Abstract
Background
Low levels of total 25-hydroxyvitamin D are common among black Americans. Vitamin D–binding protein has not been considered in the assessment of vitamin D deficiency.
Methods
In the Healthy Aging in Neighborhoods of Diversity across the Life Span cohort of blacks and whites (2085 participants), we measured levels of total 25-hydroxyvitamin D, vitamin D–binding protein, and parathyroid hormone as well as bone mineral density (BMD). We genotyped study participants for two common polymorphisms in the vitamin D–binding protein gene (rs7041 and rs4588). We estimated levels of bioavailable 25-hydroxyvitamin D in homozygous participants.
Results
Mean (±SE) levels of both total 25-hydroxyvitamin D and vitamin D–binding protein were lower in blacks than in whites (total 25-hydroxyvitamin D, 15.6±0.2 ng per milliliter vs. 25.8±0.4 ng per milliliter, P<0.001; vitamin D–binding protein, 168±3 μg per milliliter vs. 337±5 μg per milliliter, P<0.001). Genetic polymorphisms independently appeared to explain 79.4% and 9.9% of the variation in levels of vitamin D–binding protein and total 25-hydroxyvitamin D, respectively. BMD was higher in blacks than in whites (1.05±0.01 g per square centimeter vs. 0.94±0.01 g per square centimeter, P<0.001). Levels of parathyroid hormone increased with decreasing levels of total or bioavailable 25-hydroxyvitamin D (P<0.001 for both relationships), yet within each quintile of parathyroid hormone concentration, blacks had significantly lower levels of total 25-hydroxyvitamin D than whites. Among homozygous participants, blacks and whites had similar levels of bioavailable 25-hydroxy vitamin D overall (2.9±0.1 ng per milliliter and 3.1±0.1 ng per milliliter, respectively; P = 0.71) and within quintiles of parathyroid hormone concentration.
Conclusions
Community-dwelling black Americans, as compared with whites, had low levels of total 25-hydroxyvitamin D and vitamin D–binding protein, resulting in similar concentrations of estimated bioavailable 25-hydroxyvitamin D. Racial differences in the prevalence of common genetic polymorphisms provide a likely explanation for this observation. (Funded by the National Institute on Aging and others.)
Low levels of total 25-hydroxyvitamin D, which are more common in black Americans than in white Americans, are associated with negative health outcomes in epidemiologic studies.1-4 Such studies are responsible for the routine clinical practice of screening for vitamin D deficiency. Among the possible effects of vitamin D deficiency, the strongest evidence is for a role in skeletal disorders,5,6 but clinical investigations of vitamin D supplementation to decrease the risk of fracture have been inconclusive.7-10
Because blacks consistently have lower levels of total 25-hydroxyvitamin D than whites, they are frequently given a diagnosis of vitamin D deficiency.11-13 Yet, as compared with whites, blacks have higher bone mineral density (BMD) and a lower risk of fragility fracture.14-16 Elevated levels of parathyroid hormone, often considered a sensitive marker of vitamin D deficiency, are more common in blacks than in whites.17 However, the relation between levels of parathyroid hormone and total 25-hydroxyvitamin D may differ in blacks and whites.18
Vitamin D–binding protein is the primary vitamin D carrier protein, binding 85 to 90% of total circulating 25-hydroxyvitamin D.19 The non– vitamin D–binding protein fraction (bioavailable 25-hydroxyvitamin D) consists primarily of albumin-bound 25-hydroxyvitamin D (10 to 15% of total 25-hydroxyvitamin D), with less than 1% of total 25-hydroxyvitamin D in the free form. Vitamin D–binding protein appears to inhibit some actions of vitamin D, because the bound fraction may be unavailable to act on target cells.20,21 Common genetic polymorphisms in the vitamin D– binding protein gene produce variant proteins that differ in their affinity for vitamin D.22,23 The prevalence of these polymorphisms differs between racial groups.24,25 Clinical assays measure the level of total 25-hydroxyvitamin D without distinguishing fractions bound to carrier proteins.
We conducted a study to determine whether vitamin D–binding protein genotypes and concentrations of circulating vitamin D–binding protein differ between black Americans and white Americans, possibly accounting for observed racial differences in manifestations of vitamin D deficiency.
Methods
Study Population
Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) is a population-based cohort study involving 3720 participants that is supported by the Intramural Research Program of the National Institute on Aging.26 Study participants, who were 30 to 64 years of age and living in Baltimore at the time of enrollment, were recruited from 13 contiguous U.S. Census tracts. Participants were randomly selected within strata based on age, race, sex, and socio-economic status; those who did not identify themselves as black or white were excluded. The institutional review board of the National Institute of Environmental Health Sciences, National Institutes of Health, approved the protocol. The Partners HealthCare Human Research Committee exempted the present study from the requirement for review. The first and last authors vouch for the accuracy of the data and analyses.
Data Collection
We used cross-sectional data from the HANDLS study that were collected between 2004 and 2008. After providing written informed consent and being interviewed, participants underwent an examination on a mobile research vehicle in which blood was sampled, height and weight were measured, and bone densitometry was performed. Dietary intake of calcium and vitamin D were determined by means of the U.S. Department of Agriculture Automated Multiple-Pass Method. Only participants who completed the examination, including bone densitometry (performed with the use of the Lunar DPX-IQ densitometer [Lunar] and restricted to participants weighing <122.5 kg [270 lb]), and who had sufficient blood samples available were included in the present study (2085 participants) (Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). BMD at the femoral neck was used in this study, given its relevance as a risk factor for hip fracture.27
Laboratory Analyses
Blood samples drawn at the examination were stored at −80°C. Levels of total 25-hydroxyvitamin D (D2 and D3) were measured with the use of tandem mass spectrometry (interassay coefficient of variation, 8.6%). Levels of vitamin D– binding protein were measured by means of a commercial enzyme-linked immunosorbent assay (R&D Systems) that uses two monoclonal antibodies in a sandwich format (interassay coefficient of variation, 7.2%). Levels of intact parathyroid hormone were measured with the use of the Elecsys Parathyroid Hormone Immunoassay (Modular Analytics E170, Roche Diagnostics) (interassay coefficient of variation, 2.5%). Calcium levels were corrected for the participant's albumin level as follows: corrected calcium = (measured calcium in mg per deciliter) + [0.8 × (4.0 − serum albumin in g per deciliter)].
Genotyping
DNA samples from the participants were genotyped for two common single-nucleotide polymorphisms (SNPs) in the coding region of the vitamin D–binding protein gene (rs4588 and rs7041) (see the Methods section in the Supplementary Appendix). These polymorphisms were chosen because of their high prevalence in the general population, their association with race, and their known link with vitamin D–binding protein function.22-25 We successfully genotyped samples from 1981 participants (95.0%).
Calculation Of Bioavailable 25-Hydroxyvitamin D
Bioavailable 25-hydroxyvitamin D was defined as circulating 25-hydroxyvitamin D not bound to vitamin D–binding protein, which is analogous to the definition of bioavailable testosterone.28 Concentrations of bioavailable 25-hydroxyvitamin D were calculated in 1025 homozygotes, for whom we could use a single genotype-specific binding affinity constant on the basis of the presence of a single vitamin D–binding protein variant (see the Methods section in the Supplementary Appendix).22 Calculated concentrations of bioavailable 25-hydroxyvitamin D were validated by direct measurement in a subgroup of homozygous participants with the use of a competitive radioligand-binding assay (see the Methods section and Fig. S2 and S3 in the Supplementary Appendix). Measured and calculated 25-hydroxyvitamin D concentrations were correlated (Pearson's r = 0.81 in 32 Gc1F homozygotes and 0.90 in 13 Gc1S homozygotes; P<0.001 for both relationships) (Fig. S4 in the Supplementary Appendix).
Statistical Analysis
The characteristics of the study participants were compared according to race with the use of t-tests or chi-square tests and are presented as means ±SE or numbers and percentages. Non-normally distributed variables were natural log–transformed for parametric testing. Adjusted means were derived from multivariable linear regression models containing terms for age, sex, body-mass index (BMI), status with respect to poverty (defined as self-reported household income of <125% of the federal poverty level in 2003), season, smoking status, and calcium intake. Microalbuminuria (defined as a urinary microalbumin-to-creatinine ratio >30 μg of microalbumin per milligram of creatinine) was included as a covariate in models predicting levels of vitamin D–binding protein and total 25-hydroxyvitamin D. Squared semi-partial correlation coefficients (expressed as percentages) are presented for multivariable linear regression models exploring variation in total 25-hydroxyvitamin D and vitamin D–binding protein. Total r2 values are presented for unadjusted models and for the overall variance explained in multivariable models.
Chi-square tests were used to compare allele frequencies according to race. Race-stratified linear regression models were used to summarize associations of levels of vitamin D–binding protein and total 25-hydroxyvitamin D with the two SNPs of interest (rs7041 and rs4588). For a subgroup of 774 samples from black participants with complete data from genomewide association studies, we created two models, one including 10 principal components from a discriminant analysis of racial groups and a second with only one covariate, percent African ancestry. Adjustment for population substructure had little effect on the model. Thus, these covariates are not included in reported results.
Participants were divided into quintiles to examine relationships between 25-hydroxyvitamin D measures and markers of vitamin D status (parathyroid hormone level, calcium level, and BMD).
Statistical analyses were conducted with the use of SAS software, version 9.2 (SAS Institute). Two-tailed P values of less than 0.05 were considered to indicate statistical significance, with the exception of the genotype analysis, in which the significance threshold was adjusted for the presence of two SNPs, with P values of less than 0.025 considered to indicate statistical significance.
Results
Characteristics of the Participants
Blacks (1181 participants) and whites (904 participants) were similar in terms of age, sex, BMI, and menopausal status (Table 1). Blacks were more likely than whites to be impoverished, to be active smokers, and to have microalbuminuria. Blacks were less likely than whites to have received a diagnosis of osteoporosis or to have been prescribed osteoporosis therapies. Use of hormone-replacement therapy and medications that affect vitamin D metabolism (e.g., antiepileptic agents and glucocorticoids) was uncommon (Table 1).
Table 1. Characteristics of the Study Participants Overall and According to Race*.
| Characteristic | Overall (N = 2085) |
Blacks (N = 1181) |
Whites (N = 904) |
P Value |
|---|---|---|---|---|
| Age — yr | 48.3±0.2 | 48.3±0.3 | 48.3±0.3 | 0.92 |
| Male sex — no. (%) | 921 (44.2) | 523 (44.3) | 398 (44.0) | 0.91 |
| BMI† | 29.6±0.2 | 29.4±0.2 | 29.8±0.2 | 0.14 |
| Household income <125% of poverty line — no. (%) | 850 (40.8) | 573 (48.5) | 277 (30.6) | <0.001 |
| Score on Houston Activity Scale‡ | 2.4±0.1 | 2.2±0.1 | 2.8±0.1 | <0.001 |
| Current smoker — no./total no. (%) | 930/1938 (48.0) | 552/1091 (50.6) | 378/847 (44.6) | 0.01 |
| Diagnosis of osteoporosis — no./total no. (%) | 51/1730 (2.9) | 19/946 (2.0) | 32/784 (4.1) | 0.01 |
| Prescribed osteoporosis therapies — no. (%)§ | 29 (1.4) | 10 (0.8) | 19 (2.1) | 0.02 |
| Postmenopausal — no. of women/total no. (%) | 623/1104 (56.4) | 345/626 (55.1) | 278/478 (58.2) | 0.42 |
| Prescribed HRT — no. of women/total no. (%) | 27/1105 (2.4) | 10/618 (1.6) | 17/487 (3.5) | 0.045 |
| Microalbuminuria — no./total no. (%)¶ | 37/1383 (2.7) | 27/710 (3.8) | 10/673 (1.5) | 0.01 |
| Estimated GFR of <60 ml/min/1.73 m2 — no./total no. (%)║ | 114/2039 (5.6) | 67/1141 (5.9) | 47/898 (5.2) | 0.53 |
| Prescribed antiepileptic agents — no. (%)** | 14 (0.7) | 6 (0.5) | 8 (0.9) | 0.30 |
| Prescribed glucocorticoids — no. (%)†† | 28 (1.3) | 20 (1.7) | 8 (0.9) | 0.11 |
| Dietary vitamin D intake — IU/day | 152±4 | 149±5 | 157±6 | 0.38 |
| Dietary calcium intake — mg/day | 731±11 | 720±14 | 744±17 | 0.10 |
Race was self-reported. Plus–minus values are means ±SE. P values of less than 0.05 were considered to indicate statistical significance. HRT denotes hormone-replacement therapy.
The body-mass index (BMI) is the weight in kilograms divided by the square of the height in meters.
Scores on the Houston Activity Scale range from 0 to 7, with higher scores indicating greater habitual physical activity. Data were missing for 785 black participants (66.5%) and 672 white participants (74.3%).
Osteoporosis therapies included pamidronate, neridronic acid, olpadronate, alendronate, ibandronate, risedronate, zoledronate, denosumab, teriparatide, and raloxifene.
Microalbuminuria was defined as a urinary microalbumin-to-creatinine ratio of more than 30 μg of microalbumin per milligram of creatinine.
The estimated glomerular filtration rate (GFR) was calculated with the use of the Chronic Kidney Disease Epidemiology Collaboration equation.
Antiepileptic agents included phenobarbital, carbamazepine, phenytoin, and primidone.
Glucocorticoids included prednisone, hydrocortisone, methylprednisolone, prednisolone, and dexamethasone.
Total 25-Hydroxyvitamin D, Vitamin D–Binding Protein, and Markers of Vitamin D Status
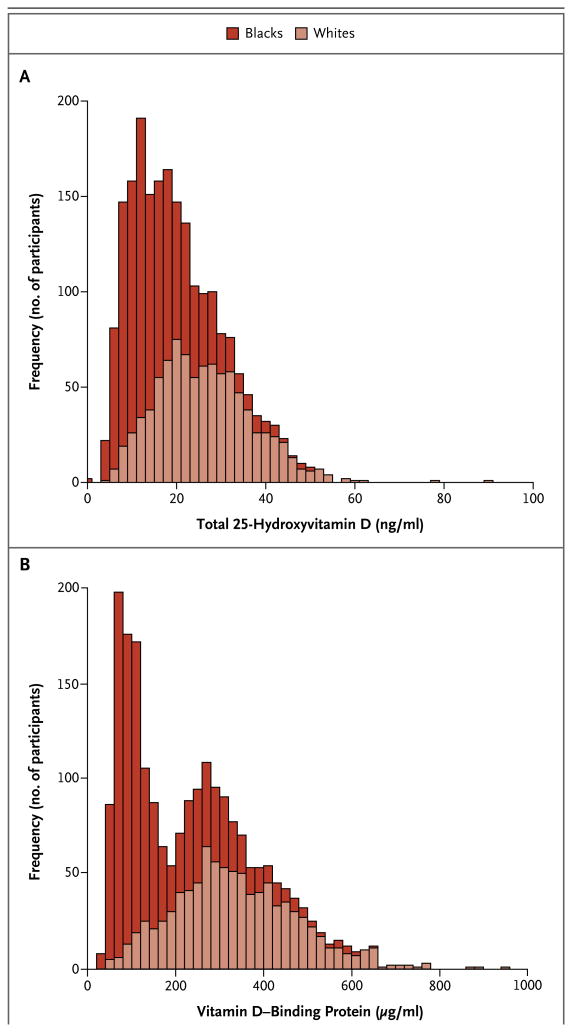
Unadjusted levels of total 25-hydroxyvitamin D were lower in blacks than in whites (15.6±0.2 ng per milliliter vs. 25.8±0.4 ng per milliliter, P<0.001) (Fig. 1A). Racial differences in total 25-hydroxyvitamin D levels persisted after multivariable adjustment (17.3±0.3 ng per milliliter in blacks vs. 25.5±0.4 ng per milliliter in whites, P<0.001). There were seasonal differences in 25-hydroxyvitamin D levels (Table S1 in the Supplementary Appendix). Race explained 22.7% of the variation in total 25-hydroxyvitamin D levels in an unadjusted model.
Figure 1. Levels of Total 25-Hydroxyvitamin D and Vitamin D-Binding Protein in Community-Dwelling White and Black Study Participants.
Histograms representing stacked distributions are shown. Mean (±SE) levels of total 25-hydroxyvitamin D were significantly lower in blacks than in whites (15.6±0.2 ng per milliliter vs. 25.8±0.4 ng per milliliter, P<0.001) (Panel A), as were levels of vitamin D-binding protein (168±3 μg per milliliter vs. 337±5 μg per milliliter, P<0.001) (Panel B).
Unadjusted levels of vitamin D–binding protein were lower in blacks than in whites (168±3 μg per milliliter vs. 337±5 μg per milliliter, P<0.001) (Fig. 1B). Racial differences in vitamin D–binding protein levels persisted after multivariable adjustment (169±5 μg per milliliter in blacks vs. 339±5 μg per milliliter in whites, P<0.001). There were seasonal differences in vitamin D– binding protein levels; they appeared to explain 0.5% of the variation in vitamin D–binding protein levels (Table S1 in the Supplementary Appendix). Race explained 30.5% of the variation in vitamin D–binding protein levels in an unadjusted model.
Adjusted mean BMD at the femoral neck was greater in blacks than in whites (1.05±0.01 g per square centimeter vs. 0.94±0.01 g per square centimeter, P<0.001), as were adjusted mean calcium levels (9.11±0.01 mg per deciliter vs. 8.99±0.01 mg per deciliter, P<0.001). Adjusted mean levels of parathyroid hormone were higher in blacks than in whites (39±1 pg per milliliter vs. 34±1 pg per milliliter, P<0.001). When we excluded participants with measurable 25-hydroxyvitamin D2, our findings did not change appreciably (data not shown).
Genetic Polymorphisms, Vitamin D–Binding Protein, and Total 25-Hydroxyvitamin D
Blacks were more likely than whites to have the T allele at rs7041, whereas whites were more likely than blacks to have the G allele at this location (P<0.001 for both comparisons); blacks were less likely to have the A allele at rs4588 (P<0.001) (Table 2).
Table 2. Influence of Genetic Polymorphisms on Levels of Vitamin D–Binding Protein and Total 25-Hydroxyvitamin D*.
| SNP | Reference Allele | Variant Allele | Variant Allele Frequency | Change in Vitamin D–Binding Protein Level per Variant Allele Copy (95% CI) | P Value | Change in Total 25-Hydroxyvitamin D Level per Variant Allele Copy (95% CI) | P Value |
|---|---|---|---|---|---|---|---|
| μg/ml | ng/ml | ||||||
|
| |||||||
| Blacks | |||||||
|
| |||||||
| rs7041 | G | T | 0.83 | −189.4 (−195.7 to −183.1) | <0.001 | −2.0 (−2.9 to −1.1) | <0.001 |
|
| |||||||
| rs4588 | C | A | 0.10 | 57.0 (49.2 to 64.7) | <0.001 | −0.5 (−1.7 to 0.6) | 0.33 |
|
| |||||||
| Whites | |||||||
|
| |||||||
| rs7041 | G | T | 0.42 | −189.1 (−201.0 to −177.3) | <0.001 | 0.2 (−1.3 to 1.7) | 0.77 |
|
| |||||||
| rs4588 | C | A | 0.28 | 48.9 (36.0 to 61.8) | <0.001 | −2.5 (−4.1 to −0.9) | 0.003 |
Data on 1126 blacks and 855 whites were included in the analysis. CI denotes confidence interval, and SNP single-nucleotide polymorphism. P values of less than 0.025 were considered to indicate statistical significance (adjusted for two SNPs).
The T allele at rs7041 was associated with decreased levels of vitamin D–binding protein in both blacks and whites (Table 2). The A allele at rs4588 was associated with higher vitamin D– binding protein levels in both blacks and whites after we accounted for the allele at rs7041. The polymorphisms at rs7041 and rs4588 had additive effects on vitamin D–binding protein concentrations (Table 2). Genetic variants independently appeared to explain 79.4% of the variation in vitamin D–binding protein levels after we accounted for other factors. After genetic variants were taken into account, race appeared to explain less than 0.1% of the variation in vitamin D– binding protein levels.
The T allele at rs7041 was associated with decreased levels of total 25-hydroxyvitamin D among blacks. In whites, the A allele at rs4588 was associated with decreased levels of total 25-hydroxyvitamin D (Table 2). These genetic polymorphisms appeared to explain 9.9% of the variation in total 25-hydroxyvitamin D levels after other factors were taken into account. In the same model, season and race appeared to explain 10.5% and 7.3% of the variation in total 25-hydroxyvitamin D levels, respectively, whereas sex, age, smoking, calcium intake, BMI, poverty, and microalbuminuria each appeared to account for less than 2.0% of the variation. Overall, 31.2% of the variation in total 25-hydroxyvitamin D levels appeared to be explained in a model containing the aforementioned variables. The concentration of vitamin D– binding protein and the genotype of vitamin D– binding protein appeared to explain a similar amount of variation.
Findings In Homozygous Participants
Vitamin D–Binding Protein Phenotypes and Bioavailable 25-Hydroxyvitamin D
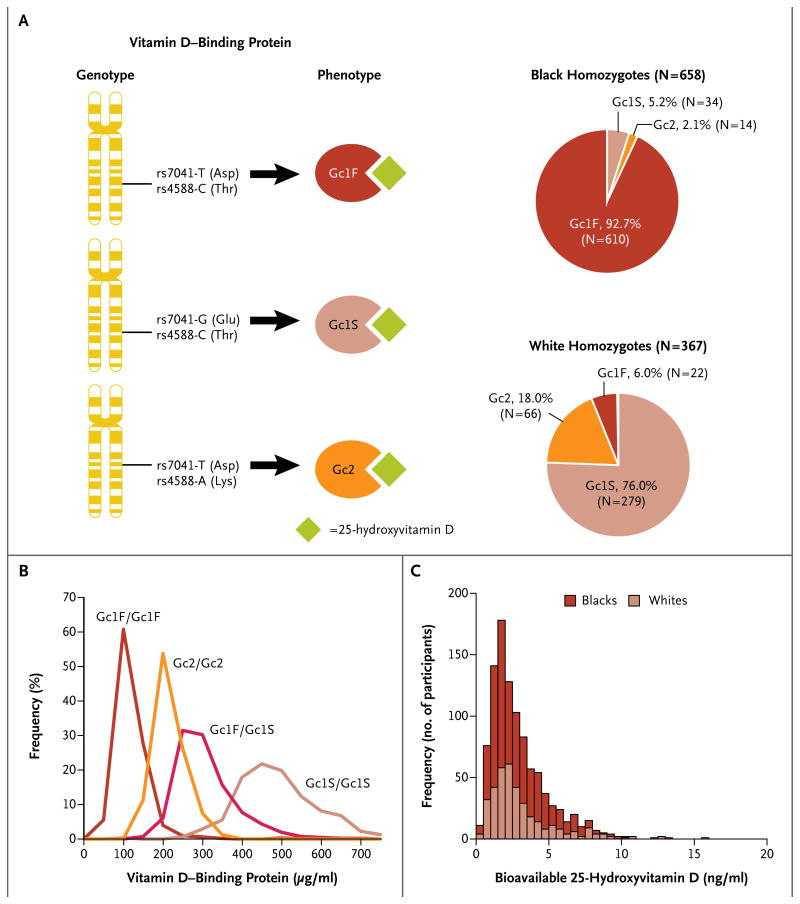
Figure 2A shows the percentage of homozygous participants in each racial group with each variant vitamin D–binding protein (resulting from unique combinations of rs7041 and rs4588). Vitamin D–binding protein levels were lowest in Gc1F homozygous participants, highest in Gc1S homozygous participants, and intermediate in Gc2 homozygous participants (P<0.001 for all comparisons) (Fig. 2B). Among all 1025 homozygous participants, calculated levels of bioavailable 25-hydroxyvitamin D were similar in blacks and whites (2.9±0.1 ng per milliliter and 3.1±0.1 ng per milliliter, respectively; P = 0.71) (Fig. 2C).
Figure 2. Variant Vitamin D–Binding Proteins and Bioavailable 25-Hydroxyvitamin D.
As shown in Panel A, unique combinations of the rs7041 and rs4588 polymorphisms produce amino acid changes resulting in variant vitamin D–binding proteins (left side of panel; Asp denotes aspartic acid, Glu glutamic acid, Lys lysine, and Thr threonine). The Gc1F phenotype was most common in black homozygotes, whereas the Gc1S phenotype was most common in white homozygotes (right side of panel). As shown in Panel B, levels of vitamin D–binding protein were lowest in Gc1F/Gc1F homozygotes (632 participants, 93±2 μg per milliliter), highest in Gc1S/Gc1S homozygotes (313 participants, 468±6 μg per milliliter), and intermediate in Gc2/Gc2 homozygotes (80 participants, 190±4 μg per milliliter). Plasma vitamin D–binding protein concentrations in Gc1F/Gc1S heterozygotes (413 participants, 285±4 μg per milliliter) were intermediate between those of Gc1F/Gc1F homozygotes and Gc1S/Gc1S homozygotes. These differences were significant (P<0.001 for all comparisons). Panel C shows a histogram representing stacked distributions. Among homozygous participants, levels of bioavailable 25-hydroxyvitamin D were similar in blacks and whites (2.9±0.1 ng per milliliter in blacks and 3.1±0.1 ng per milliliter in whites, P = 0.71).
Markers of Vitamin D Status and 25-Hydroxyvitamin D
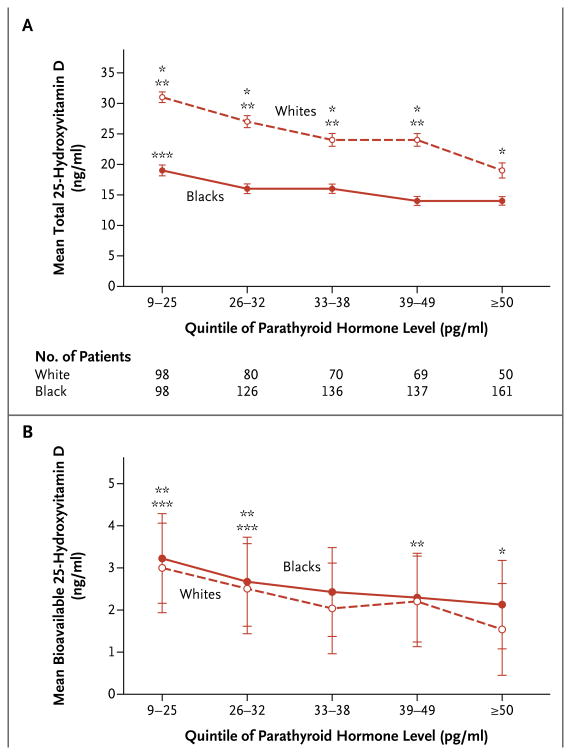
BMD was not associated with levels of bioavailable or total 25-hydroxyvitamin D in black homozygous participants; however, in white homozygous participants, BMD generally increased with increasing levels of total or bioavailable 25-hydroxyvitamin D (Table S2 in the Supplementary Appendix). Calcium levels increased with increasing levels of total 25-hydroxyvitamin D in blacks only (Table S2 in the Supplementary Appendix). Lower levels of total or bioavailable 25-hydroxyvitamin D were associated with higher levels of parathyroid hormone in homozygotes of both races (P<0.001 for all relationships) (Table S2 in the Supplementary Appendix). As compared with white homozygotes with similar parathyroid hormone levels, black homozygotes had significantly lower levels of total 25-hydroxyvitamin D (Fig. 3A). In contrast, homozygous blacks and whites with similar parathyroid hormone levels had similar levels of bioavailable 25-hydroxyvitamin D (Fig. 3B). Relationships between total 25-hydroxyvitamin D levels and markers of vitamin D status in homozygotes were similar to those in the overall study population.
Figure 3. Total and Bioavailable 25-Hydroxyvitamin D Levels among Homozygous Blacks and Whites with Similar Parathyroid Hormone Levels.
Within quintiles of parathyroid hormone values, blacks generally had lower levels of total 25-hydroxyvitamin D levels than whites (Panel A) but similar levels of bioavailable 25-hydroxyvitamin D (Panel B). I bars indicate standard errors. One asterisk denotes P<0.01 for the comparisons between blacks and whites within the quintile, two asterisks P<0.01 for the comparison with the highest quintile among whites, and three asterisks P<0.01 for the comparison with the highest quintile among blacks.
Discussion
Because levels of total 25-hydroxyvitamin D are consistently lower in black Americans than in white Americans, blacks are frequently classified as being vitamin D–deficient.11-13 In our study involving community-dwelling adults, we found that levels of vitamin D–binding protein are also lower in blacks, probably because of the high prevalence of a common genetic variant. Lower levels of vitamin D–binding protein in blacks appear to result in levels of bioavailable 25-hydroxyvitamin D that are equivalent to those in whites. These data, combined with previous data from our group,29 suggest that low total 25-hydroxyvitamin D levels do not uniformly indicate vitamin D deficiency and call into question routine supplementation in persons with low levels of both total 25-hydroxyvitamin D and vitamin D– binding protein who lack other traditional manifestations of this condition.
Thresholds for vitamin D sufficiency have been based on total 25-hydroxyvitamin D levels at which calcium absorption declines or parathyroid hormone levels increase.30,31 Because experimental data are inconclusive, controversy surrounds the precise level of total 25-hydroxyvitamin D at which these changes occur.30,31 We studied a community-dwelling population, in which overt vitamin D deficiency was rare; in fact, few participants had parathyroid hormone levels outside the normal range. Still, on the basis of the current guidelines (suggesting a threshold for sufficiency of 20 or 30 ng per milliliter), 77 to 96% of our black participants would be classified as vitamin D–deficient.32,33 Labeling the majority of the black participants as vitamin D–deficient would be inconsistent with the observation that they had higher BMD, higher calcium levels, and only slightly higher parathyroid hormone levels than their white counterparts.
Low levels of vitamin D–binding protein in blacks may provide protection against the manifestations of vitamin D deficiency despite low levels of total 25-hydroxyvitamin D. The bio-availability of other lipophilic hormones, such as thyroid hormone, is known to be influenced by the concentration of carrier proteins. When the concentration of the thyroxine-binding globulin is low or undetectable, there is a lower total thyroid hormone requirement for sufficiency.34 Analogously, mice that lack vitamin D–binding protein have low levels of total 25-hydroxyvitamin D but do not show signs of vitamin D deficiency.20 Therefore, low levels of total 25-hydroxyvitamin D probably do not indicate true vitamin D deficiency when levels of vitamin D–binding protein are also low, as in many black Americans. Bioavailable 25-hydroxyvitamin D may be a more appropriate cross-racial marker of vitamin D sufficiency; however, investigations in populations with overt vitamin D deficiency are required before routine clinical use is warranted.
Levels of total 25-hydroxyvitamin D are, in part, genetically determined.24,35,36 In our study, genetic polymorphisms in vitamin D–binding protein appeared to account for a greater proportion of the variation in total 25-hydroxyvitamin D levels than most factors known to be associated with 25-hydroxyvitamin D levels.35-37 The effect of vitamin D–binding protein polymorphisms on total 25-hydroxyvitamin D concentrations appeared to be mediated by the concentration of vitamin D –binding protein, an observation that is consistent with the findings in a previous study.38 Data in genetically modified mice suggest that the function of vitamin D–binding protein is to prolong the half-life of 25-hydroxyvitamin D, supporting this hypothesis.20 Although mice lacking vitamin D–binding protein do not have manifestations of overt deficiency at baseline, they are more susceptible to deficiency than normal mice when deprived of vitamin D.20 Vitamin D–binding protein prolongs the half-life of 25-hydroxyvitamin D by serving as a reservoir and aiding in the reabsorption of filtered vitamin D through megalin in the kidney.20,39 We speculate that low levels of vitamin D–binding protein may confer a predisposition to inadequate 25-hydroxyvitamin D levels when vitamin D sources are scarce. Levels of vitamin D–binding protein only partially explained racial differences in levels of total 25-hydroxyvitamin D; other factors, including skin pigmentation and other polymorphisms, probably contribute to low levels of total 25-hydroxyvitamin D in blacks.1,40,41
Our study has certain limitations. First, given the cross-sectional and observational nature of the study, we were unable to predict the effects of vitamin D–binding protein levels on the risk of fracture. Second, measurement of bone-turnover markers, levels of 1,25-dihydroxyvitamin D, and urinary calcium excretion might have provided additional insight into the effect of vitamin D– binding protein on mineral metabolism. Third, we did not have data on the use of vitamin D supplements. However, when we excluded participants with measurable 25-hydroxyvitamin D2, which suggests exogenous supplementation with vitamin D derived from plants or fungi, our findings did not change. Further investigation is needed to determine the effects of supplementation on total and bioavailable 25-hydroxyvitamin D levels in persons with different vitamin D–binding protein genotypes. Finally, we relied predominantly on calculation of bioavailable 25-hydroxyvitamin D rather than direct measurement. Among homozygous participants, however, direct measurement of bioavailable 25-hydroxyvitamin D was well correlated with calculated levels.
There is an alternative commercially available assay for measuring vitamin D–binding protein levels; the results of that assay are inconsistent with those of the assay used in this study (Fig. S5 and S6 in the Supplementary Appendix). The vitamin D–binding protein levels we report correlate inversely with the percentage of bioavailable 25-hydroxyvitamin D measured directly. Given the lack of genotype-specific standards in our direct assay format, we could not accurately report absolute concentrations. Our data should provide an impetus for the development of assays that directly measure bioavailable 25-hydroxyvitamin D.
Vitamin D deficiency is certainly present in persons with very low levels of total 25-hydroxyvitamin D accompanied by hyperparathyroidism, hypocalcemia, or low BMD. However, community-dwelling blacks with total 25-hydroxyvitamin D levels below the threshold used to define vitamin D deficiency typically lack the accompanying characteristic alterations. The high prevalence among blacks of a polymorphism in the vitamin D–binding protein gene that is associated with low levels of vitamin D–binding protein results in levels of bioavailable 25-hydroxyvitamin D that are similar to those in whites, despite lower levels of total 25-hydroxyvitamin D. Alterations in vitamin D–binding protein levels may therefore be responsible for observed racial differences in total 25-hydroxyvitamin D levels and manifestations of vitamin D deficiency. To improve the determination of vitamin D status in diverse populations, the measurement of vitamin D–binding protein will most likely need to be incorporated into the assessment.
Supplementary Material
Acknowledgments
Supported in part by the National Institute on Aging Intramural Research Program at the National Institutes of Health (NIH) (project ZIA AG000513) and grants from the NIH (K24 DK094872 and R01 DK094486, to Dr. Thadhani). Dr. Karumanchi is a Howard Hughes Medical Institute investigator.
We thank Dr. Ngozi Ejiogu, the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) clinical staff, and study manager Jennifer Norbeck for participant evaluation and study management; the Health Disparities Research Section staff (Nicole Noren Hooten, Kim Jacobs, Megan Fitzpatrick, Althaf Lohani, and Janice Barnes) for handling and processing of all HANDLS biomaterials; Vance Morgan and Hardeep Ranu from the Partners HealthCare Center for Personalized Genetic Medicine for genotyping the HANDLS participants; Dr. Kathryn Lucchesi for her critical review of a draft of the manuscript; and the NIH (Bethesda, MD) for use of the high-performance computational capabilities of the Biowulf Linux cluster.
Footnotes
Drs. Berg, Bhan, Karumanchi, and Thadhani report being co-inventors on a patent pending on the use of bioavailable vitamin D for the assessment of vitamin D status. No other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Adams JS, Hewison M. Update in vitamin D. J Clin Endocrinol Metab. 2010;95:471–8. doi: 10.1210/jc.2009-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Melamed ML, Michos ED, Post W, Astor B. 25-Hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168:1629–37. doi: 10.1001/archinte.168.15.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–11. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas MK, Lloyd-Jones DM, Thadhani RI, et al. Hypovitaminosis D in medical inpatients. N Engl J Med. 1998;338:777–83. doi: 10.1056/NEJM199803193381201. [DOI] [PubMed] [Google Scholar]
- 6.Cauley JA, Lacroix AZ, Wu L, et al. Serum 25-hydroxyvitamin D concentrations and risk for hip fractures. Ann Intern Med. 2008;149:242–50. doi: 10.7326/0003-4819-149-4-200808190-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med. 1992;327:1637–42. doi: 10.1056/NEJM199212033272305. [DOI] [PubMed] [Google Scholar]
- 8.Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669–83. doi: 10.1056/NEJMoa055218. Erratum, N Engl J Med 2006;354:1102. [DOI] [PubMed] [Google Scholar]
- 9.Sanders KM, Stuart AL, Williamson EJ, et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303:1815–22. doi: 10.1001/jama.2010.594. Erratum, JAMA 2010;303:2357. [DOI] [PubMed] [Google Scholar]
- 10.Aloia JF, Talwar SA, Pollack S, Yeh J. A randomized controlled trial of vitamin D3 supplementation in African American women. Arch Intern Med. 2005;165:1618–23. doi: 10.1001/archinte.165.14.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitchell DM, Henao MP, Finkelstein JS, Burnett-Bowie SA. Prevalence and predictors of vitamin D deficiency in healthy adults. Endocr Pract. 2012;18:914–23. doi: 10.4158/EP12072.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gutiérrez OM, Farwell WR, Kermah D, Taylor EN. Racial differences in the relationship between vitamin D, bone mineral density, and parathyroid hormone in the National Health and Nutrition Examination Survey. Osteoporos Int. 2011;22:1745–53. doi: 10.1007/s00198-010-1383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ginde AA, Liu MC, Camargo CA., Jr Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169:626–32. doi: 10.1001/archinternmed.2008.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hannan MT, Litman HJ, Araujo AB, et al. Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. J Clin Endocrinol Metab. 2008;93:40–6. doi: 10.1210/jc.2007-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bischoff-Ferrari HA, Dietrich T, Orav EJ, Dawson-Hughes B. Positive association between 25-hydroxy vitamin D levels and bone mineral density: a populationbased study of younger and older adults. Am J Med. 2004;116:634–9. doi: 10.1016/j.amjmed.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 16.Cauley JA, Lui LY, Ensrud KE, et al. Bone mineral density and the risk of incident nonspinal fractures in black and white women. JAMA. 2005;293:2102–8. doi: 10.1001/jama.293.17.2102. [DOI] [PubMed] [Google Scholar]
- 17.Kritchevsky SB, Tooze JA, Neiberg RH, et al. 25-Hydroxyvitamin D, parathyroid hormone, and mortality in black and white older adults: the Health ABC study. J Clin Endocrinol Metab. 2012;97:4156–65. doi: 10.1210/jc.2012-1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wright NC, Chen L, Niu J, et al. Defining physiologically “normal” vitamin D in African Americans. Osteoporos Int. 2012;23:2283–91. doi: 10.1007/s00198-011-1877-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bikle DD, Gee E, Halloran B, Kowalski MA, Ryzen E, Haddad JG. Assessment of the free fraction of 25-hydroxyvitamin D in serum and its regulation by albumin and the vitamin D-binding protein. J Clin Endocrinol Metab. 1986;63:954–9. doi: 10.1210/jcem-63-4-954. [DOI] [PubMed] [Google Scholar]
- 20.Safadi FF, Thornton P, Magiera H, et al. Osteopathy and resistance to vitamin D toxicity in mice null for vitamin D binding protein. J Clin Invest. 1999;103:239–51. doi: 10.1172/JCI5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bikle DD, Gee E. Free, and not total, 1,25-dihydroxyvitamin D regulates 25-hydroxyvitamin D metabolism by keratinocytes. Endocrinology. 1989;124:649–54. doi: 10.1210/endo-124-2-649. [DOI] [PubMed] [Google Scholar]
- 22.Arnaud J, Constans J. Affinity differences for vitamin D metabolites associated with the genetic isoforms of the human serum carrier protein (DBP) Hum Genet. 1993;92:183–8. doi: 10.1007/BF00219689. [DOI] [PubMed] [Google Scholar]
- 23.Braun A, Bichlmaier R, Cleve H. Molecular analysis of the gene for the human vitamin-D-binding protein (group-specific component): allelic differences of the common genetic GC types. Hum Genet. 1992;89:401–6. doi: 10.1007/BF00194311. [DOI] [PubMed] [Google Scholar]
- 24.Engelman CD, Fingerlin TE, Langefeld CD, et al. Genetic and environmental determinants of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels in Hispanic and African Americans. J Clin Endocrinol Metab. 2008;93:3381–8. doi: 10.1210/jc.2007-2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Constans J, Hazout S, Garruto RM, Gajdusek DC, Spees EK. Population distribution of the human vitamin D binding protein: anthropological considerations. Am J Phys Anthropol. 1985;68:107–22. doi: 10.1002/ajpa.1330680110. [DOI] [PubMed] [Google Scholar]
- 26.Evans MK, Lepkowski JM, Powe NR, LaVeist T, Kuczmarski MF, Zonderman AB. Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS): overcoming barriers to implementing a longitudinal, epidemiologic, urban study of health, race, and socioeconomic status. Ethn Dis. 2010;20:267–75. [PMC free article] [PubMed] [Google Scholar]
- 27.Cummings SR, Black DM, Nevitt MC, et al. Bone density at various sites for prediction of hip fractures. Lancet. 1993;341:72–5. doi: 10.1016/0140-6736(93)92555-8. [DOI] [PubMed] [Google Scholar]
- 28.Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab. 1999;84:3666–72. doi: 10.1210/jcem.84.10.6079. [DOI] [PubMed] [Google Scholar]
- 29.Powe CE, Ricciardi C, Berg AH, et al. Vitamin D-binding protein modifies the vitamin D-bone mineral density relationship. J Bone Miner Res. 2011;26:1609–16. doi: 10.1002/jbmr.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sai AJ, Walters RW, Fang X, Gallagher JC. Relationship between vitamin D, parathyroid hormone, and bone health. J Clin Endocrinol Metab. 2011;96:E436–46. doi: 10.1210/jc.2010-1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosen CJ, Abrams SA, Aloia JF, et al. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab. 2012;97:1146–52. doi: 10.1210/jc.2011-2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30. doi: 10.1210/jc.2011-0385. Erratum, J Clin Endocrinol Metab 2011;96:3908. [DOI] [PubMed] [Google Scholar]
- 33.Dietary references intakes for calcium and vitamin D. Washington, DC: Institute of Medicine; 2011. [Google Scholar]
- 34.Mori Y, Takeda K, Charbonneau M, Refetoff S. Replacement of Leu227 by Pro in thyroxine-binding globulin (TBG) is associated with complete TBG deficiency in three of eight families with this inherited defect. J Clin Endocrinol Metab. 1990;70:804–9. doi: 10.1210/jcem-70-3-804. [DOI] [PubMed] [Google Scholar]
- 35.Wang TJ, Zhang F, Richards JB, et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 2010;376:180–8. doi: 10.1016/S0140-6736(10)60588-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levin GP, Robinson-Cohen C, de Boer IH, et al. Genetic variants and associations of 25-hydroxyvitamin D concentrations with major clinical outcomes. JAMA. 2012;308:1898–905. doi: 10.1001/jama.2012.17304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bertrand KA, Giovannucci E, Liu Y, et al. Determinants of plasma 25-hydroxyvitamin D and development of prediction models in three US cohorts. Br J Nutr. 2012;108:1889–96. doi: 10.1017/S0007114511007409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lauridsen AL, Vestergaard P, Hermann AP, et al. Plasma concentrations of 25-hydroxy-vitamin D and 1,25-dihydroxyvitamin D are related to the phenotype of Gc (vitamin D-binding protein): a cross-sectional study on 595 early postmenopausal women. Calcif Tissue Int. 2005;77:15–22. doi: 10.1007/s00223-004-0227-5. [DOI] [PubMed] [Google Scholar]
- 39.Nykjaer A, Dragun D, Walther D, et al. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell. 1999;96:507–15. doi: 10.1016/s0092-8674(00)80655-8. [DOI] [PubMed] [Google Scholar]
- 40.Aloia JF. African Americans, 25-hydroxyvitamin D, and osteoporosis: a paradox. Am J Clin Nutr. 2008;88:545S–50S. doi: 10.1093/ajcn/88.2.545S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity of skin to synthesise vitamin D3. Lancet. 1982;1:74–6. doi: 10.1016/s0140-6736(82)90214-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.