Abstract
Although acute myocardial infarction (AMI) occurs primarily in the elderly, this disease also affects young adults. Few studies have, however, presented data on relatively young patients hospitalized with AMI. The objectives of this population-based study were to examine recent trends in the magnitude, clinical characteristics, management, and in-hospital and long-term outcomes associated with ST-segment elevation acute myocardial infarction (STEMI) and non-ST-segment elevation acute myocardial infarction (NSTEMI) in patients 30–54 years old. We reviewed the medical records of 955 residents of the Worcester (MA) metropolitan area between the ages of 30 and 54 years who were hospitalized for an initial STEMI or NSTEMI in 6 annual periods between 1999 and 2009 at 11 greater Worcester medical centers. Between 1999 and 2009, the proportion of young adults hospitalized with an STEMI decreased from approximately two-thirds to two-fifths of all patients with an initial AMI. Patients with STEMI were less likely to have a history of heart failure, hypertension, hyperlipidemia, and kidney disease than NSTEMI patients. Both groups received similar effective medical therapies during their acute hospitalization. In-hospital clinical complications and mortality were low and no significant differences in these endpoints were observed between STEMI and NSTEMI patients or with regards to 1 year post-discharge death rates (1.9% vs. 2.8%). The present results demonstrate recent decreases in the proportion of relatively young patients diagnosed with an initial STEMI. Patients with STEMI and NSTEMI had similar in-hospital outcomes and long-term survival. Trends in these and other important outcomes warrant continued monitoring.
Keywords: STEMI and NSTEMI, Young patients
Introduction
Using data from the population-based Worcester Heart Attack Study,1–4 we examined overall differences, and decade long trends, in the clinical characteristics, management, and in-hospital and long-term-outcomes associated with ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation myocardial infarction (NSTEMI) in young adults between the ages of 30 and 54 years who were hospitalized with a first acute myocardial infarction (AMI) at all greater Worcester (MA) medical centers in 6 biennial periods between 1999 and 2009.
Methods
The Worcester Heart Attack Study (WHAS) is an ongoing population-based clinical/epidemiologic investigation describing long-term trends in the incidence rates, hospital management practices, and death rates of greater Worcester, MA, residents hospitalized with AMI at all 11 metropolitan Worcester medical centers.1–4 For the present study we limited our sample to adults 30 to 54 years of age who were hospitalized with an independently validated initial AMI during 1999, 2001, 2003, 2005, 2007, and 2009. These years were selected due to funding availability and because we were interested in the surveillance of acute coronary disease in this central MA population on a biennial basis. This study was approved by the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School.
The methods used in this coronary disease surveillance study have been described elsewhere in detail.1–7 In brief, the medical records of potentially eligible residents of central Massachusetts who were hospitalized with discharge diagnoses consistent with the possible presence of AMI at all central MA medical centers were identified through the review of computerized hospital databases. Based on the independent review of previous and current hospital medical records by trained nurse and physician abstractors, patients with a prior history of AMI were excluded from the present population since we were interested in descriptive the descriptive epidemiology of patients with a first AMI in the present study. Diagnoses of STEMI and NSTEMI were made using standardized criteria.6,8 Since 2003, in the absence of electrocardiographic abnormalities, a diagnosis of NSTEMI was accepted when elevations in various cardiac biomarker assays, including troponin, were accompanied by typical clinical symptomatology and acute presentation.6,8
Trained study physicians and nurses abstracted clinical, demographic, and treatment related data from the medical records of patients with confirmed AMI.1–7 Receipt of cardiac medications, cardiac catheterization, percutaneous coronary intervention (PCI), and coronary artery bypass surgery, as well as development of important clinical complications during the patient’s index hospitalization, were determined using pre-established criteria.1–7 Survival status after hospital discharge was determined through a review of hospital records and a search of death certificates for residents of the Worcester metropolitan area. Follow-up was continued through 2011.
Short and long-term outcomes in each period were examined by calculating inhospital, 1 year, and 2 year case-fatality rates; trends in these endpoints were examined through the use of chi-square tests for trend. Logistic regression modeling was used to assess the significance of 1 and 2-year post discharge all-cause death rates in patients with STEMI versus NSTEMI while controlling for several potentially confounding demographic and clinical characteristics of prognostic importance.
Results
A total of 955 residents of the Worcester metropolitan area aged 30 to 54 years were hospitalized with an initial confirmed AMI at all 11 medical centers in central Massachusetts during the 6 years under study. The average age of this population was approximately 47 years and three quarters were men (Table 1). Overall, 52% of all young adults hospitalized for AMI were diagnosed with STEMI during the years under study. The percentage of patients with STEMI declined significantly between 1999 and 2009. In 1999, approximately two-thirds of all initial AMIs in our young adult population were STEMI in nature, whereas by 2009, two-fifths of all first AMIs in young adults had evidence of electrocardiographic ST-segment elevation.
Table 1.
Characteristics of young patients hospitalized with an initial acute myocardial infarction
| STEMI | NSTEMI | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Total (n=501) | 1999/2001 (n=209) | 2003/2005 (n=162) | 2007–2009 (n=130) | Total (n=454) | 1999/2001 (n=137) | 2003/2005 (n=162) | 2007–2009 (n=176) |
| Age (years) mean ± SD | ||||||||
| 47.3 ± 5.1 | 47.3 ± 5.3 | 46.9 ± 5.3 | 48.0 ± 4.7 | 47.8 ± 5.2 | 48.1 ±4.9 | 47.8 ± 5.1 | 47.6 ± 5.5 | |
| Male | 397 (79.4%) | 169 (80.9%) | 129 (79.6%) | 99 (76.2%) | 342 (75.3%) | 110 (80.3%) | 101 (71.6%) | 131 (74.4%)* |
| White | 435 (93.2%) | 185 (94.3%) | 137 (91.3%) | 113 (93.4%) | 378 (88.5%) | 118 (90.1%) | 115 (88.5%) | 145 (87.4%)* |
| Pre-hospital delay (median hours) | 1.5 | 1.5 | 1.5 | 1.6 | 2.0 | 2.0 | 2.0 | 2.1 |
| Angina pectoris | 39 (7.8%) | 26 (12.4%) | 11 (6.8%) | 2 (1.5%) | 46 (10.1%) | 16 (11.7%) | 18 (12.8%) | 12 (6.8%) |
| Current smoker | 261 (52.1%) | 98 (46.9%) | 87 (53.7%) | 76 (58.5%) | 228 (50.2%) | 66 (48.2%) | 78 (55.3%) | 84 (47.7%)* |
| Diabetes mellitus | 93 (18.6%) | 35 (16.8%) | 34 (21.0%) | 24 (18.5%)* | 112 (24.7%) | 28 (20.4%) | 37 (26.2%) | 47 (26.7%)* |
| Heart failure | 19 (3.8%) | 8 (3.8%) | 8 (4.9%) | 3 (2.3%)* | 40 (8.8%) | 11 (8.0%) | 15 (10.6%) | 14 (8.0%) |
| Hyperlipidemia1 | 278 (55.5%) | 105 (50.2%) | 92 (56.8%) | 81 (62.3%) | 275 (60.6%) | 75 (54.7%) | 72 (51.1%) | 128 (72.7%)* |
| Hypertension2 | 229 (45.7%) | 88 (42.1%) | 76 (46.9%) | 65 (50.0%)* | 254 (56.0%) | 65 (47.5%) | 83 (58.9%) | 106 (60.2%) ** |
| Body mass index (kg/m2) | ||||||||
| 25–29.9 | 177 (35.5%) | 55 (26.3%) | 65 (40.1%) | 57 (43.9%) | 138 (30.4%) | 35 (25.6%) | 43 (30.5%) | 60 (34.1%) |
| >30 | 245 (48.9%) | 120 (57.4%) | 75 (46.3%) | 50 (38.5%) | 244 (53.7%) | 91 (66.4%) | 66 (46.8%) | 87 (49.4%) |
| Presenting symptoms | ||||||||
| Abdominal pain | 19 (3.8%) | 12 (5.7%) | 5 (3.1%) | 2 (1.5%) | 21 (4.6%) | 4 (2.9%) | 8 (5.7%) | 9 (5.1%) ** |
| Back pain | 82 (16.4%) | 39 (18.7%) | 28 (17.3%) | 15 (11.5%) | 63 (13.9%) | 18 (13.1%) | 24 (17%) | 21 (11.9%) |
| Chest pain | 429 (85.6%) | 162 (77.5%) | 147 (90.7%) | 120 (92.3%) | 376 (82.8%) | 101 (73.7%) | 118 (83.7%) | 157 (89.2%) |
p< 0.05;
p< 0.001
Footnote: Hyperlipidemia1: Serum total cholesterol > 240 mg/dl; Hypertension2: Systolic blood pressure > 140 mm Hg and/or Diastolic blood pressure >90 mm Hg
Overall, patients with NSTEMI (n=454) were more likely to be obese and to have a history of heart failure, hypertension, and hyperlipidemia in comparison to patients with STEMI (n=501) (Table 1). Individuals hospitalized for NSTEMI were less likely to have presented to all central MA hospitals with chest pain, left arm pain, and diaphoresis while patients with STEMI tended to seek medical care sooner after the onset of acute coronary symptoms.
In all patients, the proportion of those with a history of angina decreased markedly during the period under study, particularly among STEMI patients (Table 1). Patients with STEMI were also less likely to have presented with diabetes over time. On the other hand, patients with NSTEMI had a marked increase in the prevalence of hypertension and hyperlipidemia during the years under surveillance.
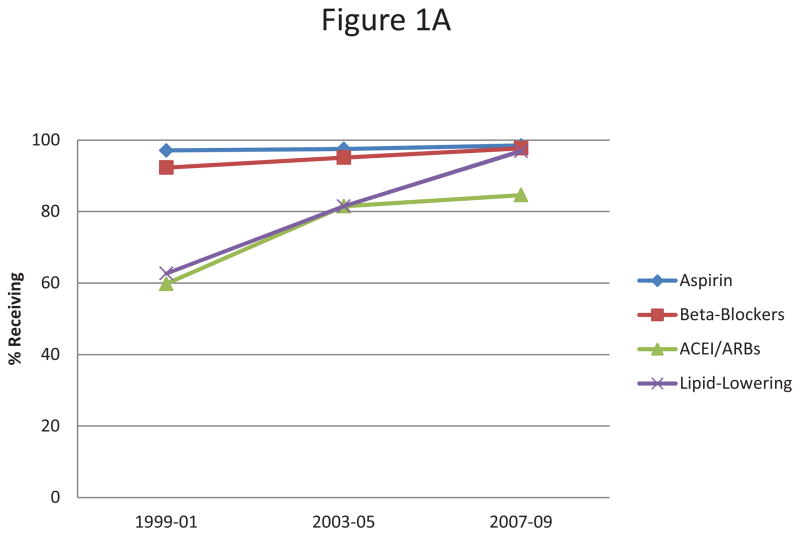
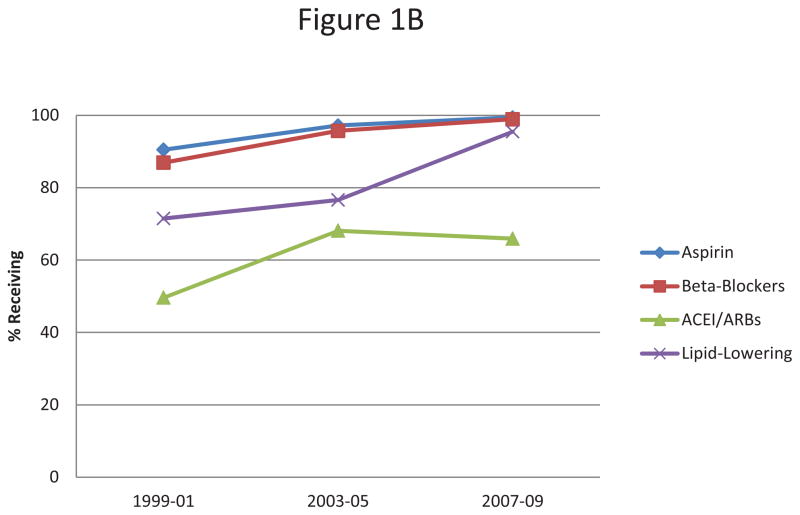
There were no significant differences between our respective comparison groups in the proportion of patients who were prescribed each of the effective cardiac medications examined. Throughout the study period, all patients were increasingly more likely to be prescribed each of the examined evidence-based cardiac medications while admitted to tall central MA hospitals (Figures 1A–B). A greater increase in the hospital use of ACE inhibitors/ARBs was noted among patients with STEMI over time, whereas a greater increase in the use of aspirin and beta-blockers was noted in patients with NSTEMI (Figures 1A–B).
Figure 1.
Figure 1A Receipt of hospital medical therapies in patients with an initial STEMI
Figure 1B Receipt of hospital medical therapies in hospitalized patients with an initial NSTEMI
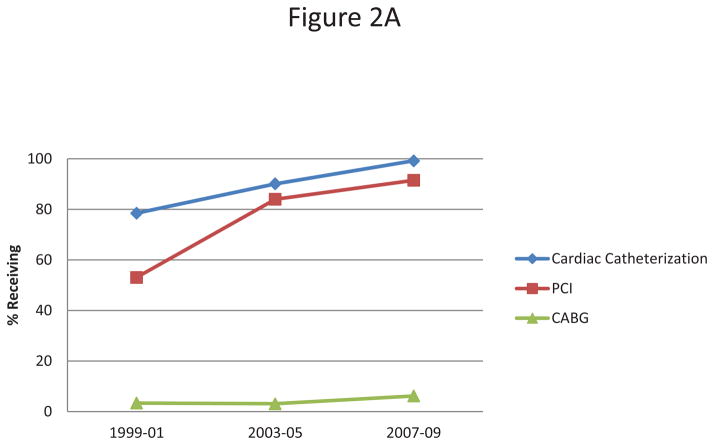
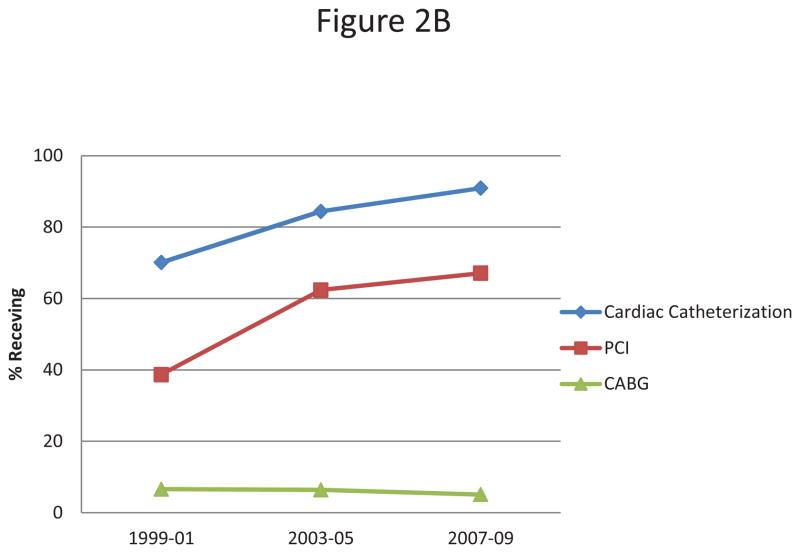
Patients with STEMI were more likely to have undergone cardiac catheterization and a PCI during their index hospitalization in comparison to patients diagnosed with NSTEMI. The proportion of patients undergoing cardiac catheterization increased from 79% to 99% and from 70% to 91%, in patients with STEMI and NSTEMI, respectively, between 1999 and 2009. The proportion of patients receiving a PCI increased from 53% to 92%, and from 39% to 67%, in patients with STEMI and NSTEMI, respectively, during the years under study (Figures 2A–B). When PCI was performed, door-to-balloon time was approximately 3 hours for STEMI patients compared to 22 hours for patients hospitalized with NSTEMI.
Figure 2.
Figure 2A Receipt of cardiac interventions in patients hospitalized with an initial STEMI
Figure 2B Receipt of cardiac interventions in patients hospitalized with an initial NSTEMI
There were no significant differences in the proportion of patients who developed several important hospital clinical complications, such as heart failure and atrial fibrillation, or who died during their index hospitalization, in patients with either an initial STEMI or NSTEMI (Table 2). Patients with STEMI were more likely to have developed cardiogenic shock, atrial fibrillation, and heart failure than patients with NSTEMI who were more likely to have developed acute stroke during their index hospitalization at all greater Worcester medical centers (Table 2).
Table 2.
Risk of developing selected hospital complications in young patients hospitalized with an initial acute myocardial infarction
| STEMI | P-Value | NSTEMI | P-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Complication | Total (n = 501) | 1999/01 (n =209) | 2003/05 (n = 162) | 2007/09 (n = 130) | Total (n = 454) | 1999/01 (n = 137) | 2003/05 (n = 141) | 2007/09 (n = 176) | ||
| Atrial fibrillation | 26 (5.2%) | 12(5.7%) | 9 (5.6%) | 5 (3.9%) | 0.26 | 15 (3.3%) | 7 (5.1%) | 6 (4.3%) | 2 (1.1%) | 0.24 |
| Heart failure | 85 (17.0%) | 42 (20.1%) | 14 (8.6%) | 29 (22.3%) | 0.28 | 51 (11.2%) | 20 (14.6%) | 17 (12.1%) | 14(8.0%) | 0.20 |
| Cardiogenic shock | 23 (4.6%) | 12 (5.7%) | 2 (1.2%) | 9 (6.9%) | 0.18 | 7 (1.5%) | 5 (3.7%) | 2 (1.4%) | 0 | 0.18 |
| Death | 17 (3.4%) | 6 (2.9%) | 4 (2.5%) | 7 (5.4%) | 0.22 | 12 (2.6%) | 5 (3.7%) | 5 (3.6%) | 2 (1.1%) | 0.11 |
| Length of Stay (median; days) | 3.0 | 4.0 | 3.0 | 3.0 | 0.27 | 3.0 | 3.0 | 3.0 | 3.0 | 0.88 |
In-hospital case-fatality rates for patients with STEMI remained relatively stable and low between 1999/01 and 2003/05, and increased slightly during the most recent study years. On the other hand, in-hospital death rates declined consistently in patients presenting with NSTEMI (Table 2).
Overall all-cause post-discharge death rates at 1 and 2 years in both patient groups were low. Death rates at 1 and 2 years were 0.6% and 0.7% for patients with STEMI, and 1.2% and 1.3% for those discharged after an NSTEMI, respectively (Table 3). Mortality remained relatively stable and low between 1999 and 2009 for STEMI patients while fluctuating somewhat for patients discharged from all central MA hospitals after an NSTEMI (Table 3). After controlling for several demographic and clinical factors of prognostic importance, the odds of dying at 1 (adjusted OR= 0.39; 95% CI 0.11;1.32) and 2 years (adjusted OR= 0.59; 95% CI 0.23;1.55) after hospital discharge for STEMI and NSTEMI patients were not significantly different, albeit consistently lower for those discharged after an initial STEMI.
Table 3.
Mortality rates at selected post-discharge time points in young patients hospitalized with an initial acute myocardial infarction
| Study period | Overall | 1999/01 | 2003/05 | 2007/09 | P-Value* | |
|---|---|---|---|---|---|---|
| STEMI | ||||||
| 1-year | 1.5%** | 0.6% | 2.1% | 1.9% | 0.81 | |
| 2-year | 2.4% | 2.4% | 2.8% | 1.9% | 0.63 | |
| NSTEMI | ||||||
| 1-year | 4.1% | 2.8 % | 6.6 % | 2.8% | 0.46 | |
| 2-year | 5.1% | 4.2% | 8.2 % | 2.8% | 0.36 | |
p for trend
p<0.01 when comparing 1-year overall mortality rates between STEMI and NSTEMI
Discussion
We found that the proportion of comparatively young residents of central MA hospitalized at all metropolitan Worcester medical centers with a first episode of STEMI decreased over time. The frequency of in-hospital clinical complications and hospital and post-discharge mortality were low and no significant differences in these endpoints were observed between patients with STEMI or NSTEMI.
Patients with NSTEMI presented with a higher frequency of most of the cardiovascular comorbidities examined at the time of their index hospitalization than patients who developed a STEMI. Similar results were reported in a study that combined data from 14 international randomized clinical trials with more than 120,000 patients with AMI.9 In the younger NSTEMI patients, hypertension and hyperlipidemia were more frequently diagnosed as compared to patients with STEMI.9 The prevalence of smoking was high in our patient population. Similar results were reported in a multicenter observational study of patients with AMI admitted to 60 coronary care units throughout Spain in 2000.10 These findings suggest a continuing need for interventions targeting smoking and other potentially preventable/treatable risk factors in young and middle-aged individuals to prevent the development of AMI.
The proportion of young patients diagnosed with an initial STEMI declined during the period under study. A similar change in the ratio of NSTEMIs to STEMIs was observed in the National Registry of Myocardial Infarction between 1990 and 2006.11 One potential explanation for our findings, and for the observed decline in the percentage of patients hospitalized with STEMI during recent years, was likely due to changes in the diagnosis of AMI that have incorporated the results of the more sensitive troponin assays which has likely led to more patients being diagnosed with NSTEMI (vs. unstable angina) over time.
Patients with STEMI were more likely to have undergone a PCI compared to patients with NSTEMI during their index hospitalization. Following current guidelines, early revascularization with PCI is the preferred first choice for the treatment of patients presenting with an STEMI.12 However, in a prospective study of 200 patients less than 35 years old hospitalized with AMI in 76 hospitals between 1997 and 2008, patients with NSTEMI were more likely to have received a PCI than those with STEMI.13 Similar to our findings, in a study of more than 44,000 AMI patients admitted to 113 hospitals between 1999 and 2005, increases in the utilization of PCI from 17% to 35%, and from 32% to 64%, respectively, for NSTEMI and STEMI patients were observed.14
The inconsistencies between previously published results and the findings of the present investigation with regards to the use of coronary interventions during hospitalization for AMI are most likely related to the younger age of patients in our study, different years under study, geographic, and physician practice differences. There are also data that clearly support the benefit of early revascularization with PCI in patients with STEMI, whereas catheterization followed by early revascularization among patients with NSTEMI has shown less consistent positive results.15
We failed to find any significant differences in our principal hospital outcomes between patients hospitalized with an initial STEMI or NSTEMI. The low frequency of various in-hospital adverse events was not unexpected since there tend to be fewer comorbidities and better overall health status in relatively young adult populations.16,17 Similar results have been reported from the Global Registry of Acute Coronary Events that described trends in the frequency of in-hospital events among comparatively young adults who were hospitalized with STEMI/NSTEMI between 1999 and 2007.14
In examining all-cause death rates during the first 2 years after hospital discharge for either STEMI or NSTEMI, no significant differences in post-discharge survival were observed between these two groups. Previous studies have reported similar findings on the long-term prognosis of patients with STEMI compared to patients with NSTEMI.13,18 In a large prospective study that was carried out at 76 hospitals in Switzerland between 1997 and 2008, the in-hospital death rate for young patients was 2.1% for patients who developed a STEMI and even lower for patients with an NSTEMI.13 These findings suggest that mortality rates are low after an AMI in young hospitalized patients and little differences exist in these rates between young patients who develop either a STEMI or NSTEMI.
The strengths of our study include its population-based design, inclusion of all hospitals from a well characterized metropolitan area, and decade-long perspective into the characteristics, management, and in-hospital and long-term outcomes in young patients hospitalized with either a STEMI or NSTEMI. Our study also has several limitations. Possible changes in the definition of AMI subtypes during the years under study may have contributed to the findings observed. The nonrandomized nature of our study precluded adjustment for the receipt of various treatment practices. We were unable to analytically control for other potentially important factors that may have influenced prognosis after AMI, including infarct size, serum lipid or blood pressure levels, or presence of adverse lifestyle practices.
Acknowledgments
Funding Source: National Institutes of Health (RO1 HL35434)
Dr. Tisminetzky is funded by Diversity Supplement R01 HL35434-29
Partial salary support is provided to Drs. McManus, Gore, and Goldberg by National Institute of Health grant 1U01HL105268-01 and to Dr. McManus by National Institutes of Health Grant KL2RR031981.
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434). Partial salary support for Drs. Goldberg and McManus was provided for by the National Institutes of Health grant 1U01HL105268-01. Dr. Tisminetzky was funded by Diversity Supplement National Institutes of Health R01 HL35434-29. Partial salary support was additionally provided to Dr. McManus by National Institutes of Health grant KL2RR031981.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975 2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Cir Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 3.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 4.Botkin NF, Spencer FA, Goldberg RJ, Lessard D, Yarzebski J, Gore JM. Changing trends in the long-term prognosis of patients with acute myocardial infarction: A population-based perspective. Am Heart J. 2006;151:199–205. doi: 10.1016/j.ahj.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): The Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 6.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McManus DD, Piacentine SM, Lessard D, Gore J, Yarzebski J, Spencer F, Goldberg RJ. Thirty-year (1975 to 2005) trends in the incidence rates, clinical features, treatment practices, and short-term outcomes of patients <55 years of age hospitalized with an initial acute myocardial infarction. Am J Cardiol. 2011;108:477–482. doi: 10.1016/j.amjcard.2011.03.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BA, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow RO, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasché P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S Writing Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. ESC Committee for Practice Guidelines (CPG) Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. [Google Scholar]
- 9.Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM, Brener SJ, Ellis SG, Lincoff AM, Topol EJ. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003;290:898–904. doi: 10.1001/jama.290.7.898. [DOI] [PubMed] [Google Scholar]
- 10.Morillas P, Bertomeu V, Pabón P, Ancillo P, Bermejo J, fernandez C, Aros F PRIAMHO II Investigators. Characteristics and outcomes of acute myocardial infarction in young patients. The PRIAMHO II study. Cardiology. 2006;107:217–225. doi: 10.1159/000095421. [DOI] [PubMed] [Google Scholar]
- 11.Rogers WJ, Frederick PD, Stoehr E, Canto JG, Ornato JP, Gibson CM, Pollack CV, Jr, Gore JM, Chandra-Strobos N, Peterson ED, French WJ. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1026–1034. doi: 10.1016/j.ahj.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 12.O’Gara P, Kushner F, Ascheim D, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Schoenenberger AW, Radovanovic D, Stauffer JC, Windecker S, Urban P, Niedermaier G, Keller PF, Gutzwiller F, Erne P AMIS Plus Investigators. Acute coronary syndromes in young patients: presentation, treatment and outcomes. Int J Cardiol. 2011;148:300–304. doi: 10.1016/j.ijcard.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA, Jr, Granger CB, Flather MD, Budaj A, Quill A, Gore JM GRACE Investigators. Declines in rates of death and hearth failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–1900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 15.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC, Jr, Jacobs AK, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction); American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association of Cardiovascular and Pulmonary Rehabilitation; Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/nonST-elevation myocardial infarction. Circulation. 2007;116:e148–e304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 16.Doughty M, Mehta R, Bruckman D, Das S, Karavite D, Tsai T, Eagle K. Acute myocardial infarction in the young—the University of Michigan experience. Am Heart J. 2002;143:56–62. doi: 10.1067/mhj.2002.120300. [DOI] [PubMed] [Google Scholar]
- 17.Awad HH, McManus DD, Anderson FA, Jr, Gore JM, Goldberg RJ. Young patients hospitalized with an acute coronary syndrome. Coron Artery Dis. 2013;24:54–60. doi: 10.1097/MCA.0b013e32835b0bf7. [DOI] [PubMed] [Google Scholar]
- 18.Montalescot G, Dallongeville J, Van Belle E, Rouanet S, Baulac C, Degrandsart A, Vicaut E OPERA Investigators. STEMI and NSTEMI: are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (the OPERA registry) Eur Heart J. 2007;28:1409–1417. doi: 10.1093/eurheartj/ehm031. [DOI] [PubMed] [Google Scholar]