Abstract
Objective
To examine associations between racial/ethnic concordance and BP control, and determine if patient trust and medication adherence mediate these associations.
Design
Cross-sectional study of 723 hypertensive African American and White patients receiving care from 205 White and African American providers at 119 primary care clinics, from 2001–2005. Racial/ethnic concordance was characterized as dyads where both the patient and physician were of the same race/ethnicity; discordance occurred in dyads where the patient was African American and the physician was White. Patient perceptions of trust and medication adherence were assessed with self-report measures. Blood pressure readings were abstracted from patients’ medical charts using standardized procedures.
Results
Six hundred thirty seven patients were in race/ethnic-concordant relationships; 86 were in race/ethnic-discordant relationships. Concordance had no association with blood pressure control. White patients in race/ethnic-concordant relationships were more likely to report better adherence than African American patients in race/ethnic-discordant relationships (OR: 1.27 95% CI: 1.01, 1.61 p = 0.04). Little difference in adherence was found for African American patients in race/ethnic-concordant vs. discordant relationships. Increasing trust was associated with significantly better adherence (OR: 1.17 95% CI: 1.04, 1.31, p < 0.01) and a trend toward better BP control among all patients (OR: 1.26, 95% CI: 0.97, 1.63, p=0.07).
Conclusions
Patient trust may influence medication adherence and BP control regardless of patient-physician racial/ethnic composition.
Keywords: blood pressure control, trust, medication adherence, racial/ethnic concordance
Introduction
In the last decade there has been a major global shift in the leading causes of death from infectious diseases to non-communicable diseases. The prevalence of cardiovascular diseases (CVD) in particular is growing exponentially, due in part to the rapidly increasing rates of hypertension (HTN) in many countries (World Health Organization [WHO], 2013). In 2008, CVD accounted for 17 million deaths a year worldwide; HTN accounted for over half (9.4 million) of the reported deaths (WHO, 2013). Low and middle income countries carry a disproportionate burden of HTN where weak health care systems result in a higher proportion of patients with undiagnosed, untreated and uncontrolled HTN. In the United States, uncontrolled HTN accounts for the greatest proportion of racial/ethnic disparities in premature CVD morbidity and mortality between African Americans and Whites (Ong et al., 2007; Roger et al., 2011). As such, improving blood pressure (BP) control in patients with HTN is of paramount importance if we are to address the increasing global burden of CVD mortality.
The quality of the patient-physician relationship can play a pivotal role in the detection and management of HTN, particularly for underserved populations. A growing body of literature has documented the beneficial effects of collaborative patient-physician relationships on patient outcomes (Stewart et al., 1995; 2000). More importantly, the importance of qualities such as patient-centeredness and shared decision-making have been demonstrated in the United States as well as in international contexts (Osborn and Squires, 2012). In our previous work (blinded for peer review), we demonstrated that collaborative patient-physician relationships play an influential role on African American patients’ adherence to their antihypertensive medications when receiving care from White providers. Extending these findings to HTN control will provide much needed data on the reasons for the disproportionate rates of premature CVD-related mortality among African Americans.
Recently, several researchers have called attention to the need to elucidate the circumstances under which African American patients are more likely to experience negative outcomes when receiving care from White physicians (racial/ethnic discordance) (Meghani et al. 2009, Martin and Cooper 2013). Lower levels of trust in the physician, as reported by some African American patients, may be one such factor (Doescher et al. 2000). Trust is based on physician qualities of integrity (e.g., honesty), technical and interpersonal competence, and the ability to uphold patient fidelity (e.g., respect) and confidentiality in the interaction (Hall et al. 2001, 2002). Studies have shown trust to be a significant and direct predictor of patients’ adherence to treatment recommendations, above their satisfaction with the medical visit (Golin et al. 2002; Roberts 2002). African American patients in race/ethnic-discordant relationships are more likely to report lower trust in their physician as compared to race/ethnic-concordant relationships (Cooper et al. 2003). Thus, if African American patients in race/ethnic-discordant relationships feel they are unable to trust their physicians, they may be more likely to discontinue their medication use, resulting in poorer BP control. To our knowledge, the relationships among these factors have not been tested.
This study was designed to examine the associations between patient-physician racial/ethnic concordance and BP control. We also looked at the effects of patient trust and medication adherence on these associations (Figure 1). We hypothesized that a higher proportion of patients in race/ethnic-discordant relationships would exhibit poorer BP control than patients in race/ethnic-concordant relationships. Moreover, we hypothesized that lower levels of patient trust and poor medication adherence would mediate the relationship between race/ethnic-discordance and poor BP control.
Figure 1.
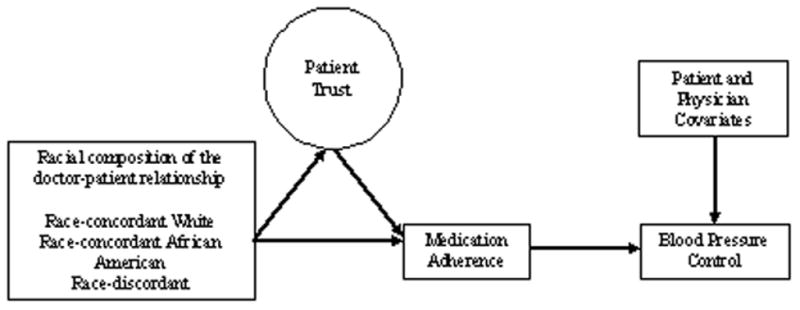
Model Examining Relationship between Patient-Physician Racial/Ethnic Concordance on BP Control, as Mediated by Patient Trust and Medication Adherence
Methods
Participants
This study analyzed cross-sectional survey data and medical record audit data from general internists and family physicians and their hypertensive patients who participated in the 2001–2005 Minimizing Error, Maximizing Outcome (MEMO) study. This longitudinal study was designed to explore the relationships between work conditions, physician outcomes, and quality of care. Details of the MEMO study are described elsewhere (Linzer et al. 2005). Briefly, MEMO investigators recruited physicians from 119 primary care clinics in five regions: inner city clinics in New York City and Chicago; academic and managed care clinics in Milwaukee and Madison, Wisconsin; and small town or rural clinics in central Wisconsin. Practices were included if at least 50% of physicians chose to participate. Up to 6 patients per participating physician were also recruited. Patients were contacted by mail from lists generated by ICD-9 codes when such codes were available, or by researchers in waiting rooms. Patient eligibility criteria for the MEMO study included age 18 or older; at least one of three clinical conditions (diabetes, hypertension, congestive heart failure); ability to read in English, Spanish, or Chinese; and at least two visits with their MEMO physician in the previous year. In addition to completing a self-administered survey, patients provided permission for an audit of their medical records covering an 18-month period of time. The institutional review board at each participating organization approved the research protocol; all participants provided written informed consent.
For this subset analysis, physicians were included if they self-identified as non-Hispanic African American or White. Patients were limited to those who: 1) self-identified as non-Hispanic African American or White; 2) received care from a non-Hispanic African American or White physician; 3) had a diagnosis of hypertension (ICD: 401–401.9); and 4) were taking at least one anti-hypertensive medication. For the purposes of this study, we defined the term ‘White’ to describe patients with European ancestral origins (Bhopal and Donaldson 1998). The term ‘African American’ describes patients with African ancestral origin (Agyemang, Bhopal, and Bruijnzeels 2005).
Study Measures
Patient-physician Relationships were grouped into 3 categories
a) race/ethnic-concordant White dyads wherein both the patient and physician self-identified as White; b) race/ethnic-concordant African American dyads wherein both the patient and physician self-identified as African American; and c) race/ethnic-discordant dyads where the patient was African American and the physician was White. Due to inadequate sample size, data from subjects in White patient-African American physician relationships were not included.
Blood Pressure (BP) Control
BP readings were collected by trained MEMO personnel as part of a medical record audit process that followed a standardized template based on national quality guidelines. The audit covered an 18-month period, from six months before the physician’s enrollment in MEMO to 12 months after enrollment. Patients were categorized as having adequate BP control if the chart audit revealed a systolic BP<140 and diastolic BP<90 mmHg for at least 50% of recorded readings for patients without comorbid disease, or systolic BP<130 and diastolic BP<80 mmHg for at least 50% of recorded readings for patients with chronic kidney disease and/or diabetes. These parameters followed criteria outlined in the Seventh Report of the Joint National Committee’s (JNC-7) (Chobanian et al. 2003).
Patient Trust
Patient trust was measured with a four-item instrument that assessed each dimension of Hall’s framework (Hall et al. 2001) of patient trust in the physician: trust in the physician’s competence, overall global trust, fidelity aspects of trust, and honesty (Kao et al. 1998). The four survey questions included: How much do you trust your physician’s judgment about your medical care?; How much do you trust your physician to put your health and well-being above all financial considerations?; How much do you trust your physician to make appropriate medical decisions regardless of health plan rules?; How much do you trust your physician overall? Possible responses ranged from 1=not at all to 5=completely. The measure demonstrated excellent composite reliability (0.923) and convergent validity (average variance extracted = 75.5%) in this study sample.
Medication Adherence
Patients were asked to respond to a single question on the survey: In a typical week, how close do you come to following your doctor’s recommendations about medications? Possible responses included: Always take all my medicines. Usually take all my medications (80% of the time). Sometimes take all my medications (less than 80% of the time). For this analysis, the responses were dichotomized as always take all my medicines vs. usually/sometimes take all my medicine. This measure was developed for the MEMO study and evaluated via field testing by the investigators in the original patient sample (Linzer et al. 2005).
Covariates
Physician data included sex, age, medical specialty, and clinic location (rural/inner city/suburban). Data on patient sex, age, number of anti-hypertensive medications, and number of comorbid conditions (e.g., diabetes, kidney disease) were collected. Data on patient education level (e.g., less than a high school (HS) degree, HS degree, some college and above) as a proxy for social class was also collected based on a substantial body of research showing that the influence of race/ethnicity and social class on outcomes are inherently intertwined within the patient-physician relationship (IOM 2003). Analyses were conducted to assess the suitability of our education variable as a proxy of social class using one clinic level variable (total percent of patients that are uninsured and/or have Medicaid) and one provider level variable (provider perceived access to clinical resources, such as supplies and equipment). Results showed that as the percent of uninsured/Medicaid patients increased, the level of patient education decreased (r=−0.34, SE=0.06). A decrease in physician perceived access to resources was also associated with a decrease in the level of patient education (r=0.18; SE=0.033).
Statistical Analyses
Patient and physician demographics were compared between groups using chi-square for categorical variables and independent z-tests for continuous variables. Multivariate logistic regression models, adjusting for the patient and physician covariates, were used to estimate the direct effects of racial/ethnic dyad composition on BP control. Using Mackinnon’s (2008) model of mediation analysis, a 2-level (patient-physician) structural probit regression model was constructed to assess the indirect (mediating) effect of patient trust and medication adherence on BP control (Figure 1). In these models, we controlled for patient (age, sex, educational level and number of anti-hypertensive medications), physician-level (age, sex, specialty, clinic location) variables. Since trust was a scaled variable, we did not want to disregard measurement error, which could result in biased parameter estimates and standard errors (Hayduk 1987). To compensate, we used an “errors in variables” approach that incorporated measurement error into our model using the composite indicator structure equation alpha method suggested by McDonald, et al.(2005) To interpret the findings, probit coefficients were converted to odds ratios (OR) with 95% confidence intervals (95% CI). Chi-square statistic, confirmatory factor index (CFI) and weighted root-mean-square-residual (WRMR) were used to assess the model fit (Hu and Bentler 1999). Goodness of fit of the overall model was assessed using a CFI>0.95 and WRMR <0.90 (Yu and Muthen 2001). For chi-square a non-significant p-value of p>0.05 was used.
Results
Physician and Patient Characteristics
The final sample was comprised of 205 physicians and 723 patients. Sixty-one percent of physicians were male with a mean age of 44.2 (standard deviation [SD]: 9.74) years. Physicians were evenly divided between family physicians and general internists (Table 1). African American physicians in race/ethnic-concordant relationships were significantly more likely to be female than were White physicians in race/ethnic-concordant relationships (66.6% vs. 35.6%, p<0.05). Overall, the physicians had been practicing at their current sites for 8.29 (SD: 7.3) years; White physicians in race/ethnic-concordant relationships, however, worked at their clinics twice as long as their African American colleagues in race/ethnic-concordant relationships. White physicians saw 661 of the 723 patients (91%).
Table 1.
Physician Characteristics by Patient-Physician Racial/Ethnic Concordance
| Physician Characteristic | All Physicians (n=205) | Race/ethnic- Concordant (White/White patient- physician dyad) (n=171) | Race/ethnic- Concordant (African American/ African American patient-physician dyad) (n=15) | Race/ethnic-Discordant (White physician/African American patient dyad) (n=19) |
|---|---|---|---|---|
| Number of patients in study | 723 | 575 | 62 | 86 |
| Mean age (SD) | 44.2 (9.74) | 44.8 (9.48) | 40.6 (9.22) | 41.8 (12.2) |
| Sex (female): % (n) | 39.0% (80/205) | 35.6% (61/171) | 66.6% (10/15)a | 47.3% (9/19) |
| Mean years at clinic (SD) | 8.29 (7.32) | 8.84 (7.68) | 4.33 (4.77)a | 6.47 (5.14) |
| Medical specialty (Family Medicine): % (n) | 53.6% (110/205) | 57.8% (99/171) | 40.0% (6/15) | 26.3% (5/19)b |
p <0.05 for the contrast between race/ethnic-concordant White and race/ethnic-concordant African American dyads
p <0.05 for the contrast between race/ethnic-concordant White and race/ethnic-discordant dyads
As illustrated in Table 2, most patients were male, had a mean age of 60.6 years, and reported at least some post-high school education. The mean BP was 141/79 mmHg, and 49% of the sample had adequate BP control according to chart audit data. Patients were prescribed a mean of 3.22 (SD 1.71) antihypertensive medications. On average, patients had three (SD 1.78) chronic comorbid conditions, with 51% having diabetes. Most patients (81%) reported always taking their medications as prescribed. The mean physician trust score was high at 4.59 (SD 0.61) on the scale of 1–5.
Table 2.
Patient Characteristics by Patient-Physician Racial/Ethnic Concordance
| Patient Characteristic | All Patients (n=723) | Race/Ethnic- Concordant (White/White patient-physician dyad) (n=575) | Race-Concordant (African American/African American patient- physician dyad) (n=62) | Race-Discordant (White physician/ African American patient dyad) (n=86) |
|---|---|---|---|---|
| Mean age | 60.61 (12.40) | 61.92 (12.46)a,b | 55.33 (12.31) | 56.56 (11.76) |
| Sex (female): % (n) | 37.2% (253/680) | 40.1% (217/541)b | 30.6% (19/62) | 22.1% (17/77) |
| Education: % (n) | ||||
| Less than high school | 7.76% (56/722) | 5.40% (31/574)a,b | 14.52% (9/62) | 18.60% (16/86) |
| High school | 28.53% (206/722) | 27.35% (157/574) | 32.26% (20/62) | 33.72% (29/86) |
| Some college/Tech school | 29.09% (210/722) | 27.35% (157/574) | 35.48% (22/62) | 36.05% (31/86) |
| College | 17.59% (127/722) | 19.69% (113/574)b | 11.29% (7/62) | 8.14% (7/86) |
| Grad school | 17.04 (123/722) | 20.21% (116/574)a,b | 6.45% (4/62) | 3.49% (3/86) |
| Mean # comorbid conditions (SD) | 3.10 (1.78) | 3.27 (1.82)a,b | 2.08 (1.33)c | 2.72 (1.46) |
| Kidney disease: n (%) | 9.31% (67/720) | 10.1% (58/573) | 3.2% (2/62) | 8.2% (7/85) |
| Diabetes: n (%) | 51.1% (369/722) | 52.4% (301/574) | 46.7% (29/62) | 45.3% (39/86) |
| # antihypertensive meds (SD) | 3.22 (1.71) | 3.21 (1.57) | 3.56 (1.78) | 3.33 (2.04) |
| Systolic BP (SD) | 141.3 (43.3) | 141.2 (47.7) | 143.9 (19.9) | 139.9 (15.4) |
| Diastolic BP (SD) | 79.1 (9.7) | 78.3 (9.5)a | 84.8 (10.5)c | 80.1 (9.0) |
| BP control: % (n) | 48.9% (267/545) | 49.6% (208/419) | 45.1% (28/62) | 48.4% (31/64) |
| Adherence: % (n) | ||||
| Always take | 80.9% (583/720) | 83.7% (481/573)a,b | 71.0% (44/62) | 68.2% (58/85) |
| Usually take | 18.1% (131/720) | 15.7% (90/573)a,b | 29.0% (18/62) | 27.1% (23/85) |
| Sometimes take | 0.8% (6/720) | 0.3% (2/573)b | 0.0% (0/62) | 4.7% (4/85) |
| Non-adherent: %: (n) | 19.0% (137/720) | 16.0% (92/573) | 29.0% (18/62) | 31.7% (27/85) |
| Mean trust, 1=none to 5=complete (SD) | 4.59 (0.61) | 4.58 (0.61) | 4.70 (0.61) | 4.62 (0.57) |
p <0.05 for the contrast between race/ethnic-concordant White and race/ethnic-concordant African American dyads
p <0.05 for the contrast between race/ethnic-concordant White and race/ethnic-discordant dyads
p <0.05 for the contrast between race/ethnic-concordant African American and race/ethnic-discordant dyads
Eighty-eight percent of patients were in race/ethnic-concordant relationships: 80% in a White/White dyad and 9% in an African American/African American dyad. Twelve percent of African American patients were in race/ethnic-discordant relationships with White physicians. White patients in White race/ethnic-concordant relationships were more likely to be older, attend graduate school, have a greater number of medical comorbidities, and report always taking their antihypertensive medications compared to African American patients in either concordant or discordant relationships. African American patients in race/ethnic-discordant dyads were least likely to report always being adherent to their medications, but this reached statistical significance only when compared to White patients in race/ethnic-concordant relationships.
Multivariate Logistic Regression Model Results
Table 3 illustrates the associations between racial/ethnic composition, trust, adherence, and BP control after adjusting for the patient and physician covariates. We found no direct associations between racial/ethnic composition of the dyad and BP control. White patients in race/ethnic-concordant relationships were 27% as likely to report better adherence to their medications as African American patients in race/ethnic-discordant relationships (OR: 1.27; 95% CI: 1.01, 1.61, p=0.04) There were no significant differences in adherence levels for African American patients in race/ethnic-concordant vs. discordant relationships. Overall, patients who reported better adherence to their medications were 73% as likely to have their BP controlled as those who reported poorer adherence (OR: 1.73, 95% CI: 1.12, 2.66; p=0.01). Higher levels of trust were associated with better medication adherence (OR: 1.17; 95% CI: 1.04, 1.31, p<0.001) and a tendency toward better BP control (OR: 1.26; 95% CI: 0.97, 1.63, p=0.07).
Table 3.
Adjusted Odds Ratios of the Associations between Patient- Physician Racial/Ethnic Concordance, Patient Trust, Medication Adherence, and BP Control
| MEDICATION ADHERENCE| | BP CONTROL | |||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| DIRECT EFFECTS | ||||
| Racial/Ethnic Concordance | ||||
| White-White | 1.27 (1,00, 1.61) | 0.04 | 0.86 (0.52, 1.43) | 0.58 |
| African American-African American | 1.07 (0.88, 1.29) | 0.47 | 0.87 (0.43, 1.79) | 0.72 |
| Race/Ethnic-discordant | - | - | - | - |
| Medication Adherence | ||||
| Always Adherent | 1.73 (1.12, 2.66) | 0.01 | ||
| Trust | 1.17 (1.04, 1.31) | <0.01 | 1.26 (0.97, 1.63) | 0.07 |
| INDIRECT EFFECTS | ||||
| RCW→Trust→Adherence | 0.99 (0.96, 1.01) | 0.48 | ||
| RCB→Trust→Adherence | 1.01 (0.97, 1.05) | 0.47 | ||
| RCW→Trust→BP Control | 0.98 (0.94, 1.03) | 0.50 | ||
| RCB→Trust→BP Control | 1.02 (0.96, 1.08) | 0.49 | ||
| RCW→Trust→Adherence→ BP Control | 0.99 (0.98, 1.00) | 0.50 | ||
| RCB→Trust→Adherence→ BP Control | 1.00 (0.98, 1.02) | 0.50 | ||
| RCW→Adherence→BP Control | 1.08 (0.97, 1.20) | 0.11 | ||
| RCB→Adherence→BP Control | 1.02 (0.95, 1.09) | 0.48 | ||
| Trust→Adherence→BP Control | 1.05 (0.99, 1.12) | 0.08 | ||
Adjusted for patient age, sex, education level and number of anti-hypertensive medications, and physician age, sex, specialty, and clinic location.
BP = Blood pressure; RCW = Race/Ethnic-Concordant White; RCA = Race/Ethnic-Concordant African American
Results of the mediation analyses showed a marginal indirect effect of trust on medication adherence leading to BP control, indicating that the relationship between trust and BP control is partially explained by medication adherence (OR: 1.05; 95% CI: 0.99,1.12, p = 0.08). The model provided a good fit to the data, CFI = 1.00, WRMR = 0.571, with a chi-square of 11.77, degrees of freedom (df) = 14, p = 0.62. Including patient education in our main models with racial/ethnic concordance did not substantially change our study findings.
Discussion
This study sought to elucidate the mechanisms through which racial/ethnic concordance might affect clinical outcomes. Contrary to our primary hypothesis, African American patients in race/ethnic-discordant patient-physician relationships were not associated with differences in BP control. This finding is consistent with a similar study that found no relationship between race/ethnic discordance and uncontrolled systolic BP among 108, 555 patients with diabetes (Traylor et al. 2009). However, we did find that racial/ethnic concordance was associated with better medication adherence among White patients receiving care from White physicians. To date, findings related to racial/ethnic concordance and medication adherence have been mixed (King et al. 2004; Schoenthaler et al. 2012; Traylor et al. 2012).
Due to the lack of association between racial/ethnic concordance and BP control, we were unable to demonstrate that trust and medication adherence served as mediators of poorer BP control for patients in race/ethnic-discordant relationships, as predicted by our second hypothesis. Previous studies report no association between racial/ethnic discordance and trust in the physician among hypertensive patients (Benkert et al. 2006). We did find a direct effect of trust in the physician on medication adherence, which corroborates previous findings that trust is an important predictor of medication adherence. For example, in a study of 1,305 African American and White patients with HIV, a one-point increase in patient trust was associated with an 18% increased odds of better adherence to antiretroviral medications (Saha et al. 2010). A prospective study of HIV patients bolsters this finding, reporting that trust was associated with medication adherence at the 4-week follow-up (Golin et al. 2002). Finally, among a mixed sample of chronically ill patients, of which 21% were hypertensive, patients were significantly more likely to report being adherent to their treatment if the patient-physician relationship was perceived as trusting and collaborative (Fuertes et al. 2007). Our data suggest that trust may partially explain the relationship between medication adherence and BP control. Future studies that assess the multiple dimensions of trust and utilize objective adherence assessments are needed to confirm this finding.
Limitations
Several limitations of this study should be noted. The cross-sectional design precludes any causal inference between patient trust, medication adherence and BP control. Because this was a secondary analysis of observational study data, we could not randomize patients to race/ethnic-concordant vs. discordant physicians. Thus, we were unable to assess whether patients preferentially chose their physician; the ability to choose a physician in terms of race/ethnicity can explain a significant portion of variance between race/ethnic concordance and satisfaction, use of preventive services, and rating provider care as excellent (Chen et al. 2005; Laveist and Nuru-Jeter 2002; Saha, Arbelaez, and Cooper 2003). The lack of a White patient-African American physician group may have limited the ability to detect an effect of race/ethnic discordance on medication adherence and BP control. Moreover, excluding this group could potentially introduce bias if, for example, White patients preferentially chose not to select African American physicians. However, only a small percentage of African American physicians (6%) were practicing at the participating clinics and thus available to patients for selection. We constructed dyads based on self-reported race of the patient and physician. We recognize the limitation of using the term ‘race’ which assumes genetic homogeneity within groups (Bhopal 2004). Moreover, data collected on ethnicity was limited to whether or not the patient was of Hispanic or Latino origin, as dictated by the United States Census Bureau (US Census 2001). As a result; we may have created dyads that were racially similar but also ethnically diverse.
We did not assess the duration of the patient-physician relationship; however, while not a direct assessment of relationship length, White physicians in this study had worked at their clinics twice as long as their African American colleagues. Thus, it is plausible that patients with White physicians enjoyed more continuity, potentially resulting in better adherence. Medication adherence was assessed with a single self-report measure for all prescribed medications, which may have led to an overestimation of adherence levels. However, the data show a significant association between a response of always being adherent and BP control. Finally, responses on our measure of trust were high potentially causing a ceiling effect, which would limit our ability to detect significant differences in the outcomes. Moreover, the measure was limited to perceptions of one’s physician and may not have captured other dimensions of trust that may be affected by racial/ethnic concordance; for example, distrust in the health care system as a whole, or in health insurers (Zheng et al. 2002; Rose et al. 2004). More qualitative data are needed to identify the specific dimensions and targets of patient trust that may be affected by patient-physician racial/ethnic concordance.
Conclusions and Implications
We found that high levels of trust were associated with medication adherence and BP control for patients in both race/ethnic-concordant and discordant dyads. This finding supports a growing body of evidence, which suggests that interpersonal factors that characterize the quality of the patient-physician relationship may be more important for addressing health disparities than patient-physician racial matching (as defined as a biological construct) (Street et al. 2008, Meghani et al. 2009, Martin and Cooper 2013). For example, recent research has demonstrated that perceptions of social concordance (Thorton et al. 2012) and personal similarity (Street et al. 2008) are more important predictors of patient positive affect, trust, satisfaction, and intention to adhere to treatment recommendations than racial identity. The current study corroborates these findings by demonstrating that patient trust in the physician was associated with better adherence for all patients, regardless of patient-physician racial/ethnic concordance.
Patient trust is a modifiable factor that can be addressed in future interventions directed at the patient, physician and health care system (Pearson and Raeke 2000). For example, trust in the physician is an important facilitator of self-efficacy, which plays an important role in a patient’s ability to enact and maintain self-management behaviors such as adhering to medications (Johnson et al. 2006; Lee and Lin 2009). One way to build self-efficacy is through engaging in participatory decision-making in the patient-physician relationship (Doescher et al. 2000; Johnson et al. 2006). Thus, interventions that activate patients in their care as well as help physicians to engage in more positive communicative behaviors can bolster self-efficacy leading to medication adherence and improved health outcomes.
Health system interventions directed at positive communication and information-sharing may also influence patient trust. At the interpersonal level, physician communication training focused on positive and empathic communication (e.g., increasing eye contact and dynamic positive interactions) can improve patient trust (Asan and Montague 2012). At the organizational level, regular assessments of patient trust with targeted directives to improve and understand barriers to trust can create an organizational culture that values patient-physician trust. Finally, health information technologies that offer shared visit notes or patient portals to increase access to information and enhance transparency may also increase trust in physicians (Andreassen et al. 2006; Delbanco et al.).
Key Messages.
Despite mounting evidence that patient-physician racial/ethnic concordance affects processes of care (e.g., patient satisfaction, health service utilization), the impact on clinical outcomes such as blood pressure control is unclear.
Higher levels of trust were associated with better medication adherence and a tendency toward better BP control, irrespective of patient-physician racial/ethnic concordance.
Future research is needed to understand whether interventions that facilitate patient trust at the interpersonal and organizational levels can improve heath behaviors and clinical outcomes for all patients.
Acknowledgments
Design and conduct of the MEMO Study was supported by the Agency for Healthcare Research and Quality (grant number 5 R01 HS011955).
Footnotes
An oral presentation of this manuscript was presented at the 34th Annual Meeting of the Society of General Internal Medicine in Phoenix, AZ, on May 5, 2011.
Conflict of Interest Statement: The authors have no conflicts of interest to disclose.
Contributor Information
Dr. Antoinette Schoenthaler, Email: Antoinette.Schoenthaler@nyumc.org, NYU School of Medicine, New York, United States
Dr. Enid Montague, Northwestern University, Evanston, United States
Ms. Linda Baier Manwell, University of Wisconsin School of Medicine & Public Health, Madison, United States
Dr. Roger Brown, University of Wisconsin-Madison, Madison, United States
Dr. Mark D. Schwartz, NYU School of Medicine, New York, United States
Mark Linzer, Hennepin County Medical Center, Minneapolis, United States.
References
- Agyemang C, Bhopal R, Bruijnzeels M. Negro, Black, African, African Caribbean, African American or what? Labelling African origin populations in the health arena in the 21st century. Journal Epidemiological Community Health. 2005;59:1014–1018. doi: 10.1136/jech.2005035964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreassen HK, Trondsen M, Kummervold PE, Gammon D, Hjortdahl P. Patients who use e-mediated communication with their doctor: new constructions of trust in the patient-doctor relationship. Qualitative Health Research. 2006;16(2):238–48. doi: 10.1177/1049732305284667. [DOI] [PubMed] [Google Scholar]
- Asan O, Montague E. Physician interactions with electronic health records in primary care. Health Systems. 2012 doi: 10.1057/hs.2012.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benkert R, Peters RM, Clark R, Keves-Foster K. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. Journal of the National Medical Association. 2006;(9):1532–40. [PMC free article] [PubMed] [Google Scholar]
- Bhopal R, Donaldson L. White, European, Western, Caucasian, or What? Inappropriate labeling in research on race, ethnicity, and health. American Journal of Public Health. 1998;88(9):1303–1307. doi: 10.2105/ajph.88.9.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. Journal of Epidemiological Community Health. 2004;58:441–445. doi: 10.1136/jech.2003013466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FM, Fryer GE, Jr, Phillips RL, Jr, Wilson E, Pathman DE. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Annals of Family Medicine. 2005;3(2):138–43. doi: 10.1370/afm.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, African American HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;(11):907–15. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Delbanco T, Walker J, Bell SK, Darer JD, Elmore JG, Farag N, Feldman HJ, Mejilla R, Ngo L, Ralston JD, Ross SE, Trivedi N, Vodicka E, Leveille SG. Inviting Patients to Read Their Doctors’ Notes: A Quasi-experimental Study and a Look Ahead. Annals of Internal Medicine. (7):461–70. doi: 10.7326/0003-4819-157-7-201210020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Archives of Family Medicine. 2000;(10):1156–63. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- Fuertes JN, Mislowack A, Bennett J, Paul L, Gilbert TC, Fontan G, Boylan LS. The physician-patient working alliance. Patient Education and Counseling. 2007;(1):29–36. doi: 10.1016/j.pec.2006.09.013. [DOI] [PubMed] [Google Scholar]
- Golin CE, Liu H, Hays RD, Miller LG, Beck CK, Ickovics J, Kaplan AH, Wenger NS. A prospective study of predictors of adherence to combination antiretroviral medication. Journal of General Internal Medicine. 2002;(10):756–65. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? The Milbank Quarterly. 2001;(4):613–39. v. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, Balkrishnan R. Measuring patients’ trust in their primary care providers. Medical Care Research and Review. 2002;(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- Hayduk LA. Structural equation modeling with LISREL. Baltimore: Johns Hopkins University Press; 1987. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indicies in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- IOM (Institute of Medicine) Unequal Treatment: Confronting racial and ethnic disparities in healthcare. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Johnson MO, Chesney MA, Goldstein RB, Remien RH, Catz S, Gore-Felton C, Charlebois E, Morin SF. Positive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV-infected adults: A mediation model. AIDS Patient Care and STDs. 2006;(4):258–68. doi: 10.1089/apc.2006.20.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. Journal of General Internal Medicine. 1998;(10):681–6. doi: 10.1046/j.1525-1497.1998.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King WD, Wong MD, Shapiro MF, Landon BE, Cunningham WE. Does racial concordance between HIV-positive patients and their physicians affect the time to receipt of protease inhibitors? Journal of General Internal Medicine. 2004;(11):1146–53. doi: 10.1111/j.1525-1497.2004.30443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health and Social Behavior. 2002;(3):296–306. [PubMed] [Google Scholar]
- Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Social Science and Medicine. 2009;(6):1060–8. doi: 10.1016/j.socscimed.2008.12.033. [DOI] [PubMed] [Google Scholar]
- Linzer M, Baier Manwell L, Mundt M, Williams E, Maguire A, McMurray J, Plane MB. Organizational Climate, Stress, and Error in Primary Care: The MEMO Study. In: Henriksen K, Battles JB, Marks ES, editors. Advances in Patient Safety: From Research to Implementation (Volume 1: Research Findings) D. I. Lewin; Rockville (MD): 2005. [PubMed] [Google Scholar]
- Might want to include the main MEMO paper from Annals of IM 2009, Linzer lead author?
- MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associations; 2008. [Google Scholar]
- Martin KD, Cooper LA. Maximizing the benefits of we” in race-discordant patient-physician relationships: Novel insights raise intriguing questions. Journal of General Internal Medicine. 2013;28(9):1119–21. doi: 10.1007/s1160601324487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RA, Behson SJ, Seifert CF. Strategies for dealing with measurement error in multiple regression. Journal of Academcy of Business and Economics. 2005;3:80–97. [Google Scholar]
- Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethnicity & Health. 2009;14(1):107–30. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- Osborn R, Squires D. International Perspectives on Patient Engagement: Results from the 2011 Commonwealth Fund Survey. Journal of Ambulatory Care Management. 2012;35(2):118–28. doi: 10.1097/JAC.0b013e31824a579b. [DOI] [PubMed] [Google Scholar]
- Pearson SD, Raeke LH. Patients’ trust in physicians: many theories, few measures, and little data. Journal of General Internal Medicine. 2000;15(7):509–13. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts KJ. Physician-patient relationships, patient satisfaction, and antiretroviral medication Adherence among HIV-infected adults attending a public health clinic. AIDS Patient Care STDS. 2002;16(1):43–50. doi: 10.1089/108729102753429398. [DOI] [PubMed] [Google Scholar]
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MRS, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 123(4):e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose A, Peters N, Shea JA, Armstrong K. Development and testing of the health care system distrust scale. Journal of General Internal Medicine. 2004;19(1):57–63. doi: 10.1111/j.1525-1497.2004.21146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. American Journal of Public Health. 2003;93(10):1713–9. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Jacobs EA, Moore RD, Beach MC. Trust in physicians and racial disparities in HIV care. AIDS Patient Care and STDs. 2010;24(7):415–20. doi: 10.1089/apc.2009.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Schoenthaler A, Allegrante JP, Chaplin W, Ogedegbe G. The Effect of Patient-Provider Communication on Medication Adherence in Hypertensive Black Patients: Does Race Concordance Matter? Annals of Behavioral Medicine. 2012;46:372–82. doi: 10.1007/s12160-011-9342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart MA. Effective physician-patient communication and health outcomes: A review. Canadian Medical Association Journal. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Stewart MA, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. Journal of Family Practice. 2000;49(9):796–804. [PubMed] [Google Scholar]
- Street RL, Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Annals of Family Medicine. 2008;6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton RLJ, Powe N, Roter D, Cooper LA. Patient–physician social concordance, medical visit communication and patients’ perceptions of health care quality. Patient Education and Counseling. 2011;85(3):e201–e208. doi: 10.1016/j.pec.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? Journal of General Internal Medicine. 2012;25(11):1172–7. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traylor AH, Subramanian U, Uratsu CS, Mangione CM, Selby JV, Schmittdiel JA. Patient race/ethnicity and patient-physician race/ethnicity concordance in the management of cardiovascular disease risk factors for patients with diabetes. Diabetes Care. 2009;33(3):520–5. doi: 10.2337/dc09-0760. dc09-0760 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. Questions and Answers for Census 2000 Data on Race. 2001 Retrieved September 3, 2013 from http://web.archive.org/web/20100304131211/http://www.census.gov/Press-Release/www/2001/raceqandas.html.
- World Health Organization (WHO) A global brief on hypertension: World Health Day 2013. World Health Organization Press; Geneva, Switzerland: 2013. [Google Scholar]
- Yu CY, Muthen BO. Muthen and Muthen, editor. Evaulation of model fit indices for latent variable models with categorical and continuous outcomes. CA; Los Angeles: 2001. [Google Scholar]
- Zheng B, Hall MA, Dugan E, Kidd KE, Levine D. Development of a scale to measure patients’ trust in health insurers. Health Services Research. 2002;37(1):187–202. [PubMed] [Google Scholar]


