Abstract
A subject-specific step counting method with a high accuracy level at all walking speeds is needed to assess the functional level of impaired patients. The study aim was to validate step counts and cadence calculations from acceleration data by comparison to video data during dynamic activity. Custom-built activity monitors, each containing one tri-axial accelerometer, were placed on the ankles, thigh, and waist of 11 healthy adults. ICC values were greater than 0.98 for video inter-rater reliability of all step counts. The activity monitoring system (AMS) algorithm demonstrated a median (interquartile range; IQR) agreement of 92% (8%) with visual observations during walking/jogging trials at gait velocities ranging from 0.1 m/s to 4.8 m/s, while FitBits (ankle and waist), and a Nike Fuelband (wrist) demonstrated agreements of 92% (36%), 93% (22%), and 33% (35%), respectively. The algorithm results demonstrated high median (IQR) step detection sensitivity (95% (2%)), positive predictive value (PPV) (99% (1%)), and agreement (97% (3%)) during a laboratory-based simulated free-living protocol. The algorithm also showed high median (IQR) sensitivity, PPV, and agreement identifying walking steps (91% (5%), 98% (4%), and 96% (5%)), jogging steps (97% (6%), 100% (1%), and 95% (6%)), and less than 3% mean error in cadence calculations.
Keywords: Accelerometer, step detection, body-worn sensors, gait velocity
1. Introduction
Physical inactivity is an independent risk factor for chronic disease and disability and is estimated to result in 3.2 million deaths world-wide each year [1]. Regular physical activity has been associated with health improvements in many populations [2]. Many commonly used mobility assessment methods have limitations such as subjectivity [3] or involve clinical-based evaluations that fail to mimic real-world functional requirements, such as the 10 m walk test which underestimates gait velocity predictions in a community setting [4]. It is important to quantitatively assess mobility in the free-living environment as health and wellness measure. This can be accomplished with accurate measurement of step counts and cadence in the home and community.
Step counting is one of the most commonly used measures of physical activity [5]. Sensors can provide objective information on movement while their small size and light weight allow for home deployment. One of the main issues associated with step counts as a physical activity measure is that high accuracy is needed. Many previous studies have assessed the step count and gait event accuracy of pedometers, accelerometers, and gyroscopes [6–11]. However, limited information on the algorithms and the data analysis methods are provided and the protocols performed are overly simplified, often consisting of long periods of continuous walking which are inconsistent with most daily living activities. The step detection accuracy of many sensors has also been shown to decrease for shorter activity duration and at slower walking speeds [8, 12–14], particularly in older patients. The need for accurate step counts at slow walking speeds is of critical importance as slow walking speeds can be indicative of movement disorders [15], mobility disability [16], and have been linked to high risk for reduced function, morbidity, and mortality [17]. Increases in walking speed and the ability to vary cadence demonstrate increased function level [18], reduced risk, and higher predictions of survival [17, 19]. While a small number of studies have shown that results from the methods they used are not affected by different walking speeds, accuracy during shuffling, stair climbing, and jogging have yet to be investigated and only limited gait velocity ranges are examined [14, 20, 21]. Furthermore, the use of step counts as a measure of physical activity is limited as the characteristics of the steps are unknown. An activity monitoring system (AMS) capable of identifying walking step counts, jogging step counts, and the ability to vary cadence while walking and jogging can be beneficial as it gives information on an individual’s functional level. Furthermore, an objective portable method for the functional assessment of patients, particularly those with slow walking speeds, could serve as a beneficial motivational rehabilitation tool and an effective clinical outcomes measure in the free-living environment.
The aim of this study was to determine the validity and reliability of a custom-designed AMS as an objective adaptive step counter. The algorithm’s accuracy was validated with visual step counts and was compared to two commercial step counters (Fitbit Tracker (Fitbit, San Francisco, CA) and Nike+ Fuelband (Nike, Beaverton, OR)) during walking and jogging trials at a range of gait velocities. The validity and reliability of the AMS algorithm were also evaluated for walking and jogging segments in healthy adults during a protocol of simulated free-living dynamic activities in the laboratory by comparison to video recordings.
2. Materials and Methods
2.1 Experimental Design
Accelerometer and video data were acquired from 12 (3 M, 9 F) healthy adults as they performed 7 to 10 walking/jogging trials in a straight line over an 8.5 m walkway (with additional room to accelerate and decelerate). Subjects wore two different commercial devices (Fitbit monitors on the right lateral ankle and the waist and a Nike Fuelband on the right wrist) in addition to the AMS which consisted of accelerometers below the navel on the waist, on the right thigh lateral midpoint, and bilateral ankles. Gait velocities were calculated based on the distance travelled and the time duration recorded by photocells placed at either end of the walkway. For the initial trial, subjects were asked to walk at a self-selected normal gait velocity. Following each trial, subjects were given instructions to walk/jog at a slower/faster speed, until a suitable range of gait velocities was obtained. The steps were counted visually by two raters. A total of 105 trials were recorded in total. Accelerometer and video data were also recorded as subjects performed an approximately 5 minute protocol of static and dynamic activities involving standing, sitting, lying, postural transitions, walking, stair climbing, and jogging in the laboratory [22]. Verbal cues were provided by an investigator for each task. Additionally, subjects were asked to fidget to simulate activity during selected sitting and standing tasks. All activities were performed at self-selected speeds. At the time of evaluation, the subjects’ median (range) age and average (SD) body mass index (BMI) were 31 (25–55) years, and 24.7 (5.5) kg·m−2, respectively. Exclusion criteria were a history of musculoskeletal deficits, neurological impairment, or lower extremity surgery. The study protocol was approved by the Mayo Clinic Institutional Review Board and each subject provided written informed consent before participating.
2.2 Data Collection
The AMS consisted of four Mayo Clinic custom-built activity monitors which were secured with straps. Each activity monitor incorporated a tri-axial MEMS accelerometer (analog, ±16g, Analog Devices), and onboard data storage of up to 0.5 GB [22]. Monitors were programmed to sample each axis at 100 Hz. Video data were simultaneously acquired at 60 Hz using a handheld camera. Video data were synchronized to accelerometer data by three vertical jumps performed by subjects prior to and following the described protocol. The four accelerometers were also synchronized to each other after the final jump.
2.3 Signal Processing
Step numbers and heel-strike timings for AMS step detection were determined from the bilateral ankle activity monitors (Figure 1). All accelerometer data post-processing and analysis were performed offline using MATLAB (Version 7.11.0, Mathworks, Natick, MA). A median filter, with a window size of 3, was applied to the orthogonal raw acceleration signals to remove any high-frequency noise spikes. The resulting filtered signal was separated into its gravitational component using a third-order zero phase lag elliptical low pass filter, with a cut-off frequency of 0.25 Hz, 0.01 dB passband ripple and −100 dB stopband ripple. Subtracting the gravitational component from the original median filtered signal provided the bodily motion component [23].
Figure 1.
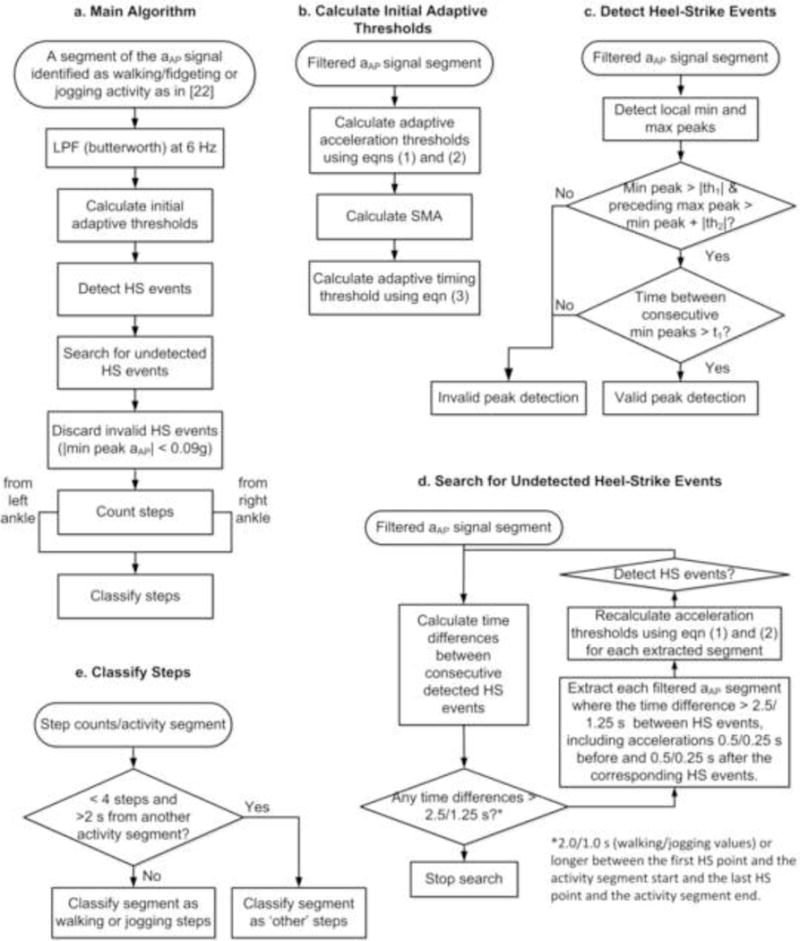
Flowchart of the step detection algorithm applied to the acceleration values of each segment of dynamic activity detected from the postural and activity detection algorithm. (a) shows the main stages of the algorithm, (b) – (e) describe the algorithm in additional detail. HS: heel-strike, LPF: low pass filter, aAP: anteroposterior acceleration.
2.4 Activity Detection
In a parallel study by the authors [22], dynamic activity was detected by calculating when the signal magnitude area (SMA) of the bodily motion component of the waist accelerometer data exceeded a threshold of 0.135 g [24] for epochs of 1 s. Of those seconds of data (which were below 0.135g) identified as non-activity, a continuous wavelet transform using a Daubechies 4 Mother Wavelet was applied to the waist acceleration signal. Data which fell within a range of 0.1–2.0 Hz was further identified as activity, if it exceeded a scaling threshold of 1.5 over each second [22]. Upright activity was identified using the angles estimated from the waist and thigh accelerometers. Activity was characterized as jogging when the SMA exceeded 0.8 g and as walking (including stair climbing and fidgeting of the feet while standing) when the SMA was between 0.135 g and 0.8 g. The threshold of 0.8g was determined from this dataset [22], based on comparisons of SMA to video data for a single subject and validated across all subjects.
2.5 Step Detection
During identified walking and jogging segments, the anteroposterior accelerations (aAP) of the ankles were filtered using a low-pass butterworth filter with a cut-off frequency of 6 Hz and analyzed using a peak detection method [9] with adaptive aAP thresholds similar to those previously formulated for angular velocity [20] and an adaptive timing threshold to calculate the number of steps taken (Figure 1).
Gait events, gait velocity, and cadence are useful when describing normal and pathological gait [25]. Step counting methods are often based on toe-off, heel-strike, and/or midswing identification with defined absolute thresholds determining the acceleration values these gait events must reach and how much time must lapse between consecutive gait events to identify valid steps [9]. As gait velocity, cadence, and swing phase usually decrease with increasing disability, the gait event accelerations also decrease and the time between gait events increases [25]. These parameter changes can cause accuracy issues when using absolute thresholds to assess subjects with slower/pathological gait velocities. Even within-subject gait velocity changes can reduce accuracy, i.e. walking slowly while performing household chores, may result in activity underestimation [26]. To overcome these issues, our algorithm incorporates adaptive thresholds for acceleration and time between gait events.
Calculate Initial Adaptive Thresholds (Figure 1b)
The adaptive peak detection thresholds allow for greater step detection accuracy at different walking speeds. For each continuous data segment classified as walking or jogging, adaptive aAP thresholds to detect heel-strike points were calculated,
| (1) |
where is the mean of the aAP signal and N is the number of samples,
| (2) |
In addition to adaptive aAP thresholds, adaptive timing thresholds were also calculated. The timing threshold, t1, was calculated for each walking segment using
| (3) |
where fs is the sampling frequency and SMA is the signal magnitude area of the waist. A minimum value for t1 was set at 0.5 s.
Detect Heel-Strike Events (Figure 1c)
Local minimum and maximum peaks of the aAP signal were detected. Local minimum peaks were considered valid heel-strike points if their magnitudes were greater than |th1| g, and had a preceding maximum whose magnitude was at least |th2| g greater than the minimum. If two minimum peaks were found within t1 s of each other for walking and 0.25 s of each other for jogging, only the one of greater amplitude was considered as a heel-strike point.
Search for Undetected Heel-Strike Events (Figure 1d)
Adaptive thresholds do not work well when high heel-strike acceleration variability occurs. In order to address this issue of activity with high heel-strike acceleration variability (particularly during walking segments which included stair climbing), the algorithm was extended to check for missing steps in each segment of data by calculating the time difference between each successive heel-strike point. For walking, if there was a time interval of 2.5 s or longer between successive heel-strike points (2.0 s or longer between the first heel-strike point and the start of the activity segment and the last heel-strike point and the end of the activity segment), the acceleration thresholds (equations (1) – (2)) were recalculated for the segment of data within 0.5 s from either heel-strike point and new heel-strike points were looked for within that segment. For jogging, if the time interval was 1.25 s or longer between successive heel-strike points (1 s or longer between the first heel-strike point and the start of the activity segment and the last heel-strike point and the end of the activity segment), the acceleration thresholds were recalculated for the segment of data within 0.25 s from either heel-strike point and new heel-strike points were sought within that segment.
Discard Invalid Heel-Strike Events
Activity monitor acceleration readings are accurate to within 0.09 g. Therefore, any heel-strike points with aAP magnitudes less than 0.09 g were discarded.
Count Steps
For each activity segment, steps counts from both the right and left ankle acceleration data were summed.
Classify Steps (Figure 1e)
To identify walking or jogging steps from other less meaningful steps such as fidgeting, a previous study ignored any activity which lasts for less than five seconds [27]. However, discarding five second activity segments in this study could mean ignoring as high as 15 steps per activity segment. Another study recommended discounting steps if less than two steps with the right leg occur in a ten second window and no steps occur in the ten second windows on either side [28]. Applying this method to the present study resulted in the classification of all fidgeting and walking segments with less than four steps were classified as ‘walking’ which resulted in an overestimation in walking step counts. In this study, any segments with less than four steps total detected from the right and left ankles which were preceded and followed by more than two seconds of no activity were not considered as walking or jogging and their steps were categorized as ‘other’. The two seconds threshold was chosen to account for possible activity classification errors at the first and last one second epochs of activity segments [22]. This characterization was also applied to video observation.
Calculate Cadence
Cadence was calculated from
| (4) |
where n is the total number of steps in the activity segment, tn is the time (min) when the heel-strike point of the nth step occurs and t1 is the time (min) when the heel-strike point of the first step occurs.
2.6 Reliability
Video data were imported into Windows Movie Maker (Microsoft, Seattle, WA). Two raters, each with greater than one year of gait analysis experience, manually determined the walking, jogging and ‘other’ step counts for each activity. The video data were considered the gold standard for all validation analysis. Intraclass correlations (ICC(A,1)) across all subjects were used to determine the reliability of inter-rater observations [29].
2.7 Validity
AMS algorithm step counts were validated against the steps counted manually from the video data for each subject. Agreement is the percentage of steps detected using the AMS algorithm compared with those counted manually from the video data. Sensitivity is the ratio of true positives to the total number of true positives and false negatives. Positive predictive value (PPV) is the ratio of true positives to the total number of true positives and false positives. Heel-strike times (i.e. times at which the non-stance leg made contact with the floor) were visually identified to calculate cadence from the video data and sensitivity, PPV, and agreement were used to assess the AMS algorithm’s ability to accurately detect steps. The AMS algorithm, Fitbits, and Nike Fuelband accuracies were compared using agreement values only.
The Bland-Altman and ICC(A,1) methods were utilized to compare step counts and cadence as determined by the AMS algorithm and video observation [30]. In the Bland-Altman plots, systematic error is present if the mean is greater than or less than zero. Systematic error is considered to be significant if both repeatability coefficients are on the same side of zero.
3. Results
Eleven of the twelve participants completed the protocol as prescribed. Data from one subject were excluded since the protocol was not followed correctly. The total time to complete the protocol of static and dynamic activities averaged (SD) 359 (42) s and the mean (SD) total number of steps taken was 282 (20).
3.1 Reliability
Inter-rater reliability of step detection using video observation was high, with ICC(A,1) values of 1 for the walking/jogging trials and greater than 0.98 for steps taken during walking, steps taken during jogging and the total number of steps taken throughout the simulated free-living protocol (Table 1). All further analyses were performed comparing AMS algorithm identification to a single observer chosen at random.
Table 1.
Inter-rater reliability for the 5 minute protocol of static and dynamic activities
| Task | Rater 1a | Rater 2 a | ICC(A,1) b |
|---|---|---|---|
| Walking | 195.0 (16.4) | 196.7 (17.1) | 0.982 (0.919, 0.996) |
| Jogging | 86.5 (13.7) | 87.0 (12.6) | 0.988 (0.956, 0.997) |
| All Activity | 281.5 (19.7) | 283.7 (19.9) | 0.981 (0.907, 0.995) |
Average (SD) total step count for each activity as determined by two raters.
Values provided are the estimated ICC(A,1) with lower and upper bounds for the 95% confidence interval (McGraw and Wong, 1996).
3.2 Validity
The AMS algorithm demonstrated a median (IQR) agreement of 92% (8%) with manual step counts as gait velocities ranged from 0.1 m/s to 4.8 m/s compared with median (IQR) agreements of 92% (36%), 93% (22%), and 33% (35%) using Fitbit (ankle), Fitbit (waist), and Nike Fuelband (wrist), respectively (Figure 2). The AMS algorithm median agreement was highest for gait velocities lower than 0.5 m/s (Table 2). The lowest median (IQR) agreements occurred between 1.0 and 1.5 m/s and 1.5 and 2.0 m/s, both at 89% (7%). For gait velocities ranging from 0.1 m/s to 4.8 m/s, step counts were underestimated by a mean of 1.5 steps and there was no significant systematic error (Figure 3). The ICC(A,1) value was greater than 0.97. Four of the five outliers occurred at gait velocities less than 0.62 m/s due mostly to very low ankle peak aAP as well as due to some seconds of activity not being detected. The fifth outlier occurred at approximately 1.25 m/s due to missed seconds of activity. The Fitbit demonstrated higher median agreement values than the AMS algorithm between 0.5–2 m/s but didn’t detect steps for velocities less than 0.5 m/s when located on the waist and detected only approximately 50% of steps for velocities less than 0.5 m/s and greater than 2 m/s when located on the ankle.
Figure 2.
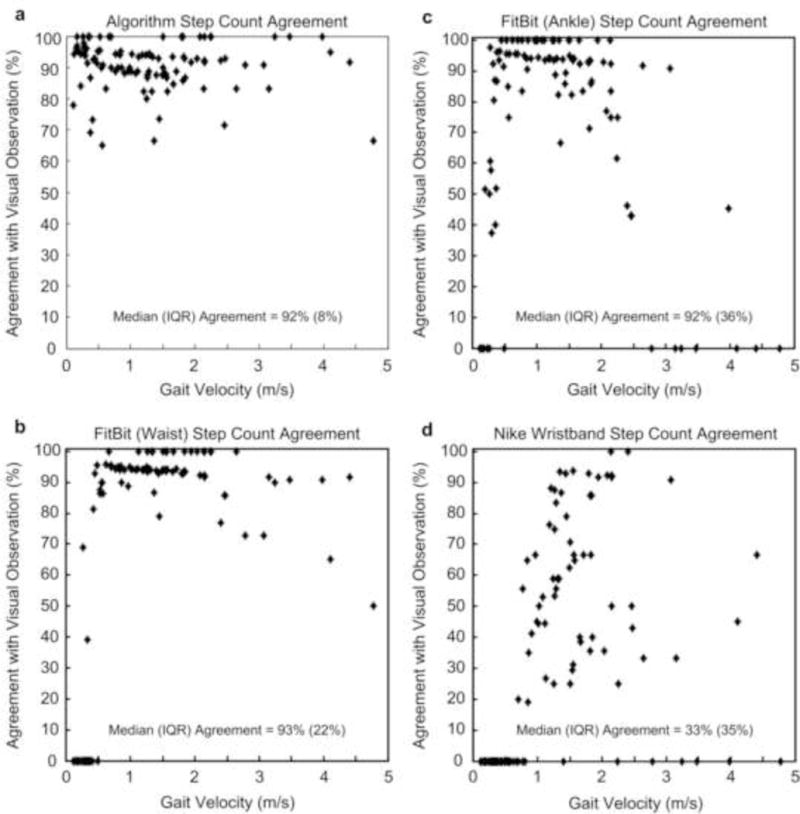
Step count agreement with visual observations for (a) the activity monitoring system algorithm, (b) Fitbist located at the right lateral ankle, (c) Fitbit located at the waist, and (d) Nike Fuelband worn on the wrist as gait velocity ranges from 0.1 m/s to 4.8 m/s.
Table 2.
Median (IQR) agreement of algorithm, Fitbit (ankle), Fitbit (waist) and Nike Fuelband step counts compared with visual, and median (IQR) number of steps for different gait velocity ranges
| Gait Velocity Range (m/s) | < 0.5 | 0.5 – 1.0 | 1.0 – 1.5 | 1.5 – 2.0 | > 2.0 |
|---|---|---|---|---|---|
| Activity Monitor (%): | 95 (6) | 90 (6) | 89 (7) | 89 (7) | 92 (11) |
| Fitbit (Ankle) (%): | 52 (91) | 96 (6) | 94 (11) | 93 (7) | 46 (85) |
| Fitbit (Waist) (%): | 0 (0) | 94 (5) | 94 (1) | 94 (7) | 92 (16) |
| Nike Fuelband (%): | 0 (0) | 0 (41) | 59 (33) | 66 (47) | 43 (91) |
| Number of Steps: | 31 (14) | 20 (4) | 17 (2) | 15 (1) | 12 (5) |
Figure 3.
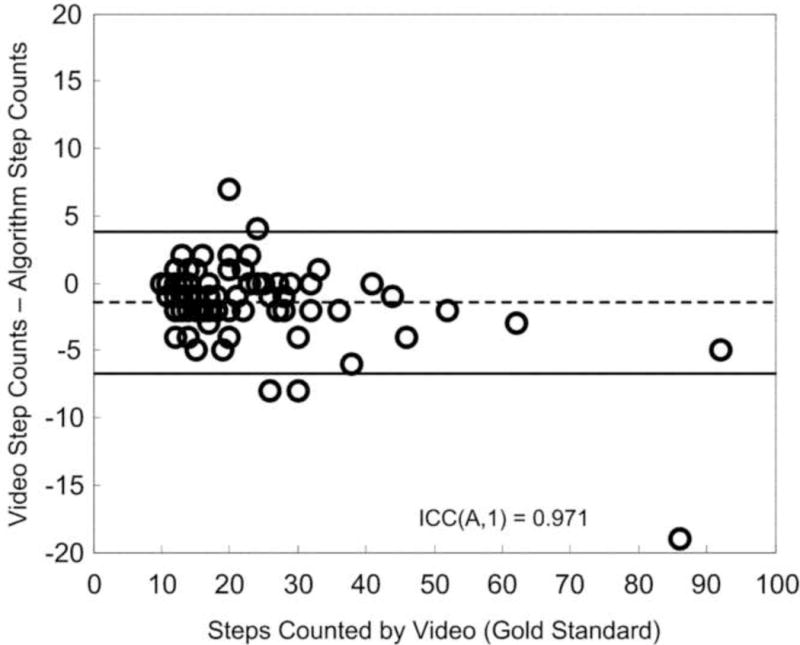
Bland Altman plot demonstrating the difference between the activity monitoring system algorithm and visual step counts as the number of steps taken changes (as a result of changes in gait velocity). The dashed line is the mean, while the solid lines represent the repeatability coefficient (± 1.96 SD).
Steps were detected for each upright dynamic activity segment during the protocol for each subject and were classified as walking (Figure 4a and b), jogging (Figure 4c), or other. Stair walking demonstrated high variability of peak accelerations (Figure 4a). The number of steps taken for each segment ranged from 2 to 115. For the group, step detection median (IQR) sensitivity was 95% (2%) across subjects, with 91% (5%) for walking and 97% (6%) for jogging (Figure 5a). The step detection median (IQR) PPV was 99% (1%) across subjects, with 98% (4%) for walking and 100% (1%) for jogging (Figure 5b). The step detection median (IQR) agreement was 97% (3%), with 96% (5%) for walking and 95% (6%) for jogging. The step counts from the AMS algorithm showed good agreement when compared to video data (ICC(A,1) values greater than 0.75) except for steps classified as ‘other’ (ICC(A,1) value was 0.4) (Figure 6). No significant systematic errors were present. Mean percentage errors were approximately 5% for all walking segments, 1% for the longest walking segment on level ground and stairs, 3% for the longest walking segment on level ground, 3% for all jogging segments, 4% for all activity combined and 63% for other. The median (IQR) sensitivity, PPV, and agreement, and ICC(A,1) values increased from 91% (5%), 98% (4%), 96% (5%), and 0.75 for all walking (Figure 5a, 5b, and 6a) to 96% (2%), 99% (3%), 97% (2%), and 0.97 for the longest walking segment on both level ground and stairs (Figure 5a, 5b and 6b) and to 97% (4%), 100% (0%), 97% (5%), and 0.93 for the longest walking segment on level ground only (Figure 5a, 5b, and 6c). The calculated mean cadences were 103 steps/min for walking on level ground, 102 steps/min for walking on level ground and stairs, and 155 steps/min for jogging. Correlations between video observation and AMS algorithm identification were high for cadence calculations (ICC(A,1) values greater than 0.82) and showed excellent agreement across all subjects for the longest walking segment on level ground, the longest walking segment on both level ground and stairs and the two jogging segments (Figure 7). No significant systematic errors were present and mean percentage errors were less than 1% for walking on level ground (except for one outlier), 3% for the first jogging segment (except for one outlier), 2% for walking on level ground and stairs (except for one outlier), and 3% for the second jogging segment (except for one outlier).
Figure 4.
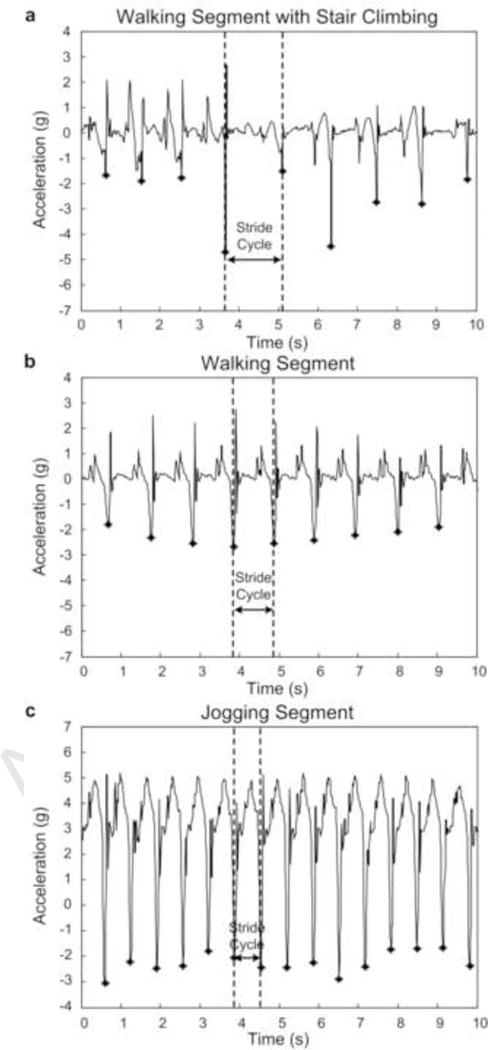
Sample of 10 s duration of right ankle anteroposterior accelerations for one representative subject from the longest identified (a) walking (on flat ground and during stair climbing), (b) walking (on flat ground), and (c) jogging segments. Each heel-strike detected using peak detection with adaptive thresholds is denoted with an asterisk.
Figure 5.
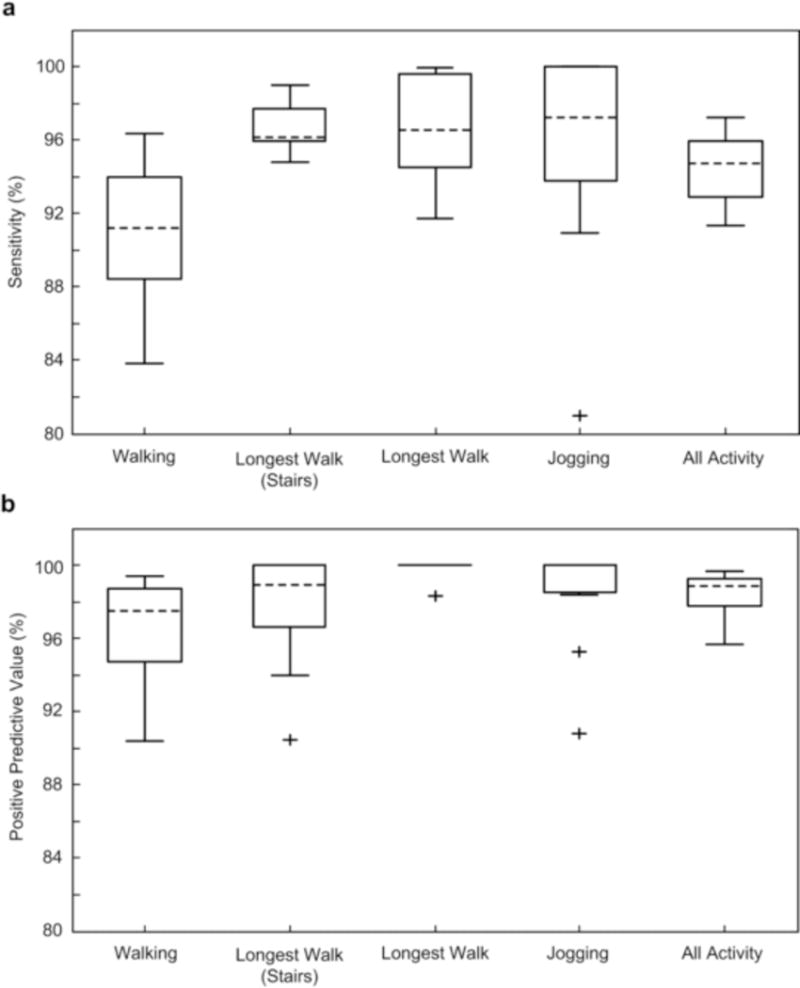
Step detection sensitivity (A) and positive predictive value (B) when identifying all walking steps, walking steps during the longest activity segment which includes stair climbing, walking steps during the longest activity segment on flat ground only, jogging steps, and the total number of steps compared to video identification. The central line represents the median, the edges of the box are the 25th and 75th percentiles, and the whiskers extend to ± 1.5 of the interquartile range. Outliers beyond this range are labeled as +. For the PPV of jogging, the median value is equal to 100%. For the PPV of the longest walking segment on level ground, the median value, the 25th and 75th percentiles are equal to 100%.
Figure 6.
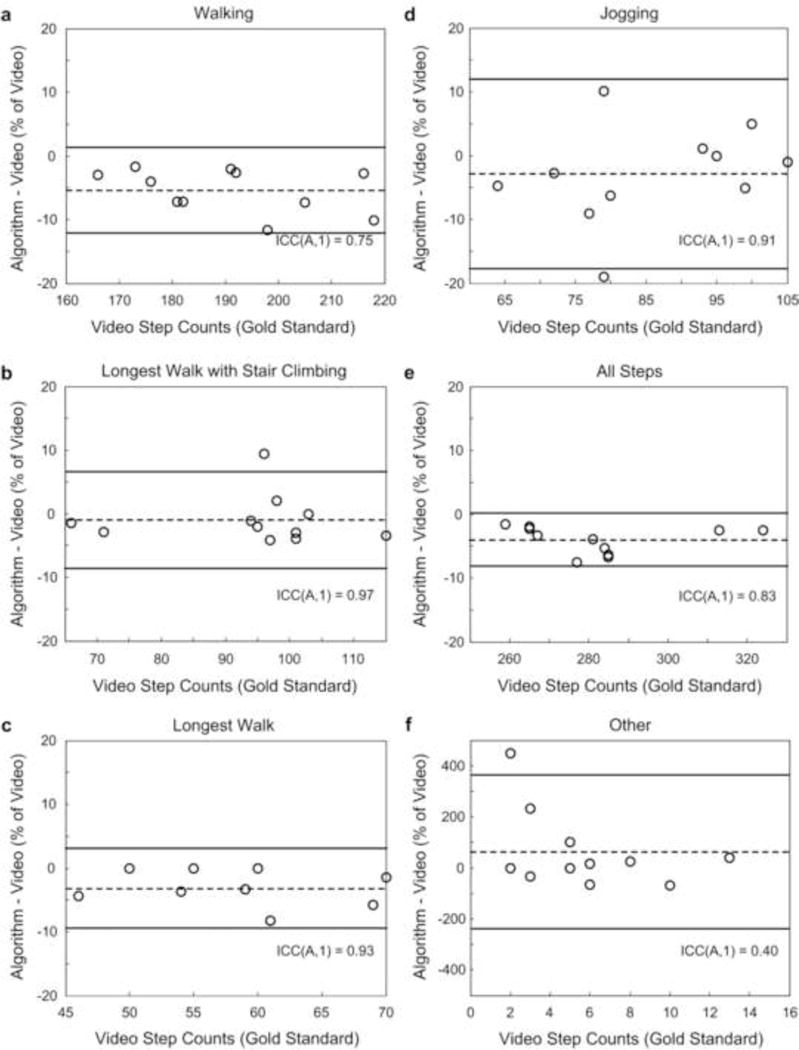
Bland-Altman plots demonstrating percentage difference for step detection when using activity monitoring system algorithm and video identifications for (a) walking, (b) walking during the longest activity segment including stair climbing, (c) walking during the longest activity segment on level ground only, (d) jogging, (e) the entire protocol, and (f) all steps classified as ‘Other’. The dashed line represents the mean, while the solid lines represent the repeatability coefficients (± 1.96 SD). ICC(A,1) values are also presented.
Figure 7.
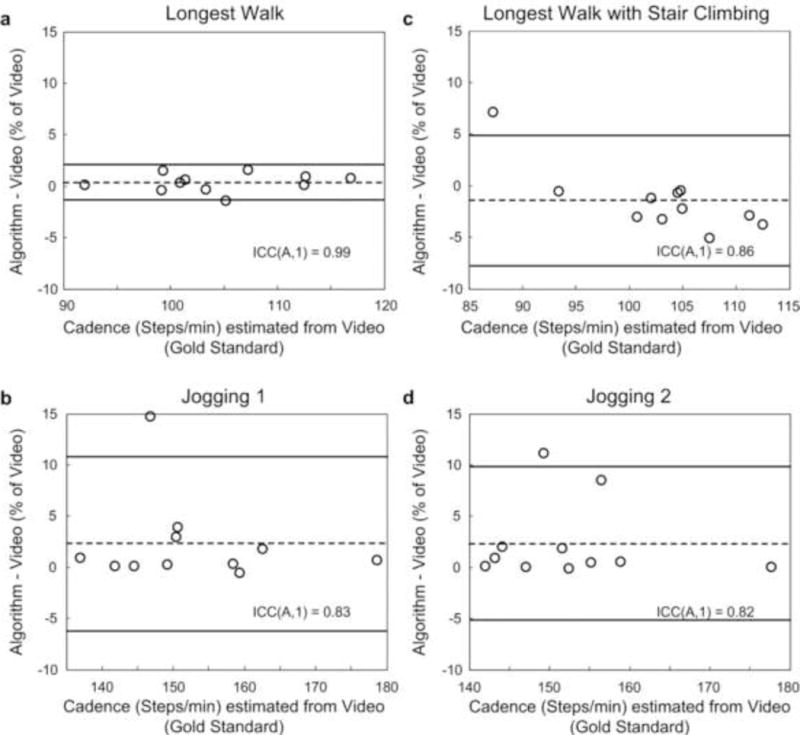
Bland-Altman plots demonstrating percentage difference for cadence when using activity monitoring system algorithm and video identifications for (a) the longest walking segment on level ground, (b) the first jogging segment, (c) the longest walking segment including stair climbing, and (d) the second jogging segment. The dashed line represents the mean, while the solid lines represent the repeatability coefficients (± 1.96 SD). ICC(A,1) values are also presented.
4. Discussion
The study aim was to validate an algorithm using an AMS to measure step counts and cadence during walking and jogging for a wide range of gait velocities. There is a need for an accurate objective step counter for patients with slow walking speeds as they would benefit most from a motivational tool capable of accurately monitoring activity increases. The described step detection algorithm incorporates an adaptive acceleration threshold heel-strike detection algorithm capable of managing activity segments with high acceleration variability and includes adaptive timing thresholds for robustness across a large gait velocity range. The step detection algorithm was used in combination with a postural and activity detection algorithm so that only upright dynamic activity was analyzed and to enable the data analysis of a protocol with a continuous flow of static and dynamic activities such as would occur in free-living.
The small discrepancies between the two video raters (Table 1) were due to subjective differences in deciding which steps taken during fidgeting could be classified as valid steps and deciding when the activity switched between walking and jogging. With some subjects, step counts were less accurate, mostly due to small inaccuracies of walking and jogging segment detection at the beginnings and ends (walking detection median (IQR) sensitivity was 87% (7%) and PPV of 95% (3%), while jogging detection median (IQR) sensitivity was 97% (7%) and PPV of 100% (2%)) [22], resulting in one or more missing steps. These inaccuracies can be attributed to the segmentation of both the accelerometer and video data to one second windows when identifying dynamic upright activity.
For gait velocities from 0.1 to 4.8 m/s, the AMS algorithm detected steps with a higher median agreement and/or smaller IQR than the Fitbits and Nike Fuelband (Figure 2, Table 2). Furthermore, Fitbit does not incorporate postural detection and may overestimate steps in free-living from leg movement during sitting and lying in addition to upright posture. Nike Fuelband agreement was poor across all velocities and also includes no postural detection. Previous studies have also reported difficulties in obtaining accurate step counts at slow and high walking speeds [8, 14, 31, 32]. A small number of studies report good accuracy for all walking speeds [14, 20, 21, 31]. However, many of these studies do not specify gait velocities and refer to them as ‘slow, normal, or fast-paced’, while studies that specify gait velocities look at smaller ranges starting at 0.5 to 0.9 m/s [14, 32] and don’t exceed 2 m/s. Studies using the Stepwatch activity monitor (SAM) to detect strides and activity levels in stroke patients and elderly adults have reported good agreement ranging from ‘acceptable’ to ‘excellent’ with visual step counts at gait velocities as low as 0.08 m/s [33, 34]. However, SAM requires two one minute calibration walk tests at self-selected normal and fast walking speeds for each patient in the laboratory prior to testing in a free-living environment. Calibration tests are repeated until SAM shows at least 94% agreement with visual counts.
The lowest median agreement in this study occurred between 1.0 and 2.0 m/s which is the typical range of normal walking speeds [35], while the highest agreement occurred for velocities lower than 0.5 m/s and higher than 2 m/s (Table 2). Steps taken ranged from 10 to 92, increasing as gait velocity decreased. Similar to previous studies, longer duration trials (i.e. trials where gait velocity was less than 0.5 m/s) demonstrated greater agreement as missed steps usually occur at activity segment ends [13]. At higher gait velocities, peak acceleration amplitudes increased in magnitude and decreased in magnitude variability, resulting in increased step detection accuracy, particularly at gait velocities higher than 2 m/s. The ability of the AMS algorithm to accurately detect steps for less than 0.5 m/s suggests that it would be a beneficial outcome measures tool for rehabilitating patients with slow walking speeds.
The 3% mean agreement difference from manual step counts (Figure 6e) was due mostly to activity segments with fidgeting of the feet while standing or with less than 4 steps. The lower step detection accuracy when considering all walking was due to the inclusion of very short walking segments (Figure 6a). The slightly higher step detection accuracy when considering walking on both level ground and stairs (Figure 6b) compared to level ground only (Figure 6c) was also due to segment length. Step detection accuracy would be expected to increase for longer walking and jogging segments as the inaccuracies occur mostly at the segment’s beginning and end, consistent with previous studies on step detection and activity classification [13, 27, 36]. A small number of studies have produced slightly higher agreement values (at gait velocities >0.8 m/s) than the step detection results in this study, however they involved activity segments which were isolated and much longer in length [14, 37].
The calculated mean cadences for walking and jogging were consistent with previous studies on walking and jogging of healthy adults at a self-selected speed [38, 39]. The mean percentage cadence calculation errors (Figure 7) are comparable to results from a recent accelerometry study involving real-time cadence calculation during the 5 m walk test [12]. In the current study, the small cadence calculation errors were due to missed steps. Cadence variability has been shown to be an important factor when assessing patient function levels [18]. The most accurate pedometers can give step counts within ±3% of the manual step count, with step counts being classed as ‘acceptable’ when within ±10% [6, 40, 41]. The 97% median step count agreement value in this study when compared to video step counts and high agreement of cadences suggest that this method would be suitable for counting walking and jogging steps using tri-axial accelerometers placed on the waist, thigh, and bilaterally on the ankles in a free-living environment. However, it is possible that other daily living activities not examined in this study may inhibit step detection accuracy. The advantage of using accelerometers for step counting, rather than traditional pedometers, is that it can also provide data such as gait event timings, amplitudes, and other spatiotemporal parameters. Accelerometers use less battery power than gyroscopes, making them more suitable for home deployment studies.
Stair climbing activity could not be identified separate to walking on level ground as the SMA/second calculations showed no distinguishable differences. However, the results presented here suggest that walking and stair climbing activity levels were similar and counting stair climbing steps as walking steps is sufficient for assessing activity using step counts. Previous studies have shown that the energy expended walking down stairs is similar to slow walking on level ground [42] and a third of that expended walking upstairs [43]. It is important to note that patient compliance issues have been reported in previous studies due to multiple sensor use which can be cumbersome for long-term data collections [44, 45]. While accurate step counts can be used to effectively assess the functional status of impaired individuals, factors such as behavior and environment should also be considered in healthy individuals. Conducting this study in a free-living environment would be more realistic but more difficult than in a laboratory. Many validation studies have used simplified laboratory-based testing methods (standing or sitting still or continuous periods of walking [8, 24, 41]). We instructed subjects to perform activities as naturally as they could, i.e. standing while moving their feet as standing completely still is not expected in a free-living environment [26], and switching between activities such as walking to sitting down and fidgeting of the body and/or legs. In addition, the laboratory space included stairs, a chair, and a bed. Only 12 healthy subjects were included in this study. While many studies use similar subject numbers [12, 32, 36], algorithm robustness should be tested on a larger subject number before applying it to the general population and also be validated before use in pathological or elderly populations. Each subject walked/jogged approximately 300 m during the protocol. While this is short compared to daily distances travelled in the community, it is similar to the distance tested in many studies [9, 14, 41]. Furthermore, as we tested a range of walking durations (activity segments of 2 to 115 steps), an overall longer duration of activity may not have a large effect on step detection accuracy. Another study limitation is that fidgeting was misclassified as walking in subjects that moved their feet a lot while standing. Some short walking segments were misclassified as ‘other’ if steps at the segment’s beginning and end were undetected, resulting in an AMS algorithm step count of less than four. This contributed to lowering walking and ‘other’ step detection accuracy (Figure 6a and f). The poor accuracy for detecting ‘other’ steps was also due to short activity duration resulting in missed steps and to the subjectivity of visually identifying fidgeting. A recent study also reported difficulty in fidgeting detection in the home with accelerometry methods and video observation [26]. However, the advantage of the method presented here is that adaptive acceleration and timing thresholds allow for use on a wide range of gait velocities and, therefore, potentially a wide range of patient populations and ages.
5. Conclusion
While this study involves a simulated protocol conducted in a laboratory environment, the results suggest that the proposed analysis methods are suitable for step counting using tri-axial accelerometers on the ankles, thigh, and waist in a free-living environment.
Acknowledgments
Funding was provided by DOD DM090896, NIH T32 HD07447, and NIH K12 HD065987. The body-worn motion detection and recording units were provided by Dr. Barry Gilbert, James Bublitz, Kevin Buchs, Charles Burfield, Christopher Felton, Dr. Clifton Haider, Michael Lorsung, Shaun Schreiber, Steven Schuster, and Daniel Schwab from the Mayo Clinic Special Purpose Processor Development Group. The information or content and conclusions do not necessarily represent the official position of, nor should any official endorsement be inferred by the National Institutes of Health, the United States Navy, the Department of Defense, or the U.S. Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflict of interest.
Contributor Information
Emma Fortune, Email: fortune.emma@mayo.edu.
Vipul Lugade, Email: lugade.vipul@mayo.edu.
Melissa Morrow, Email: morrow.melissa@mayo.edu.
Kenton Kaufman, Email: kaufman.kenton@mayo.edu.
References
- 1.Alwan A. Global status report on noncommunicable diseases 2010. 1. Italy: World Health Organization; 2011. [Google Scholar]
- 2.Aadahl M, von Huth Smith L, Pisinger C, Toft UN, Glumer C, Borch-Johnsen K, et al. Five-year change in physical activity is associated with changes in cardiovascular disease risk factors: the Inter99 study. Prev Med. 2009;48:326–31. doi: 10.1016/j.ypmed.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 3.Shulman LM, Pretzer-Aboff I, Anderson KE, Stevenson R, Vaughan CG, Gruber-Baldini AL, et al. Subjective report versus objective measurement of activities of daily living in Parkinson’s disease. Mov Disord. 2006;21:794–9. doi: 10.1002/mds.20803. [DOI] [PubMed] [Google Scholar]
- 4.Taylor D, Stretton CM, Mudge S, Garrett N. Does clinic-measured gait speed differ from gait speed measured in the community in people with stroke? Clin Rehabil. 2006;20:438–44. doi: 10.1191/0269215506cr945oa. [DOI] [PubMed] [Google Scholar]
- 5.Thomas JR, Nelson JK, Silverman SJ. Research methods in physical activity. 5. Champaign (IL): Human Kinetics Publishers; 2005. [Google Scholar]
- 6.Crouter SE, Schneider PL, Karabulut M, Bassett DR., Jr Validity of 10 electronic pedometers for measuring steps, distance, and energy cost. Medicine Science in Sports and Exercise. 2003;35:1455–60. doi: 10.1249/01.MSS.0000078932.61440.A2. [DOI] [PubMed] [Google Scholar]
- 7.Esliger DW, Probert A, Gorber SC, Bryan S, Laviolette M, Tremblay MS. Validity of the Actical accelerometer step-count function. Medicine and Science in Sports and Exercise. 2007;39:1200–4. doi: 10.1249/mss.0b013e3804ec4e9. [DOI] [PubMed] [Google Scholar]
- 8.Le Masurier G, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Medicine and Science in Sports and Exercise. 2003;35:867–71. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- 9.Salarian A, Russmann H, Vingerhoets FJG, Dehollain C, Blanc Y, Burkhard PR, et al. Gait assessment in Parkinson’s disease: Toward an ambulatory system for long-term monitoring. IEEE Trans Biomed Eng. 2004;51:1434–43. doi: 10.1109/TBME.2004.827933. [DOI] [PubMed] [Google Scholar]
- 10.Rueterbories J, Spaich EG, Larsen B, Andersen OK. Methods for gait event detection and analysis in ambulatory systems. Med Eng Phys. 2010;32:545–52. doi: 10.1016/j.medengphy.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Mansfield A, Lyons GM. The use of accelerometry to detect heel contact events for use as a sensor in FES assisted walking. Med Eng Phys. 2003;25:879–85. doi: 10.1016/s1350-4533(03)00116-4. [DOI] [PubMed] [Google Scholar]
- 12.Yang CC, Hsu YL, Shih KS, Lu JM. Real-time gait cycle parameter recognition using a wearable accelerometry system. Sensors (Basel) 2011;11:7314–26. doi: 10.3390/s110807314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dijkstra B, Zijlstra W, Scherder E, Kamsma Y. Detection of walking periods and number of steps in older adults and patients with Parkinson’s disease: accuracy of a pedometer and an accelerometry-based method. Age and Ageing. 2008;37:436–41. doi: 10.1093/ageing/afn097. [DOI] [PubMed] [Google Scholar]
- 14.Ryan CG, Grant PM, Tigbe WW, Granat MH. The validity and reliability of a novel activity monitor as a measure of walking. British Journal of Sports Medicine. 2006;40:779–84. doi: 10.1136/bjsm.2006.027276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lowry KA, Smiley-Oyen AL, Carrel AJ, Kerr JP. Walking stability using harmonic ratios in Parkinson’s disease. Mov Disord. 2009;24:261–7. doi: 10.1002/mds.22352. [DOI] [PubMed] [Google Scholar]
- 16.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M31. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 17.Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55:1727–34. doi: 10.1111/j.1532-5415.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- 18.Hafner BJ, Smith DG. Differences in function and safety between Medicare Functional Classification Level-2 and -3 transfemoral amputees and influence of prosthetic knee joint control. J Rehabil Res Dev. 2009;46:417–33. [PubMed] [Google Scholar]
- 19.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA-J AM Med Assoc. 2011;305:50–8. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greene BR, McGrath D, O’Neill R, O’Donovan KJ, Burns A, Caulfield B. An adaptive gyroscope-based algorithm for temporal gait analysis. Med Biol Eng Comput. 2010;48:1251–60. doi: 10.1007/s11517-010-0692-0. [DOI] [PubMed] [Google Scholar]
- 21.Ichinoseki-Sekine N, Kuwae Y, Higashi Y, Fujimoto T, Sekine M, Tamura T. Improving the Accuracy of Pedometer Used by the Elderly with the FFT Algorithm. Med Sci Sports Exerc. 2006;38:1674–81. doi: 10.1249/01.mss.0000227641.68360.c2. [DOI] [PubMed] [Google Scholar]
- 22.Lugade VA, Fortune E, Morrow MM, Kaufman KR. Validity of using tri-axial accelerometers to measure human movement – Part I: Posture and Movement Detection. Medical Engineering & Physics. doi: 10.1016/j.medengphy.2013.06.005. Accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karantonis DM, Narayanan MR, Mathie M, Lovell NH, Celler BG. Implementation of a real-time human movement classifier using a triaxial accelerometer for ambulatory monitoring. IEEE Trans Inf Technol Biomed. 2006;10:156–67. doi: 10.1109/titb.2005.856864. [DOI] [PubMed] [Google Scholar]
- 24.Mathie MJ, Coster AC, Lovell NH, Celler BG. Detection of daily physical activities using a triaxial accelerometer. Med Biol Eng Comput. 2003;41:296–301. doi: 10.1007/BF02348434. [DOI] [PubMed] [Google Scholar]
- 25.Ounpuu S. The biomechanics of walking and running. Clin Sports Med. 1994;13:843–63. [PubMed] [Google Scholar]
- 26.Dijkstra B, Kamsma Y, Zijlstra W. Detection of gait and postures using a miniaturised triaxial accelerometer-based system: accuracy in community-dwelling older adults. Age Ageing. 2010;39:259–62. doi: 10.1093/ageing/afp249. [DOI] [PubMed] [Google Scholar]
- 27.Bussmann JB, Tulen JH, van Herel EC, Stam HJ. Quantification of physical activities by means of ambulatory accelerometry: a validation study. Psychophysiol. 1998;35:488–96. doi: 10.1017/s0048577298971153. [DOI] [PubMed] [Google Scholar]
- 28.Orendurff MS, Schoen JA, Bernatz GC, Segal AD, Klute GK. How humans walk: bout duration, steps per bout, and rest duration. J Rehabil Res Dev. 2008;45:1077–89. doi: 10.1682/jrrd.2007.11.0197. [DOI] [PubMed] [Google Scholar]
- 29.McGraw KO, Wong S. Forming inferences about some intraclass correlation coefficients. Psychol Methods. 1996;1:30–46. [Google Scholar]
- 30.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 31.Storti KL, Pettee KK, Brach JS, Talkowski JB, Richardson CR, Kriska AM. Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine and Science in Sports and Exercise. 2008;40:59–64. doi: 10.1249/mss.0b013e318158b504. [DOI] [PubMed] [Google Scholar]
- 32.Zijlstra W, Hof AL. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait and Posture. 2003;18:1–10. doi: 10.1016/s0966-6362(02)00190-x. [DOI] [PubMed] [Google Scholar]
- 33.Haeuber E, Shaughnessy M, Forrester LW, Coleman KL, Macko RF. Accelerometer monitoring of home- and community-based ambulatory activity after stroke. Archives of Physical Medicine and Rehabilitation. 2004;85:1997–2001. doi: 10.1016/j.apmr.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 34.Resnick B, Nahm E-S, Orwig D, Zimmerman SS, Magaziner J. Measurement of Activity in Older Adults: Reliability and Validity of the Step Activity Monitor. Journal of Nursing Measurement. 2001;9:275–90. [PubMed] [Google Scholar]
- 35.Oberg T, Karsznia A, Oberg K. Basic gait parameters: reference data for normal subjects, 10–79 years of age. J Rehabil Res Dev. 1993;30:210–23. [PubMed] [Google Scholar]
- 36.Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006;40:992–7. doi: 10.1136/bjsm.2006.030262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Foster RC, Lanningham-Foster LM, Manohar C, McCrady SK, Nysse LJ, Kaufman KR, et al. Precision and accuracy of an ankle-worn accelerometer-based pedometer in step counting and energy expenditure. Preventive Medicine. 2005;41:778–83. doi: 10.1016/j.ypmed.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 38.Blanc Y, Balmer C, Landis T, Vingerhoets F. Temporal parameters and patterns of the foot roll over during walking: normative data for healthy adults. Gait Posture. 1999;10:97–108. doi: 10.1016/s0966-6362(99)00019-3. [DOI] [PubMed] [Google Scholar]
- 39.Kirby RL, Nugent ST, Marlow RW, MacLeod D, Marble A. Coupling of cardiac and locomotor rhythms. J Appl Physiol. 1989;66:323–9. doi: 10.1152/jappl.1989.66.1.323. [DOI] [PubMed] [Google Scholar]
- 40.Schneider PL, Crouter SE, Bassett DR. Pedometer measures of free-living physical activity: comparison of 13 models. Medicine and Science in Sports and Exercise. 2004;36:331–5. doi: 10.1249/01.MSS.0000113486.60548.E9. [DOI] [PubMed] [Google Scholar]
- 41.Schneider PL, Crouter SE, Lukajic O, Bassett DR., Jr Accuracy and reliability of 10 pedometers for measuring steps over a 400-m walk. Medicine and Science in Sports and Exercise. 2003;35:1779–84. doi: 10.1249/01.MSS.0000089342.96098.C4. [DOI] [PubMed] [Google Scholar]
- 42.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 43.Bassett DR, Vachon JA, Kirkland AO, Howley ET, Duncan GE, Johnson KR. Energy cost of stair climbing and descending on the college alumnus questionnaire. Med Sci Sports Exerc. 1997;29:1250–4. doi: 10.1097/00005768-199709000-00019. [DOI] [PubMed] [Google Scholar]
- 44.Atallah L, Lo B, King R, Guang-Zhong Y. Sensor positioning for activity recognition using wearable accelerometers. IEEE Trans Biomed Circuits Syst. 2011;5:320–9. doi: 10.1109/TBCAS.2011.2160540. [DOI] [PubMed] [Google Scholar]
- 45.Allen FR, Ambikairajah E, Lovell NH, Celler BG. Classification of a known sequence of motions and postures from accelerometry data using adapted Gaussian mixture models. Physiol Meas. 2006;27:935–51. doi: 10.1088/0967-3334/27/10/001. [DOI] [PubMed] [Google Scholar]


