Abstract
BACKGROUND
The United States has a culturally and demographically diverse populace, and the aim of this study was to examine differences in health preferences by gender, age, ethnicity, and race.
METHODS
We assessed preferences for health outcomes defined by the PROMIS-29 survey in a sample of the U.S. population. Based on the survey’s 540 paired comparisons trading off lifespan and 7 domains of health-related quality of life (HRQoL), we compared the choices between men and women, adults age 18 to 54 years and 55 years and older, Hispanics and non-Hispanics and non-Hispanic Blacks and Whites. For each subgroup, we estimated the value of 122 HRQoL outcomes on a quality-adjusted life year (QALY) scale and tested for subgroup differences.
RESULTS
Compared to men, women preferred reduced lifespan over losses in HRQoL, particularly for depression. Compared to the younger adults, older adults preferred reduced lifespan over the symptoms of depression, anxiety, and fatigue. Compared to non-Hispanic Whites, Hispanics preferred reduced lifespan over depression and sleep disturbance, but held similar values on losses in physical functioning. Among non-Hispanics, Blacks preferred reduced lifespan over losses in ability to climb stairs and to fall asleep compared to Whites, but held similar values on mental health outcomes.
CONCLUSION
With the growing emphasis on patient-centeredness and culturally sensitive treatment, it is important to recognize the diversity in values placed on potential losses in HRQoL, particularly mental health outcomes. Demographic differences in preferences may influence comparative or cost effectiveness of treatments as perceived by one or another subgroup.
Keywords: Quality-adjusted life years, discrete choice experiments, patient-reported outcomes, preferences, Health-related Quality of Life (HRQoL)
INTRODUCTION
Demographic differences in health preferences are important considerations in health policy, the implementation of clinical guidelines, medical decision making, and study design. Not all decisions relating to public resources follow the “tyranny of the majority,” where the majority interests are placed above those of a minority.(1) Health policy may allocate greater authority to the preferences of a greatly affected minority (e.g., sickle-cell and African Americans). Likewise, in clinical guidelines, it may be more appropriate to value health outcomes from a specific perspective (e.g., women and menopausal symptoms).(2–5) Physicians who wish to personalize treatments may prescribe differently or tailor clinic protocols, because they take the time to inquire about the preferences of the patient in front of them and account for the variability of preferences within the clinic populations.(6–8) Knowledge of differences in health preferences also influences study design, particularly quota sampling. For example, if men and women share values on all domains of health, studies that oversample men or women would produce identical results (e.g., U.S. valuation of the EQ-5D).(3, 9, 10)
In addition to health utility, differences in health preference may reflect differences in the interpretation of patient-reported outcomes (PROs). The Patient-Reported Outcomes Measurement Information System® (PROMIS®) includes publicly available health-related quality of life (HRQoL) measures, such as the PROMIS-29.(11) The PROMIS initiative is a network of NIH-funded research sites working to develop tools to measure health outcomes.(12) Through a process known as item banking, PROMIS has established a catalog of psychometric evidence on publicly available PRO items that measure key HRQoL domains. The PROMIS-29 is an adult profile instrument available in English and Spanish that measures 7 domains of HRQoL over the last 7 days with four 5-level (i.e., response categories) items per domain, as well as an eighth domain (pain intensity) with a single 11-level item.(13) For each domain, the 4 items were selected based on feedback from content experts and using item response theory to select the relatively more informative items.(14–16)
The aim of the PROMIS Valuation Study is to value such PROs from the perspective of adult members of the U.S. general population and cancer survivors.(17) Using data from discrete choice experiments (DCEs) in the PROMIS Valuation Study,(18) we examined differences in health preferences (i.e., values) by prominent demographic groups (gender, age, ethnicity, and race) in the United States. This study applies quotas on each paired comparison, thereby controlling for differential response by demographic characteristics. Key to the analyses is the extent to which different sub-groups (e.g., males versus females) are willing to trade off years of life to avoid decreases in functioning (physical or social) or increases in symptom burden (anxiety, depression, fatigue, sleep disturbance, and pain).
METHODS
Theory Underlying Quality-Adjusted Life Year (QALY) and Choice
For the purposes of this study, values (V) are expressed on a QALY scale, where a year with no health problems is 1 QALY. For example, a value of 10 QALYs would be associated with 10 years with no health problems, and a value of 0 QALYS is associated with being dead for 10 years. While sometimes used interchangeably, value and utility are different concepts. For this paper, we define value as a preference-based measure representing the choices of a group or subgroup of individuals (e.g., females), and utility as an unobserved (latent) individual trait that governs a person’s choice (i.e., episodic random utility model).(19–21) The 2 concepts are linked because value is inferred from the choices of multiple individuals. Specifically, a paired-comparison task may ask a respondent which health episodes he/she prefers: A or B? By definition, the episodes A and B have the same value (VA=VB) if and only if exactly half of the respondents choose A instead of B. For example, in the PROMIS-29 Valuation Study, some respondents were asked to choose between 10 years feeling “sometimes worthless, helpless, depressed, and hopeless” and a range of years with “no health problems” followed by death (see Figure 1). The “50/50 mark” was approximately 7.4 years (i.e., V [sometimes worthless, helpless, depressed and hopeless, 10 years] = 7.4 QALYs). When fewer or more respondents choose A instead of B, this imbalance implies the extent of difference in value, VA-VB.
Figure 1.
Example of a paired comparison: sometimes feeling worthless, helpless, depressed and hopeless for 10 years vs. reduced lifespan with no health problems
This study was designed to compare the values of 8 subgroups of respondents: gender (male; females), age (18–54 years; 55 years or older), Hispanic ethnicity (Hispanic; non-Hispanic), and race (non-Hispanic Black; non-Hispanic White). We hypothesize that subgroups of respondents may disagree on the value of a health episode (i.e., the location of the 50/50 mark). Such differences can be assessed based on choice probabilities or based on the results of a multi-attribute utility (MAU) regression. The MAU results have the advantage of integrating across choice probabilities to describe decrements in value attributable to losses in HRQoL. Each decrement, dh, is a downward shift on a QALY scale, which implies a decrease in the likelihood of choosing a particular health episode.
Health Outcomes
In the paired comparisons, 7 HRQoL domains (Physical Functioning, Anxiety, Depression, Fatigue, Sleep Disturbance, Social Functioning, and Pain) were described using the PROMIS-29 v1.0.(22) The pain domain has 2 subdomains (interference and intensity). The first 6 domains and pain interference have four 5-category items each (i.e., 16 decrements each). Pain intensity is assessed using a single 11-point numeric rating scale anchored between no pain (0) and worse imaginable pain (10). Each loss in HRQoL (e.g., rarely depressed) was expressed as lasting 10 years followed by death and parameterized using 122 decrements in value on a QALY scale (i.e., (7x16)+10 for pain). The duration of 10 years is conventionally used in time trade-off tasks as a compromise between avoiding proximal mortality (i.e., not too soon) and promoting realism for older respondents whose life expectancy may not exceed 10 years.(23)
Survey
The PROMIS Valuation Study recruited U.S. respondents from 7 panel vendors, with each vendor recruiting 1000 participants who completed the survey. To be eligible for the study, respondents had to be 18 years or older and reside in the U.S. Each panel vendor sent its members an e-mail invitation containing payment information and a member-specific hyperlink that, once activated, opened the study’s informed consent page. After providing informed consent, respondents completed the screener, self-reported health, DCE, and follow-up components of the survey. The DCE component consisted of 30 paired comparisons. An introduction to DCE demonstrated the concept of a paired comparison and began with a choice between an apple and an orange. The next 2 examples illustrated the range of difficulty in choosing between health scenarios with the understanding that the respondent “must live in 1 of the 2 scenarios” (i.e., forced choice). First, respondents were asked"which health scenario do you prefer? Good health for 10 years or poor health for 10 years,” followed by a second, more ambiguous example (bad vs. poor health) that introduced the potential ambiguity of scenario descriptions.
Aside from the trade-off between HRQoL attributes, the 2 scenarios in a pair had a set of attributes in common (i.e., pivot). This pivot was modified by 2 differences in attributes (i.e., bipedal partial profile).(24) For example, which do you prefer: 10 years in fair health (pivot) with mild pain and no depression versus mild depression and no pain (biped)? For the first 6 pairs, the task directed respondents to choose between scenarios with either reduced lifespan or 1 of 6 “health problems” for 10 years, including 3 levels of a depression symptom (rarely; sometimes; or often feeling worthless, helpless, depressed, and hopeless) and 3 levels of mild pain (1, 2, or 3 on a pain scale from 0 [no pain] to 10 [worst pain imaginable]). For the remaining 24 pairs, the pivot was 10 years in Good, Fair, and Poor health with 2 compensating health problems (biped) followed by death (8 bipedal pairs with each pivot).
Each respondent in a panel was randomly assigned 1 of 1000 unique sequences of 30 pairs based on his/her demographic characteristics (reported in survey and verified by vendor) to guarantee that each pair-specific sample corresponds to demographic quotas. Each pair choosing between reduced lifespan and health problem had between 571 and 772 responses and each pair choosing between 2 health problems had between 359 and 398 responses. All study procedures were approved by the University of South Florida Institutional Review Board (IRB # Pro00000076) and are described in greater detail in a report posted online.(9)
Statistical Analysis
For each of the 8 subgroups, demographic weights based on the 2010 U.S. Census were applied to each paired-comparison response to calculate the subgroups’ 540 pair-specific probabilities, p1…p540. Each probability was approximately normally distributed with standard error, ó = sqrt(p × (1–p) /n).(25, 26) To estimate the 122 decrements in the MAU regression for each subgroup, dh, we minimized the sum of squared error surrounding the 540 subgroups’ probabilities, , where P(.) was a cumulative density function, dB/(dA+dB), and α was a scaling term that adjusts the proportional relationship between P(.), and pk for 2 behavioral issues: satisficing (answering questions without regard to content) (9, 27) and non-trading (i.e., price inelastic demand; consistently choosing either reduced lifespan to avoid poor health or choosing poor health to avoid any loss in lifespan).(17, 28) To assess the differences between subgroup values, p-values were estimated by percentile bootstrap with pair-quota stratification and 1000 resampling iterations. For purposes of presentation, we reported the sign of significant differences with a p-value of 0.01 or less; however, the subgroup estimates and p-values are provided in the Supplemental Digital Content 1.
RESULTS
Between March and July 2012, we recruited 29,031 respondents across the United States. Among the 29% who met the survey requirements, 90% completed the survey with a median duration of 20 minutes (interquartile range 16 to 28 minutes). Table 1 compares the respondent characteristics to the 2010 U.S. Census, which was largely comparable due to study design and due to quota sampling at the pair level.
Table 1.
Respondent Characteristics*
| N=7557 | Study % (#) |
US 2010 Census % |
|---|---|---|
| Age in years | ||
| 18 to 34 | 28 (2125) | 31 |
| 35 to 54 | 36 (2711) | 37 |
| 55 and older | 36 (2721) | 33 |
| Sex | ||
| Male | 48 (3657) | 49 |
| Female | 52 (3900) | 51 |
| Race | ||
| White | 84 (6195) | 75 |
| Black or African American | 12 (887) | 12 |
| American Indian or Alaska Native | 1 (53) | 1 |
| Asian | 2 (165) | 5 |
| Native Hawaiian or other Pacific Islander | <1 (34) | <1 |
| Some other race | - | 5 |
| Two or more races | 3 (223) | 2 |
| Hispanic ethnicity | ||
| Hispanic or Latino | 13 (972) | 14 |
| Not Hispanic or Latino | 87 (6585) | 86 |
Demographic quota sampling was applied to each paired comparison to assure nationally representative estimates for each pair.
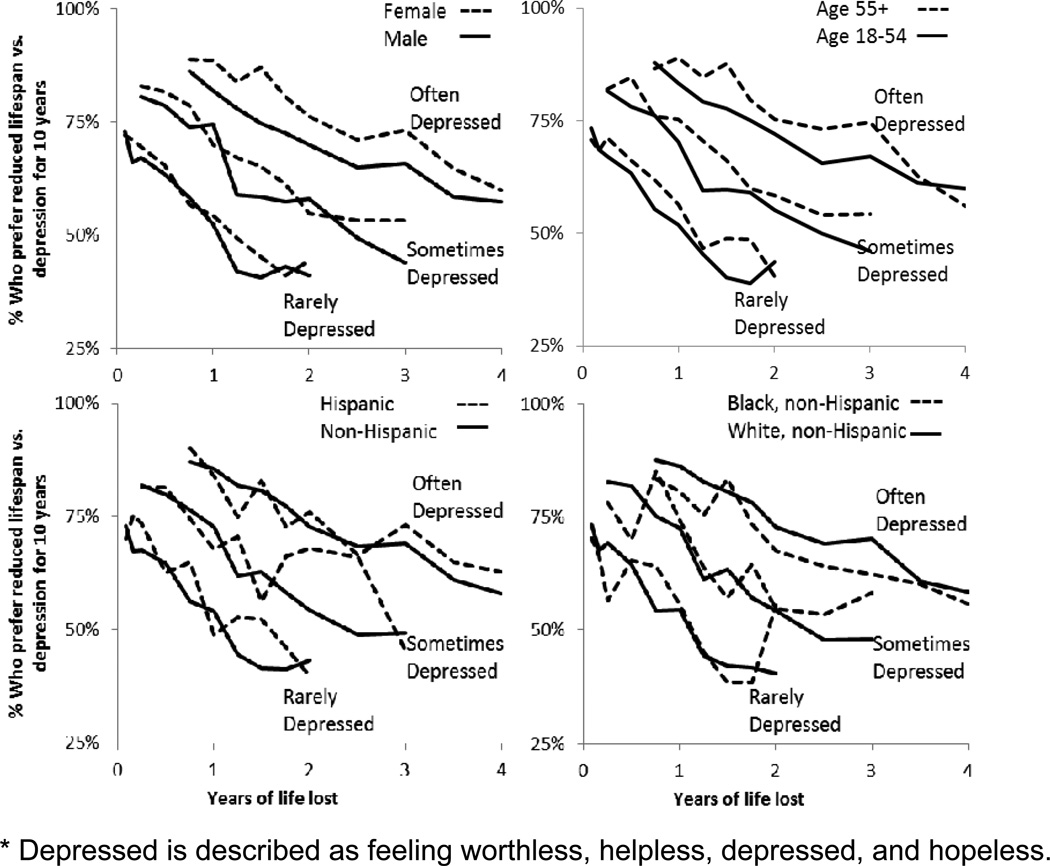
For each of the 8 subgroups, 30 probabilities were estimated and illustrated as trends in choice between reduced lifespan and levels of depression (Figure 2). As expected, reducing lifespan (i.e., years of life lost ranging from 0 to 4 years) decreased the percentage of respondents who preferred reduced lifespan over depression. Also, increasing frequency of depression increased the percentage of respondents who preferred reduced lifespan over depression.
Figure 2.
Percentage of respondents who prefer reduced lifespan vs. depression for 10 years by gender, age, ethnicity, and race
The gap between the trend lines by gender, age, ethnicity, and race are summarized in Table 2, which shows that women preferred reduced lifespan over depression compared to men. Adults age 55 or older preferred reduced lifespan over depression compared to younger adults, and Hispanics preferred reduced lifespan over depression compared to non-Hispanics. No differences in pain preferences were identified by gender or age; however, Hispanic and Black adults preferred reduced lifespan over low levels of pain relative to non-Hispanic and White respondents, respectively.
Table 2.
Differences in the percentage of respondents who prefer reduced lifespan over levels of depression or pain
| Female vs. Male |
Age 55+ vs. 18 to 54 |
Hispanic vs. Non-Hispanic |
Black vs. White* |
|||||
|---|---|---|---|---|---|---|---|---|
| Health Problem | % | p-value | % | p-value | % | p-value | % | p-value |
| Feeling worthless, helpless, depressed and hopeless | ||||||||
| Often | 5.9 | <0.001 | 4.0 | <0.001 | 1.9 | 0.204 | −3.7 | 0.018 |
| Sometimes | 3.1 | 0.005 | 4.6 | <0.001 | 3.3 | 0.047 | 1.5 | 0.383 |
| Rarely | 2.1 | 0.062 | 3.4 | 0.004 | 3.8 | 0.027 | −0.2 | 0.916 |
| Pain intensity scale from 0 (no pain) to 10 (worst pain imaginable) | ||||||||
| Pain Intensity 3 | −1.5 | 0.160 | −1.0 | 0.357 | 5.1 | 0.001 | 8.6 | <0.001 |
| Pain Intensity 2 | −0.2 | 0.844 | −0.1 | 0.886 | 5.2 | 0.001 | 11.8 | <0.001 |
| Pain Intensity 1 | −0.6 | 0.518 | 1.1 | 0.304 | 6.4 | <0.001 | 11.2 | <0.001 |
Black and White subgroups exclude Hispanic adults and adult of other or mixed race.
Table 3 describes significant demographic differences in value for the 122 losses in HRQoL captured by the PROMIS-29. Women placed a higher value on 54 of the 122 losses in HRQoL than men; however, these differences largely occurred at the extreme levels. Men did not value any loss more than women (i.e., no minus signs in the columns comparing values by gender). Older adults placed a higher value on anxiety, depression, and fatigue than younger adults; however, younger adults valued 4 losses more than older adults (1 physical function, 1 social functioning, and 2 pain interference). Hispanics placed a higher value on depression and sleep disturbance than non-Hispanics. Among non-Hispanics, Blacks placed a higher value on reduced lifespan over losses in ability to climb stairs and to fall asleep compared to Whites, but held similar values on mental health outcomes. Overall, the results showed few significant differences in the value of social function and pain interference, except between men and women at extreme social functioning and when pain interferes with enjoyment of life. Differences in the value of pain intensity were not significant (not shown in Table 3; see Supplemental Digital Content 1), except that women valued levels 8, 9, and 10 (representing severe pain) more than men, and Blacks valued levels 1, 2, and 3 more than Whites.
Table 3.
Significant differences in the value of HRQoL by domain
| Females vs. Males† |
Age 55+ vs. 18–54 |
Hispanic vs. Non- Hispanic |
Black vs. White |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level of HRQOL* | 2 | 3 | 4 | 5 | 2 | 3 | 4 | 5 | 2 | 3 | 4 | 5 | 2 | 3 | 4 | 5 |
| Physical Functioning | + | + | + | + | + | |||||||||||
| Chores | + | + | + | − | ||||||||||||
| Stairs | + | + | + | + | + | + | ||||||||||
| Walk | + | + | + | + | ||||||||||||
| Errands | + | + | + | + | + | |||||||||||
| Anxiety | + | + | + | + | + | + | + | |||||||||
| Fearful | + | + | + | + | + | + | + | |||||||||
| Focus | + | + | + | + | + | + | ||||||||||
| Worries | + | + | + | + | + | + | + | |||||||||
| Uneasy | + | + | + | + | + | |||||||||||
| Depression | + | + | + | + | + | + | + | + | + | + | ||||||
| Worthless | + | + | + | + | ||||||||||||
| Helpless | + | + | + | + | + | + | ||||||||||
| Depressed | + | + | + | + | + | + | + | + | + | |||||||
| Hopeless | + | + | + | + | + | |||||||||||
| Fatigue | + | + | + | + | + | + | + | + | ||||||||
| Fatigued | + | + | ||||||||||||||
| Starting | + | + | + | + | + | + | ||||||||||
| Run-Down | + | + | + | + | + | + | + | + | ||||||||
| Fatigue Ave | + | + | + | |||||||||||||
| Sleep Disturbance | + | + | + | + | + | + | + | + | + | |||||||
| Quality | + | + | + | − | ||||||||||||
| Refreshing | + | + | + | + | ||||||||||||
| Problem | + | + | + | + | + | + | ||||||||||
| Difficulty | + | + | + | + | + | |||||||||||
| Social Functioning | + | + | ||||||||||||||
| Amount | + | − | ||||||||||||||
| Work | + | + | ||||||||||||||
| Personal | + | |||||||||||||||
| Routine | + | |||||||||||||||
| Pain Interference‡ | ||||||||||||||||
| Day to day | ||||||||||||||||
| Home | ||||||||||||||||
| Social Activities | ||||||||||||||||
| Enjoyment | + | + | − | − | ||||||||||||
HRQoL decreases from level 1 to level 5. Black and White subgroups exclude Hispanic adults and adult of other or mixed race. Significance is defined by the difference in value between groups at a p-value less the 0.01. All attribute descriptions, values and p-values are reported in the Appendix.
For example, the plus signs (+) suggest that women value physical functioning more than men, particularly walking and errands. Minus signs (−) would signify the contrary.
Differences in the value of pain intensity were not significant (not shown; see Appendix), except that women value levels 8, 9 and 10 more than men and Black adults value levels 1, 2 and 3 more than White adults.
DISCUSSION
This paper examines the differences in health preferences by gender, age, ethnicity, and race using a preference-based measure of 7 HRQoL domains. The results suggest that women place a higher value on HRQoL than men, particularly on severe reductions. Likewise, adults aged 55 and older value mental health more than younger adults. Few differences were found by ethnicity and race, except for sleep disturbance and mild pain. The differences by gender and age may be explained by differences in the value of lifespan or shifts caused by health experiences that may favor HRQoL over longevity.
There are pros and cons to proposing an aggregate (or overall population-based) value set versus a subgroup value set whose source preferences are aggregated on the basis of age, race, or gender group, and their potential applications should first be carefully considered. As Dolan stated, there are 3 questions we ask when calculating the “quality adjustment” part of the QALY: What is to be valued? How is it to be valued? Who is to value it?(29) The allocation of healthcare resources in government-funded healthcare systems typically uses the preferences of the general population as the source of (societal) preferences to avoid individual or subgroup self-interest. Further, if subgroup-based value sets were adopted for resource allocation, the possibility of a “QALY trap” arises, which is biased against the adoption of health technology in patient/respondents who systematically value health outcomes higher.(30) Our present study identified a proportion of health-state pairs with differences based on gender (49 of 122 pairs), older respondents compared to younger,(20) and, to a much lesser extent, race/ethnicity. In contrast with our current study, previous health valuation studies have found that race has an impact;(3) age also contributes to different valuations,(3, 31) and presence of disease has produced inconsistent results.(32–34) However, the use of subgroup-based value sets could inform treatment guidelines for other purposes, such as understanding which health outcomes are more desirable to women than men, which could then be extrapolated to personalized medicine. The threshold at which to deem differences as meaningful enough to necessitate subgroup-based stratification remains unclear.
Aside from differences in preferences, a wide range of literature reports that depressive symptoms are more accessible and more often expressed by women than men when they do occur.(35) This suggests that moderate depression among women is similar to a lower level of depression among men. In other words, a woman’s moderate level of depression is less detrimental than a man’s moderate level. However, this study finds that women preferred reduced lifespan over more severe levels of depression more than did men, which may contribute to their greater motivation to express depression.
Research has demonstrated ethnic differences in reporting pain and in pain perceptions.(4, 5, 19, 35–39) The finding that Hispanics value mild levels of pain more than non-Hispanics is consistent with previous research.(40–42) For example, Bates et al. (1993) found that Hispanics report greater pain intensity as well as affective and sensory aspects of pain than non-Hispanics. Rahim-Williams et al. (2007) found that Hispanics and non-Hispanic African Americans reported greater pain sensitivity than non-Hispanic Whites on 3 experimental tests. In addition, there is some evidence supporting variations in pain intensity assessment among race/ethnic subgroups.(40) Greater extreme response tendency has been observed for Hispanics enrolled in Medicaid managed-care than Whites enrolled in commercial managed-care on 0–10 global ratings of pain intensity.(43)
The PROMIS-29 profile questionnaire served as the basis for the DCEs. The PROMIS-29 selects 7 common outcome domains from a larger array of outcome domains to efficiently represent the multidimensional concept of HRQoL. These domains (pain, fatigue, sleep, depression, anxiety, physical function, and social function) do not include areas such as cognitive function, anger, or other symptoms that might, for some people, also drive the way health is valued and may be included in future research.
Limitations
Although this study provides important information on group-specific differences in health preference ratings, some limitations are noted. First, even though the forced choice method is widely applied in research, a limitation is that no qualitative study of these paired comparisons was conducted. Second, the survey was conducted with people who can read English. Generalizability to people with low literacy or to those who read and speak other languages is not certain. This may limit generalizability to the Hispanics in the U.S. who can read English and may, therefore, be more acculturated to U.S. society than their non-English-speaking counterparts. Third, this study was conducted with a web-based survey, thus those underserved populations without access are not represented. Although great care was taken to validate respondent identities and apply demographic quota sampling at the pair level to address potential biases in gender, age, and race/ethnicity groups, it should be noted that the respondents for this study are experienced survey takers, thus, their responses may not accurately reflect those of the general U.S. due to unobservable factors. Future research may also examine the interaction of these demographic groups (e.g., older vs. younger Hispanic respondents) and the effects of health on health preferences.
Conclusions
This is the first valuation study conducted in the U.S. on the PROMIS measures. The PROMIS initiative represents a significant investment by the NIH to standardize the measurement of HRQoL to enhance healthcare research in the U.S. and globally. The PROMIS measures are being used in clinical trials, comparative effectiveness research studies, and population surveillance initiatives. As the PROMIS enables researchers to have more reliable and valid HRQoL measures, to inform decision making and public policy, this study serves a critical need to understand how different demographic populations of the U.S. value such domains as physical and social function and symptoms including depression, anxiety, sleep disturbance, and pain. This valuation study is a first step towards a broader understanding of the valuing of health domains from a societal perspective. Follow-up studies will compare U.S. general population values to cancer survivors. Recognizing these differences allows decision makers to consider how health policies or interventions may differentially impact the populations they serve.
Supplementary Material
Supplemental Digital Content 1. Tables that illustrate the value of physical functioning, anxiety, depression, fatigue, sleep, social functioning, and pain interference by respondent characteristics (supplemental_digital_content_1.pdf)
Acknowledgements
Financial support for this study was provided in part by an NCI R01 grant (1R01CA160104). Ron D. Hays was supported in part by grants from the NIA (P30-AG021684) and the NIMHD (P20MD000182). The funding agreement(s) ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
The authors thank Carol Templeton, Michelle Owens, and Shannon Hendrix-Buxton at Lee H. Moffitt Cancer Center & Research Institute for their contributions to the research and creation of this paper. We also greatly appreciate the external review comments from Dennis Fryback and David Feeny on the study methodology. The opinions expressed in this paper do not represent those of these reviewers.
Contributor Information
Benjamin M. Craig, Health Outcomes and Behavior, Moffitt Cancer Center and University of South Florida.
Bryce B. Reeve, Health Policy and Management, University of North Carolina at Chapel Hill, 1101 E McGavran-Greenberg Hall, Campus Box 7411, Chapel Hill, NC 27599-7411 Phone: 919-843-8793; Fax: 919-843-6362; bbreeve@email.unc.edu.
David Cella, Medical Social Sciences, Northwestern University, 710 North Lake Shore Drive, Suite 729, Chicago, IL 60611-3435 Phone: 312-503-1086; Fax: 312-503-9800; d-cella@northwestern.edu.
Ron D. Hays, Health Services, University of California, Los Angeles and RAND, Santa Monica, CA, 911 Broxton Avenue, Los Angeles, CA 90024-1736 and RAND, Santa Monica, CA Phone: 310-794-2294; Fax: 310-794-0732; drhays@ucla.edu.
A. Simon Pickard, Pharmacy Practice, University of Illinois at Chicago, 833 South Wood Street, Chicago, IL 60612-7230 Phone: 312-413-3357; Fax: 312-996-0379; pickard1@uic.edu.
Dennis A. Revicki, United BioSource Corporation, 5656 Eastwind Drive, Sarasota, FL 34233 dennis.revicki@unitedbiosource.com.
REFERENCES
- 1.Tocqueville Ad. Democracy in America / by Alexis de Tocqueville. London: Saunders and Otley; 1835. ([London] : R. Taylor); 1835. [Google Scholar]
- 2.Zarate V, Kind P, Chuang LH. Hispanic Valuation of the EQ-5D Health States: A Social Value Set for Latin Americans. Value in Health. 2008;11:1170–1177. doi: 10.1111/j.1524-4733.2008.00349.x. [DOI] [PubMed] [Google Scholar]
- 3.Shaw JW, Johnson JA, Chen S, et al. Racial/ethnic differences in preferences for the EQ-5D health states: results from the US valuation study. Journal of Clinical Epidemiology. 2007;60:479–490. doi: 10.1016/j.jclinepi.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Cykert S, Joines JD, Kissling G, et al. Racial differences in patients' perceptions of debilitated health states. Journal of General Internal Medicine. 1999;14:217–222. doi: 10.1046/j.1525-1497.1999.00320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo N, Wang QN, Feeny D, et al. Measuring health preferences for Health Utilities Index Mark 3 health states: A study of feasibility and preference differences among ethnic groups in Singapore. Medical Decision Making. 2007;27:61–70. doi: 10.1177/0272989X06297103. [DOI] [PubMed] [Google Scholar]
- 6.Burgess DJ, Gravely AA, Nelson DB, et al. A National Study of Racial Differences in Pain Screening Rates in the VA Health Care System. Clinical Journal of Pain. 2013;29:118–123. doi: 10.1097/AJP.0b013e31826a86ae. [DOI] [PubMed] [Google Scholar]
- 7.Llewellynthomas HA, Sutherland HJ, Thiel EC. Do Patients' Evaluations of a Future Health State Change When They Actually Enter That State? Medical Care. 1993;31:1002–1012. doi: 10.1097/00005650-199311000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Stiggelbout AM, Kiebert GM, Kievit J, et al. Utility Assessment in Cancer Patients: Adjustment of Time Tradeoff Scores for the Utility of Life Years and 17 Comparison with Standard Gamble Scores. Medical Decision Making. 1994;14:82–90. doi: 10.1177/0272989X9401400110. [DOI] [PubMed] [Google Scholar]
- 9.Craig B, Reeve BB. Methods Report on the PROMIS Valuation Study: Year 1. [Accessed October 11, 2012];2012 Available at: http://labpages.moffitt.org/craigb/Publications/Report120928.pdf. [Google Scholar]
- 10.Hadorn DC, Uebersax J. Large-Scale Health Outcomes Evaluation- How Should Quality-Of-Life be Measured.1. Calibration of a Brief Questionnaire and a Search for Preference Subgroups. Journal of Clinical Epidemiology. 1995;48:607–618. doi: 10.1016/0895-4356(94)00185-s. [DOI] [PubMed] [Google Scholar]
- 11.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult selfreported health outcome item banks: 2005-2008. Journal of Clinical Epidemiology. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NIH. PROMIS: Dynamic Tools to Measure Health Outcomes from the Patient Perspective. 2011 Available at: http://www.nihpromis.org/ [Google Scholar]
- 13.Revicki DA, Kawata AK, Harnam N, et al. Predicting EuroQol (EQ-5D) scores from the patient-reported outcomes measurement information system (PROMIS) global items and domain item banks in a United States sample. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2009;18:783–791. doi: 10.1007/s11136-009-9489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reeve BB, Hays RD, Bjorner JB, et al. Psychometric evaluation and calibration of health-related quality of life item banks - Plans for the patient-reported outcomes measurement information system (PROMIS) Medical Care. 2007;45:S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- 15.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) Progress of an NIH roadmap cooperative group during its first two years. Medical Care. 2007;45:S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeWalt DA, Rothrock N, Yount S, et al. Evaluation of item candidates - The PROMIS qualitative item review. Medical Care. 2007;45:S12–S21. doi: 10.1097/01.mlr.0000254567.79743.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craig BM, Busschbach JJV. Revisiting United States valuation of EQ-5D states. J Health Econ. 2011;30:1057–1063. doi: 10.1016/j.jhealeco.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Craig BM, Reeve BB, Brown PM, et al. Valuation of Health Outcomes Measured Using the PROMIS-29. J Health Econ [Under Review] doi: 10.1016/j.jval.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bansback N, Brazier J, Tsuchiya A, et al. Using a discrete choice experiment to estimate health state utility values. J Health Econ. 2012;31:306–318. doi: 10.1016/j.jhealeco.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Craig BM, Busschbach JJ. The episodic random utility model unifies time trade-off and discrete choice approaches in health state valuation. Popul Health Metr. 2009;7:3. doi: 10.1186/1478-7954-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hadorn DC, Hays RD, Uebersax J, et al. Improving task comprehension in the measurement of health state preferences - a trial of informational cartoon figures and a paired-comparison task. Journal of Clinical Epidemiology. 1992;45:233–243. doi: 10.1016/0895-4356(92)90083-y. [DOI] [PubMed] [Google Scholar]
- 22.PROMIS-29 Profile v1.0. [Accessed June 06, 2012];2008-2012 Available at: https://www.assessmentcenter.net/ac1//files/pdf/44b7636201a34267a9213db7f69f2c6d.pdf. [Google Scholar]
- 23.Feeny D. Standardization and regulatory guidelines may inhibit science and reduce the usefulness of analyses based on the application of preference-based measures for policy decisions. Medical decision making : an international journal of the Society for Medical Decision Making. 2013;33:316–319. doi: 10.1177/0272989X12468793. [DOI] [PubMed] [Google Scholar]
- 24.Chrzan K. Using partial profile choice experiments to handle large numbers of attributes. International Journal of Market Research. 2010;52:827–840. [Google Scholar]
- 25.Urban FM. The Application of Statistical Methods to the Problems of Psychophysics. Philadelphia: Psychological Clinic Press; 1908. [Google Scholar]
- 26.Urban FM. Urban's Solution (Minimum Normit X2) In: Bock RD, Jones LV, editors. The Measurement and Prediction of Judgment and Choice. San Francisco: Holden-Day; 1968. pp. 33–49. [Google Scholar]
- 27.Barge S, Gehlbach H. Using the Theory of Satisficing to Evaluate the Quality of Survey Data. Res High Educ. 2012;53:182–200. [Google Scholar]
- 28.Attema AE, Versteegh MM, Oppe M, et al. Lead Time to TTO: Leading to Better Health State Evaluations? Health Economics. 2013;22:376–392. doi: 10.1002/hec.2804. [DOI] [PubMed] [Google Scholar]
- 29.Dolan P. Thinking About it: Thoughts About Health and Valuing QALYs. Health Economics. 2011;20:1407–1416. doi: 10.1002/hec.1679. [DOI] [PubMed] [Google Scholar]
- 30.Ubel PA, Richardson J, Menzel P. Societal value, the person trade-off, and the dilemma of whose values to measure for cost-effectiveness analysis. Health Economics. 2000;9:127–136. doi: 10.1002/(sici)1099-1050(200003)9:2<127::aid-hec500>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 31.Dolan P. The effect of experience of illness on health state valuations. Journal of Clinical Epidemiology. 1996;49:551–564. doi: 10.1016/0895-4356(95)00532-3. [DOI] [PubMed] [Google Scholar]
- 32.Kind P, Dolan P. The Effect of Past and Present Illness Experience on the Valuations of Health States. Medical Care. 1995;33:AS255–AS263. [PubMed] [Google Scholar]
- 33.Krabbe PFM, Tromp N, Ruers TJM, et al. Are patients' judgments of health status really different from the general population? Health and Quality of Life Outcomes. 2011;9 doi: 10.1186/1477-7525-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pickard AS, Tawk R, Shaw JW. The effect of chronic conditions on stated preferences for health. European Journal of Health Economics. 2013;14:697–702. doi: 10.1007/s10198-012-0421-8. [DOI] [PubMed] [Google Scholar]
- 35.Van de Velde S, Bracke P, Levecque K. Gender differences in depression in European countries. Cross-national variation in the gender gap in depression. Social Science & Medicine. 2010;71:305–313. doi: 10.1016/j.socscimed.2010.03.035. [DOI] [PubMed] [Google Scholar]
- 36.Ayalon L, King-Kallimanis BL. Trading Years for Perfect Health: Results From the Health and Retirement Study. Journal of Aging and Health. 2010;22:1184–1197. doi: 10.1177/0898264310371980. [DOI] [PubMed] [Google Scholar]
- 37.Hernandez A, Sachs-Ericsson N. Ethnic differences in pain reports and the moderating role of depression in a community sample of Hispanic and Caucasian participants with serious health problems. Psychosomatic Medicine. 2006;68:121–128. doi: 10.1097/01.psy.0000197673.29650.8e. [DOI] [PubMed] [Google Scholar]
- 38.Mulvaney-Day NE, Horvitz-Lennon M, Chen CN, et al. Valuing health in a racially and ethnically diverse community sample: an analysis using the valuation metrics of money and time. Quality of Life Research. 2010;19:1529–1540. doi: 10.1007/s11136-010-9713-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van der Pol M, Cairns J. Comparison of two methods of eliciting time preference for future health states. Social Science & Medicine. 2008;67:883–889. doi: 10.1016/j.socscimed.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 40.Bates MS, Edwards WT, Anderson KO. Ethnocultural influences on variation in chronic pain perception. Pain. 1993;52:101–112. doi: 10.1016/0304-3959(93)90120-E. [DOI] [PubMed] [Google Scholar]
- 41.Rahim-Williams FB, Riley JL, Herrera D, et al. Ethnic identity predicts experimental pain sensitivity in African Americans and Hispanics. Pain. 2007;129:177–184. doi: 10.1016/j.pain.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zinke JL, Lam CS, Harden RN, et al. Examining the Cross-cultural Validity of the English Short-form McGill Pain Questionnaire Using the Matched Moderated Regression Methodology. Clinical Journal of Pain. 2010;26:153–162. doi: 10.1097/AJP.0b013e3181b99f56. [DOI] [PubMed] [Google Scholar]
- 43.Weech-Maldonado R, Elliott MN, Oluwole A, et al. Survey response style and differential use of CAHPS rating scales by Hispanics. Medical Care. 2008;46:963–968. doi: 10.1097/MLR.0b013e3181791924. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Tables that illustrate the value of physical functioning, anxiety, depression, fatigue, sleep, social functioning, and pain interference by respondent characteristics (supplemental_digital_content_1.pdf)