Sir,
Granuloma annulare is a benign, self-limiting, necrobiotic disorder of unknown etiology. The clinical variants are localized, generalized, perforating, and subcutaneous patterns.[1] Histopathologic features comprise granulomatous inflammation in a palisaded or interstitial pattern associated with varying degrees of connective tissue degeneration and mucin deposition. Generalized granuloma annulare is a rare variant comprising 8%-15% of all cases of granuloma annulare. It presents as widespread papules some of which may coalesce to form small annular plaques. Lesions may be skin colored, pink, violaceous, tan, or yellow. Unlike in localized disease, the trunk is frequently involved, in addition to the neck and extremities. It runs a protracted course.[2] Various types of trauma, including that of a biopsy, have been observed to initiate resolution of lesions.[3]
A 66-year-old man presented with progressive, asymptomatic papular eruption since 5 years. The patient was in good health and denied any recent illness or ingestion of medications. He gave history of similar lesions 20 years ago that persisted for more than 8 years and resolved after medication. The nature of medication is not known. There was no history of diabetes mellitus. On examination, scattered multiple papules ranging in size from 0.5 to 1.0 cm were noted [Figure 1]; papules were distributed throughout the body, with sparing of face. They were very dense over thighs and arms.
Figure 1.

Multiple papules on the forearm
Initial laboratory examination revealed the following normal or negative results; complete blood cell count, erythrocyte sedimentation rate, liver and renal function tests, urinalysis, random blood sugar, anti-HIV and chest X-ray. A clinical differential diagnoses of eruptive syringoma, eruptive xanthoma, and disseminated granuloma annulare were considered. A 4 mm punch biopsy was obtained from the lesion on the side of the trunk, which showed microscopic features of granuloma annulare. When the patient returned for follow-up 4 weeks later, the lesions throughout the body had completely resolved [Figure 2]. No additional treatment was recommended, and the patient was advised to return for follow-up once again after one month. When he returned after a month, there were no lesions evident. He showed complete resolution of all lesions which were present since five years, without any treatment. After skin biopsy, we observed a dramatic improvement.
Figure 2.

Lesions resolved after biopsy
The histopathological examination revealed infiltration of histiocytes between disrupted collagen bundles and perivascular lymphocytic infiltration. There were associated mucinous changes. The findings were consistent with the interstitial variant of granuloma annulare [Figure 3].
Figure 3.
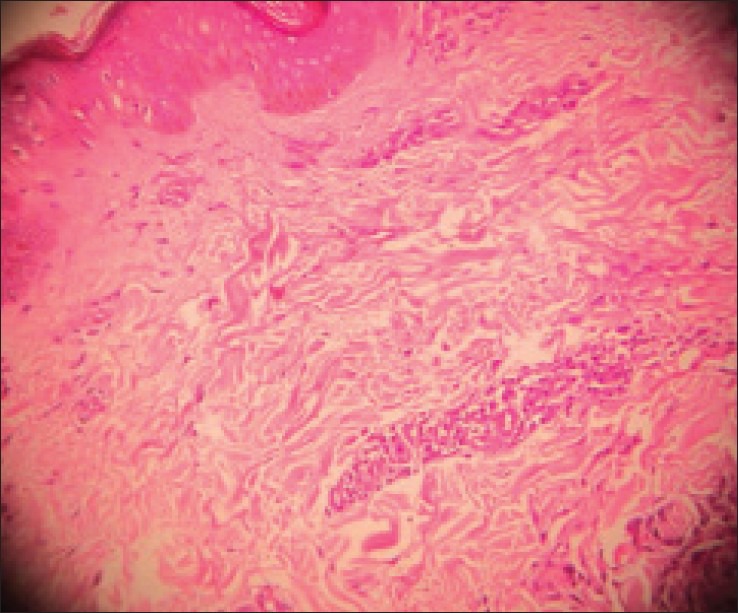
Histopathologial examination revealing infiltration of histiocytes between disrupted collagen bundles and perivascular lymphocytic infiltration. There were associated mucinous changes (H and E, ×10)
Biopsy scar mark is seen on the lateral side of the chest [Figure 4].
Figure 4.

Biopsy scar mark on the lateral part of chest
Most cases of granuloma annulare resolve spontaneously. In our patient, the lesions were present since 5 years, and resolved completely after performing biopsy. Though natural resolution is a possible mechanism, biopsy as a triggering factor for resolution cannot be ruled out.
A postal questionnaire survey was carried out by Wells and Smith.[4] Clinical notes of 280 patients suffering from granuloma annulare were examined. They found that 52 patients had biopsies with no effect on the natural course of the disease. A total of 11 biopsies were performed on the group in which the lesions were still present. Some of these patients had multiple lesions, so the fate of the particular lesion biopsied was not ascertained, but in others, the lesions biopsied had persisted.
Levin et al.,[5] noted resolution of patch type granuloma annulare at the site of biopsy. However, lesions at the unbiopsied site persisted. Histopathology revealed interstitial variant. Interestingly in our case also, biopsy findings were consistent with interstitial variant. In the present case, lesions disappeared not only at biopsy site, but also at the unbiopsied site.
Levin et al.,[5] proposed that controlled injury to the skin could alter cellular and extracellular milieu and possibly clear inflammatory process like granuloma annulare. Granuloma annulare responding to physical modalities of treatment like psoralen ultraviolet A range and cryotherapy, and the curious case of generalized granuloma annulare sparing the vaccination site[6] are cited as examples.
One hypothetical mechanism by which biopsy or other forms of wounding could trigger resolution of granuloma annulare is by initiating an orderly process of wound healing with formation of granulation tissue, remodeling of the extracellular matrix, neovascularization, and wound contraction.[5,7]
Malakar and Dhar[8] reported spontaneous resolution of vitiligo patches distant from autologous skin graft site and used the term remote reverse Koebner's phenomenon. In our case also lesions distant from the biopsied site resolved spontaneously. Further research is warranted regarding the presence of remote reverse Koebner's phenomenon in the interstitial variant of generalized granuloma annulare.
REFERENCES
- 1.Burns DA. Necrobiotic disorders. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Oxford: Wiley-Blackwell; 2010. pp. 60.5–60.7. [Google Scholar]
- 2.Prendiville JS. Granuloma annulare. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffel DJ, editors. Fitzpatrick's Dermatology in General Medicine. New York: McGraw Hill; 2008. p. 1959. [Google Scholar]
- 3.Mathai R. Necrobiotic disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. Mumbai: Bhalani Publishing House; 2010. pp. 1193–5. [Google Scholar]
- 4.Wells RS, Smith MA. The natural history of granuloma annulare. Br J Dermatol. 1963;75:199–205. [Google Scholar]
- 5.Levin NA, Patterson JW, Yao LL, Wilson BB. Resolution of patch-type granuloma annulare lesions after biopsy. J Am Acad Dermatol. 2002;46:426–9. doi: 10.1067/mjd.2002.118344. [DOI] [PubMed] [Google Scholar]
- 6.Huilgol SC, Liddell K, Black MM. Generalized granuloma annulare sparing vaccination sites. Clin Exp Dermatol. 1995;20:51–3. doi: 10.1111/j.1365-2230.1995.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 7.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738–46. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 8.Malakar S, Dhar S. Spontaneous repigmentation of vitiligo patches distant from the autologous skin graft sites: A remote reverse Koebner›s phenomenon? Dermatology. 1998;197:274. doi: 10.1159/000018013. [DOI] [PubMed] [Google Scholar]


