Abstract
Morningness-Eveningness (ME) can be defined by the difference in individual diurnal preference observed from general behavioral patterns including sleep habits. The Horne & Östberg Morningness-Eveningness Questionnaire (MEQ) has been used for classifying ME types. We examined the reliability of a Korean version of the MEQ (Korean MEQ) and verified its validity by comparing responses on the Korean MEQ to objectively-recorded sleep-wake rhythms. After translating and back translating the MEQ from English into Korean, we examined the internal consistency of 19 items of the Korean MEQ in 91 subjects, and the test–retest reliability in 21 subjects who took the Korean MEQ twice, four weeks apart. The Korean MEQ was then administered to 1,022 young adult subjects. A subset of 46 morning, neither, and evening type subjects took part in a validation study in which their rest-activity timing was collected by actigraphy for 7 days. Cosinor analyses on these data were done to obtain the acrophase and amplitude of the sleep-wake rhythm. Cronbach's alpha of the total scores from the Korean MEQ was 0.77, and the test-retest reliability intra-class correlation coefficient was 0.90 (p<0.0001). There was a significant negative correlation between Korean MEQ score and reported sleep-wake timing among the entire cohort (p<0.0001). There was a significant difference in bedtime and wake time (on both work and free days), and in the mean sleep-wake rhythm acrophase, between ME types (p<0.01). In this study, the validity of the Korean MEQ was verified by illustrating the difference in acrophases of the sleep-wake rhythm between the ME types in young adults
Keywords: Korean MEQ, Sleep-wake rhythm, Sleep-wake timing, Test-retest reliability, ME type
INTRODUCTION
Morningness-eveningness (ME) is defined as diurnal preference, which reflects individual differences in the preferred time of activity, revealed in general behavior patterns, including sleep habits (Adan et al., 2012a). It has been generally shown that individuals with evening type (ET) tend to have later bedtimes and wake times than those with morning type (MT). In addition, ET tend to complain of poorer sleep quality than individuals with morning type (MT), hypothesized to be due to their irregular sleep timing and duration between weekdays and weekends as evidenced by greater caffeine intake and extended sleep on weekends (Taillard et al., 1999).
Besides these sleep-wake habits, ME types have been reported to show other behavioral differences including physiological response to stress (Willis et al., 2005; Roeser et al., 2012), speed of cognitive performance (Duffy et al., 2001), adaptation to shift work, characteristics of personality, and life style (Tankova et al., 1994). The Morningness-Eveningness Questionnaire (MEQ) of Horne and Östberg (1976) has been widely used for assessing diurnal types, and translations of the MEQ have been standardized in many countries (Torsvall et al., 1980; Ishihara et al., 1987; Tankova, Adan et al., 1994; Taillard et al., 2004; Jankowski et al., 2008).
The validation of the MEQ has usually been done by verifying the temporal difference in the timing of circadian rhythms of physiological variables such as melatonin, rectal temperature, or oral temperature between MTs and ETs (Horne et al., 1976; Ishihara et al., 1987; Liu et al., 2000; Griefahn et al., 2001).
It has also been done by examining differences in sleep timing and structure using nocturnal polysomnography (NPSG) (Ishihara et al., 1987), differences in light exposure using actigraphy (Staples et al., 2009), and differences in subjective sleep-wake habits (Taillard et al., 2004). Objective measurement of the sleep-wake rhythm can also be done using actigraphy (Thun et al., 2012), and has been demonstrated to be highly correlated with sleep timing as assessed by NPSG.
Demographic factors such as age, gender and work schedule need to be considered in testing the validity of the MEQ, as each of those factors has been shown to affect diurnal type (Roenneberg et al., 2007; Randler, 2011; Adan et al., 2012a). The tendency of eveningness in population samples usually increases during the teenage and young adult years, and it changes to morningness with aging (Roenneberg et al., 2007; Randler, 2011; Adan et al., 2012a). Several studies have compared MEQ scores in different age groups, finding that MEQ scores are influenced by age (Adan et al., 1990; Carrier et al., 1997; Duffy et al., 1999; Taillard et al., 2004; Roenneberg et al., 2007). Tankova et al. (Tankova et al., 1994) proposed that the critical age of change in ME preference is 50 years old based on Ishihara’s study. The initial validation of the MEQ was conducted by Horne and Östberg in young adults aged 18–32 years (Horne & Östberg, 1976). While Taillard validated the MEQ in middle-aged adults (Taillard et al., 2004), most validation studies have been conducted in college students and young adults (Horne & Östberg, 1976; Ishihara et al., 1987; Kerkhof et al., 1996; Jankowski & Ciarkowska, 2008).
Although age is closely related to ME preference, the distribution of the ME types by gender is not so clear (Adan & Almirall, 1990; Tankova et al., 1994). As reviewed by Adan et al. (Adan et al., 2012b), while some studies have reported that MT is more commonly observed among females (Chelminski et al., 1997; Adan et al., 2002; Borisenkov et al., 2012), other studies have reported that MT is greater in males (Merikanto et al., 2012) or have not found gender differences (Zimmermann, 2011). Such discrepancies have been hypothesized to be due to large age variances in sample populations (Randler, 2007).
Although studies of individual differences in circadian rhythms were recently carried out in Korea (Lee et al., 2005; Yang et al., 2005), those studies had limitations in describing sleep-wake habits and associated clinical features by ME type, because a standardized and validated Korean MEQ was not available. We therefore aimed in the present study to develop and test the reliability of a Korean version of the MEQ, and to verify its validity by comparing sleep-wake rhythms measured by actigraphy in young adult ME types identified using the Korean MEQ.
METHODS
Translation and back-translation of Korean MEQ
The MEQ was translated from English into Korean with the intent that people with various educational and cultural backgrounds could easily understand it. Correct grammar and vocabulary were used according to the content of the original version. Rather than direct translation of some of the English words that do not translate well into Korean, such words were replaced by commonly used Korean words with similar meanings. We administered the initial translated version of the Korean MEQ to 30 adults who visited the Health Promotion Center at Kangwon National University Hospital, and then made slight adjustments to it based on feedback from those individuals. This revised Korean MEQ was back-translated to English by a bilingual clinical psychologist, and this back-translated version was reviewed by a native English speaker who was familiar with the original questionnaire. The back-translated version was compared with the original English version of the MEQ, and further adjustment was made in the final Korean MEQ.
Test-retest reliability and internal consistency of Korean MEQ
We conducted a test-retest reliability evaluation of the Korean MEQ in 21 subjects. Each took the Korean MEQ, and four weeks later re-took the Korean MEQ. We also examined the internal consistency of responses on the Korean MEQ for 91 subjects.
After completing these initial tests on the Korean MEQ, the questionnaire was included as part of a larger Korean Sleep-Wake Questionnaire (SWQ-K).
Administration and validation of Korean MEQ - Subjects
The Korean MEQ, included as part of a larger Korean Sleep-Wake Questionnaire [SWQ-K, which also included a Korean version of the Epworth Sleepiness Scale (K-ESS; (Cho et al., 2011) and the Pittsburgh Sleep Quality Index translated into Korean (Korean PSQI)], was administered to subjects aged 18 years or older who visited the Chunchon National Museum or the Health Promotion Centers at Kangwon National University Hospital and Hyosung Hospital in Korea between May 2010 and February 2012. Because most prior validation studies of the MEQ were conducted in college students and young adults (Horne & Östberg, 1976; Ishihara, Miyasita et al., 1987; Kerkhof & Van Dongen, 1996; Jankowski & Ciarkowska, 2008), we selected adults aged 20–39 years for our validation of the Korean MEQ. After excluding subjects who fell outside this age range, those who were shift workers, those reporting a current sleep disorder diagnosis, and those with incomplete (n=6) or missing MEQ data (n=5), 1,022 subjects (mean age 32.3 ± 5.4 years, 330 men, 692 women) remained. The standard scores of the MEQ proposed by Horne & Östberg (Horne & Östberg, 1976) were used to categorize the subjects as morning type (MT), neither type (NT), or evening type (ET).
All participants were asked if they would be willing to take part in a validation study in which their sleep-wake rhythm was measured by actigraphy. From the 1,022 subjects who completed the Korean MEQ, 131 indicated their willingness to participate in an actigraphy study. Each of these individuals was screened before selecting participants for the actigraphy study. Subjects were excluded from taking part in the actigraphy study: (1) when their PSQI score was five or higher and poor sleep quality was identified by clinical interview (n=6); (2) when they were currently undergoing treatment for insomnia, psychiatric illness, or medical illness that could potentially impact sleep (n=6); (3) when they reported a history of drug/alcohol abuse or dependence, or currently taking medications known to affect sleep (n=7). Of the initial 131 participants who had agreed to take part in the actigraphy study, 112 were eligible to participate. Of these, 16 were MT, 20 were ET, and the remainder were NT. We invited all 16 of the MT and all 20 of the ET subjects, and the most recent 21 of the NT subjects in order to recruit the subjects with a higher motivation for the actigraphy validation study. Among 57 subjects, 46 subjects (15 MT, 16 ET, and 15 NT subjects) were selected for analysis, after excluding 6 subjects who had problems in wearing the actigraph and 5 subjects whose actiwatch data were collected at 15-second intervals by a technical error (Table 4).
Table 4.
Demographic characteristics and questionnaire scores in MT, NT and ET subjects
| MT (N=15) | NT (N=15) | ET(N=16) | ||
|---|---|---|---|---|
| Mean (SD) | p | |||
| Age (years) | 33.3 (6.11) | 31.00 (7.54) | 29.06 (7.24) | 0.228 |
| Gender† | ||||
| Female: male | 11:4 | 13:2 | 12:4 | 0.626 |
| Education (years) | 14.67 (2.06) | 16.47 (2.88) | 15.50 (2.03) | .0219 |
| Korean MEQ | 64.20 (5.0) | 49.93 (4.23) | 36.00 (5.03)* | <0.001 |
| K-ESS | 7.27 (2.94) | 9.20 (3.86) | 9.07 (4.45) | 0.384 |
| Korean PSQI | 4.00 (2.17) | 3.87 (1.85) | 4.93 (1.59) | 0.176 |
p<0.01 (Kruskal Wallis test or †X2 test)
MT: Morning type; NT: Neither type; ET: Evening type
MEQ: Morningness-Eveningness Questionnaire
K-ESS: Korean version of Epworth Sleepiness Scale
PSQI: Pittsburg Sleep Quality Index
Each participant in the actigraphy validation study provided written informed consent after full explanation of the procedures, and the study was approved by the Institutional Review Board at Kangwon National University Hospital. The study was conducted in accordance with the Declaration of Helsinki and the COPE guidelines (Portaluppi et al., 2010).
Validation of Korean MEQ - Sleep-wake rhythm collection and analysis
Each participant in the actigraphy validation study wore an activity monitor (Actiwatch-2, Philips-Respironics Co.) and maintained a sleep-wake log for seven days. Activity data were collected at one minute intervals.
The acrophase and amplitude of the sleep-wake rhythm were calculated by a curve fitting technique using the wrist activity data (Ancoli-Israel et al., 2003). Because the raw wrist activity data were recorded as 0 or 1, cosinor analysis was applied in order to transform the non-continuous variable to sleep-wake rhythm using the least-squares method. Amplitude was defined as the difference between the maximum and mean value of the cosine curve fit to the 24 hour cycle. Acrophase was defined as the phase angle of the maximum value of a sine function fitted to the raw data of a rhythm. The following was the functional formula for the cosinor analysis, and used the values (h=4)
Yt = f (t) + zt,
,
p is the length of period (24 hours),
αh1 is the amplitude, αh2 is the acrophase,
zt = ρ1zt−1 + ρ2zt−2 + ρ3zt−3 + … + ρqzt−q + εt, εt ~ N(0,σ2).
Statistical analysis
The test-retest reliability of the Korean MEQ was analyzed by Wilcoxon signed ranks test and Spearman correlation analysis. Cronbach’s alpha was used to quantify internal consistency of the Korean MEQ-K. To verify the construct validity of the Korean MEQ, a factor structure for the 4-factor model previously identified (Caci et al., 2009) was tested with the confirmatory factor analysis (CFA), using Amos 18.
The items with a factor loading of 0.4 or greater were defined as statistically significant (Comrey et al., 1992). Comparisons of acrophase and amplitude of the sleep-wake rhythm between MT, NT and ET groups were done by Kruskal-Wallis test to verify the criterion validity, and the Mann-Whitney test was applied for post-hoc analysis. Pearson correlation analyses between Korean MEQ score and the amplitude or acrophase of the sleep-wake rhythm derived from actigraphy were performed. Correlations between Korean MEQ score and weekday and weekend wake times for all 1,022 participants was also performed. All statistical analyses were done using SPSS for Windows (version 15.0) (SPSS, Inc, an IBM Company, Chicago, Illinois, USA). Null hypotheses of no difference were rejected if p-values were less than .05.
RESULTS
Reliability and internal consistency
For the test-retest reliability analysis, the total scores and each item score of the Korean MEQ were not significantly different between the first and second tests. The intraclass Spearman correlation coefficient of the total score of the Korean MEQ between the test and retest was 0.90 (p<0.0001), and those of the item scores were significantly correlated with r ranging between 0.47 and 0.85. Six of the items were not significantly correlated, with five of those items having r between 0.22 and 0.43 (see Table 1).
Table 1.
Test-retest reliability of the Korean MEQ (N=21)
| Item number |
1st Test | 2nd Test | Z | p† | Spearman Correlation |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | r | p | ||||
| 1 | 3.62 | 1.02 | 3.43 | .75 | −1.41 | .157 | .831 | <.0001 | |
| 2 | 3.00 | .71 | 3.14 | .79 | −.74 | .461 | −.328 | .147 | |
| 3 | 2.76 | .83 | 2.62 | .92 | −1.13 | .257 | .802 | <.0001 | |
| 4 | 2.62 | .92 | 2.81 | .93 | −1.10 | .271 | .604 | <.01 | |
| 5 | 2.86 | .91 | 2.57 | .75 | −1.90 | .058 | .749 | <.01 | |
| 6 | 1.90 | .77 | 1.76 | .70 | −1.00 | .317 | .620 | <.01 | |
| 7 | 2.48 | .81 | 2.48 | .51 | .00) | 1.000 | .643 | <.01 | |
| 8 | 2.38 | .87 | 2.29 | .72 | −.71) | .480 | .614 | <.01 | |
| 9 | 2.67 | .91 | 2.90 | .89 | −1.67 | .096 | .749 | <.0001 | |
| 10 | 3.33 | .86 | 3.10 | .63 | −1.18 | .238 | .333 | .140 | |
| 11 | 4.19 | 1.99 | 4.19 | 1.78 | .00 | 1.000 | .814 | <.0001 | |
| 12 | 1.62 | 1.36 | 1.95 | .92 | −.92 | .355 | .227 | .321 | |
| 13 | 2.05 | 1.02 | 2.00 | 1.00 | −.28 | .782 | .641 | <.01 | |
| 14 | 2.24 | .83 | 2.38 | .87 | −.76 | .448 | .352 | .118 | |
| 15 | 2.86 | 1.01 | 2.71 | .90 | −.55 | .582 | .471 | <.05 | |
| 16 | 1.86 | .73 | 1.81 | .75 | −.28 | .782 | .432 | .051 | |
| 17 | 3.24 | 1.18 | 3.10 | 1.04 | −.87 | .386 | .587 | <.01 | |
| 18 | 3.19 | .87 | 3.14 | .73 | −.30 | .763 | .215 | .350 | |
| 19 | 3.24 | 1.73 | 3.43 | 1.81 | −1.00 | .317 | .854 | <.0001 | |
| Total score | 52.10 | 11.48 | 51.81 | 10.19 | −.28 | .776 | .898 | <.0001 | |
:Wilcoxon signed ranks test
MEQ: Morningness-Eveningness Questionnaire
Cronbach’s alpha was used to determine internal consistency of the 19 items on the MEQ. For the total items of the Korean MEQ, Chronbach’s alpha was 0.77. This ranged between 0.74 and 0.78 if each item was deleted (Table 2). The item-total correlation coefficients of items 2, 10, 12 and 14 were between 0.04 and 0.09, and Cronbach's α was increased from 0.77 to 0.81 when these 4 items were deleted. All items of the Korean MEQ were included for the validation study, for there was little change in internal consistency when any of the items were deleted (Table 2).
Table 2.
Internal consistency of the Korea MEQ (N=91)
| Item number |
Mean | SD | Corrected item-total correlation |
Chronbach's α if item deleted |
|---|---|---|---|---|
| 1 | 3.77 | 0.85 | .45 | .76 |
| 2 | 3.14 | 0.68 | .07 | .78 |
| 3 | 2.67 | 0.92 | .35 | .76 |
| 4 | 2.49 | 0.91 | .56 | .75 |
| 5 | 2.70 | 0.76 | .52 | .75 |
| 6 | 1.86 | 0.83 | .29 | .76 |
| 7 | 2.36 | 0.75 | .49 | .75 |
| 8 | 2.33 | 0.91 | .37 | .76 |
| 9 | 2.93 | 0.95 | .48 | .75 |
| 10 | 3.29 | 1.03 | .04 | .78 |
| 11 | 4.20 | 1.78 | .59 | .74 |
| 12 | 1.53 | 1.29 | .08 | .78 |
| 13 | 2.29 | 1.04 | .26 | .77 |
| 14 | 2.33 | 0.97 | .09 | .78 |
| 15 | 3.01 | 0.92 | .43 | .76 |
| 16 | 1.87 | 0.82 | .14 | .77 |
| 17 | 3.21 | 0.91 | .38 | .76 |
| 18 | 3.20 | 0.69 | .53 | .75 |
| 19 | 3.04 | 1.99 | .60 | .74 |
| Total | Chronbach's α=.77 | |||
MEQ: Morningness-Eveningness Questionnaire
Validity
The adequacy of the 4-factor model was explored by several goodness-of-fit indices. RMSEA indicated a good fit (0.049), and a χ2 test indicated an acceptable fit [χ2/df (502.84/146) = 3.4, p < 0.001] although the other fit indices were below the thresholds for the acceptable fit (NFI=0.820; IFI = 0.865; CFI = 0.863; NNFI = 0.822) (Hu et al., 1999). For the 4-factor model, seven items (2, 8, 10, 12, 13, 14, and 16) showed low and non-significant factor loadings (<0.4), and the five of these items (2, 8, 10, 12, and 16) were included in factor 3 (Retiring). Particularly, item 12 and 16 showed very low factor loadings. All other factor loadings were significant and ranged above 0.40 (Table 3).
Table 3.
Factor loading for confirmatory factor analysis of the Korean MEQ (N=1,022)
| Item | Factor 1 | Factor 2 | Factor 3 | Factor 4 |
|---|---|---|---|---|
| 11 | 0.559 (0.699) | (0.002) | (0.169) | (0.178) |
| 1 | 0.537(0.414) | (0.007) | (0.253) | (0.339) |
| 18 | 0.531(0.490) | (0.007) | (0.334) | (0.040) |
| 17 | 0.521(0.653) | (0.014) | (0.156) | (0.006) |
| 9 | 0.436(0.418) | (0.237) | (0.239) | (0.274) |
| 15 | 0.421(0.526) | (0.080) | (0.005) | (0.148) |
| 7 | (0.045) | 0.653(0.950) | (0.004) | (0.051) |
| 4 | (0.195) | 0.581(0.644) | (0.008) | (0.077) |
| 5 | (0.048) | 0.576(0.946) | (0.032) | (0.035) |
| 6 | (0.011) | 0.486(0.211) | (0.113) | (0.044) |
| 19 | (0.346) | (0.179) | 0.748(0.460) | (0.144) |
| 8 | (0.262) | (0.022) | 0.363(0.455) | (0.393) |
| 2 | (0.041) | (0.001) | 0.324(0.753) | (0.171) |
| 10 | (0.183) | (0.031) | 0.289(0.579) | (0.077) |
| 14 | (0.034) | (0.086) | 0.234(0.214) | (0.038) |
| 16 | (0.116) | (0.052) | 0.090(0.632) | (0.131) |
| 12 | (0.044) | (0.059) | 0.031(0.587) | (0.117) |
| 3 | (0.093) | (0.046) | (0.110) | 0.565(0.471) |
| 13 | (0.011) | (0.067) | (0.099) | 0.372(0.562) |
(): reference values from Caci et al. (2009)
Factor 1 (items 1, 9, 11, 15, 17 and 18): Peak Time; Factor 2 (items 4, 5 and 7): Morning Affect; Factor 3 (items 2, 8, 10, 12, 16 and 19): Retiring; Factor 4 (items 3 and 13): Rising
MEQ: Morningness-Eveningness Questionnaire
Loadings greater than |0.400| are in bold.
Comparison of MT, NT and ET groups
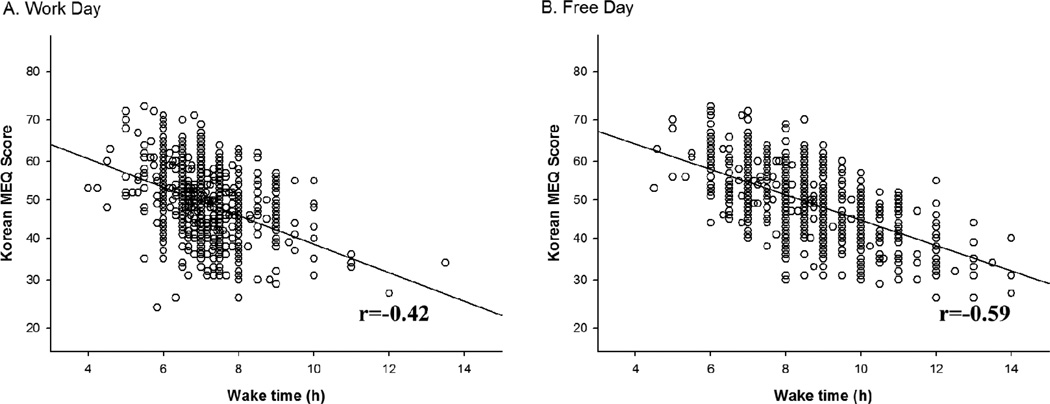
There were significant differences in the bedtimes, wake times, and the timing of mid-sleep on both work days and free days between the MT, NT and ET groups, with those of the ET subjects being significantly later than those of the MT subjects (see Table 5). There was a significant negative correlation between Korean MEQ score and bedtime [both on work days (r=−0.46, p<0.0001 and on free days r=−0.53, p<0.0001)], and between Korean MEQ score and wake time (see Figure 1). The sleep durations of the ET subjects on free days were significantly longer than those of the MT subjects. There was no difference in self-reported sleep latency, sleep need, or caffeine intake between the three groups (Table 5)
Table 5.
Self-reported sleep-wake habits, sleep need, and caffeine intake in MT, NT and ET subject
| MT (N=15) | NT (N=15) | ET (N=16) | |||
|---|---|---|---|---|---|
| Mean (SD) | p | Post hoc | |||
| Work day: | |||||
| Bedtime | 23:25 (55) | 23:00 (235) | 00:23 (47)* | 0.044 | MT<ET |
| Wake time | 06:16 (43) | 07:27 (30) | 07:51 (94)** | <0.001 | MT<NT=ET |
| Midsleep time | 02:51 (34) | 03:37 (49) | 04:07 (67)** | <0.0001 | MT<NT=ET |
| Sleep latency (min) | 13.33 (12.38) | 9.17 (7.42) | 18.68 (12.76) | 0.089 | |
| Sleep duration (hr) | 6.67 (1.29) | 7.20 (1.24) | 7.50 (1.17) | 0.211 | |
| Free day: | |||||
| Bedtime | 23:36 (55) | 23:37 (223) | 01:36 (102)** | 0.003 | MT=NT<ET |
| Wake time | 06:49 (45) | 08:37 (80) | 10:02 (115)** | <0.001 | MT<NT<ET |
| Midsleep time | 03:12 (39) | 04:31 (74) | 05:49(101)** | <0.001 | MT<NT<ET |
| Sleep latency (min) | 13.83 (10.85) | 8.87 (6.84) | 17.61 (11.56) | 0.095 | |
| Sleep duration (hr) | 7.10 (1.12) | 8.60 (1.23) | 9.32 (1.31)** | <0.001 | MT<NT=ET |
| Sleep need (hr) | 7.40 (1.39) | 8.33 (1.11) | 8.61 (1.52) | 0.71 | |
| Caffeine intake (cup/ day) | 2.25 (1.07) | 1.93 (1.32) | 2.52 (2.11) | 0.488 | |
p<0.05,
p<0.01 (Kruskal-Wallis test)
SD presented as minutes
MT: Morning type; NT: Neither type; ET: Evening type
Figure 1.
Correlation of habitual wake time on work days (left panel) and free days (right panel) with Korean MEQ score among all 1,022 subjects.
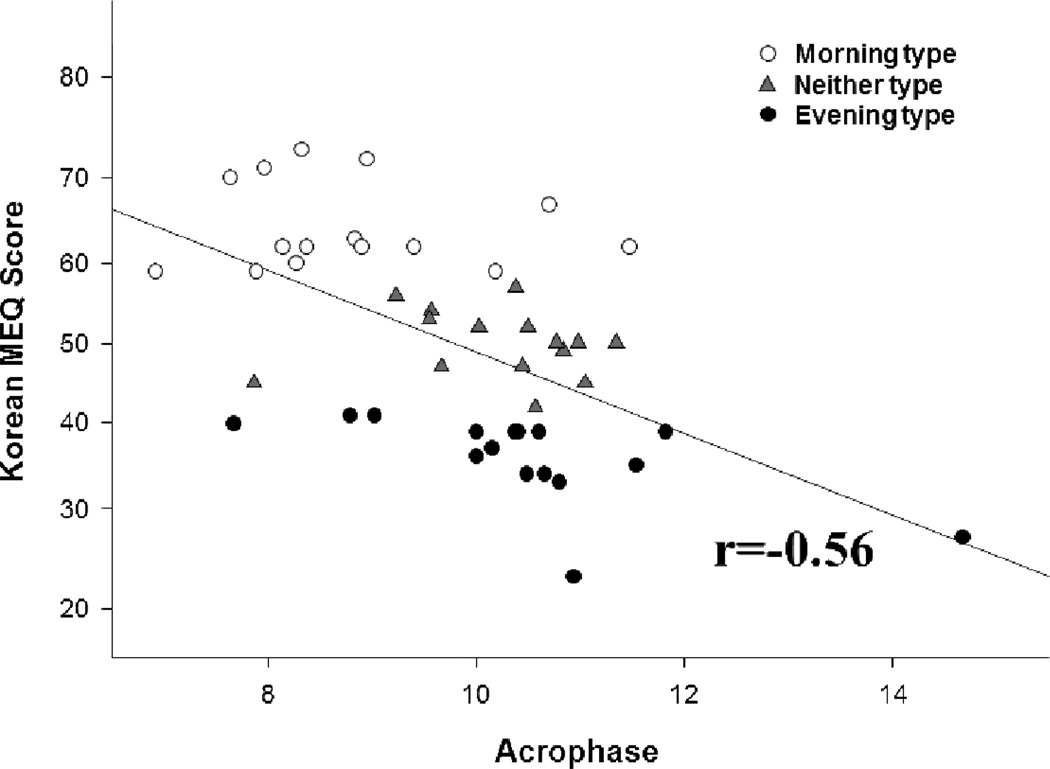
Activity data from three subjects who drank alcohol or removed the actigraph during the daytime were excluded from analysis. Data from three additional subjects with technical errors in actigraphy or sleep log data were also excluded. Data from five subjects whose actigraphy data were collected in 15 second epochs rather than one minute epochs were also excluded, for consistency in the sleep-wake rhythm analysis. Data from forty-six subjects (15 MT, 16 ET and 15 NT subjects) were included in the final analysis (Table 4). The mean acrophase of the sleep-wake rhythm was significantly different between MT, NT and ET groups, with those of MT subjects significantly earlier than those of ET subjects (Table 6). There was no difference in the mean sleep-wake amplitude among the three groups (Table 6). The Korean MEQ scores were negatively correlated with the acrophases of the sleep-wake rhythm among all the subjects (see Figure 2)
Table 6.
Actigraphy acrophase and amplitude in MT, NT and ET subjects
| MT (N=15) | NT (N=15) | ET (N=16) | |||
|---|---|---|---|---|---|
| Mean (SD) | p | Post hoc | |||
| Acrophase | 08:47 (72) | 10:11 (53) | 10:29 (90)* | 0.003 | MT<NT=ET |
| Amplitude | 0.568 (0.078) | 0.562 (0.063) | 0.541 (0.086) | 0.568 | |
p<0.01 (Kruskal-Wallis test)
SD presented as minutes
MT: Morning type; NT: Neither type; ET: Evening type
Figure 2.
Correlation of sleep-wake rhythm acrophase with Korean MEQ score in Morning Type (open circle, N=15), Neither Type (triangle, N=15), and Evening Type (filled circle, N=16) subjects.
DISCUSSION
We found that the Korean MEQ showed an internal consistency similar to that found previously in both Polish (Jankowski & Ciarkowska, 2008) and Japanese (Ishihara et al., 1987) versions of the MEQ. In a recent review of various scales of circadian typology (Di Milia et al., 2013), the MEQ as well as the Composite Scale of Morningness and the Preferences Scale each showed high levels of reliability (>0.80). In our study, Cronbach`s alpha for the Korean MEQ was slightly lower.
The test-retest correlation coefficient of the Korean MEQ scores was 0.90 in our study. However, in six individual items the correlation coefficient was relatively lower (−0.33~ 0.43) where no difference in the intraclass item scores was found. Four of the 6 items with low test-retest correlation were associated with evening activity. In a study of the sleep-wake habits in residents of Papua New Guinea (Siegmund et al., 1998), it was observed that intra-individual diurnal variations of evening activity were greater than those of the morning activity, a result of the reduced synchronization to external zeitgebers. Therefore, our result of relatively lower test-retest correlations in the items relating to evening activity could reflect greater variability in the onset time of the main sleep episode in the evening. In fact, the answers to item 14, a question about night duty, were consistent in only 4 of the 14 subjects without shift work history (29%) but were consistent in 5 of the 7 subjects with a shift work history (71%). This suggests that the reliability of item 14 is lower for subjects who have not experienced shift work. This aspect of item 14 should be considered in interpreting our results.
A 4-factor model was identified in the validation of a French version of the MEQ (Caci et al., 2009). It consisted of peak time (items 1, 9, 11, 15, 17 and 18), morning affect (items 4, 5 and 7), retiring (items 2, 8, 10, 12, 16 and 19) and rising (items 3 and 13) factors. Our result of confirmatory factor analysis for a four-factor model indicated acceptable construct validity (RMSEA= 0.049, χ2/df = 3.4). On the other hand, Smith et al., (Smith et al., 1989) reported that two factors (morning and evening factors) were extracted from the original 19-item English MEQ (Smith et al., 1989). We therefore applied confirmatory factor analysis for a two-factor model to our data as well. The RMSEA for the two-factor model indicated a reasonable fit (RMSEA= 0.063), but the other fit indices including χ2/df (502.837/146=5.09) were below the thresholds for acceptable fit and lower compared to those of the four-factor model. This suggests that the factor structure of the Korean MEQ is better explained by the 4-factor model. All items included in factors 1 (peak time) and 2 (morning affect) were observed with a significant factor loading just as identified by Caci et al., (Caci et al., 2009). However, factor 3 (retiring) was not suitably explained. This discrepancy might result from cross-cultural differences. Two items of factor 4 (rising) were consistent with the results of Caci et al. (Caci et al., 2009), although the factor loading in item 13 was lower. Besides, four items (2, 10, 12, and 14) with relatively lower item-total correlation coefficients among 19 items would be deleted in order to develop a reduced version of Korean MEQ. Nevertheless, we applied all the items to the Korean MEQ since one of the aims of this study was to show a cross-cultural validity for the scale. In the overall cohort, we found a significant negative correlation between Korean MEQ score and bedtime or wake time, with a stronger correlation in both cases when weekend (free day) vs. weekday wake time was used. This finding is likely due to weekday sleep-wake times in this population being constrained by the need to rise for work, while weekend sleep-wake times may be less constrained and thus better reflect the underlying chronotype (Taillard et al., 1999). This concept has been described as “social jet lag” (Wittmann et al., 2006).
In the validation subset in our study, there was a significant negative association between Korean MEQ score and the timing of activity acrophase, whereby the lower the MEQ score (more eveningness) the more delayed the activity acrophase was. Furthermore, we found the mean activity acrophase of the ET group was nearly two hours later than that of the MT group, consistent with a prior study that used actigraphy (Kerkhof & Van Dongen, 1996). This difference was even greater on free days than on work days as previously reported (Giannotti et al., 2002; Mongrain et al., 2004). However, among the MT group there was no difference in the bedtime and wake time between work days and free days. This finding is similar to prior reports (Pullman et al., 2012). We also found that sleep duration on free days in the ET group was extended compared to the MT group (and compared to ET weekday sleep duration), consistent with previous reports (Giannotti et al., 2002; Mongrain et al., 2004; Pullman et al., 2012) and with our finding in the larger study cohort. We did not find any significant difference in ESS or PSQI score by ME-preference, but this could be due to our relatively small sample size.
In their original validation study of the MEQ, Horne and Östberg found a difference of approximately one hour in the timing of the oral temperature rhythm between M and E types, with self-reported sleep times differing by one to two hours (Horne & Östberg, 1976). The timing of sleep and wakefulness is the most obvious rhythmic human behavior, and is determined in part by an underlying circadian rhythm (Roenneberg et al., 2007; Soehner et al., 2011). Other studies have reported that the difference in the timing of a variety of physiological circadian rhythms between M and E types ranges from approximately one to five hours (Yoon et al., 1994; Kerkhof & Van Dongen, 1996; Duffy et al., 1999; Baehr et al., 2000; Liu et al., 2000; Griefahn, 2002). Although our study did not assess the timing of any physiologic circadian rhythms, the activity rhythm acrophase showed clear differences in behavioral characteristics between the M and E types, verifying that the Korean MEQ is a valid questionnaire for the classification of ME types.
All together, the sleep-wake patterns between the M and E types classified by the Korean MEQ were well differentiated and similar to findings from previous studies, suggesting that the Korean MEQ is a robust and useful scale for the classification of chronotypes among Koreans.
Our study does have limitations. First, physiological markers of endogenous circadian rhythms such as rectal temperature or melatonin were not measured. Additional studies will be required to examine differences in endogenous circadian rhythms and sleep architecture among the ME types classified by the Korean MEQ, although we did observe a difference in sleep-wake rhythm timing between the groups similar to that reported with other language versions of the MEQ. While our study ensured the homogeneity of study subjects and comparability with the original MEQ by limiting the subjects’ ages, additional studies will be required to test and determine norms for other age groups in Korea. Finally, our study participants overall were well-educated and of high socio-economic status, and thus the Korean MEQ may not be valid for use in less educated or lower socio-economic individuals.
ACKNOWLEDGMENTS
This paper was presented at the 2012 Annual Meeting of the Associated Professional Sleep Societies in Boston, United States. This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-0003160 to JHL). JFD was supported by NIH grants R01 HL080978, R01 AG044416, R01 HL093279, P01 AG09975 and by the Brigham and Women’s Hospital BRI Fund to Sustain Research Excellence.
Dr. Duffy reports that she has received investigator-initiated research funding from Philips-Respironics that is unrelated to the present study. Dr. Duffy is a member of the Board of Directors of the Sleep Research Society.
Footnotes
DECLARATION OF INTEREST
The authors report no financial conflicts of interest associated with the present paper.
REFERENCES
- Adan A, Almirall H. Adaptation and standardization of a Spanish version of the morningness-eveningness questionnaire: Individual differences. Pers. Individ. Dif. 1990;11:1123–1130. [Google Scholar]
- Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C. Circadian typology: a comprehensive review. Chronobiol. Int. 2012a;29:1153–1175. doi: 10.3109/07420528.2012.719971. [DOI] [PubMed] [Google Scholar]
- Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C. Circadian typology: A comprehensive review. Chronobiol. Int. 2012b;29:1153–1175. doi: 10.3109/07420528.2012.719971. [DOI] [PubMed] [Google Scholar]
- Adan A, Natale V. Gender differences in morningness-eveningness preference. Chronobiol. Int. 2002;19:709–720. doi: 10.1081/cbi-120005390. [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S, Cole R, Alessi C, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–392. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- Baehr EK, Revelle W, Eastman CI. Individual differences in the phase and amplitude of the human circadian temperature rhythm: With an emphasis on morningness-eveningness. J. Sleep Res. 2000;9:117–127. doi: 10.1046/j.1365-2869.2000.00196.x. [DOI] [PubMed] [Google Scholar]
- Borisenkov MF, Kosova AL, Kasyanova ON. Impact of perinatal photoperiod on the chronotype of 11- to 18-year-olds in northern European Russia. Chronobiol. Int. 2012;29:305–310. doi: 10.3109/07420528.2011.653612. [DOI] [PubMed] [Google Scholar]
- Caci H, Deschaux O, Adan A, Natale V. Comparing three morningness scales: age and gender effects, structure and cut-off criteria. Sleep Med. 2009;10:240–245. doi: 10.1016/j.sleep.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Carrier J, Monk TH, Buysse DJ, Kupfer DJ. Sleep and morningness-eveningness in the 'middle' years of life (20–59y) J. Sleep Res. 1997;6:230–237. doi: 10.1111/j.1365-2869.1997.00230.x. [DOI] [PubMed] [Google Scholar]
- Chelminski I, Ferraro FR, Petros T, Plaud JJ. Horne and Ostberg Questionnaire: a score distribution in a large sample of young adults. Pers. Individ. Dif. 1997;23:647–652. [Google Scholar]
- Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011;15:377–384. doi: 10.1007/s11325-010-0343-6. [DOI] [PubMed] [Google Scholar]
- Comrey AL, Lee HB. A first course in factor analysis. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.; 1992. [Google Scholar]
- Di Milia L, Adan A, Natale V, Randler C. Reviewing the Psychometric Properties of Contemporary Circadian Typology Measures. Chronobiol. Int. 2013:1–11. doi: 10.3109/07420528.2013.817415. [DOI] [PubMed] [Google Scholar]
- Duffy JF, Dijk DJ, Hall EF, Czeisler CA. Relationship of endogenous circadian melatonin and temperature rhythms to self-reported preference for morning or evening activity in young and older people. J. Investig. Med. 1999;47:141–150. [PMC free article] [PubMed] [Google Scholar]
- Duffy JF, Rimmer DW, Czeisler CA. Association of intrinsic circadian period with morningness-eveningness, usual wake time, and circadian phase. Behav. Neurosci. 2001;115:895–899. doi: 10.1037//0735-7044.115.4.895. [DOI] [PubMed] [Google Scholar]
- Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J. Sleep Res. 2002;11:191–199. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]
- Griefahn B. The validity of the temporal parameters of the daily rhythm of melatonin levels as an indicator of morningness. Chronobiol. Int. 2002;19:561–577. doi: 10.1081/cbi-120004226. [DOI] [PubMed] [Google Scholar]
- Griefahn B, Künemund C, Bröde P, Mehnert P. Zur Validität der deutschen Übersetzung des Morningness-Eveningness-Questionnaires von Horne und Östberg. Somnologie. 2001;5:71–80. [Google Scholar]
- Horne JA, Östberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling. 1999;6:1–55. [Google Scholar]
- Ishihara K, Miyasita A, Inugami M, Fukuda K, Miyata Y. Differences in sleep-wake habits and EEG sleep variables between active morning and evening subjects. Sleep. 1987;10:330–342. doi: 10.1093/sleep/10.4.330. [DOI] [PubMed] [Google Scholar]
- Jankowski KS, Ciarkowska W. Diurnal variation in energetic arousal, tense arousal, and hedonic tone in extreme morning and evening types. Chronobiol. Int. 2008;25:577–595. doi: 10.1080/07420520802261770. [DOI] [PubMed] [Google Scholar]
- Kerkhof GA, Van Dongen HPA. Morning-type and evening-type individuals differ in the phase position of their endogenous circadian oscillator. Neurosci. Lett. 1996;218:153–156. doi: 10.1016/s0304-3940(96)13140-2. [DOI] [PubMed] [Google Scholar]
- Lee JH, Cho YW, Sohn SI, Lee H, Lim JG, Yi SD, Lee MY. Excessive daytime sleepiness and quality of sleep in Korean middle and high school students. J. Kor. Sleep Soc. 2005;2:24–40. [Google Scholar]
- Liu X, Uchiyama M, Shibui K, Kim K, Kudo Y, Tagaya H, Suzuki H, Okawa M. Diurnal preference, sleep habits, circadian sleep propensity and melatonin rhythm in healthy human subjects. Neurosci. Lett. 2000;280:199–202. doi: 10.1016/s0304-3940(00)00793-x. [DOI] [PubMed] [Google Scholar]
- Merikanto I, Kronholm E, Peltonen M, Laatikainen T, Lahti T, Partonen T. Relation of chronotype to sleep complaints in the general Finnish population. Chronobiol. Int. 2012;29:311–317. doi: 10.3109/07420528.2012.655870. [DOI] [PubMed] [Google Scholar]
- Mongrain V, Lavoie S, Selmaoui B, Paquet J, Dumont M. Phase relationships between sleep-wake cycle and underlying circadian rhythms in Morningness-Eveningness. J. Biol. Rhythms. 2004;19:248–257. doi: 10.1177/0748730404264365. [DOI] [PubMed] [Google Scholar]
- Portaluppi F, Smolensky MH, Touitou Y. Ethics and methods for biological rhythm research on animals and human beings. Chronobiol. Int. 2010;27:1911–1929. doi: 10.3109/07420528.2010.516381. [DOI] [PubMed] [Google Scholar]
- Pullman RE, Roepke SE, Duffy JF. Laboratory validation of an in-home method for assessing circadian phase using dim light melatonin onset (DLMO) Sleep Med. 2012;13:703–706. doi: 10.1016/j.sleep.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randler C. Gender differences in morningness�eveningness assessed by self-report questionnaires: A meta-analysis. Pers. Individ. Dif. 2007;43:1667–1675. [Google Scholar]
- Randler C. Age and gender differences in morningness–eveningness during adolescence. J. Genet. Psychol. 2011;172:302–308. doi: 10.1080/00221325.2010.535225. [DOI] [PubMed] [Google Scholar]
- Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, Merrow M. Epidemiology of the human circadian clock. Sleep Med. Rev. 2007;11:429–438. doi: 10.1016/j.smrv.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Roeser K, Obergfell F, Meule A, Vogele C, Schlarb AA, Kubler A. Of larks and hearts--morningness/eveningness, heart rate variability and cardiovascular stress response at different times of day. Physiol. Behav. 2012;106:151–157. doi: 10.1016/j.physbeh.2012.01.023. [DOI] [PubMed] [Google Scholar]
- Siegmund R, Tittel M, Schiefenhovel W. Activity monitoring of the inhabitants in Tauwema, a traditional Melanesian village: Rest/activity behaviour of Trobriand islanders (Papua New Guinea) Biol. Rhythm Res. 1998;29:49–59. [Google Scholar]
- Smith CS, Reilly C, Midkiff K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. J. Appl. Psychol. 1989;74:728–738. doi: 10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- Soehner AM, Kennedy KS, Monk TH. Circadian preference and sleep-wake regularity: associations with self-report sleep parameters in daytime-working adults. Chronobiol. Int. 2011;28:802–809. doi: 10.3109/07420528.2011.613137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staples VS, Archer SN, Arber S, Skene DJ. Daily light exposure profiles in older non-resident extreme morning and evening types. J. Sleep Res. 2009 doi: 10.1111/j.1365-2869.2009.00762.x. [DOI] [PubMed] [Google Scholar]
- Taillard J, Philip P, Bioulac B. Morningness/eveningness and the need for sleep. J. Sleep Res. 1999;8:291–295. doi: 10.1046/j.1365-2869.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- Taillard J, Philip P, Chastang JF, Bioulac B. Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J. Biol. Rhythms. 2004;19:76–86. doi: 10.1177/0748730403259849. [DOI] [PubMed] [Google Scholar]
- Tankova I, Adan A, Buela-Casal G. Circadian typology and individual differences. A review. Pers. Individ. Dif. 1994;16:671–684. [Google Scholar]
- Thun E, Bjorvatn B, Osland T, Steen VM, Sivertsen B, Johansen T, Lilleholt TH, Udnes I, Nordhus IH, Pallesen S. An actigraphic validation study of seven morningness-eveningness inventories. Eur. Psychol. 2012;17:222–230. [Google Scholar]
- Torsvall L, Åkerstedt T. A diurnal type scale. Scand. J. Work Environ. Health. 1980;6:283–290. doi: 10.5271/sjweh.2608. [DOI] [PubMed] [Google Scholar]
- Willis TA, O'Connor DB, Smith L. The influence of morningness-eveningness on anxiety and cardiovascular responses to stress. Physiol. Behav. 2005;85:125–133. doi: 10.1016/j.physbeh.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol. Int. 2006;23:497–509. doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005;115:250–256. doi: 10.1542/peds.2004-0815G. [DOI] [PubMed] [Google Scholar]
- Yoon JS, Kook SH, Shin IS, Shin MS, Choi Y, Lee MS, Lee HY. A comparison of nighttime sleepiness, performance, and body temperature between morning-type and evening-type persons. Sleep Med. Psychophysiology. 1994;1:47–59. [Google Scholar]
- Zimmermann LK. Chronotype and the transition to college life. Chronobiol. Int. 2011;28:904–910. doi: 10.3109/07420528.2011.618959. [DOI] [PubMed] [Google Scholar]