Abstract
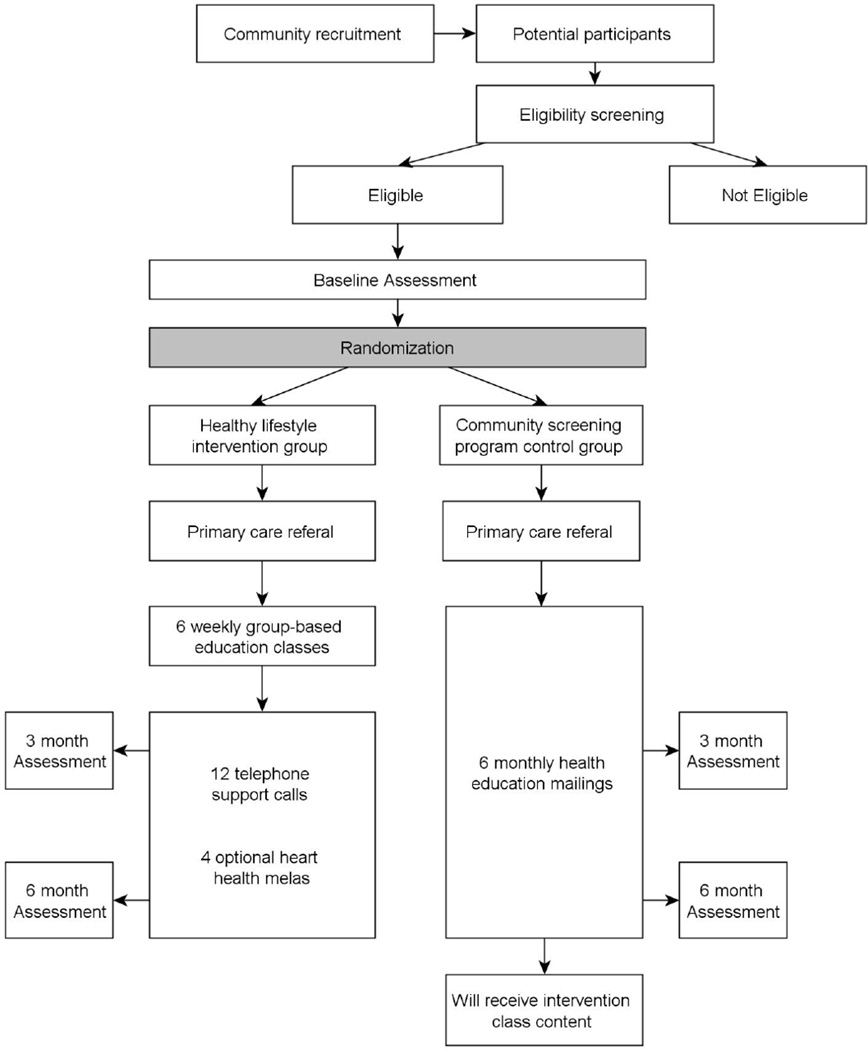
Disseminating and implementing evidence-based, cardiovascular disease (CVD) prevention lifestyle interventions in community settings and in ethnic minority populations is a challenge. We describe the design and methods for the South Asian heart lifestyle intervention (SAHELI) study, a pilot study designed to determine the feasibility and initial efficacy of a culturally-targeted, community-based lifestyle intervention to improve physical activity and diet behaviors among medically underserved South Asians (SAs). Participants with at least one CVD risk factor will be randomized to either a lifestyle intervention or a control group. Participants in both groups will be screened in a community setting and receive a primary care referral after randomization. Intervention participants will receive 6 weeks of group classes, followed by 12 weeks of individual telephone support where they will be encouraged to initiate and maintain a healthy lifestyle goal. Control participants will receive their screening results and monthly mailings on CVD prevention. Primary outcomes will be changes in moderate/vigorous physical activity and saturated fat intake between baseline, 3-, and 6-month follow-up. Secondary outcomes will be changes in weight, clinical risk factors, primary care visits, self-efficacy, and social support. This study will be one of the first to pilot-test a lifestyle intervention for SAs, one of the fastest growing racial/ethnic groups in the U.S. and one with disparate CVD risk. Results of this pilot study will provide preliminary data about the efficacy of a lifestyle intervention on CVD risk in SAs and inform community-engaged CVD prevention efforts in an increasingly diverse U.S. population.
Keywords: cardiovascular disease prevention, lifestyle intervention, randomized control trial, South Asian, culture
1. Introduction
People of South Asian descent, including Asian Indians and Pakistanis, are among the fastest growing racial/ethnic group in the U.S., with current population estimates approaching 3.4 million [1, 2]. Many studies have shown that South Asians have a 3- to 5-fold increase in the risk for myocardial infarction and cardiovascular death as compared with other ethnic groups [3–8]. Behavioral factors contribute significantly to the increased cardiovascular disease (CVD) risk observed in South Asians; among all U.S. Asians, South Asians have the highest rates of overweight/obesity [9] and report the least physical activity [10]. Clinic-based screening, lifestyle advice, and medication are key interventions to reducing CVD risk factors in individual patients [11–13]. However, evidence suggests that traditional health care system approaches are limited in their ability to influence individual health behaviors in South Asian immigrants and other ethnic minority populations because of a failure to recognize the social, cultural, and ecological context of South Asians’ CVD risk [14, 15].
Increasingly, published data support the benefits of multiple risk factor lifestyle interventions as a means to reduce CVD-related morbidity and mortality [12]. Primary prevention interventions that are focused on improving health behaviors and controlling clinical risk factors could lead to a substantial impact on South Asians’ CVD-related morbidity and mortality and inform primary prevention efforts in other racial/ethnic minority communities. However, large gaps remain in the ability to adapt and implement lifestyle interventions across diverse populations and settings [16–18]. Strategies for reaching racial/ethnic minority populations include the development of interventions that are culturally-targeted [19] as well as the use of community-based participatory research (CBPR) [15, 20].
The long-term goal of this research is to determine if a culturally-targeted, primary prevention lifestyle intervention provided to South Asian immigrants in a community-based setting will improve physical activity, dietary behaviors, psychosocial outcomes, and clinical CVD risk factors. This paper describes the active intervention group and the research design of the ongoing South Asian Heart Lifestyle Intervention (SAHELI). To the best of our knowledge, this is the first CVD prevention lifestyle intervention systematically targeted to the needs of South Asian Americans, a rapidly growing population at very high risk for CVD.
2. Study Design and Methods
2.1 Primary research goals
The primary research goals will be to pilot-test SAHELI, via a 2-arm randomized design, and examine its feasibility and initial efficacy to improve moderate/vigorous physical activity and saturated fat intake among South Asians in a community-based setting.
2.2 Participants, setting, and community engagement
The term South Asian is used to group together individuals from India, Pakistan, Bangladesh, Sri Lanka, Nepal, and Bhutan [2]. This study’s focus will be on Indians and Pakistanis, who comprise 90% of South Asians in the U.S. and in the Rogers Park neighborhood of Chicago, IL [2, 21], where this study will take place. Rogers Park is a major entry hub for immigrants [21]. Although the early wave of South Asian immigrants to the U.S. included mostly highly-educated professionals, the most recent wave includes individuals in non-professional positions who have lower education levels and limited English proficiency [1]. Rogers Park has a high proportion of medically underserved South Asian immigrants, meaning that they face economic, linguistic, and cultural barriers to health care [1]. Studies show that lower socioeconomic status and inadequate access to health care are associated with increased CVD risk and mortality [18, 22, 23]. In 2008, the research team and community partners conducted a survey in Rogers Park to assess health needs and guide planning of the intervention; 85% of South Asians from a convenience sample in Rogers Park were overweight/obese and 81% had at least one CVD risk factor [24]. Metropolitan Asian Family Services (MAFS) will be the partner community-based organization (CBO) and study site. MAFS provides social services to 1300 South Asian families, all of whom are below 100% of the federal poverty level.
This study will use a CBPR framework, meaning that the community and academic partners will collaboratively conduct research that is relevant and responsive to the needs of this South Asian community [25]. Community members and the CBO will be involved in planning and implementing SAHELI, recruiting and retaining medically underserved South Asians with limited English proficiency, and disseminating results and benefits to the local community. The study partners will build on formative community-engaged research [24, 26–29], and will conduct capacity building activities, develop a memorandum of understanding, and form a community advisory board (CAB) to provide a structure for and oversight of the partnership and research study. The CAB will be involved in study design, review of study materials and questionnaires to ensure cultural equivalence, and will also provide input on intervention content. The current project will be the partnership’s second collaborative study. Earlier work examined the socio-cultural context of South Asians’ CHD risk behaviors [24, 26–29].
2.3 Intervention design process
Culturally-targeted lifestyle interventions must target the deeper structures of culture [30, 31]. A review of primary prevention interventions targeted to minorities revealed that the most common forms of cultural targeting are matching intervention materials and messages to observable, surface characteristics of culture (i.e., language, dress, food) [30]. While this is important, because it increases audience interest and initial receptivity to messages, targeting the surface characteristics of culture is unlikely to result in behavior change [30]. Others, building on anthropological and sociological theory, have suggested that health promotion interventions are more likely to impact behavior change when interventions target the deeper structures of culture, such as the target groups’ beliefs about the causes of health and illness and their unique facilitators and barriers to behavior change [19, 31, 32].
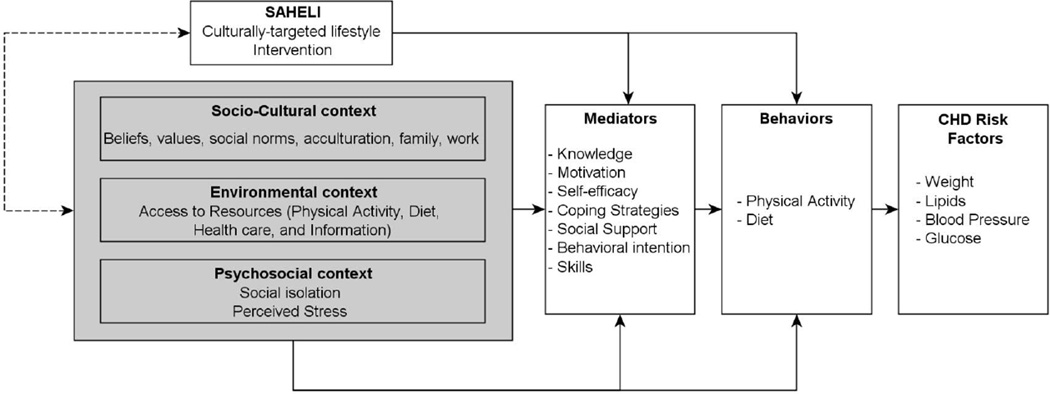
In our formative mixed-methods research [24, 26–29], we found that South Asians’ explanatory models (EMs) of coronary heart disease (CHD) differed from the biomedical model underlying most CVD prevention messages [24, 28, 29]. Although South Asians’ EMs did include unhealthy diet and physical inactivity, their EMs emphasized stress as the root cause of CHD [28]. When asked how one can prevent CHD, few talked about controlling cholesterol or blood pressure, but 40% mentioned reducing stress. In addition to being targeted to surface structures of culture (language, images), SAHELI was developed using a multi-dimensional framework (Figure 1) [33], to target the deeper structures of socio-cultural context because these were found to affect health behaviors in South Asians. For example, the study team will incorporate South Asians EMs into SAHELI by including educational content that explicitly acknowledges the role that stress plays in CVD and will develop experiential activities to help South Asians cope with and reduce stress (Figure 1).
Figure 1.
Multidimensional framework used to develop the South Asian Heart Lifestyle Intervention (SAHELI).
Adapted from: Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine. 2006;62(7):1650–1671
Socio-cultural constraints and poor social support were also found to be barriers to a healthy lifestyle in this group [26]. For example, South Asian women previously reported that they did not exercise because of gender norms, concerns about modesty, and lack of role models. SAHELI will include an exercise session where men and women will exercise separately and participate in culturally-salient exercise activities. The intervention will address the lack of social support through group-based activities, during which participants will be encouraged to learn from each other, and at the heart health melas, where participants will be asked to bring their families so they can also learn about healthy lifestyle.
2.3.1 Eligibility
The inclusion criteria will be individuals who self-identify as Asian Indian or Pakistani, 30–59 years, with at least one CVD risk factor. CVD risk factors will include: obesity (body mass index > 25 kg/m2- cutoff for obesity in South Asians) [34], hypertension (Systolic blood pressure ≥140 or diastolic blood pressure ≥ 90) [35], hyperlipidemia (Total cholesterol ≥200 or LDL cholesterol ≥130) [36], pre-diabetes (Fasting plasma glucose >100 or Hemoglobin A1c between 5.7–6.4%) [37], or diabetes (FPG>126, Hemoglobin A1c >6.4 or on diabetes medications) [37]. The exclusion criteria are listed in Table 1.
Table 1.
Exclusion criteria in the SAHELI trial.
| Specific exclusion criteria | Exclusion category and justification |
|---|---|
| Inability to speak English, Hindi, or Urdu | May interfere with the participant's ability to participate fully in the study intervention. |
| History of clinically evident CVD (e.g. heart attack, stroke) |
This is primary prevention intervention. |
| On insulin for diabetes | These individuals usually require more intensive diabetes self-management education. |
| Pregnant, lactating, or planning to become pregnant during the study period |
May influence study outcomes independently of study participation. |
| Household member enrolled in study | |
| Conditions that inhibit moderate intensity physical activity |
Indicate that study participation may be unsafe. |
| Systolic blood pressure ≥190 or diastolic blood pressure |
|
| ≥105 | |
| Triglycerides ≥ 400 | |
| Significant medical or psychiatric co- morbidities |
|
| Plans to move out of the area within 2 years | May influence the ability to obtain accurate responses to study questionnaires at follow- up. |
2.3.2 Recruitment and screening
The University Institutional Review Board approved the study protocol. CBO staff will recruit participants using fliers and outreach at community events. Study fliers will also be mailed to South Asian households on the CBO mailing list, and interested participants will be asked to call CBO staff. Study staff will also call any household that receives a mailing to determine if there is an interested participant.
Potential participants will be screened for initial eligibility by telephone. Those who are eligible and interested after the telephone interview will attend a baseline study visit at the CBO. Potential participants will be instructed to fast overnight for the baseline visit. The baseline visit will include: anthropometric assessment; fasting blood draw to measure plasma lipids and glucose; administration of survey questionnaires; and receipt of an accelerometer to track physical activity. Staff will also administer three 24-hour food recalls (including one weekend day) prior to randomization. The first food recall will be administered in-person at the baseline visit, and the second and third recalls will be completed over the telephone.
2.3.3 Randomization
All eligible participants will be randomized into one of the groups by a computer-generated list which will be maintained at the academic site. Participants will be stratified by gender in equal numbers. Within each stratum, participants will be randomized to one of the two groups, the culturally tailored lifestyle intervention group (intervention) or the control group (control). Study staff will disclose the random assignments to CBO staff who will inform the participant. After randomization, participants in the intervention group will be queried again about language preference and assigned to the group classes based on language preference. Hindi and Urdu speakers will be in one class because the spoken languages are almost identical, and the English speakers will be in another class.
Due to the nature of the intervention, complete masking of participants and study team will not be possible. To help mitigate bias, baseline data will be collected prior to randomization, and each study group will be assigned a non-revealing label for use on documents. Investigators, study staff and CBO staff were not blinded to the study hypothesis. Study participants were blinded to the study hypothesis; however, CBO staff and the CAB were concerned about the ethics of randomizing participants to a control group because this study takes place in a medically underserved community where people lack access to basic health care information and services [21]. The community partners also felt that this could decrease trust and engagement among community members. To address this, the CAB modified the study protocol such that the control group will receive the intervention classes once the final 6-month assessments are completed.
2.4 Outcome measures
Study outcome measures are listed in Table 2 along with timing of follow-up testing.
Table 2.
Study outcome measures.
| Measurement Time Point | ||||
|---|---|---|---|---|
| Measurements | Telephone Screening |
Baseline | 3-month | 6-month |
| Questionnaires | ||||
| Eligibility | ■ | |||
| Demographics | ■ | |||
| Traditional Cultural beliefs | ■ | |||
| Medical history | ■ | ■ | ||
| Medication use | ■ | ■ | ■ | |
| Primary care visits and completion of initial primary care referral |
■ | ■ | ||
| Typical Weekly Physical Activity Survey (TWPAS) [38] |
■ | ■ | ■ | |
| Social Support and Exercise Survey [40] | ■ | ■ | ■ | |
| Stress Coping survey [41] | ■ | ■ | ■ | |
| Social Network Analysis Questionnaire | ■ | ■ | ||
| Perceived Preventability of Heart Disease [24] | ■ | ■ | ■ | |
| Adverse events | ■ | ■ | ||
| 24-hour Food Recalls | ■ | ■ | ■ | |
| Accelerometers (worn for 7 days) | ■ | ■ | ■ | |
| Anthropometric and Clinical Measures | ■ | ■ | ■ | |
| Weight | ■ | ■ | ■ | |
| Height | ■ | ■ | ■ | |
| Waist circumference | ■ | ■ | ■ | |
| Blood pressure | ■ | ■ | ■ | |
| Fasting plasma lipids | ■ | ■ | ■ | |
| Fasting plasma glucose | ■ | ■ | ■ | |
2.4.1 Average minutes of moderate/vigorous physical activity
Physical activity will be calculated as the average minutes of moderate/vigorous physical activity (i.e., counts/min ≥1952) per day and will be assessed using accelerometers. Accelerometers (Actigraph, model 7164) will be worn at baseline, 3- and 6-month assessments for 7 consecutive days. The Typical Weekly Physical Activity Survey (TWPAS), adapted from the Cross-Cultural Activity Participation Study [38], will also be administered to measure time spent in and frequency of various physical activities during a typical week in the past month.
2.4.2 Dietary measurement
Percent of kilocalories from saturated fat per day will be measured using three sets of 24-hour food recalls at baseline, 3- and 6-months, including one in-person recall and two phone recalls (including one weekend day). Dietary intake data will be collected and analyzed using Nutrition Data System for Research (Version 2011, Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN.) Secondary diet outcomes will be fruit and vegetable servings and percent of kilocalories from fiber per day.
2.4.3 Anthropometric and clinical outcomes
Body weight will be measured in kilograms using a standardized, calibrated scale. Height will be measured in centimeters using a stadiometer. Three blood pressure measurements will be obtained with one-minute between measurements, using equipment and procedures that meet the recommendations for blood pressure measurement [39]. Fasting plasma lipids and glucose will be measured from a venous blood sample.
2.4.4 Psychosocial measures
Social support for physical activity behaviors will be measured using the Social Support for Diet and Exercise Behaviors scale [40]. Stress coping behaviors will be measured using an adapted version of the COPE questionnaire [41].
2.4.5 Social network analysis questionnaire
We will adapt a social network questionnaire [42] to collect data on participants’ social network characteristics and how individuals in the close, personal network influence food and physical activity preferences and constraints.
2.4.6 Feasibility measurements
Recruitment rate will be calculated as the ratio of individuals who completed a telephone screen to those who were randomized and will be compared to recruitment rates for other studies of lifestyle interventions in minority populations.
Retention rate will be calculated for the total study population and for each group separately. Program Adherence will be determined for intervention participants by measuring class attendance, completion of follow-up phone calls, and self-reported behavior goals.
2.4.7 Additional measures
Primary care visits and completion of primary care referral will be measured by self-report. CVD-related knowledge, attitudes, and perceptions will be measured using a combination of close- and open-ended questions. Descriptive data on demographics, traditional cultural beliefs scale, language preferences, years in the U.S., medical history, and current medication use will be collected. Participants will be asked to bring in all current medications, including prescriptions, over the counter, vitamins, supplements, herbals, or traditional (e.g. ayurvedic) medications. The study team and CAB will choose instruments that have been successfully used in the study team’s prior work, that are linked to the intervention’s conceptual model, and that will minimize participant burden. Instruments that have not been previously translated will be translated into Hindi and Urdu by the academic and CBO staff and reviewed by the CAB to ensure literacy-appropriateness and cultural equivalence. Study participants will receive $25 as an incentive each time they return their accelerometers at baseline, 3-, and 6-month assessments.
2.5 Study interventions
2.5.1 Linkage to primary care
After randomization, all participants (intervention and control) will be given a primary care referral by CBO staff. Uninsured participants will be referred to a federally qualified health center or other lower-cost primary care clinics located in the neighborhood. CBO staff will follow-up with all participants within 4 weeks of the baseline assessment to determine if they need assistance in making a primary care appointment.
2.5.2 Healthy lifestyle intervention
SAHELI combines standard behavioral strategies that have been shown to improve the effectiveness of lifestyle interventions [43–47] and culturally-targeted strategies [30], developed from our formative work [24, 28, 29] to help South Asians adopt healthy lifestyles and reduce CVD risk (Table 3). The culturally-targeted strategies will include implementing the intervention in a CBO-setting that is trusted and provides social services to immigrants, incorporating South Asians’ EMs of CHD, culturally-salient activities such as yoga, increasing social support through group activities and heart health melas for participants and their families, and a focus on health behavior change within the socio-cultural context of South Asian immigrants. SAHELI will be delivered by bicultural and multilingual bachelors and masters-level health educators with training, supervision, and bi-weekly feedback from a Registered Dietician (PS) and the Principal Investigator (NK). A manualized educator guide will be used to train the health educators.
Table 3.
Active ingredients of SAHELI.
| Standard evidence-based behavioral strategies [43–47] |
Culturally-targeted strategies from formative work |
|---|---|
|
|
Group classes will be held weekly for 6 weeks and last between 60–90 minutes. Each class will covers a different topic (#1: What is Heart Disease and Understanding Your Risk Factors; #2: How to Get More Exercise; #3: Eat Less Fat and Salt; #4: Enjoy Fruits, Vegetables, & Grains; #5: Maintain A Healthy Weight; #6: Taking Care of Stress and Tension). Participants will watch the video pertaining to the class topic, followed by discussion, experiential activities, goal-setting, and closing review. Classes will teach participants goal-setting techniques for creating and maintaining specific, measurable, and realistic goals [48] with attention to physical activity, diet, weight, and stress management. Participants will be taught about national physical activity (e.g. 150 minutes of moderate intensity physical activity per week) and diet (e.g. 7 servings of fruits and vegetables per day) recommendations; however, they will be encouraged to set a realistic goal based on their current behaviors and will be advised on how to gradually change their activity and diet towards recommended amounts.
Individual telephone support will start after classes end, bi-weekly for 6 weeks and then monthly for 6 weeks. Phone counseling will use a motivational interviewing framework to focus on self-reflection, behavior goals, and problem solving [49]. Calls will follow a semi-structured script, last approximately 15 minutes, and will be systematically tracked.
As part of SAHELI, there will be 4 heart health melas over the course of 12 months. Mela means 'to meet' in Hindi and Urdu and are festive gatherings that can be religious, cultural, or social. Melas will be open to intervention participants and their families and will be held at MAFS or nearby Chicago Park District locations. Because intervention groups will start at different times, participants will have the opportunity to attend 3 or 4 melas. The melas will incorporate culturally-salient activities which will be designed to reinforce healthy behaviors and increase group cohesion and support [50]. Activities will include yoga, healthy cooking demonstrations, aerobic exercise that builds on South Asian folk dance and competitions with prizes (e.g. who can make the tastiest and healthiest salad).
2.5.3 Control
The design of the control group reflects the typical protocol of many community screening programs [51]. In addition to primary care referral, participants randomized to the control group will receive their baseline screening results and monthly mailings of National Heart, Lung, and Blood Institute’s print education materials on heart disease, diet, exercise, and weight (translated into Hindi and Urdu by academic and CBO staff). Control participants will be advised to follow-up with a primary care physician for further advice. Other than assistance to make a primary care appointment, control participants will have no further contact with study staff until their follow-up assessments. This was chosen as the most appropriate and justifiable control group given that it approximates the basic education and referral that most community screening programs provide [51].
After completing the 6-month follow up testing, control participants will be offered a one-day session to cover the material from the group classes and will also receive the multimedia videos. The CBO partner and the CAB felt it was important to offer the intervention education to the control group as a way to maintain trust and study retention.
2.6 Fidelity and quality control
2.6.1 Fidelity
The study PI and research staff will complete a fidelity checklist after each class and the health educators will complete a checklist after each telephone support call. The intervention protocol will be manualized, and all intervention classes and calls will be digitally recorded. The PI (NK) and the study dietician (PS) will review 20% of randomly selected class and support call transcripts for protocol adherence using fidelity checklists and the Motivational Interviewing Treatment Integrity scale [52].
2.6.2 Quality control
All study staff will be trained to conduct study measurements using standardized study protocols. Accelerometer data will be verified for each participant after each measurement time point. Study participants who do not have sufficient data per study protocol (at least 10 hours a day for a minimum of 4 days of which one is a weekend day) will be asked to re-wear the monitor one time.
2.7 Statistical analysis
The analytic plan will be designed to compare SAHELI to the control group on feasibility and initial efficacy at 3- and 6-months following randomization. As a first step, the equivalence of the random assignment of groups with regard to key baseline characteristics will be assessed. Other analyses will include patterns of missing data, distributional properties of measures, and correlations among outcomes. If the data are non-normal, we will either make a suitable transformation or use generalized linear mixed-effects models [53]. For longitudinal analyses we will use the SAS procedures Proc MIXED and Proc NLMIXED (SAS Institute Inc. (2003), The SAS System, V. 9.2. Cary, NC).
Data will be analyzed on an intent to treat basis. We will compare retention rates between the 2 groups using a Chi-square test or Fisher’s exact test. The primary aim will be to test for differences in physical activity and % kilocalories from saturated fat by treatment group at 3- and 6-months. The basic modeling approach will be to use mixed-effects models for longitudinal data [54]. In these analyses, we will examine changes across time in order to assess the independent effects of time. In addition to the effect of time, the main independent variables will be the two treatment groups (SAHELI and control). We will examine specifically the treatment by time interaction to test whether change in physical activity and saturated fat consumption over time differs by treatment group.
The SAHELI group will be compared to the control group on change in secondary outcomes at 3- and 6- months. Analyses will mirror those described for physical activity and diet. All analyses will be performed in SAS v. 9.2 (Cary, NC) at a two-sided type I error rate of 5%.
2.8 Power calculations
In terms of power for longitudinal designs, we will use formulas [55] for comparing SAHELI versus the control group for the primary efficacy outcomes. Each treatment group will consist of 30 participants (total 60 participants). We will conservatively assume an attrition rate of 13% at the final 6-month time point (i.e., there will be at least 52 subjects at the final time point). For physical activity, we will assume a standard deviation of 91 minutes of weekly moderate activity as observed in WISEWOMAN, a lifestyle intervention for minority women [56]. For saturated fat, we will assume a standard deviation of 4.3% for daily % of kilocalories from saturated fat as observed in a study of U.S. South Asians [57]. Using an estimate from the Make Better Choices study [58], we will assume an intra-class correlation of 0.5. Based on these assumptions, with a sample size of 60, the study will have 80% power to detect a difference between treatment groups of 60 minutes of weekly moderate/vigorous activity and 2.8 daily % kilocalories from saturated fat.
3. Discussion
Advances in cardiovascular disease prevention are currently limited by the failure to translate evidence-based lifestyle interventions into high risk communities [14, 15, 46]. Increasingly, published data support the benefits of multiple risk factor lifestyle interventions for improving cardiovascular health [11] and decreasing CVD risk [12, 13, 59–61]. South Asians, who are one of the fastest growing ethnic groups in the U.S., have high CVD risk and may require special considerations when designing and implementing primary prevention lifestyle intervention programs [10, 62, 63]. The study team’s prior research [24, 28, 29] suggests that CVD prevention interventions may be more effective if they are adapted to the socio-cultural context of communities, and that clinic-based interventions may be limited in their capacity to reach underserved communities.
Despite the potential benefits of lifestyle intervention to reduce CVD risk, there is almost no research on how best to adapt these interventions for South Asians [13, 63, 64]. The SAHELI trial will use a socio-ecological framework that integrates the deeper structures of culture with evidence-based behavioral change strategies and CBPR methods to engage underserved South Asians in CVD prevention research. Few behavioral intervention trials include non-English speakers and underserved Asian Americans [13, 18, 22, 23, 47]. This innovative model can guide the dissemination and implementation of culturally-targeted interventions for other high-risk ethnic minorities. If SAHELI significantly improves physical activity and diet compared to the control group, the next step is a larger-scale comparative effectiveness trial of different approaches to reduce CVD risk and mortality in South Asian Americans. The proposed research has potential to directly inform current health care efforts to implement evidence-based lifestyle intervention in real-world settings and with diverse populations.
Figure 2.
Study overview.
Acknowledgments
Funding and Acknowledgements
This work is supported by the National Heart Lung and Blood Institute [grant number R21-HL113743]. The authors thank the community advisory board members, and Manasi Jayprakash, Selema Hamouda, Courtney Reynolds, Ankita Puri-Taneja, and Anukool Vasudevan for assistance with data collection, developing intervention materials, data entry, and technical support.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Asian American Justice Center and Asian Pacific American Legal Center. A Community of Contrasts: Asian Americans and Pacific Islanders in the United States. 2012. [Google Scholar]
- 2.South Asian Americans Leading Together. A Demographic Snapshot of South Asians in the United States. 2012 Available from: http://saalt.org/resources/reports-and-publications/#factsheets.
- 3.McKeigue PM, et al. Association of early-onset coronary heart disease in South Asian men with glucose intolerance and hyperinsulinemia. Circulation. 1993;87(1):152–161. doi: 10.1161/01.cir.87.1.152. [DOI] [PubMed] [Google Scholar]
- 4.Anand SS, Yusuf S. Risk factors for cardiovascular disease in Canadians of South Asian and European origin: a pilot study of the Study of Heart Assessment and Risk in Ethnic Groups (SHARE) Clin Invest Med. 1997;20(4):204–210. [PubMed] [Google Scholar]
- 5.Coronary heart disease risk factors vary among south asian groups. Bmj. 1999;319(7204) :B. [PMC free article] [PubMed] [Google Scholar]
- 6.Ismail J, et al. Risk factors for non-fatal myocardial infarction in young South Asian adults. Heart. 2004;90(3):259–263. doi: 10.1136/hrt.2003.013631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joshi P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 8.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14(7):499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. International Journal of Obesity. 2000;24(9):1188–1194. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- 10.Ye JL, et al. Cardiovascular Risk Factors among Asian Americans: Results from a National Health Survey. Annals of Epidemiology. 2009;19(10):718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lloyd-Jones DM, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 12.Mozaffarian D, Wilson PW, Kannel WB. Beyond established and novel risk factors: lifestyle risk factors for cardiovascular disease. Circulation. 2008;117(23):3031–3038. doi: 10.1161/CIRCULATIONAHA.107.738732. [DOI] [PubMed] [Google Scholar]
- 13.Artinian NT, et al. Interventions to Promote Physical Activity and Dietary Lifestyle Changes for Cardiovascular Risk Factor Reduction in Adults A Scientific Statement From the American Heart Association. Circulation. 2010;122(4):406–441. doi: 10.1161/CIR.0b013e3181e8edf1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woolf SH, et al. Putting it together: finding success in behavior change through integration of services. Ann Fam Med. 2005;3(Suppl 2):S20–S27. doi: 10.1370/afm.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Etz RS, et al. Bridging primary care practices and communities to promote healthy behaviors. Am J Prev Med. 2008;35(5 Suppl):S390–S397. doi: 10.1016/j.amepre.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 16.Mensah GA. Eliminating disparities in cardiovascular health six strategic imperatives and a framework for action. Circulation. 2005;111(10):1332–1336. doi: 10.1161/01.CIR.0000158134.24860.91. [DOI] [PubMed] [Google Scholar]
- 17.Mensah GA, Dunbar SB. A framework for addressing disparities in cardiovascular health. Journal of Cardiovascular Nursing. 2006;21(6):451–456. doi: 10.1097/00005082-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Mensah GA, et al. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 19.Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 20.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu. Rev. Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 21.Rangaswamy P, Kalayil AL. Making Data Count: South Asian Americans in the 2000 Census with Focus on Illinois. South Asian American Policy and Research Institute (SAAPRI); 2005. [Google Scholar]
- 22.Nazroo JY. South Asian people and heart disease: an assessment of the importance of socioeconomic position. Ethn Dis. 2001;11(3):401–411. [PubMed] [Google Scholar]
- 23.Rosengren A, et al. Education and risk for acute myocardial infarction in 52 high, middle and low-income countries: INTERHEART case-control study. Heart. 2009;95(24):2014–2022. doi: 10.1136/hrt.2009.182436. [DOI] [PubMed] [Google Scholar]
- 24.Kandula NR, et al. Knowledge gaps and misconceptions about coronary heart disease among U.S. South Asians. Am J Prev Med. 2010;38(4):439–442. doi: 10.1016/j.amepre.2009.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Minkler M. Linking science and policy through community-based participatory research to study and address health disparities. Am J Public Health. 2010;100(Suppl 1):S81–S87. doi: 10.2105/AJPH.2009.165720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kandula NR, et al. A community and culture-centered approach to developing effective cardiovascular health messages. J Gen Intern Med. 2012;27(10):1308–1316. doi: 10.1007/s11606-012-2102-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang JW, et al. South Asian American perspectives on overweight, obesity, and the relationship between weight and health. Prev Chronic Dis. 2012;9:E107. doi: 10.5888/pcd9.110284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tirodkar MA, et al. Explanatory models of coronary heart disease among South Asian immigrants. Patient Educ Couns. 2011;85(2):230–236. doi: 10.1016/j.pec.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tirodkar MA, et al. Explanatory Models of Health and Disease Among South Asian Immigrants in Chicago. Journal of Immigrant and Minority Health. 2011;13(2):385–394. doi: 10.1007/s10903-009-9304-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Netto G, et al. How can health promotion interventions be adapted for minority ethnic communities? Five principles for guiding the development of behavioural interventions. Health Promotion International. 2010;25(2):248–257. doi: 10.1093/heapro/daq012. [DOI] [PubMed] [Google Scholar]
- 31.Resnicow K, et al. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 32.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(Suppl 3):S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 33.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Social Science & Medicine. 2006;62(7):1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 34.Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 35.Chobanian AV, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 36.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 37.Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ainsworth BE, et al. Moderate physical activity patterns of minority women: The cross-cultural activity participation study. Journal of Womens Health & Gender-Based Medicine. 1999;8(6):805–813. doi: 10.1089/152460999319129. [DOI] [PubMed] [Google Scholar]
- 39.Pickering TG, et al. Recommendations for blood pressure measurement in humans and experimental animals part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 40.Sallis JF, et al. The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 41.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of personality and social psychology. 1989;56(2):267. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 42.Cornwell B, et al. Social networks in the NSHAP study: rationale, measurement, and preliminary findings. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64(suppl 1):i47–i55. doi: 10.1093/geronb/gbp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spring B, et al. Make Better Choices (MBC): Study design of a randomized controlled trial testing optimal technology-supported change in multiple diet and physical activity risk behaviors. Bmc Public Health. 2010;10 doi: 10.1186/1471-2458-10-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Glasgow RE, et al. Practical behavioral trials to advance evidence-based behavioral medicine. Annals of Behavioral Medicine. 2006;31(1):5–13. doi: 10.1207/s15324796abm3101_3. [DOI] [PubMed] [Google Scholar]
- 45.Spring B, et al. Invitation to a dialogue between researchers and clinicians about evidencebased behavioral medicine. Annals of Behavioral Medicine. 2005;30(2):125–137. doi: 10.1207/s15324796abm3002_5. [DOI] [PubMed] [Google Scholar]
- 46.Satterfield JM, et al. Toward a Transdisciplinary Model of Evidence-Based Practice. Milbank Quarterly. 2009;87(2):368–390. doi: 10.1111/j.1468-0009.2009.00561.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Greaves CJ, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. Bmc Public Health. 2011;11 doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spahn JM, et al. State of the Evidence Regarding Behavior Change Theories and Strategies in Nutrition Counseling to Facilitate Health and Food Behavior Change. Journal of the American Dietetic Association. 2010;110(6):879–891. doi: 10.1016/j.jada.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 49.Rollnick S, Miller WR, Butler C. Motivational interviewing in health care : helping patients change behavior. New York: Guilford Press; 2008. [Google Scholar]
- 50.Lee RE, et al. Mediating effects of group cohesion on physical activity and diet in women of color: health is power. Am J Health Promot. 2012;26(4):e116–e125. doi: 10.4278/ajhp.101215-QUAN-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.West B, et al. Observations and Recommendations for Community-Based Diabetes Screenings. Diabetes Educator. 2010;36(6):887–893. doi: 10.1177/0145721710386973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moyers TB, et al. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28(1):19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 53.Pinheiro JC, Bates DM. Approximations to the log-likelihood function in the nonlinear mixed-effects model. Journal of Computational and Graphical Statistics. 1995;4(1):12–35. [Google Scholar]
- 54.Hedeker D, Gibbons RD. Longitudinal data analysis. Hoboken, N.J: Wiley-Interscience; 2006. [Google Scholar]
- 55.Hedeker D, Gibbons RD, Waternaux C. Sample size estimation for longitudinal designs with attrition: Comparing time-related contrasts between two groups. Journal of Educational and Behavioral Statistics. 1999;24(1):70–93. [Google Scholar]
- 56.Keyserling TC, et al. Randomized trial of a clinic-based, community-supported, lifestyle intervention to improve physical activity and diet: The North Carolina enhanced WISEWOMAN project. Preventive Medicine. 2008;46(6):499–510. doi: 10.1016/j.ypmed.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 57.Jonnalagadda SS, Diwan S. Nutrient intake of first generation Gujarati Asian Indian immigrants in the US. Journal of the American College of Nutrition. 2002;21(5):372–380. doi: 10.1080/07315724.2002.10719238. [DOI] [PubMed] [Google Scholar]
- 58.Spring B, et al. Multiple Behavior Changes in Diet and Activity A Randomized Controlled Trial Using Mobile Technology Behavior Changes in Diet and Activity. Archives of internal medicine. 2012;172(10):789–796. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Angermayr L, Melchart D, Linde K. Multifactorial Lifestyle Interventions in the Primary and Secondary Prevention of Cardiovascular Disease and Type 2 Diabetes Mellitus-A Systematic Review of Randomized Controlled Trials. Annals of Behavioral Medicine. 2010;40(1):49–64. doi: 10.1007/s12160-010-9206-4. [DOI] [PubMed] [Google Scholar]
- 60.Elmer PJ, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-Month results of a randomized trial. Annals of Internal Medicine. 2006;144(7):485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 61.Maruthur NM, Wang NY, Appel LJ. Lifestyle Interventions Reduce Coronary Heart Disease Risk Results From the PREMIER Trial. Circulation. 2009;119(15) doi: 10.1161/CIRCULATIONAHA.108.809491. p. 2026-U24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sriskantharajah J, Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help? Family practice. 2007;24(1):71–76. doi: 10.1093/fampra/cml066. [DOI] [PubMed] [Google Scholar]
- 63.Daniel M, Wilbur J. Physical Activity Among South Asian Indian Immigrants: An Integrative Review. Public Health Nursing. 2011;28(5):389–401. doi: 10.1111/j.1525-1446.2010.00932.x. [DOI] [PubMed] [Google Scholar]
- 64.Patel M, Phillips-Caesar E, Boutin-Foster C. Barriers to lifestyle behavioral change in migrant South asian populations. J Immigr Minor Health. 2012;14(5):774–785. doi: 10.1007/s10903-011-9550-x. [DOI] [PMC free article] [PubMed] [Google Scholar]