Abstract
Background
Electronic communication between providers occurs daily in clinical practice but has not been well studied.
Purpose
To assess the impact of provider-to-provider electronic communication tools on communication and healthcare outcomes through literature review.
Data sources
OVID Medline, Pubmed, Google Scholar, CINAHL, and Academic Search Premier.
Study Selection
Publication in English language peer-reviewed journals. Studies provided quantitative provider-to-provider communication data, provider satisfaction statistics, or EHR communication data.
Data Extraction
Literature review.
Data Synthesis
Two reviewers conducted the title review to determine eligible studies from initial search results. Three reviewers independently reviewed titles, abstracts, and full text (where appropriate) against inclusion and exclusion criteria.
Limitations
Small number of eligible studies; few described trial design (20%). Homogeneous provider-type (physicians). English-only studies.
Conclusions
Of twenty-five included studies, all focused on physicians; most were observational (68%). Most (60%) described electronic specialist referral tools. Although overall use has been measured, there were no studies of the effectiveness of intra-EHR messaging. Literature describing the effectiveness of provider-to-provider electronic communications is sparse and narrow in scope. Complex care, such as that envisioned for the Patient Centered Medical Home, necessitates further research.
Keywords: Communication, Hospital Medicine, Electronic Health Record, Teamwork, Systematic Review
Introduction
Coordination of care within a practice, during transitions of care, and between primary and specialty care teams requires more than data exchange; it requires effective communication among healthcare providers.(1-3) In clinical terms, data exchange, communication, and care coordination are related, but they represent distinct concepts.(4) Data exchange refers to transfer of information between settings, independent of the individuals involved, whereas communication is the multistep process that enables information exchange between two people.(5) Care coordination, as defined by O'Malley, is “integration of care in consultation with patients, their families and caregivers across all of a patient's conditions, needs, clinicians and settings.”(3)
Strong collaboration among providers has been associated with improved patient outcomes.(2, 6) Yet, despite the significant role of communication in healthcare, communication may not take place at all, even at high-stakes events like transitions of care(7, 8), or it may be done poorly at the risk of substantial clinical morbidity and mortality.(9-16)
Proof of the global effectiveness of health information technology (HIT) to improve patient care is lacking, but data from some studies demonstrate real improvements in quality and safety in specific areas (17-19), especially with computerized physician order entry (CPOE)(20) and electronic prescribing.(21)
The limited information about the effect of HIT on communication focuses largely on the anticipated improvements in patient-physician communication(22-27); provider-to-provider communication within the electronic domain is not as well understood. A recent review of interventions involving communication devices such as pagers and mobile phones found limited high-quality evidence in the literature.(28) Clinicians have described what they consider to be key characteristics of clinical electronic communications systems such as security/reliability, cross coverage, overall convenience, and message prioritization.(29) Although the electronic health record (EHR) is expected to assist with this communication(30), it also has the potential to impede effective communication, leading physicians to resort to more traditional “workarounds.”(31-33)
Measuring and improving the use of electronic health records nationally were driving forces behind the creation of the “Meaningful Use” incentive program in the United States. (34) In order to receive the incentive payments, providers must meet and report on a series of measures set in three stages over the course of five years.(35) In the current state, Meaningful Use does not reward provider-to-provider communication within the EHR.(36, 37) The main communication objectives for stages 1 and 2 concentrate on patient-to-provider communication, such as patient portals and patient-to-provider messaging.(36, 37)
Understanding the current evidence for provider-to-provider communication within EHRs, its reported effectiveness, and its shortcomings may help to develop a roadmap for identifying next-generation solutions to support coordination of care.(38, 39) This review assesses the literature regarding provider-to-provider electronic communication tools (as supported within or external to an EHR). It is intended as a comprehensive view of studies reporting quantitative measures of the impact of electronic communication on providers and patients.
Methods
Definitions and Conceptual Model of Provider-to-Provider Communication
We conducted a systematic review of studies of provider-to-provider electronic communication. This review included only formal clinical communication between providers and was informed by the Coiera communications paradigm.(5) This paradigm consists of four steps: 1) Task identification, when a task is identified and associated with the appropriate individual; 2) Connection, when an attempt is made to contact that person; 3) Communication, when task specific information is exchanged between the parties; 4) Disconnection, when the task reaches some stage of completion.
Literature Review
We examined written electronic communication between providers including email, text messaging, and instant messaging. We did not review provider-to-provider telephone or telehealth communication as these are not generally supported within EHR systems. Communication in all clinical contexts was included among providers within an individual clinic or hospital and among providers across specialties or practice settings.(40) We excluded physician handoff communication because it has been extensively reviewed elsewhere and because handoff occurs largely through verbal exchange not recorded in the EHR.(41, 42) Communication from clinical information systems to providers, such as automated notification of unacknowledged orders, was also excluded as it is not within the scope of provider-to-provider interaction.
Data Sources and Searches
A comprehensive literature search was conducted in OVID Medline with the input of a medical librarian, and a parallel search was performed using PubMed. The OVID Medline query and parallel database search terms are documented (Table 1). Sub-searches were conducted in Google Scholar, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Academic Search Premier peer-reviewed journals. Subsequent studies citing the initially detected articles were found through citation maps.
Table 1. Search Strategies.
| Database | Strategy | Items Reviewed |
|---|---|---|
|
| ||
| OVID Medline | Query terms: | 1513 |
| “exp” denotes Explode and * denotes Focus | exp medicine/ or physicians or exp outpatient clinics/ or exp hospitals/ | |
| AND | ||
| *communication/ or *computer communication networks/ or *interprofessional relations/ or *continuity of patient care/ | ||
| AND | ||
| Electronic Mail or Referral and Consultation or text messaging/ or reminder systems/ | ||
|
| ||
| Pubmed | healthcare, provider, communication, messaging, email, texting, text messaging, instant messaging, paging, coordination, referral, EHR, EMR, electronic health record, electronic medical record, electronic, and physician. Excluding patient-provider and patient-physician. | 340 |
|
| ||
| Google scholar | physician-physician electronic communication excluding“physician-patient” | 940 |
|
| ||
| CINAHL | medical records and communication; or computerized patient records and communication | none |
|
| ||
| Academic Search Premier - peer reviewed journals | electronic health record and communication | 54 |
|
| ||
| communication and electronic health record | 80 | |
|
| ||
| physician-physician communication | 2 | |
|
| ||
| physicians and electronic health records | 88 | |
Study Selection
Paper Inclusion Criteria
Requirements included publication in English language peer-reviewed journals. Included studies provided quantitative provider-to-provider communication data, provider satisfaction statistics, or EHR communication data. Provider-to-staff communication was also included if it fell within the scope of studies of communication between providers.
Paper Exclusion Criteria
Studies excluded in this review were articles that reviewed EHR systems without any focus on communication between providers and those that discussed EHR models and strategies but did not include actual testing and quantitative results. Results that included non-traditional online documents or that were found on non-peer-reviewed websites were also discarded. Duplicate records or publications that covered the same study were also removed. The most common reason for exclusion was the lack of quantitative evaluation.
Data Extraction and Quality Assessment
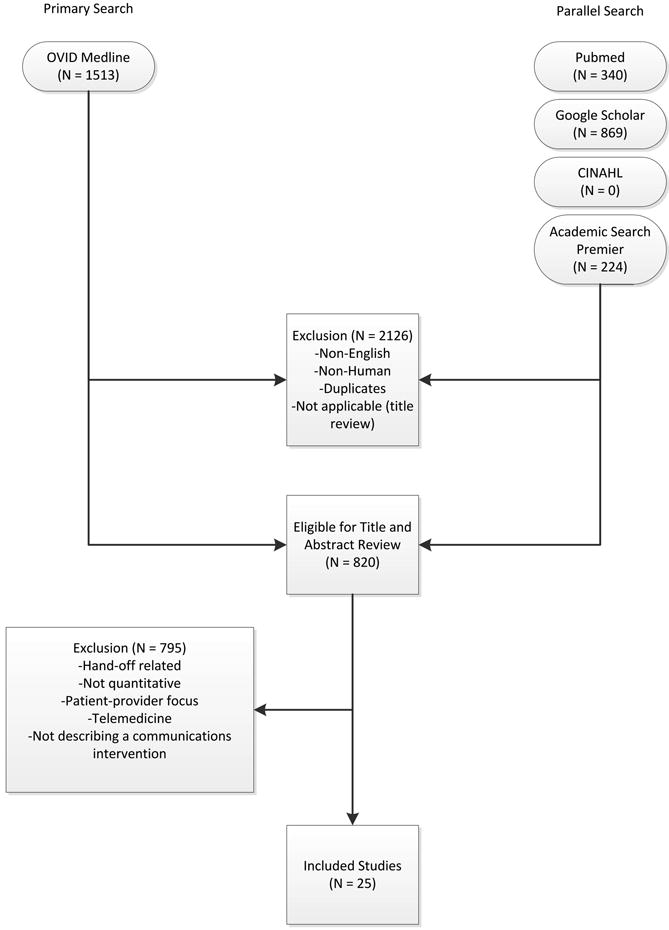
Authors (Walsh, Siegler, Stetson) reviewed titles and abstracts of resultant studies against inclusion and exclusion criteria (Figure 1). Studies were evaluated qualitatively and findings summarized. Given the heterogeneous nature of data reported, statistical analysis was not possible.
Figure 1. Literature Flow Diagram.
Results
The primary and parallel searches produced 2,946 results that were weaned through title review and exclusion of duplicates, non-English language, and non-human studies to 820 articles for title and abstract review (Figure 1). After careful review of the articles' titles, abstracts, or full content (where appropriate), twenty-five articles met inclusion criteria and presented data about provider-to-provider electronic communication, either within an EHR or through a system designed to promote provider-to-provider communication. All of the studies that met inclusion criteria focused on physicians as providers. Five studies (20%) described trial design, three (12%) were pilot studies, and seventeen (68%) were observational studies. Thirteen of twenty-five articles (52%) described studies conducted in the United States and twelve in Europe.
Most of the studies (56%) focused on electronic referrals between primary care and subspecialty providers. The clinical need was to communicate information on a specific patient with a specialist who shared responsibility for the overall plan of care. Only two studies evaluated “curbside consultation,” where providers ask for clinical recommendations without formally engaging a specialist in the plan of care for a particular patient. Table 2 summarizes included studies and has been organized with respect to clinical need under evaluation. The major themes that emerged from this review included: studies of penetration of communication tools either within the EHR system (“intra-EHR IT”) or external to the EHR (“extra-EHR IT”); electronic referrals; curbside consultations; test results reporting (“results notification”).
Table 2. Studies of Electronic Provider-to-provider Communication by Clinical Need.
| Primary Author, year (reference) | Design | Intervention | Measurement | Results |
|---|---|---|---|---|
| Need: Communicate care across clinical settings (Inpatient-Outpatient) | ||||
| Branger, 1992(46) | Observational study | Introduction of electronic messaging system in the Netherlands between hospital and primary care physicians (PCPs). | Satisfaction survey data using Likert scale of “usefulness” | Free text messaging to exchange patient data was rated “very useful” or “useful” by twenty of twenty-seven PCP respondents |
| Reponen, 2004(66) | Observational study | Finnish study of electronic referrals - XML messages between EHRs or secure web links | User questionnaire. No description of respondents was provided | Internists surveyed estimated that electronic referrals accelerate the referral process by one week |
| Need: Communicate care across specialties (Primary Care Physicians-Specialists) | ||||
| Kooijman, 1998(67) | Observational study | Survey of 45 PCPs who received notes from specialists via Electronic Data Interchange | User questionnaire with five point Likert scale of satisfaction, from one (“much better”) to five (“much worse”) | Highest satisfaction scores for speed (1.5-1.8) and efficiency (1.5-1.7) for electronic messages with lower scores for reliability (2.5-2.7) and clarity (2.5) |
| Harno, 2000(48) | Non-randomized trial | Eight-month prospective comparative study in Finland of outpatient clinics of hospitals with and without intranet referral systems. | Comparison of numbers of electronic referrals, clinic visits, costs | 43% of electronic referrals and 79% of outpatient referrals resulted in outpatient visits. 3-fold increase in productivity overall and seven fold reduction in visit costs per patient using e-mail consultation. |
| Moorman, 2001(47) | Observational study | Supersedes Branger, 1999(68). Analyzes intra-HER communications between PCPs and consultant in Netherlands re: diabetes management of patients (1994-1998). | Descriptive statistics of number of messages, content, whether message had been copied into EMR; survey of PCPs (twelve of fifteen responded) | Decline in integration by PCPs of messages in the EHR from 75% to 51% over first three years. Despite this, most PCPs wanted to extend messaging to other patient groups. |
| Bergus, 2006(69) | Observational study | Follow up of Bergus, 1998(54); evaluated formulation of clinical referrals to specialists at the University of Iowa by retrospective review of email transcripts | Analyzed taxonomy of clinical questions; assessed need for clinical consultation of 1618 clinical questions | Specialists less likely to recommend clinic consultation if referral specified the clinical task (OR 0.36, p<0.001), intervention (OR 0.62, p=0.004) or outcome (OR=0.49, p<0.001). This effect was independent of clinical content (p>0.05) |
| Dennison, 2006 (70) | Pilot study | Construction of an electronic referral pro forma to facilitate referral of patients to colorectal surgeons | Descriptive statistics. Comparisons of patient attendance rate, delays to booking and to actual appointment between fifty-four electronic referrals and 189 paper referrals | Compared to paper referrals, electronic referrals were booked more quickly (same day vs one week later on average) and patients had lower non-attendance rates (8.5% vs 22.5%). Both results stated as statistically significant but p values were not provided. |
| Shaw, 2007(49) | Observational study | Dermatology electronic referral in England | Content of 131 electronic versus 139 paper referrals to dermatologists (NHS Choose and Book)(71) | Paper superior to electronic for clinical data such as current treatments (included in 68% of paper versus 39% of electronic referrals, p<0.001); electronic superior for demographic data. |
| Gandhi, 2008(50) | Non-randomized trial | Electronic referral tool in the Partners Healthcare System in Massachusetts that included a structured referral letter generator and referral status tracker. Assigned to one intervention site and one control site. | Survey assessment. Fifty- four of 117 PCPs responded (46%), 235 of 430 specialists responded (55%), 143 out of 210 patients responded (69%) | Intervention group showed high voluntary adoption (99%), higher information transfer rates prior to subspecialty visit (62% versus 12%), and lower rates of conflicting information being given to patients (6% versus 20%) |
| John, 2008 (72) | Pilot study | Validation study of the Lower Gastrointestinal Electronic Referral Protocol (e-RP, through the Choose and Book System in the United Kingdom) intended to improve yield of colon cancers diagnosed and to reduce delays in diagnosis | Comparison of actual to simulated referral patterns through e-RP for 300 patients divided into colorectal cancer, “Two-Week Wait” suspected cancer, and routine referral groups | e-RP was more accurate than traditional referral at upgrading patients who had cancer to the appropriate “suspected cancer” referral group (85% versus 43%, p = 0.002) |
| Kim, 2009(73) | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Included reply functionality and ability to forward messaging to a scheduler for calendaring. | Impact of electronic referral system as measured by questionnaire to referring providers. 298/368 participated (24 clinics); 53.5% attending physicians | Electronic referrals improved overall quality of care (reported by 72%), guidance of pre-subspecialty visit (73%), and the ability to track referrals (89%). Small change in access for urgent issues (35% better, 49% reported no change) |
| Scott, 2009(74) | Pilot study | Pilot of urgent electronic referral system from PCPs to oncologists at South West Wales Cancer Centre | Satisfaction statistics (10-point Likert scale) collected from PCPs via interview | Over six months, ninety-nine referrals submitted; 81% were processed within one hour with high satisfaction scores |
| Were, 2009(75) | Non-randomized trial | Geriatrics consultants were provided system to make electronic recommendations (“consultant-recommended orders”) in the native CPOE system along with consult notes in the intervention versus consult notes alone in the control | Rates of implementation of consultant recommendations. Qualitative survey of users of the new system | Higher total number of recommendations 247 versus 192, p<0.05) and higher implementation rates of consultant-recommended orders in the intervention group versus control (78% versus 59%, p=0.01). High satisfaction scores on five-point Likert scale for the intervention system with good survey response rate (83%). |
| Dixon, 2010(52) | Observational study | Comparison of two extra-EHR systems (NHS Choose and Book, Dutch ZorgDomein) for booking referrals. Patients choose doctor or hospital and the system transfers demographic and clinical information between PCP and specialist | National data, patient and provider surveys, focus groups, observational studies. Focus was on patient choice, but evaluations included all aspects of the systems | Resistance from PCPs during implementation; 78% of ZorgDomein PCPs felt referrals took more time; general displeasure on the part of specialists re: quality of referrals, although not quantified |
| Patterson, 2010 (51) | Observational study | Email referral system to a neurologist in Northern Ireland. Referrals were template based and recorded as clinical episode in the Patient Administration System. Comparison of this system to conventional referrals to another neurologist | Evaluated effectiveness, cost, safety for period 2002-2007 | Decreased referral wait times (four versus thirteen weeks) and 35% cost reduction per patient for the email referral versus conventional referrals. No diminution in safety. Limitation: single neurologist participated |
| Singh, 2011 (76) | Observational study | Chart review of electronic referrals to specialist practices in a Veterans Affairs outpatient system | Follow-up actions taken by subspecialists within 30 days of receiving referral | An intra-EHR referral system was still affected by communication breakdowns.36.4% of 61,931 referrals were discontinued for inappropriate or incomplete referral requests. |
| Kim-Hwang, 2010 (77) | Observational study | Electronic referrals via a portal to San Francisco General Hospital. Follow-up to Kim, 2009 (73) | Survey of medical and surgical subspecialty consultants | Statistically significant differences in clarity of consult request in both medical and surgical clinics, in decreased inappropriate referrals in surgical clinics, in decreased use of follow-up appointments by surgical specialists and in decreased avoidable follow-up surgical visits. |
| Warren, 2011(53) | Observational study | Electronic referrals from general medical practices to public referral network of Hutt Hospital in New Zealand (2007-2010) | Retrospective analysis of transactional data from messaging system and from general inpatient tracking system. Qualitative data collection via interviews | Estimated 71% of 10,367 referrals were electronic referrals over three years. Statistically significant improvement in referral latency without change in staffing. Clinicians appreciate shared transparency of referrals but cite usability issues as barriers. |
| Need: Curbside consults (Primary Care Physicians-Specialists) | ||||
| Bergus, 1998(54) | Observational study | Evaluation of the Email Consultation Service (ECS) for curbside consultations between family physicians and subspecialists | Descriptive statistics of usage data; survey of users | Median response time 16.1 hours; 92% of questions answered; almost 90% concerned specific patients. Both groups expressed satisfaction. |
| Abbott, 2002(55) | Observational study | Evaluation of Department of Defense “Ask a Doc” physician-to-physicians email consultation system over network of twentyone states (1998-2000) | Descriptive statistics; qualitative assessment | 3121 consultations; Average response time less than 12 hours. Minimal cost and effort to initiate and sustain. Felt to mirror clinical practice. Barriers were security and assignation of credit for consultation. |
| Need: Communication of Results (Primary Care Physicians -Specialists) | ||||
| Singh, 2007(56) | Non-randomized trial | Concurrent prospective evaluation of responses to 1017 critical imaging alert notifications in a Veterans Affairs (VA) outpatient system (2006). Radiologists generated alerts. Included receipt system. | Measured percentage of unacknowledged alerts and imaging lost to follow-up | 368 of 1017 transmitted alerts were unacknowledged (36%); forty-five were completely lost to follow-up. 0.2% outpatient imaging results lost to follow-up overall. |
| Singh, 2009(57) | Non-randomized trial | Concurrent evaluation of responses to 1196 critical imaging alert notifications in a VA outpatient system (2007-2008). Similar coding system to (56) | Measured percentage of alerts acknowledged, timely follow-up; compared electronic alerts alone to combination of alerts and phone calls or admission | Percentage of alerts acknowledged didn't differ by type of communication; combination of electronic alerts with phone follow-up (OR 0.12, p<0.001) or admission (OR 0.22, p <0.001) decreased likelihood of delayed follow-up. Alerts to two providers increased the likelihood of delayed follow-up (OR 1.99, p=0.03). |
| Abujadeh, 2009(58) | Observational study | Retrospective review of emailbased alert system for abnormal imaging results at Massachusetts General Hospital 2005-2007. Email alerting by radiologist to ordering physician of non-urgent findings. | Descriptive statistics; survey of referring physicians (12/26) | 56,691 out of 1,540,254 reports were for important but not urgent findings; 93.3% generated e-mail message (6.7% failure rate); 80% of alerts were viewed Higher satisfaction for email alerts over conventional methods (e.g., facsimile) for non-urgent but important findings. |
| Need: Communicate within 1 care setting (Primary Care Physicians) | ||||
| Lanham, 2012 (78) | Observational study | Comparison of practice-level EHR use with communication patterns among physicians, nurses, medical assistants, practice managers, and non clinical staff within individual practices in Texas | Observation and semi-structured interviews. Within-practice communication patterns were categorized as fragmented or cohesive. Practice-level EHR use was categorized as homogeneous or heterogeneous | Clinical practices with cohesive withinpractice communication patterns were associated with homogeneous patterns of practice-level EHR use. |
| Murphy, 2012 (79) | Observational study | Review of note-based messaging within the EHR in outpatient clinics of large tertiary Veterans Affairs facility. Clinic staff send “additional signature request” (ASR) alerts linked to parent notes in the EHR to primary care physicians | Reason for and origin of alerts. Parent note linked to alert was also reviewed for 3 “value attributes”: urgency; potential harm if alert was missed; subjective value to PCP of the alert | 53.7% of 525 alerts reviewed were deemed of “high value” but required PCPs to review significant amounts of extraneous text (80.3% of words in parent notes) to get relevant information. Most alerts (40%) were medication prescription or refill related. |
Extra-EHR IT
A review of electronic communication in 2000 examined electronic communication among primary care physicians but notably did not distinguish between communication and data exchange.(43) Of the thirty included publications in that review, seventeen publications “dealt with electronically communicated information in general”; the remaining studies focused on notifications of test results or transitions of care, reports from specialists, or electronic communication as “replacement of traditional referral.”(43) While many studies of electronic communication described positive benefits, few included objective data, and most did not analyze provider-to-provider communication specifically. A survey of IT use outside of the EHR in 2006 documented that approximately 30% of clinicians used email to communicate with other clinicians, fewer than those who consulted on-line journals (40.8%), but many more than those who communicated with patients by email at that time (3.6%).(44)
Intra-EHR IT
A comparison of two physician surveys of EHR use in Massachusetts (one in 2005 and the second in 2007) documented an increase in the percentage of practices with an EHR, from 23% to 35%; in those practices with EHRs, only the use of electronic prescribing increased over time. Use of secure electronic referrals or messaging including secure email remained unchanged; of note, referrals and messaging were considered a singular clinical function in that study. Between 2005 and 2007, referrals or clinical messaging were available in 62% and 63% of EHR systems respectively, and they were used most or all of the time by 29-33% of the physicians who had an EHR.(45)
Electronic referrals
Fourteen articles focused on electronic referrals. Two had a pre-post or longitudinal study design(46, 47), and five included a control group.(48-51) The rest were descriptive. In most cases, electronic referral improved the transfer of information, especially when standardized message templates were created. Use of electronic referral appeared to result in reduced waiting time for appointments and enabled more efficient triage.
Barriers to integration of electronic referral in the EHR were also assessed. An intra-EHR communication system requiring a primary care physician to integrate information emailed by the consultant into the record showed the percentage of integrated notes decreasing over time.(47) Practitioners had mixed feelings about the system; although the majority (92% of respondents) felt that the system improved patient care and wanted to extend messaging to other patient groups, they also felt that electronic messaging decreased the ease of reviewing data (83%) and confused tasks and responsibilities (59%). A study of British and Dutch electronic referral systems described significant resistance on the part of practitioners to electronic referrals, and concern on the part of specialists about the quality of referrals.(52) Another study demonstrated improvement in quality of demographic data but degradation in quality of clinical information when referrals were submitted electronically.(49) A recent transactional analysis of electronic referrals in New Zealand showed high uptake and reduced referral latency compared to conventional referral; clinicians cited usability concerns as the major barrier to use.(53)
Curbside consultations via email
Two studies evaluated curbside consultations via email and documented high provider satisfaction and rapid turnaround.(54, 55) The preliminary nature of these studies raises questions of sustainability and long-term implementation.
Results Notification
Three studies focused on test result reporting from radiologists. In these studies, a radiologist could designate a result as high priority and have an email notification sent to the ordering physicians.(56-58) Urgent results were relayed by telephone. Lack of acknowledgement of alerts impacted the results of every study, and in one of these studies, alerting two physicians, rather than just one, decreased the likelihood that the results would be followed up.(57) Providers did prefer email to fax notification.(58)
Discussion
The principal findings of the literature review underline the paucity of quantitative data surrounding provider-to-provider communication. The majority of studies focused on physicians as providers without emphasis on other provider types on the care team. Most of the quantitative studies investigated electronic referrals. Data collected largely represented measures of provider satisfaction and process measures. Few quantitative studies used established models or measures of team coordination or communication.
This study extends the work of others by compiling a comprehensive view of electronic provider-to-provider communication. A recent review of devices for clinical communication tells a part of the story (28), and our review adds a comprehensive, device-agnostic look at the systems physicians and other providers use every day.
Limitations of this review include the small number of eligible studies and a homogenous provider-type (physicians). The latter is both an important finding and a limitation to generalizability of our results. Reviewed studies were in English only. The literature review by its nature is subject to publication bias.
Intra-EHR communication cannot serve all purposes nor is it a panacea for effective care coordination. One recent qualitative study warns about the pitfalls of electronic communication. Interviews with physicians from twenty-six practices elicited some concerns about the resulting decrease in face-to-face communication that has resulted from the adoption of electronic communication tools.(32) This finding brings implications: 1) a false sense of security may reduce verbal communications when they are needed most – during emergencies or when caring for complex patients who require detailed, nuanced discussion; and 2) fewer conversations within a practice can reduce both knowledge sharing and basic social interactions necessary for the maintenance of a collaboration. Lastly, privacy and confidentiality are top priorities. Common electronic communication tools are susceptible to security breaches,(47, 59) and innovations within this domain must conform to HIPAA and HITECH regulations.(60)
While electronic communication is not a complete solution for clinical collaboration, it is difficult to use face-to-face communication and telephone communication to convey large amounts of patient information while simultaneously generating a record of the transaction. Moreover, paging functions, telephone calls, and face-to-face encounters can be highly interruptive, increasing cognitive load, burdening working memory, and shifting attention from the task at hand.(14) Interruptions contribute to inefficiency and to potential for errors.(61)
Effective coordination of care for the chronically ill is one of the essential goals of the health system; it is an ongoing process that depends on constant, effective communication. Bates and Bitton have recognized this and described the crucial role that HIT will play in creating an effective Medical Home by enumerating seven domains of HIT especially in need of research.(62) In particular, they note that effective team care and care transitions will depend on an EHR that promotes both implicit and real-time communication: “it will be essential to develop communication tools that allow practices to record goals shared by providers and patients alike, and to track medical interventions and progress.”(62)
Future research could investigate a number of open questions. Overall, an emphasis should be placed on rigorous qualitative and quantitative evaluation of electronic communication. Process measures such as length of stay, hospital readmission rates, and measures of care coordination should be framed ultimately with respect to patient health outcomes. Such data are beginning to be reported.(63)
It is unclear which types of communications would be best served within the EHR and which should remain external to it. Instant communication or “chat” has not been studied sufficiently to show a demonstrable impact on patient care. Cross coverage and team identification within the EHR can be further studied with respect to workflows and best practices. Studies using structured observation or time-and-motion analysis could provide insight into use cases and workflows that providers implement to discuss patients. Future research should incorporate established models of communication (5) and coordination (64). Data on unintended consequences or harms of provider-to-provider electronic communication have been limited, and this area should be considered in subsequent work. Finally, while the scope of this review focused on communication between providers, transformative electronic communication systems should bridge communication gaps between providers and patients, as well.
As adoption of EHRs in US hospitals has increased from 15.1% of US hospitals in 2010 to 26.6% in 2011 for any type of EHR and 3.6% to 8.7% for comprehensive EHRs, (65) it is worth noting that Meaningful Use, as it stands, incentivizes patient-provider communication, but not communication between providers. Inclusion of certification criteria focused on provider-to-provider communication may spur additional innovation.
Conclusions
The optimal features to support electronic communication between providers remain underassessed, although there is preliminary evidence for the acceptability of electronic referrals. Without better understanding of electronic communication on workflow, provider satisfaction, and patient outcomes, the impact of such tools on coordination of complex medical care will be an open question, and it remains an important one to answer.
Acknowledgments
We would like to express our gratitude to Dr. Thomas Payne, Medical Director of IT Services at the University of Washington, for sharing his expertise, and to Marina Chilov, medical librarian at Columbia University, for her assistance with the literature search. We would like to thank Paul Sun, MA, for his assistance with the literature review.
Funding Sources: 5K22LM8805 [PDS]
T15 LM007079 [CW, SC]
Footnotes
Potential Conflict(s) of Interest: Dr. Stetson serves on the advisory board of the Allscripts Enterprise EHR
References
- 1.Dunn AS, Markoff B. Physician-physician communication: what's the hang-up? J Gen Intern Med. 2009;24:437–9. doi: 10.1007/s11606-009-0913-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foy R, Hempel S, Rubenstein L, Suttorp M, Seelig M, Shanman R, et al. Meta-analysis: Effect of Interactive Communication Between Collaborating Primary Care Physicians and Specialists. Ann Intern Med. 2010;152(4):247–58. doi: 10.7326/0003-4819-152-4-201002160-00010. Epub 2010/02/17. [DOI] [PubMed] [Google Scholar]
- 3.O'Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are Electronic Medical Records Helpful for Care Coordination? Experiences of Physician Practices. J Gen Intern Med. 2009;25:177–85. doi: 10.1007/s11606-009-1195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stetson PD, McKnight LK, Bakken S, Curran C, Kubose TT, Cimino JJ. Development of an ontology to model medical errors, information needs, and the clinical communication space/ Proceedings / AMIA Annual SymposiumAMIA Symposium. 2001:672–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Coiera E. Clinical communication: a new informatics paradigm. Proc AMIA Annu Fall Symp. 1996:17–21. [PMC free article] [PubMed] [Google Scholar]
- 6.Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009 Jul;8(3):CD000072. doi: 10.1002/14651858.CD000072.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Pantilat SZ, Lindenauer PK, Katz PP, Wachter RM. Primary care physician attitudes regarding communication with hospitalists. Dis Mon. 2002;48(4):218–29. doi: 10.1016/s0011-5029(02)90029-5. [DOI] [PubMed] [Google Scholar]
- 8.Bell CM, Schnipper JL, Auerbach AD, Kaboli PJ, Wetterneck TB, Gonzales DV, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–6. doi: 10.1007/s11606-008-0882-8. Epub 2008/12/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA : the journal of the American Medical Association. 1998;280(15):1311–6. doi: 10.1001/jama.280.15.1311. Epub 1998/10/30. [DOI] [PubMed] [Google Scholar]
- 10.Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. The Medical journal of Australia. 1998;169:73–6. doi: 10.5694/j.1326-5377.1998.tb140186.x. [DOI] [PubMed] [Google Scholar]
- 11.Coiera E. When conversation is better than computation. Journal of the American Medical Informatics Association : JAMIA. 2000;7(3):277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coiera EW, Jayasuriya RA, Hardy J, Bannan A, Thorpe ME. Communication loads on clinical staff in the emergency department. The Medical journal of Australia. 2002;176(9):415–8. doi: 10.5694/j.1326-5377.2002.tb04482.x. Epub 2002/06/12. [DOI] [PubMed] [Google Scholar]
- 13.Kripliani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficit in communicaiton and information transfer between hospital-based and primary care physicians. JAMA : the journal of the American Medical Association. 2007;297:831–41. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 14.Parker J, Coiera E. Improving clinical communication: a view from psychology. Journal of the American Medical Informatics Association : JAMIA. 2000;7(5):453–61. doi: 10.1136/jamia.2000.0070453. Epub 2000/09/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Academic medicine : journal of the Association of American Medical Colleges. 2004;79(2):186–94. doi: 10.1097/00001888-200402000-00019. Epub 2004/01/28. [DOI] [PubMed] [Google Scholar]
- 16.Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The Quality in Australian Health Care Study. 1995;163:458–71. doi: 10.5694/j.1326-5377.1995.tb124691.x. [DOI] [PubMed] [Google Scholar]
- 17.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care. Annals of Internal Medicine. 2006;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 18.Shekelle PG, Morton SC, Keeler EB. Costs and benefits of health information technology. Evid Rep Technol Assess. 2006;132:1–71. doi: 10.23970/ahrqepcerta132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poon EG, Wright A, Simon SR, Jenter CA, Kaushal R, Volk LA, et al. Relationship between use of Electronic Health Record features and health care quality: Results of a statewide survey. Med Care. 2010;48:203–9. doi: 10.1097/MLR.0b013e3181c16203. [DOI] [PubMed] [Google Scholar]
- 20.Longhurst CA, Parast L, Sandborg CI, Widen E, Sullivan J, Hahn JS, et al. Decrease in Hospital-wide Mortality Rate After Implementation of a Commercially Sold Computerized Physician Order Entry System. Pediatrics. 2010;126:e1–e8. doi: 10.1542/peds.2009-3271. [DOI] [PubMed] [Google Scholar]
- 21.Kaushal R, Kern LM, Barrón Y, Quaresimo J, Abramson EL. Electronic prescribing improves medication safety in community-based office practices. J Gen Intern Med. 2010;25:530–6. doi: 10.1007/s11606-009-1238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds A. Patient-centered Care. Radiol Technol. 2009;81(2):133–47. Epub 2009/11/11. [PubMed] [Google Scholar]
- 23.Tang PC, Lansky D. The Missing Link: Bridging The Patient-Provider Health Information Gap. Health Aff. 2005;24(5):1290–5. doi: 10.1377/hlthaff.24.5.1290. [DOI] [PubMed] [Google Scholar]
- 24.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal Health Records: Definitions, Benefits, and Strategies for Overcoming Barriers to Adoption. Journal of the American Medical Informatics Association. 2006;13(2):121–6. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liederman EM, Morefield CS. Web Messaging: A New Tool for Patient-Physician Communication. Journal of the American Medical Informatics Association. 2003;10(3):260–70. doi: 10.1197/jamia.M1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prady SL, Norris D, Lester JE, Hoch DB. Expanding the Guidelines for Electronic Communication with Patients. Journal of the American Medical Informatics Association. 2001;8(4):344–8. doi: 10.1136/jamia.2001.0080344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neill RA, Mainous AG, III, Clark JR, Hagen MD. The Utility of Electronic Mail as a Medium for Patient-Physician Communication. Arch Fam Med. 1994;3(3):268–71. doi: 10.1001/archfami.3.3.268. [DOI] [PubMed] [Google Scholar]
- 28.Wu RC, Tran K, Lo V, O'Leary KJ, Morra D, Quan SD, et al. Effects of clinical communication interventions in hospitals: A systematic review of information and communication technology adoptions for improved communication between clinicians. International journal of medical informatics. 2012 doi: 10.1016/j.ijmedinf.2012.05.014. Epub 2012/06/26. [DOI] [PubMed] [Google Scholar]
- 29.Sarkar IN, Starren J. Desiderata for personal electronic communication in clinical systems. Journal of the American Medical Informatics Association : JAMIA. 2002;9(3):209–16. doi: 10.1197/jamia.M1037. Epub 2002/04/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Enrico Coiera M., BS, PhD When Conversation Is Better Than Computation. J Am Med Inform Assoc. 7:277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bates DW. Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 2010;25:174–6. doi: 10.1007/s11606-010-1252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Malley AS, Cohen GR, Grossman JM. Electronic Medical Records and communication with patients and other clinicians: Are we talking less? 2010 Contract No.: 131 (April) [PubMed] [Google Scholar]
- 33.O'Malley AS, Reschovsky JD. Referral and consultation communication between primary care and specialist physicians: finding common ground. Archives of internal medicine. 171(1):56–65. doi: 10.1001/archinternmed.2010.480. Epub 2011/01/12. [DOI] [PubMed] [Google Scholar]
- 34.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. The New England journal of medicine. 2010;363(6):501–4. doi: 10.1056/NEJMp1006114. Epub 2010/07/22. [DOI] [PubMed] [Google Scholar]
- 35.(CMS) CfMMS. EHR Incentive Program. 2012 [cited 2012 7/30/12]; Available from: https://http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html.
- 36.(CMS) CfMMS. Meaningful Use Measures. 2012 [cited 2012 7/30/12]; Available from: https://http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/EP-MU-TOC.pdf.
- 37.Programs MaM, editor. Programs MaM. Electronic Health Record Incentive Program—Stage 2, 42 CFR. 2012. [PubMed] [Google Scholar]
- 38.O'Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 25(3):177–85. doi: 10.1007/s11606-009-1195-2. Epub 2009/12/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bates DW. Getting in step: electronic health records and their role in care coordination. J Gen Intern Med. 25(3):174–6. doi: 10.1007/s11606-010-1252-x. Epub 2010/02/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jirjis J, Weiss JB, Giuse D, Rosenbloom ST. A framework for clinical communication supporting healthcare delivery. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium. 2005:375–9. Epub 2006/06/17. [PMC free article] [PubMed] [Google Scholar]
- 41.Understanding and Improving Patient Handoffs. Joint Commission Journal on Quality and Patient Safety: Joint Commission Resources. 2010:49–96. [Google Scholar]
- 42.Stein DM, Wrenn JO, Johnson SB, Stetson PD. Signout: a collaborative document with implications for the future of clinical information systems. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium. 2007:696–700. Epub 2008/08/13. [PMC free article] [PubMed] [Google Scholar]
- 43.van der Kam WJ, Moorman PW, Koppejan-Mulder MJ. Effects of electronic communication in general practice. International journal of medical informatics. 2000;60(1):59–70. doi: 10.1016/s1386-5056(00)00096-4. [DOI] [PubMed] [Google Scholar]
- 44.Grant RW, Campbell EG, Gruen RL, Ferris TG, Blumenthal D. Prevalence of basic information technology use by U.S. physicians. J Gen Intern Med. 2006;21:1150–5. doi: 10.1111/j.1525-1497.2006.00571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simon SR, Soran CS, Kaushal R, Jenter CA, Volk LA, Burdick E, et al. Physicians' use of key functions in electronic health records from 2005 to 2007: a statewide survey. J Am Med Inform Assoc. 2009;16:465–70. doi: 10.1197/jamia.M3081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Branger PJ, Wouden JCVd, Schudel BR, Verboog E, Duisterhout JS, Lei JVD, et al. Electronic Communication Between Providers Of Primary And Secondary Care. BMJ: British Medical Journal. 1992;305(6861):1068–70. doi: 10.1136/bmj.305.6861.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moorman PW, Branger PJ, van der Kam WJ, van der Lei J. Electronic Messaging Between Primary and Secondary Care: a four-year case report. J Amer Med Inform Assoc. 2001;8(4):372–8. doi: 10.1136/jamia.2001.0080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harno K, Paavola T, Carlson C, Viikinkoski P. Patient referral by telemedicine: effectiveness and cost anslysis of an intranet system. J Telemed Telecare. 2000;6(6):320–9. doi: 10.1258/1357633001935996. [DOI] [PubMed] [Google Scholar]
- 49.Shaw LJ, de Berker D. Strengths and weaknesses of electronic referral: comparison of data content and clinical value of electronic and paper referrals in dermatology. Br J Gen Pract. 2007;57(536):223–4. [PMC free article] [PubMed] [Google Scholar]
- 50.Gandhi TK, Keating NL, Ditmore M, Kiernan D, Johnson R, Burdick E, et al. Improving Referral Communication Using a Referral Tool Within an Electronic Medical Record. AHRQ Advances in Patient Safety. 2008;3:63–74. [PubMed] [Google Scholar]
- 51.Patterson V, Humphreys J, Henderson M, Crealey G. Email triage is an effective, efficient, and safe way of managing new referrals to a neurologist. Qual Safety Health Care. 2010 May; doi: 10.1136/qshc.2009.038513. Epub May 28, 2010. [DOI] [PubMed] [Google Scholar]
- 52.Dixon A, Robertson R, Bal R. The experience of implementting choice at point of referral: a comparison of the Netherlands and England. Health Econ Policy Law. 2010;13:1–23. doi: 10.1017/S1744133110000058. [DOI] [PubMed] [Google Scholar]
- 53.Warren J, White S, Day KJ, Gu Y, Pollock M. Introduction of Electronic Referral from Community Associated with More Timely Review by Secondary Services. Applied Clinical Informatics. 2011;2(4):546–64. doi: 10.4338/ACI-2011-06-RA-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bergus GR, Sinift SD, Randall CS, Rosenthal DM. Use of an e-mail curbside consultation service by family physicians. J Fam Pract. 1998;47:357–60. [PubMed] [Google Scholar]
- 55.Abbott KC, Mann S, DeWitt D, Sales LY, Kennedy S, Poropatich RK. Physician-to-physician consultation via electronic mail: the Walter Reed Army Medical Center Ask a Doc system. Mil Med. 2002;167:200–4. [PubMed] [Google Scholar]
- 56.Singh H, Arora H, Vij MS, Rao R, Khan MM, Petersen LA. Communication outcomes of critical imaging results in a computerized notification system. J Am Med Inform Assoc. 2007;14:459–66. doi: 10.1197/jamia.M2280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Singh H, Thomas EJ, Mani S, Sittig D, Arora H, Espadas D, et al. Timely follow-up of abnormal diagnostic imaging test results in an outpatient setting: are electronic medical records achieving their potential? Archives of internal medicine. 2009;169(17):1578–86. doi: 10.1001/archinternmed.2009.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Abujudeh HH, Kaewlai R, Choy G, Whelton DG, Rosenthal DI. Important imaging finding e-mail alert system: experience after 3 years of implementation. Radiology. 2009;252:747–53. doi: 10.1148/radiol.2531082217. [DOI] [PubMed] [Google Scholar]
- 59.Hindocha N. Instant Insecurity: Security Issues of Instant Messaging Symantec [Google Scholar]
- 60.J B. Secure messaging in healthcare. Tech solutions for HIPAA-compliant messaging. J AHIMA. 2008;79(6):50–1. [PubMed] [Google Scholar]
- 61.Westbrook JI, Woods A, Rob MI, Dunsmuir WT, Day RO. Association of interruptions with an increased risk and severity of medication administration errors. Archives of internal medicine. 2010;170(8):683–90. doi: 10.1001/archinternmed.2010.65. Epub 2010/04/28. [DOI] [PubMed] [Google Scholar]
- 62.Bates DW, Bitton A. The future of health information technology in the patient-centered medical home. Health Aff (Millwood) 2010;29(4):614–21. doi: 10.1377/hlthaff.2010.0007. Epub 2010/04/07. [DOI] [PubMed] [Google Scholar]
- 63.Chen AH, Murphy EJ, Yee HF., Jr eReferral--a new model for integrated care. The New England journal of medicine. 2013;368(26):2450–3. doi: 10.1056/NEJMp1215594. Epub 2013/06/28. [DOI] [PubMed] [Google Scholar]
- 64.McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol 7: Care Coordination) Rockville (MD): 2007. [PubMed] [Google Scholar]
- 65.DesRoches CM, Worzala C, Joshi MS, Kralovec PD, Jha AK. Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff (Millwood) 2012;31(5):1092–9. doi: 10.1377/hlthaff.2012.0153. Epub 2012/04/27. [DOI] [PubMed] [Google Scholar]
- 66.Reponen J, Marttila E, Paajanen H, Turula A. Extending a multimedia medical record to a regional service with electronic referral and discharge letters. J Telemed Telecare. 2004;10S:81–3. doi: 10.1258/1357633042614276. [DOI] [PubMed] [Google Scholar]
- 67.Kooijman CJ, Kaag ME. Sending specialist reports to GPs using EDI. Stud Health Tech Inform. 1998;52(Pt. 1):408–11. [PubMed] [Google Scholar]
- 68.Branger PJ, van't Hooft A, van der Wouden JC, Moorman PW, van Bemmel JH. Shared care for diabetes: supporting communication between primary and secondary care. International journal of medical informatics. 1999;53(2-3):133–42. doi: 10.1016/s1386-5056(98)00154-3. Epub 1999/04/08. [DOI] [PubMed] [Google Scholar]
- 69.Bergus GR, Emerson M, Reed DA, Attaluri A. Email teleconsultations: well formulated clinical referrals reduce the need for clinic consultation. J Telemed Telecare. 2006;12(1):33–8. doi: 10.1258/135763306775321434. [DOI] [PubMed] [Google Scholar]
- 70.Dennison J, Eisen S, Towers M, Ingham Clark C. An effective electronic surgical referral system. Ann R Coll Surg Engl. 2006;88(6):554–6. doi: 10.1308/003588406X130642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Walford S. Choose and Book. Clin Med. 2006;6(5):473–6. doi: 10.7861/clinmedicine.6-5-473. Epub 2006/11/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.John SKP, George S, Primrose JN, Fozard BJ. Validation of the Lower Gastrointestinal Electronic Referral Protocol. Brit J Surg. 2008;95:506–14. doi: 10.1002/bjs.5908. [DOI] [PubMed] [Google Scholar]
- 73.Kim Y, Chen AH, Keith E, Yee HF, Kushel MB. Not perfect, but better: Primary care providers' experiences with electronic referrals in a safety net health system. J Gen Intern Med. 2009;24:614–19. doi: 10.1007/s11606-009-0955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Scott K. The Swansea electronic referrals project. J Telemed Telecare. 2009;15:156–8. doi: 10.1258/jtt.2009.003016. [DOI] [PubMed] [Google Scholar]
- 75.Were MC, Abernathy G, Hui SL, Kempf C, Weiner M. Using computerized provider order entry and clinical decision support to improve referring physicians' implementation of consultants' medical recommendations. Journal of the American Medical Informatics Association. 2009;16(2):196–202. doi: 10.1197/jamia.M2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Singh H, Esquivel A, Sittig DF, Murphy D, Kadiyala H, Schiesser R, et al. Follow-up actions on electronic referral communication in a multispecialty outpatient setting. J Gen Intern Med. 2011;26(1):64–9. doi: 10.1007/s11606-010-1501-z. Epub 2010/09/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim-Hwang JE, Chen AH, Bell DS, Guzman D, Yee HF, Kushel MB. Evaluating Electronic Referrals for Specialty Care at a Public Hospital. J Gen Intern Med. 2010 doi: 10.1007/s11606-010-1402-1. Epub May 29, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lanham HJ, Leykum LK, McDaniel RR., Jr Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. Journal of the American Medical Informatics Association : JAMIA. 2012;19(3):382–91. doi: 10.1136/amiajnl-2011-000263. Epub 2011/08/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Murphy DR, Reis B, Kadiyala H, Hirani K, Sittig DF, Khan MM, et al. Electronic health record-based messages to primary care providers: valuable information or just noise? Archives of internal medicine. 172(3):283–5. doi: 10.1001/archinternmed.2011.740. Epub 2012/02/15. [DOI] [PubMed] [Google Scholar]


