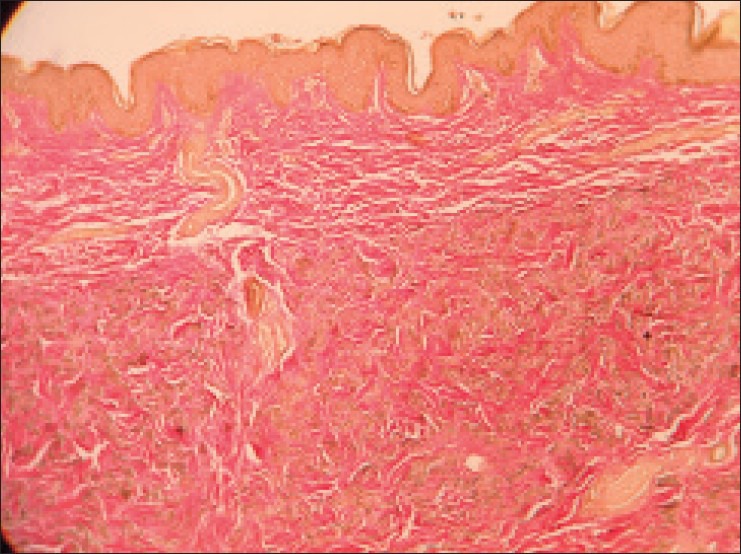
Altered and crumpled elastic fibers in the mid dermis (Verhoeff-van Gieson stain, ×10)
DISCUSSION
The skin manifestations of pseudoxanthoma elasticum (PXE) in association with elastic degeneration of the skin and heart were first described by French dermatologist Balzer in 1884. Inactivating mutations in the ABCC6 gene on the short arm of chromosome 16 can be identified in a majority of patients with PXE. Cutaneous manifestations include discrete, flat, and yellowish papules in the flexural areas, most commonly during the first or second decade of life. Usually, the lateral neck is the first affected site, as was recorded in both of our cases. These papules coalesce to form cobblestone-like plaques, giving rise to a ‘plucked chicken skin’ appearance. Other sites such as the antecubital and popliteal fossae, wrists, axillae, and groin become affected with time. Advanced disease is characterized by significant calcium deposits presenting as firm papules or plaques, occasionally extruding from the skin as ‘perforating PXE’.
The cutaneous features may lead to cosmetic concern among patients, but do not interfere with normal activities. Ophthalmic complications characterized by the presence of angioid streaks are often quite disabling. These may be detected as early as in the first decade of life. After the age of 30, their prevalence approaches 100%,[2] but these were not demonstrable in both the cases in our report.
Progressive calcification of the elastic media and intima of the medium vessels of extremities leads to the formation of atheromatous plaques,[3] resulting in intermittent claudication, loss of peripheral pulses, renovascular hypertension, angina pectoris, and myocardial infarction at a much younger age than in the unaffected population.
Cases with involvement of other systems have occasionally been reported, including urinary tract and pulmonary tissues. The mortality and morbidity of PXE is dependent on the extent of extracutaneous involvement, especially the extent of vascular disease. Fabre et al., reported the case of a 42-year-old man with PXE and recurrent bilateral nephrolithiasis in 2005.[4] Bari et al., reported a case of azotemia secondary to acute bilateral obstructive uropathy in 2007. Upon successful management, he was found to have full-blown skin and eye manifestations of PXE and was evaluated thoroughly regarding extent and potential systemic complications of PXE.[5] It is thus quite evident that chances of involvement of renal system should be kept in mind while evaluating a case of PXE.
Histologic examination of the involved skin and orcein or VVG stain shows accumulation of black-staining swollen and irregularly clumped fibers staining like elastic fibers in the middle and lower third of the dermis. Normally, elastic fibers do not stain with routine stains such as hematoxylin and eosin, but the altered elastic fibers in PXE stain faintly basophilic because of their imbibition of calcium. Von Kossa staining for calcium also shows these fibers well.[6]
A multidisciplinary approach involving dermatologists, ophthalmologists, and cardiovascular specialists is required for the management of PXE. Reconstructive surgery is advocated if sagging of skin is very prominent. Ophthalmologic care includes regular funduscopy, regular use of an Amsler grid, and prevention of retinal hemorrhage through avoidance of any inciting factor. A healthy diet and exercise regimen are key components to minimizing the extent of the cardiovascular disease. Anticoagulant medications should be avoided.
Our cases were noteworthy in terms of association of PXE with nephrocalcinosis. There are increasing reports of diffuse visceral calcifications in PXE and the literature contains reports of association with mammary and testicular calcifications.[7] To our knowledge, the association of nephrocalcinosis and PXE has been described in very few patients in the literature. The question is whether this association is entirely a chance finding or if it in fact constitutes an infrequent manifestation of PXE, is yet to be elucidated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.James WD, Berger TG, Elston DM. 11th ed. Canada: Saunders Elsevier Publications; 2011. Andrew's Diseases of the Skin: Clinical Dermatology; pp. 499–500. [Google Scholar]
- 2.Neldner KH. Pseudoxanthoma elasticum. Clin Dermatol. 1988;6:1–159. doi: 10.1016/0738-081x(88)90003-x. [DOI] [PubMed] [Google Scholar]
- 3.Goodman RM, Smith EW, Paton D, Bergman RA, Siegel CL, Ottesen OE, et al. Pseudoxanthoma elasticum: A clinical and histopathological study. Medicine (Baltimore) 1963;42:297–334. [PubMed] [Google Scholar]
- 4.Fabre B, Bayle P, Bazex J, Durand D, Lamant L, Chassaing N. Pseudoxanthoma elasticum and nephrolithiasis. J Eur Acad Dermatol Venereol. 2005;19:212–5. doi: 10.1111/j.1468-3083.2005.01007.x. [DOI] [PubMed] [Google Scholar]
- 5.Bari AU, Haq IU, Rani M, Nadeem A, Taj MA. Pseudoxanthoma elasticum and nephrolithiasis: A rare association. J Coll Physicians Surg Pak. 2007;17:686–8. [PubMed] [Google Scholar]
- 6.Johnson BL, Yan AC., Jr . Congenital Diseases (Genodermatoses) In: Elder DE, Elenitsas R, Johnson BL, editors. Lever's Histopathology of Skin. 10th ed. Philadelphia: Lippincott Williams and Wilkins publishers; 2009. pp. 152–4. [Google Scholar]
- 7.Chraïbi R, Ismaili N, Belgnaoui F, Akallal N, Bouhllab J, Senouci K, et al. Pseudoxanthoma elasticum and nephrocalcinosis. Ann Dermatol Venereol. 2007;134:764–6. doi: 10.1016/s0151-9638(07)92534-x. [DOI] [PubMed] [Google Scholar]


