Abstract
Background
The prevalence of alcohol, tobacco, and other drug (ATOD) use among emergency department (ED) patients is high and many of these patients have unrecognized and unmet substance use treatment needs. Identification of patients in the ED with problem substance use is not routine at this time.
Methods
We examined screening data, including standardized measures of ATOD use (HSI, AUDIT-C, DAST-10), from 14,866 ED patients in six hospitals across the United States. We expected younger age, male gender, higher triage acuity, and other substance use severity (ATOD) to be associated both with use versus abstinence and with severity of each substance use type. We used negative binomial hurdle models to examine the association between covariates and (1) substance use versus abstinence (logistic submodel) and with (2) severity among those who used substances (count submodel).
Results
Rates of use and problem use in our sample were similar to or higher than other ED samples. Younger patients and males were more likely to use ATOD, but the association of age and gender with severity varied across substances. Triage level was a poor predictor of substance use severity. Alcohol, tobacco, and drug use were significantly associated with using other substances and severity of other substance use.
Conclusion
Better understanding of the demographic correlates of ATOD use and severity and the patterns of comorbidity among classes of substance can inform the design of optimal screening and brief intervention procedures addressing ATOD use among ED patients. Tobacco may be an especially useful predictor.
Keywords: Emergency Department, Alcohol, Substance Abuse, Tobacco, Addiction, Negative Binomial Model
1. INTRODUCTION
The Affordable Care Act includes strong incentives for the integration of behavioral health and medical treatment (Substance Abuse and Mental Health Services Administration, 2013). Screening and Brief Intervention (SBI) programs are a good way to address substance use treatment needs during medical treatment, and numerous studies have demonstrated the effectiveness of SBI programs aimed at alcohol use problems among emergency department (ED) patients (Field et al., 2010; Havard et al., 2008). Although a few recent studies have begun to explore the effects of SBI on drug use among ED patients (Bernstein et al., 2009, 1997; Blow et al., 2010; Bonar et al., 2014; Woolard et al., 2013), published data are scarce concerning the efficacy of SBI for adult ED patients with drug use disorders.
In spite of increasing recognition of SBI as valuable, alcohol, tobacco, and other drug (ATOD) screening rates in EDs are low, and many hospitals only screen alcohol toxicology reports, which indicate only recent use, not problem severity (Cunningham et al., 2010; Terrell et al., 2008). Research documents a high need for substance use treatment in this population (Rockett et al., 2005, 2003). This, as well as the existing research (Bernstein et al., 2009; Blow et al., 2010; Woolard et al., 2013), suggests EDs are feasible sites for SBI for tobacco and other drugs beyond alcohol.
The prevalence of ATOD use problems among ED patients is 50 to 100% higher than U.S. averages (Center for Disease Control, 2012a, 2011; Cherpitel and Ye, 2008; McCabe et al., 2011; Substance Abuse and Mental Health Services Administration, 2012a). A large percentage of ED patients have unrecognized ATOD treatment needs and are more likely to be admitted to the hospital and to repeatedly utilize EDs (Hankin et al., 2013; Rockett et al., 2005, 2003). Alcohol and tobacco are the most prevalent substances used by ED patients (McCabe et al., 2011; Rockett et al., 2006), with marijuana and cocaine being the most common illicit drugs (Vitale and van de Mheen, 2006). Similar to the general population (Substance Abuse and Mental Health Services Administration, 2012a), ED patients with at-risk drinking levels are more likely to use tobacco and illicit drugs than other ED patients (Fleming et al., 2007). Likewise, tobacco-using ED patients are at higher risk of illicit drug and risky alcohol use than other ED patients (McCabe et al., 2011).
Among ED patients, as in the general population, men are more likely to use ATOD than women (Substance Abuse and Mental Health Services Administration, 2012a; Wu et al., 2012). Younger adult patients are more likely to test positive for illicit drugs or alcohol than older patients (Bogstrand et al., 2011; Vitale and van de Mheen, 2006). Younger age and being male are associated with increased likelihood of tobacco use (McCabe et al., 2011). Interestingly, while more men than women report at-risk drinking (Fleming et al., 2007), heavy drinking women are more likely to have visited an ED than heavy drinking men (Cherpitel, 1999). Younger patients are more likely to report heavy episodic drinking and marijuana use while older patients are more likely to drink daily (Fleming et al., 2007).
The aim of this study was to characterize ATOD use in a large multi-state ED patient sample collected for the National Drug Abuse Treatment Clinical Trials Network (NIDA CTN): Screening, Motivational Assessment, Referral, and Treatment in Emergency Departments (SMART-ED) study. We examined the association of gender, age, their interaction, triage acuity, and severity of use of the other two types of substances, with (1) use versus abstinence and with (2) use severity of each substance type. Building upon the foundation established by the prior research mentioned above, the current study examines participant characteristics associated with use versus abstinence and also, simultaneously, those associated with severity of use among users. Research on substance use in EDs has either occurred in single ED settings or utilized national retrospective substance use surveys that also queried ED visits. Supplementing prior research, we obtained data from ED patients during their visits to six EDs across the U.S., generating the largest sample of individuals assessed about ATOD use in-person during an ED visit. We hypothesized that ATOD use (versus abstinence) and greater ATOD severity would be associated with younger age, male gender, higher triage acuity, and higher scores on alternate substance scales (e.g., tobacco severity associated with alcohol and drug severity). This research should help ED physicians identify patients at greater risk of having more severe ATOD problems and potentially the highest need for screenings and interventions, by differentiating characteristics associated with use versus abstinence from those associated with ATOD severity among users.
2. METHODS
We examined screening data from the NIDA CTN: SMART-ED study, a large multi-center randomized controlled trial of SBI for illicit drug use in EDs. Detailed information about the protocol for the full study (clinical trials registration number NCT01207791) is available in Bogenschutz et al., 2011.
2.1 Participants
Participants were recruited from EDs of public sector hospitals affiliated with academic institutions in six states (New Mexico, West Virginia, Florida, New York, Massachusetts, and Ohio). Inclusion criteria were registration in the ED during screening hours, age ≥ 18 years, English literacy, ability to provide informed consent, and telephone access. Patients were excluded if they were significantly cognitively impaired, in police custody, or currently engaged in ED treatment that rendered them unable to participate.
Study staff attempted to screen all eligible patients registered at the EDs during recruitment hours. Research assistants (RAs) collected age, gender, and triage level from the clinical patient tracking system and then approached patients to ask if they would participate in an anonymous screening. If patients agreed, RAs used a brief script to obtain verbal consent for anonymous collection of screening data. The participant and the RA, as appropriate, entered screening data directly into tablet computers. Participant recruitment is detailed in Table 1. All participants gave verbal informed consent and the institutional review board at the University of New Mexico approved the protocol.
2.2 Measures
Results reported here are from a 20-item screening measure used in the SMART-ED study (Bogenschutz et al., 2011). Three of the four sections of the screen consisted of well-validated measures. The four sections were administered in the following order: (1) modified version of the two-item Heavy Smoking Index (HSI-M; Chabrol et al., 2005; Heatherton et al., 1989), (2) three-item Alcohol Use Disorders Identification Test – Consumption (AUDIT-C; Bradley et al., 2007; Bush et al., 1998) assessing alcohol consumption, (3) ten-item Drug Abuse Screening Test (DAST-10; Skinner, 1982) assessing drug use problems, and (4) two questions querying primary problem substance and days of past 30-day use of primary problem substance: (1) “Excluding alcohol and tobacco, what drug has caused the most difficulties recently? (If no recent difficulties, what drug have you used most often in recent months?)” and (2) “In the past 30 days, how many days have you used?”
The standard Heavy Smoking Index (HSI) measures level of severity among smokers with two questions: (1) “How many cigarettes do you smoke per day?” (scored “0” for smoking 10 or less), and (2) “How soon after you wake up do you smoke your first cigarette?” (scored “0” if after 60 minutes). Because our participants were not necessarily smokers, two screening questions were added prior to the HSI: “Do you smoke cigarettes or use any other form of tobacco?” and “Do you smoke or use tobacco every day?” Answering “no” to these two questions resulted in a score of 0 on the HSI-M. For those participants endorsing daily tobacco use, the HSI-M score was defined as the standard HSI score plus 1. Thus in the HSI-M, “0” = not a current daily tobacco user, and scores of “1” or greater indicated a range of severity of current daily use.
Possible scores were 0–7 for the HSI-M, 0–12 for the AUDIT-C, 0–10 for the DAST-10, and 0–30 for past 30-day drug use. Scores of zero on the AUDIT-C and the DAST-10 represented no use of alcohol or drugs, respectively, in the last year. Internal consistency in our sample was α= .68 for the HSI-M, α= .86 for the AUDIT-C, and α= .91 for the DAST-10. All EDs used a 5-level triage system, coded as “1” representing the highest acuity and “5” representing the lowest acuity.
2.3 Analysis Plan
Study hypotheses were evaluated with four dependent variables: HSI-M, AUDIT-C, DAST-10, and 30-day drug use. Participants reporting no ATOD use (no daily use for HSI-M) scored zero on these measures, resulting in zeros for many observations (see Table 2). The choice of statistical models was influenced by three considerations. First, excess zeros made dependent variable distributions positively skewed, motivating the use of a Poisson or negative binomial distribution. Although 30-day drug use was the only true count dependent variable, the preponderance of zeros in the other outcomes caused distributions mirroring count outcome distributions. Thus, since the data violated assumptions for ordinary least squares regression, count regression was chosen as an alternative for all four measures (Atkins et al., 2013; Neal and Simons, 2007). Second, the negative binomial distribution was chosen over the Poisson distribution because data were significantly over-dispersed (Coxe et al., 2009). Third, a hurdle model was chosen to simultaneously examine the effect of covariates on “any use” (logistic regression portion of the model) and severity of use among those who used ATOD (count regression portion of the model).
Table 2.
Descriptive statistics for outcome variables and covariates by substance use (N = 14866)
| Outcome | No Use by Drug | Use | User Mean (SD) |
|---|---|---|---|
| HSI-Ma | N = 9037 (61.57%) | N = 5640 (38.43%) | 3.51 (1.72) |
| % male*** | 54.87% | 64.66% | |
| Age – M(SD) | 38.55 (14.04) | 38.20 (12.12) | |
| Triage – M(SD)* | 3.44 (1.02) | 3.48 (0.92) | |
| AUDIT-Cb | N = 4522 (30.42%) | N = 10319 (69.41%) | 4.35 (3.07) |
| % male*** | 53.49% | 61.52% | |
| Age – M(SD)*** | 42.35 (14.01) | 36.62 (12.61) | |
| Triage – M(SD)*** | 3.35 (0.94) | 3.50 (0.99) | |
| DASTc | N = 10214 (68.71%) | N = 4561 (30.68%) | 3.73 (2.76) |
| % male*** | 54.34% | 69.57% | |
| Age – M(SD)*** | 39.66 (13.69) | 35.38 (11.90) | |
| Triage – M(SD)* | 3.44 (0.98) | 3.48 (0.97) | |
| 30-day Drug Used | N = 11662 (78.45) | N = 3204 (21.55) | 14.10 (11.57) |
| % male*** | 55.85% | 70.91% | |
| Age – M(SD)*** | 39.22 (13.59) | 35.31 (11.79) | |
| Triage – M(SD) | 3.45 (0.98) | 3.48 (0.97) | |
Heavy Smoking Index-modified as described in Method section; Total sample size for HSI-M is N = 14677 due to 171 participants using smokeless tobacco products and the remainder having missing data for this measure.
Alcohol Use Disorder Identification Test-Consumption
Drug Abuse Screening Test
Past 30-day drug use (single question)
Significant difference between use and no use groups (p < .05)
Significant difference between use and no use groups (p < .001)
We also examined the magnitude of the association between covariates and outcomes with odds ratios for dichotomous outcomes and rate ratios for count outcomes. Odds ratios represent the increase (if >1) or decrease (if <1) in the odds of being in the “no use” category when all other covariates in the model were at their mean value. Rate ratios represent the increase (if >1) or decrease (if <1) in the outcome variable for a one-unit increase in the covariate (Atkins et al., 2013).
We assessed for site effects by computing intraclass correlations for outcome measures to determine the degree that the assumption of independence of observations was violated. Intraclass correlations were near zero for all outcomes (range = 0.000–0.077), indicating clustering within sites did not account for substantial variance. Given the minimal variance explained by site, lack of site-specific covariates or hypotheses, and difficulties with convergence with only six sites using multilevel modeling, we adjusted for clustering in the data by estimating all parameters using a weighted maximum likelihood function with standard errors computed using a sandwich estimator (i.e., standard errors were adjusted for clustering in the data; Rogers, 1993). Models were estimated using Mplus version 6.12. Gender was coded −.5 for males and +.5 for females, and all other covariates were grand mean-centered.
3. RESULTS
3.1 Descriptive Statistics
Complete screening data were available from 14,866 participants in total. Participants’ average age was 38.4 years (SD = 13.32) and 59% were male. Participant recruitment is outlined in Table 1. Descriptive statistics for outcome variables and covariates by “use” versus “non-use” category are shown in Table 2. Patterns of reported substance use are shown in Table 3.
Table 1.
Participant Recruitment
| Number | Rationale |
|---|---|
| 20,762 | Patients reviewed by research assistants |
| −5,253 | Excluded, did not consent, unable to consent |
| −538 | Found ineligible after verbal consent |
| −105 | Missing age, gender, or triage data or contradictory data |
| =14,866 | Total included participants |
Table 3.
Patterns of Substance Use
| Substance Use | Percent Reporting (N = 14866) |
|---|---|
| Any Current Tobacco Use | 47 |
| Daily Tobacco Use | 39 |
| Use of Any Alcohol in Past Year | 70 |
| Risky Drinking* Over the Past Year | 45 |
| Drug Use in the Past Year | 30 |
| Past 30-day Drug Use | 22 |
| Moderate to Severe Drug Problems** | 17 |
| Identified a Problem Drug | 27 |
| Primary Problem Drug Among Drug Users | Percent Reporting (N = 4014) |
| Marijuana | 60 |
| Cocaine | 18 |
| Street Opioids | 11 |
| Prescription Opioids | 6 |
| Methamphetamine | 2 |
| Sedatives or Sleeping Pills | 1 |
| Hallucinogens | 1 |
| Prescribed Amphetamine-type Stimulants | 1 |
Risky Drinking was defined using a cut point of 4 on the AUDIT-C or any report of drinking 6 or more drinks per occasion over the past year; (Bradley et al., 2007; Bush et al., 1998).
Moderate to severe problem drug use was defined with cut point of 3 for the DAST-10 (Skinner, 1982).
3.2 Negative Binomial Hurdle Models
Results from the negative binomial hurdle models are reported in Table 4. Parameter estimates for dichotomous outcomes evaluated the association of covariates with abstinence versus any substance use (i.e., each predictor was associated with the log odds of a zero value on the outcome, rather than a non-zero value, which indicated use). For example, as seen in the dichotomous portion of Table 4 and described below, DAST-10 scores were significantly associated with daily smoking, β = −0.281, indicating that participants with higher scores on the DAST-10 were less likely to report not smoking daily (HSI-M = 0) and more likely to report smoking daily (HSI-M > 0). For the count portion of the table the parameter is positive, β = 0.026, where higher DAST-10 scores were associated with higher HSI-M scores among participants with any drug use.
Table 4.
Hurdle Model Results
| Dichotomous Outcome | Count Outcomeb | |||||||
|---|---|---|---|---|---|---|---|---|
| Covariates | Estimatea | Std Error |
p- >value |
Odds Ratios |
Estimate | Std Error |
p- value |
Rate Ratios |
| Modified Heavy Smoking Index (HSI-M) | R2=.144c | |||||||
| Gender | 0.184 | 0.034 | < .001 | 1.202 | 0.004 | 0.017 | 0.802 | 1.004 |
| Age | −0.004 | 0.004 | 0.380 | 0.996 | 0.005 | 0.001 | < .001 | 1.005 |
| Gender-by-Age | −0.002 | 0.002 | 0.203 | 0.998 | 0.005 | 0.001 | < .001 | 1.005 |
| AUDIT-C | −0.055 | 0.016 | < .01 | 0.946 | 0.012 | 0.003 | < .001 | 1.012 |
| DAST-10 | −0.281 | 0.028 | < .001 | 0.755 | 0.026 | 0.003 | <.001 | 1.026 |
| Triage level | −0.046 | 0.045 | 0.305 | 0.955 | −0.021 | 0.010 | <.05 | 0.979 |
| Alcohol Use Disorder Identification Test-Consumption (AUDIT-C) | R2=.093 | |||||||
| Gender | 0.331 | 0.078 | <.001 | 1.392 | −0.431 | 0.037 | <.001 | 0.650 |
| Age | 0.032 | 0.003 | < .001 | 1.033 | −0.003 | 0.002 | 0.221 | 0.997 |
| Gender-by-Age | 0.005 | 0.003 | 0.146 | 1.005 | −0.007 | 0.001 | < .001 | 0.993 |
| HSI-M | −0.010 | 0.028 | 0.715 | 0.990 | 0.053 | 0.009 | < .001 | 1.054 |
| DAST-10 | −0.132 | 0.025 | <.001 | 0.876 | 0.073 | 0.007 | < .001 | 1.076 |
| Triage level | −0.090 | 0.016 | < .001 | 0.914 | 0.013 | 0.008 | 0.131 | 1.013 |
| Drug Abuse Screening Test-10 (DAST-10) | R2=.246 | |||||||
| Gender | 0.489 | 0.094 | <.001 | 1.631 | −0.043 | 0.064 | 0.498 | 0.958 |
| Age | 0.031 | 0.005 | < .001 | 1.031 | 0.004 | 0.002 | <.05 | 1.004 |
| Gender-by-Age | 0.003 | 0.004 | 0.366 | 1.003 | −0.002 | 0.001 | 0.108 | 0.998 |
| HSI-M | −0.259 | 0.028 | <.001 | 0.772 | 0.127 | 0.023 | <.001 | 1.135 |
| AUDIT-C | −0.183 | 0.019 | < .001 | 0.833 | 0.032 | 0.007 | < .001 | 1.033 |
| Triage level | 0.053 | 0.025 | <.05 | 1.054 | −0.064 | 0.014 | < .001 | 0.938 |
| Past 30 Days of Drug Use | R2=.227 | |||||||
| Gender | 0.447 | 0.107 | <.001 | 1.564 | −0.022 | 0.047 | 0.649 | 0.978 |
| Age | 0.028 | 0.005 | < .001 | 1.028 | −0.005 | 0.002 | <.01 | 0.995 |
| Gender-by-Age | −0.002 | 0.005 | 0.733 | 0.998 | 0.008 | 0.004 | 0.051 | 1.008 |
| HSI-M | −0.247 | 0.028 | < .001 | 0.781 | 0.064 | 0.012 | < .001 | 1.066 |
| AUDIT-C | −0.177 | 0.021 | < .001 | 0.890 | 0.003 | 0.007 | 0.687 | 1.003 |
| Triage level | 0.051 | 0.021 | <.05 | 1.052 | −0.015 | 0.014 | 0.273 | 0.985 |
Dichotomous estimate column evaluated no substance use (as opposed to any substance use), whereas the count estimate column evaluated the association between the covariate and outcome among participants who reported substance use (use ≥ 1). Odd ratios describe the increase (if over 1) or decrease (if less than one) in the odds of being in the no use category when all other covariates in the model were at their mean value. Rate ratios can be interpreted as percentage increase (>1) or decrease (<1) in outcome for a one-unit increase in the predictor (when all other predictors in the model are zero).
The distribution used for the count outcome contained only observations > 0
R-squared refers to Count Outcome only
3.3 Tobacco Smoking (HSI-M)
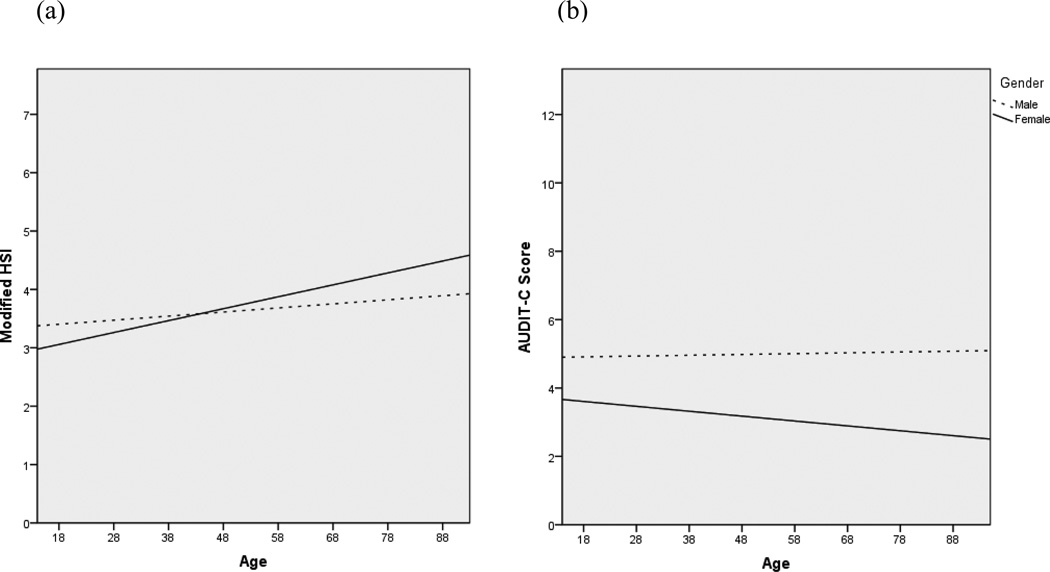
Male gender, greater alcohol use severity (AUDIT-C), and greater drug use severity (DAST-10) were associated with being a daily smoker versus not being a daily smoker. Age and triage acuity were not associated with daily smoking. Older age, greater alcohol use severity, higher drug use severity, and more severe triage acuity were associated with greater HSI-M scores among daily smokers. Gender was not associated with HSI-M scores among daily smokers. However, a gender-by-age interaction was found in which younger women smokers had lower HSI-M scores than younger men (Figure 1a), but this difference reversed across the lifespan so that there was a stronger positive relationship between age and HSI-M scores for women than for men.
Figure 1.
Significant age by gender interaction plots in the original metric of the raw data. (a) Modified HSI, (b) AUDIT-C.
3.4 Alcohol Use (AUDIT-C)
Male gender, younger age, greater drug use severity (DAST-10), and less severe triage level were associated with past year alcohol drinking versus abstaining. Smoking severity (HSI-M) was not associated with drinking versus abstaining. Among drinkers, male gender, heavier smoking, and greater drug use severity were associated with higher AUDIT-C scores. Age and triage acuity were not associated with AUDIT-C scores among drinkers. There was also a significant gender-by-age interaction such that, among drinkers, younger women exhibited less past year alcohol consumption than younger men (Figure 1b), and there was a negative relationship between age and drinking for women compared to men.
3.5 12-Month Drug Use (DAST-10) and 30-Day Drug Use Frequency
Male gender, younger age, more severe triage acuity, heavier smoking and greater alcohol use severity were associated with past year drug use versus abstinence (DAST-10 = 0 versus DAST-10 > 0) and also with past 30-day drug use versus abstinence. Among drug users, older age, more severe triage acuity, heavier smoking, and greater alcohol consumption were associated with higher DAST-10 scores. Gender was not associated with DAST-10 scores among drug users. There was no gender-by-age interaction associated with DAST-10 or past 30-day drug use frequency. Among past 30-day drug users, younger age and heavier smoking were associated with higher frequency of drug use in the past month. Gender, alcohol use severity, and triage acuity were not associated with past 30-day drug use frequency.
4. DISCUSSION
Patterns of ATOD use in this large sample of ED patients from hospitals across the U.S. were similar to those found in single ED and national database studies, confirming high rates of ATOD use among ED patients. Alcohol and tobacco represented the most frequently reported ATOD use, and among drug users the majority reported marijuana use. A wide range of other drugs was also reported in this sample. The prevalence of tobacco use in our sample was more than twice the national average (Center for Disease Control, 2011). The prevalence of alcohol use in the EDs surveyed was similar to the national average (Center for Disease Control, 2012b), but drug use prevalence was higher than the national average (Substance Abuse and Mental Health Services Administration, 2012b). Risky drinking and problem drug use prevalence in this sample were higher than those reported for ED patients in national databases by Cherpitel and Ye (2008) and over twice the national U.S. population average (Center for Disease Control, 2012a), possibly due to slightly different definitions of the constructs.
The majority of the results were as expected, with younger age, male gender, and more problematic ATOD use generally being associated with more problematic use of each substance as well as greater likelihood of use. Given our large sample size, we expected many covariates to be significant. Odds ratios and rate ratios in Table 4 help direct attention to covariates that are more powerful predictors.
The negative binomial hurdle models allowed examination of how variables are associated with use versus abstinence independently of how they are associated with severity among users. Using this approach we discovered some new information. One example was the relationship of gender with smoking and drug use. Similar to McCabe et al. (2011), men were more likely to smoke daily than women. However, in the present data there was no association of gender with smoking severity among daily smokers; men and women daily smokers were equally heavy smokers. This finding is consistent with a recent report that women are no longer at lower risk of dying from smoking-related diseases than men (Thun et al., 2013). Similar to our results for tobacco, men were more likely to have used drugs recently, but among drug users there was no difference in drug use severity or past 30-day drug use frequency between men and women. This suggests that once patients are identified as drug users or smokers in the ED, it would be erroneous to assume less severe problems for women.
Age was not associated with likelihood of being a daily smoker, but among daily smokers older smokers had heavier smoking severity. Younger participants were more likely to drink alcohol, but among those who did drink there was no association of age with severity. This is in contrast to the general U.S. population where heavy drinking and binge drinking decline with age (Substance Abuse and Mental Health Services Administration, 2012b). The lack of an age-severity effect in our sample may be specific to the ED population. Older heavier drinkers may be over-represented among ED patients, possibly due to prolonged problem drinking being associated with poor health. It may also be the case that a more complex relationship exists between age and ATOD severity among the ED population than was investigated in the current study (e.g., a u-shaped curve whereby younger and older populations are both higher on ATOD severity than middle aged individuals). As an exploratory analysis, we examined nonlinear effects of age in a subset of the models. Results were entirely consistent across models with or without nonlinear effects of age. Future research on the relationship between age and ATOD outcomes is warranted.
Degree of triage acuity was associated with ATOD use and severity, though not very robustly and not always in the direction expected. For example, more severe triage acuity was associated with participants being more likely to abstain from alcohol versus drink, but triage acuity was not associated with alcohol consumption severity among drinkers. This could be because our sampling procedure likely missed individuals with severe alcohol-related trauma and/or acute intoxication who could not be screened. We did find that participants who were screened for this study had slightly less severe triage acuity than those who were excluded (mean 3.45 compared to 3.22 respectively), however the effect size was very small. On the other hand, stronger effects of triage level were in the expected direction for drugs.
Younger participants were more likely to report past year drug use, but older age was associated with greater drug use severity among users. This suggests that ED practitioners should be careful not to assume that older patients have less severe drug problems than younger patients. It may also mean that older patients who screen positive for drugs would be good candidates for interventions. Especially since older patients may be more likely than younger ones to attend interventions after screening positive for ATOD in the ED (Blow et al., 2010).
4.1 Limitations
Similar to most SBI research, this protocol obtained self-reports of ATOD use because toxicology reports (recent intoxication) were of less interest than longer-term drug problem severity. As some research has demonstrated underreporting of current drug use among ED patients (Rockett et al., 2006), we may have underestimated levels of drug use in our sample. Moreover, some participants misusing prescriptions may not have identified them as “problem substances” (Price et al., 2011) and thus we may have particularly underestimated prescription drug misuse. However, several aspects of the study design should have reduced underreporting (e.g., tablet computers, ensuring confidentiality).
Another limitation necessitated by our design is that people with impairments rendering them unable to consent or answer questions were not assessed. Thus, unlike studies using recall or toxicology, this study missed some potentially ATOD-involved ED patients (e.g., acutely intoxicated patients or patients with intoxication-related motor vehicle crashes or suicide attempts). During recruitment prior to verbal consent, we did not record how many people were excluded for cognitive impairment or receiving ED treatment, so we cannot determine to what extent high-acuity patients may have been underrepresented. Comparisons of gender and age in this sample with national estimates of ED patients revealed that patients aged 18–65 were better represented in this sample than patients over age 65. Moreover, screened patients were slightly younger than non-screened patients.
Additionally, in order to limit assessment reactivity, we collected very little demographic information at screening. Thus, we cannot report race, ethnicity, or socioeconomic status for this sample, nor can we test the association of those variables with outcome variables. Likewise, at this screening point we only asked participants to identify primary drug of use and do not have data about other drug use. Finally, our models accounted for a small percentage of the variance in substance use outcomes, as there are many other relevant factors accounting for substance use beyond a limited number of demographic and other ATOD use characteristics.
These limitations are offset by the strengths of the study. Results are more generalizable compared to studies conducted at single EDs, because participants were recruited from EDs across diverse regions of the U.S, albeit only at academic hospitals. The sample size was large, enhancing statistical power and the potential reliability of the findings. Data were collected using well-validated measures of substance use risk. Furthermore, our study extends prior research by collecting data in an ecologically valid manner in the ED. These results also reflect a broad range of ATOD use as well as different types of illicit drugs. Additionally, the use of negative binomial hurdle models allowed us to account for large numbers of zeros, and thus to separately evaluate variables associated with ATOD use versus abstinence and variables associated with severity among users. It also produced more accurate parameter estimates compared to previous studies using ordinary least squares regression, due to the non-normally distributed residuals resulting from excess zeros (Neal and Simons, 2007).
4.2 Conclusion
These results can assist ED providers in targeting patients at risk for ATOD problems who might benefit from SBI. Gender was a good predictor of ATOD use versus non-use, but was poor at predicting severity among users. Younger patients may be more likely to be using alcohol and drugs and to be using drugs more often in the past month; however, older tobacco and drug users may have greater problem severity. Triage level was associated with severity of heavy smoking and past year drug use and severity, but not with recent use. Thus, particularly among individuals at a higher triage level, it may be more informative to screen for longer-term consequences related to use rather than relying on toxicology screening that only assesses very recent use. Other substance use was strongly associated with substance use and severity for most of the outcome measures, suggesting that screening for all ATODs would be a more robust indicator of problems than screening for alcohol alone.
In primary care settings and for alcohol use SBI represents the standard of care (Bernstein and Bernstein, 2008), but in EDs SBI is mandated only for alcohol and only for trauma patients who are admitted in Level 1 and 2 trauma centers in the United States (American College of Surgeons Committee on Trauma, 2006). In general, levels of screening in EDs are low, and many hospitals that do screen only examine toxicology reports for alcohol (Cunningham et al., 2010; Terrell et al., 2008). Our results suggest that there would be utility in greatly expanding screening in the ED beyond this to include other substances and more informative screening measures. For example, tobacco smoking may be a convenient marker for other substance use problems, as patients often easily acknowledge smoking. Given the mixed results for the association of triage level with ATOD problems, our data also support expanding SBI to include non-trauma patients and non-trauma EDs, consistent with results reported by Blow et al. (2011) who found that poly-drug users were more likely to present with medical problems than injuries.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American College of Surgeons Committee on Trauma. Resources for the optimal care of the injured patient. 2006 http://www.facs.org/trauma/optimalcare.pdf. [Google Scholar]
- Atkins DC, Baldwin SA, Zheng C, Gallop RJ, Neighbors C. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychol. Addict. Behav. 2013;27:166–177. doi: 10.1037/a0029508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J. Effectiveness of alcohol screening and brief motivational intervention in the emergency department setting. Ann. Emerg. Med. 2008;51:751–754. doi: 10.1016/j.annemergmed.2008.01.325. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann. Emerg. Med. 1997;30:181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Acad. Emerg. Med. 2009;16:1174–1185. doi: 10.1111/j.1553-2712.2009.00490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Barry KL, Murray RL, Cunningham RM, Massey LS, Chermack ST, Booth BM. Alcohol and drug use among patients presenting to an inner-city emergency department: a latent class analysis. Addict. Behav. 2011;36:793–800. doi: 10.1016/j.addbeh.2010.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blow FC, Walton MA, Murray R, Cunningham RM, Chermack ST, Barry KL, Ilgen MA, Booth BM. Intervention attendance among emergency department patients with alcohol- and drug-use disorders. J. Stud. Alcohol Drugs. 2010;71:713–719. doi: 10.15288/jsad.2010.71.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogenschutz MP, Donovan DM, Adinoff B, Crandall C, Forcehimes AA, Lindblad R, Mandler RN, Oden NL, Perl HI, Walker R. Design of NIDA CTN Protocol 0047: Screening, motivational assessment, referral, and treatment in emergency departments (SMART-ED) Am. J. Drug Alcohol Abuse. 2011;37:417–425. doi: 10.3109/00952990.2011.596971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogstrand ST, Normann PT, Rossow I, Larsen M, Mørland J, Ekeberg Ø. Prevalence of alcohol and other substances of abuse among injured patients in a Norwegian emergency department. Drug Alcohol Depend. 2011;117:132–138. doi: 10.1016/j.drugalcdep.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Bonar EE, Walton MA, Cunningham RM, Chermack ST, Bohnert ASB, Barry KL, Booth BM, Blow FC. Computer-enhanced interventions for drug use and HIV risk in the emergency room: Preliminary results on psychological precursors of behavior change. J. Subst. Abuse Treat. 2014;46:5–14. doi: 10.1016/j.jsat.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol. Clin. Exp. Res. 2007;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch. Intern. Med. 1998;158:1789. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control. Morbidity and Mortality Weekly Report. Atlanta, GA: Department of Health and Human Services; 2011. Vital Signs: Current Cigarette Smoking Among Adults aged ≥18 years---United States, 2009; pp. 1207–1212. [Google Scholar]
- Center for Disease Control. Morbidity and Mortality Weekly Report. Atlanta, GA: Department of Health and Human Services; 2012a. Vital Signs: Binge Drinking Prevalence, Frequency, and Intensity Among Adults – United States, 2010; pp. 14–19. [PubMed] [Google Scholar]
- Center for Disease Control. Hyattsville, MD: Department of Health and Human Services; 2012b. Vital and Health Statistics, 10. [Google Scholar]
- Chabrol H, Niezborala M, Chastan E, de Leon J. Comparison of the Heavy Smoking Index and of the Fagerstrom Test for Nicotine Dependence in a sample of 749 cigarette smokers. Addict. Behav. 2005;30:1474–1477. doi: 10.1016/j.addbeh.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. Emergency room and primary care services utilization and associated alcohol and drug use in the United States general population. Alcohol. Alcohol. 1999;34:581–589. doi: 10.1093/alcalc/34.4.581. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y. Drug use and problem drinking associated with primary care and emergency room utilization in the US general population: data from the 2005 National Alcohol Survey. Drug Alcohol Depend. 2008;97:226–230. doi: 10.1016/j.drugalcdep.2008.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coxe S, West SG, Aiken LS. The analysis of count data: a gentle introduction to Poisson regression and its alternatives. J. Pers. Assess. 2009;91:121–136. doi: 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Harrison SR, McKay MP, Mello MJ, Sochor M, Shandro JR, Walton MA, D’Onofrio G. National survey of emergency department alcohol screening and intervention practices. Ann. Emerg. Med. 2010;55:556–562. doi: 10.1016/j.annemergmed.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Field CA, Baird J, Saitz R, Caetano R, Monti PM. The mixed evidence for brief intervention in emergency departments, trauma care centers, and inpatient hospital settings: what should we do? Alcohol. Clin. Exp. Res. 2010;34:2004–2010. doi: 10.1111/j.1530-0277.2010.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming EA, Gmel G, Bady P, Yersin B, Givel JC, Brown D, Daeppen JB. At-risk drinking and drug use among patients seeking care in an emergency department. J. Stud. Alcohol Drugs. 2007;68:28–35. doi: 10.15288/jsad.2007.68.28. [DOI] [PubMed] [Google Scholar]
- Hankin A, Daugherty M, Bethea A, Haley L. The Emergency Department as a prevention site: a demographic analysis of substance use among ED patients. Drug Alcohol Depend. 2013;130:230–233. doi: 10.1016/j.drugalcdep.2012.10.027. [DOI] [PubMed] [Google Scholar]
- Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103:368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 1989;84:791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- McCabe CT, Woodruff SI, Zúñiga ML. Sociodemographic and substance use correlates of tobacco use in a large, multi-ethnic sample of emergency department patients. Addict. Behav. 2011;36:899–905. doi: 10.1016/j.addbeh.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Neal DJ, Simons JS. Inference in regression models of heavily skewed alcohol use data: a comparison of ordinary least squares, generalized linear models, and bootstrap resampling. Psychol. Addict. Behav. 2007;21:441–452. doi: 10.1037/0893-164X.21.4.441. [DOI] [PubMed] [Google Scholar]
- Price AM, Ilgen MA, Bohnert ASB. Prevalence and correlates of nonmedical use of prescription opioids in patients seen in a residential drug and alcohol treatment program. J. Subst. Abuse Treat. 2011;41:208–214. doi: 10.1016/j.jsat.2011.02.003. [DOI] [PubMed] [Google Scholar]
- Rockett IRH, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: a population-based emergency department study. Ann. Emerg. Med. 2005;45:118–127. doi: 10.1016/j.annemergmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Rockett IRH, Putnam SL, Jia H, Smith GS. Assessing substance abuse treatment need: a statewide hospital emergency department study. Ann. Emerg. Med. 2003;41:802–813. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- Rockett IRH, Putnam SL, Jia H, Smith GS. Declared and undeclared substance use among emergency department patients: a population-based study. Addiction. 2006;101:706–712. doi: 10.1111/j.1360-0443.2006.01397.x. [DOI] [PubMed] [Google Scholar]
- Rogers W. Regression standard errors in clustered samples. Stata Tech. Bull. 1993;13:19–23. [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addict. Behav. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012a. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-44, HHS Publication No. (SMA) 12-4713. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012b. Center for Behavioral Health Statistics and Quality, National Survey on Drug Use and Health, 2010 and 2011. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Washington, DC: Substance Abuse and Mental Health Services Administration; 2013. Innovations in Addiction Treatment: Addiction Treatment Providers Working with Integrated Primary Care Services. [Google Scholar]
- Terrell F, Zatzick DF, Jurkovich GJ, Rivara FP, Donovan DM, Dunn CW, Schermer C, Meredith JW, Gentilello LM. Nationwide survey of alcohol screening and brief intervention practices at US level I trauma centers. J. Am. Coll. Surg. 2008;207:630–638. doi: 10.1016/j.jamcollsurg.2008.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thun MJ, Carter BD, Feskanich D, Freedman ND, Prentice R, Lopez AD, Hartge P, Gapstur SM. 50-Year trends in smoking-related mortality in the United States. N. Engl. J. Med. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale S, van de Mheen D. Illicit drug use and injuries: a review of emergency room studies. Drug Alcohol Depend. 2006;82:1–9. doi: 10.1016/j.drugalcdep.2005.08.017. [DOI] [PubMed] [Google Scholar]
- Woolard R, Baird J, Longabaugh R, Nirenberg T, Lee CS, Mello MJ, Becker B. Project Reduce: Reducing alcohol and marijuana misuse: effects of a brief intervention in the emergency department. Addict. Behav. 2013;38:1732–1739. doi: 10.1016/j.addbeh.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L-T, Swartz MS, Wu Z, Mannelli P, Yang C, Blazer DG. Alcohol and drug use disorders among adults in emergency department settings in the United States. Ann. Emerg. Med. 2012;60:172.e5–180.e5. doi: 10.1016/j.annemergmed.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]