Abstract
Current emphasis on patient outcomes within sleep medicine, with a particular focus on quality improvement and contained costs, calls for sleep specialists to develop innovative models for long-term care and management of sleep disorders patients. Multidisciplinary sleep centers can facilitate highest-quality care that is timely and cost-effective. Effective resource use in a multidisciplinary sleep center can help minimize fragmentation of care, reduce effort duplication, and control costs. Proposed strategies to help achieve a balance between quality of care and cost-effectiveness include: (1) multidisciplinary specialty clinics, (2) optimized use of information technology, and (3) adoption of reliable performance measures.
Citation:
Shelgikar AV, Durmer JS, Joynt KE, Olson EJ, Riney H, Valentine P. Multidisciplinary sleep centers: strategies to improve care of sleep disorders patients. J Clin Sleep Med 2014;10(6):693-697.
Keywords: multidisciplinary, sleep disorders, cost-effectiveness, outcomes, performance measures, information technologies
A team-based approach, relying on providers from multiple disciplines, is increasingly encouraged in health care, health research, health education, and health policy.1 A team-structured approach to patient care is particularly useful for patients with challenging diagnostic and management issues because it harnesses expertise across a wide spectrum of providers. The label of “multidisciplinary” indicates that different disciplines work on a problem in parallel or sequentially, while remaining within their disciplinary boundaries.1 Sleep medicine specialists commonly adopt a multidisciplinary practice model, a reflection of the evolution of sleep medicine since its establishment as a distinct discipline.
Since the discovery of REM sleep in 1953,2 advances in sleep biology and biomedical innovation have catapulted sleep medicine into its existence as a rapidly growing medical subspecialty. Centers dedicated to evaluation and management of sleep disorders have developed during the past quarter-century,3 a reflection of the field's relatively recent emergence. In that brief time, the field has grown from roots planted in few medical subspecialties to one that spans numerous disciplines. Providers from family medicine, internal medicine, neurology, otolaryngology, pediatrics, or psychiatry may now apply to sleep medicine fellowship programs.4
A clear advantage of multidisciplinary sleep centers is the presence of a wide depth and breadth of expertise available at one institution. The balance of quality, timely access, and cost of care is especially pertinent in this era of health care reform with a growing emphasis on outcomes-based population health management. Implementation of pathways to ensure best quality, timely, cost-effective care is often an overwhelming endeavor. Potential solutions include: (1) establishment of multidisciplinary specialty clinics, (2) incorporation of advanced technology to increase patient access to care, and (3) adoption of reliable performance measures.
MULTIDISCIPLINARY SPECIALTY CLINICS
In traditional care models, patients are referred from primary care provider to specialist or from one specialist to another, which results in numerous individual evaluations.5 Patients with chronic disease frequently must navigate a series of referrals and appointments. Lack of coordination amongst providers often exists, and patients may perceive the system to be overwhelming, time-consuming, and fragmented.6
For some patients, the need for diagnostic testing and specialty care can lead to long wait times for evaluation and treatment. Patients with obstructive sleep apnea (OSA) often experience long wait times to receive care. A survey of approximately 550 Canadian physicians involved in care of OSA patients (academic and urban family physicians, respirologists, and otolaryngologists) was done to examine patient wait times. Respondents were asked to estimate patient wait times for designated events (i.e., clinic appointments, sleep lab appointments, treatment initiation) during the evaluation and management of OSA. The results showed that patients waited a mean of 11.6 months to initiate continuous positive airway pressure and a mean of 16.2 months to initiate surgical therapy.7 Delayed treatment of OSA may also lead to increased cost. Studies have shown that adults with OSA have higher healthcare utilization prior to diagnosis.8–10 Increased healthcare utilization and total annual cost in years prior to diagnosis and treatment of OSA has also been shown for children.11
One approach to improve this process is to establish multi-disciplinary specialty clinics, which focus on multi-faceted evaluation and treatment of a given disease. Multidisciplinary clinics are used in the ongoing management of chronic diseases such as diabetes mellitus and heart failure.12,13 Multidisciplinary clinics are also commonly encountered in the medical and surgical evaluation of cancer patients. In fact, the Commission on Cancer and the American College of Surgeons require multidisciplinary cancer conferences for accreditation of health centers that provide multidisciplinary care.14
This team-oriented approach has long been considered an important component of the comprehensive care of sleep disorders patients. For example, multidisciplinary clinics can be helpful in the evaluation and management of obstructive sleep apnea patients. Continuous positive airway pressure (CPAP) is a treatment option for patients with mild OSA and is indicated for treatment of moderate to severe OSA.15 However, CPAP non-adherence, defined as a mean of ≤ 4 hours of use per night, affects 29% to 83% of patients,16,17 and alternative interventions requiring input from other specialists may be needed for these individuals. Practice parameters from the American Academy of Sleep Medicine identify other treatment modalities to consider for patients who are unable or unwilling to use CPAP therapy. In these patients, oral appliances are indicated for treatment of mild to moderate OSA.18 Maxillo-mandibular advancement is indicated for patients with severe OSA who are unable to unwilling to use CPAP.19,20 Procedures such as uvulopalatopharyngoplasty and multi-level surgery, among others, may also be considered in some patients.20 Appointments with numerous specialists to discuss these options can be difficult and time-consuming. A multidisciplinary clinic, however, facilitates direct communication among specialists when considering various treatments for OSA, including weight loss and other lifestyle modification, CPAP, nasal and/or palatal surgery, mandibular advancement devices, and orthognathic surgery.21 Providers with expertise in each of these treatments evaluate the patient, and then convene to develop a treatment plan best suited to the individual. As a result of discussion among specialists, patients receive a well-reasoned, collective treatment plan rather than multiple isolated opinions.21 Multidisciplinary clinics can include not only medical and surgical specialists, but also healthcare providers from other fields. Sharma et al. recently outlined a multidisciplinary model that allows patients with sleep related breathing disorders to receive integrated care from dental sleep medicine and sleep medicine specialists.22 In this model, patients would receive collaborative evaluation, management, and follow-up from dentists and physicians with expertise in treatment of obstructive sleep apnea.
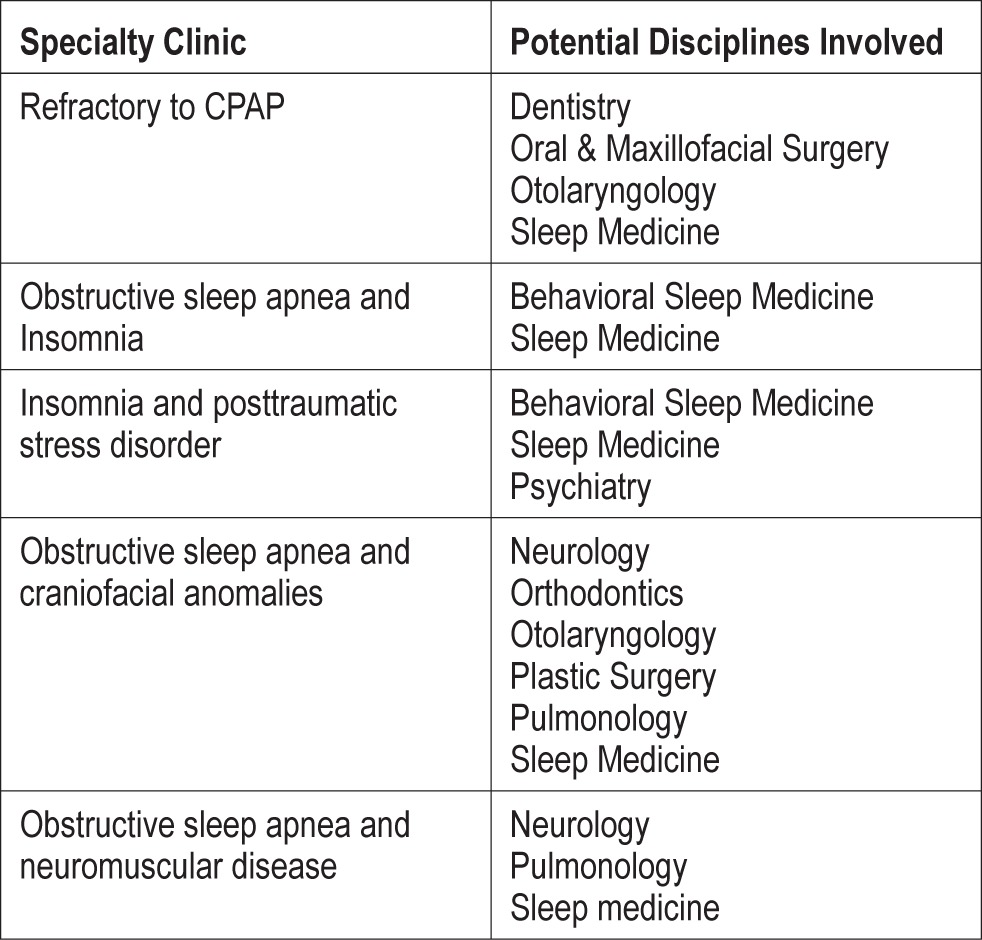
Opportunities exist for multidisciplinary clinics to serve other cohorts of sleep disorders patients, not only adults with sleep disordered breathing. Wiggs has called for the creation of pediatric multidisciplinary sleep centers to effectively meet the needs of children with sleep disorders, particularly those with intellectual disabilities and with neurological or psychiatric conditions.23 Adenotonsillectomy is the first-line treatment of obstructive sleep apnea in children with adenotonsillar hypertrophy.24,25 However, treatment can be very challenging in children with complex comorbidities such as craniofacial abnormalities, neuromuscular disease, genetic or metabolic syndromes, or cerebral palsy.26 A multidisciplinary specialty clinic could facilitate the multi-faceted evaluation, treatment, and follow-up that these children require. A treatment model for multidisciplinary evaluation and management of patients with obstructive sleep apnea and comorbid insomnia has also recently been proposed.27 Multidisciplinary insomnia clinics could be tailored to both adult and pediatric patients. Table 1 outlines potential multidisciplinary specialty clinics that multi-disciplinary sleep centers may consider utilizing to care for specific groups of sleep disorders patients.
Table 1.
Examples of specialty sleep clinics to consider in a multidisciplinary sleep center
Multidisciplinary specialty clinics and related conferences have the potential to impact patient care. Improved patient outcomes have been shown for patients with heart failure,28 amyotrophic lateral sclerosis,29 and hepatocellular carcinoma30 who are treated in multidisciplinary clinics; this list grows as multidisciplinary approaches are utilized for evaluation and management of other diseases. The field of sleep medicine, at its core, is a multidisciplinary entity. Sleep medicine centers with diverse expertise should be optimally positioned to establish successful multidisciplinary specialty clinics to enhance care of sleep disorders patients.
INFORMATION TECHNOLOGY SOLUTIONS
Cloud-computing systems are controlled by a network of external servers and data stored on these servers are easily accessed through the web. Use of cloud-based systems obviates the need for an institution or practice to maintain servers or host software. Rather, data can be moved to the cloud and provided on demand, which requires less energy, physical space, and technical staff.31 Figure 1 depicts how a cloud-based care management program provides another means of patient-provider communication. Cloud-based paradigms have been developed to enhance care in a variety of populations, including elderly patients in assisted living facilities32 and babies in neonatal intensive care units and special care nurseries.33 Xia and colleagues recently proposed a cloud-based system for real time electrocardiogram (ECG) monitoring and analysis, in which doctor and patient consoles could access the cloud system through a mobile client or a desktop/web client.34
Figure 1. Increased patient-provider communication with use of cloud-based technology.
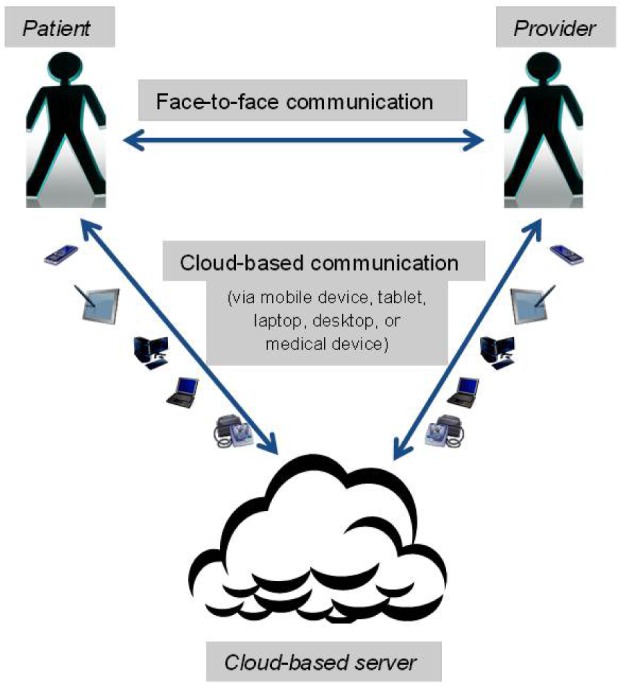
Cloud-based systems offer new possibilities for chronic disease management via enhanced patient-provider communication, easily accessible adherence data, and real-time ability to modify and optimize therapy. Most importantly, use of cloud-based systems may actually facilitate improved outcomes for patients with chronic diseases. Piette et al. used a cloud-computing system to provide self-care guidance for 85 adult diabetic patients living in an underdeveloped region of Honduras. After six weeks in the study, 98% of participants reported that due to the program they improved in aspects of diabetes management, including glycemic control (56%) or foot care (89%). In addition, mean HbA1c values reduced from 10% at baseline to 8.9% at six-week follow-up.35 Use of tele-health strategies have also been shown to improve blood pressure control36 and increase patient and provider satisfaction as well as to reduce costs.37 Similar systems could be used by multidisciplinary sleep centers to augment care of sleep disorders patients. Cloud-computing strategies have been developed to improve access, quality, and cost-effectiveness of care in outpatient and inpatient settings.38,39 Use of cloud-based tele-health technologies in the practice of multidisciplinary sleep medicine may have the potential to improve care quality and outcomes for patients with sleep disorders.
Patient privacy and integrity of protected health information must be upheld with any information technology-based solution. General guidelines are already in place to delineate accountability of information security in cloud-computing systems. The cloud user is responsible for application-level security. The cloud provider, on the other hand, is responsible for physical security and likely for enforcement of external firewall policies. Security for intermediate layers of the software stack is shared between the cloud user and the cloud operator.40 Security responsibilities are also dictated by The Health Insurance Portability and Accountability Act of 1996 (HIPAA)41 and The Health Information Technology for Economic and Clinical Health (HITECH) Act.42 Federal legislation requires a “Business Associate Contract” between third parties that handle protected health information and the client.43 This contract must specify that the cloud provider will not engage in unauthorized use or disclosure of protected health information, will use appropriate safeguards, report illegal use of protected health information, and return or destroy the protected health information upon termination of the contract.44 Adherence to clearly defined security requirements can facilitate successful use of cloud-based computing systems in patient care.
PERFORMANCE MEASURES
Multidisciplinary sleep centers have potential to facilitate high-quality care in the current era of health care reform. The Patient Protection and Affordable Care Act45 calls for Accountable Care Organizations (ACOs) as the primary mechanism to achieve high-quality, cost-effective patient care. An ACO is a team of providers, tied together under a common organizational structure, that assumes responsibility for delivering and managing the entire spectrum of care for a cohort of beneficiaries while reducing the cost of care for that same cohort.46 Payment is associated with performance measures that emphasize quality improvement as one important means of reducing costs. Thirty-three measures fall within the four following ACO quality benchmark categories: patient/caregiver experience, care coordination/patient safety, preventative health, and at-risk population/frail elderly health.47 Twelve of these 33 ACO metrics may easily pertain to multidisciplinary sleep centers, as these measures are directly applicable to obstructive sleep apnea patients. Some of these metrics may also apply to patients with other sleep disorders, particularly with continued development and validation of means to track therapeutic intervention and treatment response.
The Physician Quality Reporting System was enacted by the Centers for Medicare & Medicaid Services in 2007. Since 2012, the Physician Quality Reporting System (Physician Quality Reporting) Measures List48 has included four sleep apnea measures: (1) Assessment of Sleep Symptoms; (2) Severity Assessment at Initial Diagnosis; (3) Positive Airway Pressure Therapy Prescribed; (4) Assessment of Adherence to Positive Airway Pressure Therapy. The 2013 requirement is that the sleep apnea measures be reported for 20 patients in order to receive an incentive and avoid a financial penalty. The Parkinson disease measure groups indicate that all patients with a diagnosis of Parkinson disease should be asked about sleep disturbances at least annually. The Centers for Medicare & Medicaid Services recently published a proposed rule which stipulates that all measure groups include a minimum of six measures.49 This proposal includes a plan to increase the sleep apnea measures group, with three new measures to be added to the four measures already in place. Patient-reported outcomes should also be incorporated into quality measures.50,51
The American Academy of Sleep Medicine has also developed the Innovation Care Delivery and Management Program for Patients with OSA (ICDMPPO) with five goals: improved care coordination; increased adherence to PAP therapy; reduced comorbidities; strengthened patient satisfaction; and realized, significant cost savings for Centers for Medicare & Medicaid Services.52 The proposed paradigm details cost-effective methods to integrate and manage care of patients with obstructive sleep apnea across multiple providers. The program outlines enhanced information technology tools, such as a comprehensive patient-tracking and outcomes database and web-based educational modules, which would be necessary for successful implementation. This model may serve as a prototype for multidisciplinary sleep centers to develop comprehensive, cost-effective programs that improve patient-provider communication and patient outcomes.
Accountable care organizations currently highlight primary care settings and outcome measures rooted in chronic disease management, though specialists' roles in ACOs are largely undefined. This dynamic landscape offers sleep specialists the opportunity to define their role, and the importance of long-term, multidisciplinary management of sleep disorders, within the auspices of the Patient Protection and Affordable Care Act. The patient-centered aspect of multidisciplinary sleep centers may facilitate sleep medicine to be systematized into ACOs.
POTENTIAL PAYOFFS
The direct and indirect costs of untreated sleep disorders on a patient and public health level are profound. AlGhanim and colleagues examined the economic impact of untreated sleep disorders. These authors reported that in 2004 the total economic burden of sleep disorders in Australia, with a population of 20.1 million, was $7.494 billion (reported in 2004 United States dollars). When extrapolated to the United States population, which is ten-fold greater in size, these costs were comparable to those associated with diabetes ($132 billion in 2002). Minimal yet promising evidence exists for cost-saving within sleep medicine. Cost-effectiveness is typically expressed as incremental cost-effectiveness ratio (ICER), which is the ratio of the incremental cost and incremental change in quality adjusted life years (QALY) that stems from use of a specified treatment.53 By convention an ICER/QALY value of $50,000 is considered acceptable/beneficial, though there is evidence to suggest this limit should be higher.54 Pietzsch and colleagues used a Markov model to perform an economic analysis of the diagnosis and treatment of moderate to severe obstructive sleep apnea based on a hypothetical average cohort of 50-year-old males. Parameter ranges were derived from the literature to conduct single-variable and multi-variable sensitivity analyses, with a specific focus on cardiovascular health. The sensitivity analyses showed that CPAP therapy compared to no treatment in patients with moderate-to-severe obstructive sleep apnea had an ICER/QALY value of $15,915, which indicated significant cost-effectiveness of CPAP therapy in these OSA patients.55 Sensitivity analyses also showed that full-night polysomnography and initiation of CPAP therapy compared to no diagnosis and no treatment for the diagnosis of obstructive sleep apnea in patients with 50% pretest probability of obstructive sleep apnea had an ICER/QALY value of $17,131. These data suggest that diagnosis and treatment of obstructive sleep apnea is a cost-effective endeavor. Treatment of other sleep disorders has been shown to be cost-effective as well.56,57
CONCLUSIONS
Multidisciplinary sleep centers can improve quality and cost-effectiveness of patient care via multidisciplinary specialty clinics, thoughtful use of tele-health capabilities, and reliable performance measures. As a bona fide multidisciplinary specialty, sleep medicine provides opportunities to create and implement innovative means of improved patient care. As multi-disciplinary sleep centers find new ways to coordinate care for adult and pediatric sleep disorders patients, ongoing research will help determine which strategies best allow sleep specialists to provide high quality, cost-effective, patient-centered care.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Riney has participated in a speaking engagement with Jazz Pharmaceuticals. Mr Valentine is the Ex-Chief Executive Officer with previous ownership interest in Sleep HealthCenters, LLC, and serves as Senior Managing Director for KCP Advisory Group LLC, a consulting firm. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29:351–364. [PubMed] [Google Scholar]
- 2.Aserinsky E, Kleitman N. Regularly occurring periods of eye motility, and concomitant phenomena, during sleep. Science. 1953;118:273–4. doi: 10.1126/science.118.3062.273. [DOI] [PubMed] [Google Scholar]
- 3.Shepard JW, Jr., Buysse DJ, Chesson AL, Jr., et al. History of the development of sleep medicine in the United States. J Clin Sleep Med. 2005;1:61–82. [PMC free article] [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. Program Requirements for Graduate Medical Education in Sleep Medicine. 2012. [Accessed August 23, 2013]. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/520_sleep_medicine_07012013_1-YR.pdf.
- 5.Fennell ML, Das IP, Clauser S, Petrelli N, Salner A. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr. 2010:72–80. doi: 10.1093/jncimonographs/lgq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Metz DC, Choi J, Strosberg J, et al. A rationale for multidisciplinary care in treating neuroendocrine tumours. Curr Opin Endocrinol. 2012;19:306–13. doi: 10.1097/MED.0b013e32835570f1. [DOI] [PubMed] [Google Scholar]
- 7.Rotenberg B, George C, Sullivan K, Wong E. Wait times for sleep apnea care in Ontario: a multidisciplinary assessment. Can Respir J. 2010;17:170–4. doi: 10.1155/2010/420275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banno K, Manfreda J, Walld R, Delaive K, Kryger MH. Healthcare utilization in women with obstructive sleep apnea syndrome 2 years after diagnosis and treatment. Sleep. 2006;29:1307–11. doi: 10.1093/sleep/29.10.1307. [DOI] [PubMed] [Google Scholar]
- 9.Albarrak M, Banno K, Sabbagh AA, et al. Utilization of healthcare resources in obstructive sleep apnea syndrome: a 5-year follow-up study in men using CPAP. Sleep. 2005;28:1306–11. doi: 10.1093/sleep/28.10.1306. [DOI] [PubMed] [Google Scholar]
- 10.Ronald J, Delaive K, Roos L, Manfreda J, Bahammam A, Kryger MH. Health care utilization in the 10 years prior to diagnosis in obstructive sleep apnea syndrome patients. Sleep. 1999;22:225–9. doi: 10.1093/sleep/22.2.225. [DOI] [PubMed] [Google Scholar]
- 11.Tarasiuk A, Greenberg-Dotan S, Simon-Tuval T, et al. Elevated morbidity and health care use in children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2007;175:55–61. doi: 10.1164/rccm.200604-577OC. [DOI] [PubMed] [Google Scholar]
- 12.Codispoti C, Douglas MR, McCallister T, Zuniga A. The use of a multidisciplinary team care approach to improve glycemic control and quality of life by the prevention of complications among diabetic patients. J Okla State Med Assoc. 2004;97:201–4. [PubMed] [Google Scholar]
- 13.Ryder M, Beattie JM, O'Hanlon R, McDonald K. Multidsciplinary heart failure management and end of life care. Curr Opin Support Palliat Care. 2011;5:317–21. doi: 10.1097/SPC.0b013e32834d749e. [DOI] [PubMed] [Google Scholar]
- 14.Pawlik TM, Laheru D, Hruban RH, et al. Evaluating the impact of a single-day multidisciplinary clinic on the management of pancreatic cancer. Ann Surg Oncol. 2008;15:2081–8. doi: 10.1245/s10434-008-9929-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kushida CA, Littner MR, Hirshkowitz M, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29:375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 16.Weaver TE, Kribbs NB, Pack AI, et al. Night-to-night variability in CPAP use over the first three months of treatment. Sleep. 1997;20:278–83. doi: 10.1093/sleep/20.4.278. [DOI] [PubMed] [Google Scholar]
- 17.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kushida CA, Morgenthaler TI, Littner MR, et al. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: An update for 2005. Sleep. 2006;29:240–3. doi: 10.1093/sleep/29.2.240. [DOI] [PubMed] [Google Scholar]
- 19.Boyd SB, Walters AS, Song YN, Wang L. Comparative effectiveness of maxillomandibular advancement and uvulopalatopharyngoplasty for the treatment of moderate to severe obstructive sleep apnea. J Oral Maxil Surg. 2013;71:743–751. doi: 10.1016/j.joms.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aurora RN, Casey KR, Kristo D, et al. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33:1408–13. doi: 10.1093/sleep/33.10.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.L'Estrange PR, Battagel JM, Nolan PJ, Harkness B, Jorgensen GI. The importance of a multidisciplinary approach to the assessment of patients with obstructive sleep apnoea. J Oral Rehabil. 1996;23:72–77. doi: 10.1111/j.1365-2842.1996.tb00815.x. [DOI] [PubMed] [Google Scholar]
- 22.Sharma S, Essick G, Schwartz D, Aronsky AJ. Sleep medicine care under one roof: a proposed model for integrating dentistry and medicine. J Clin Sleep Med. 2013;9:827–33. doi: 10.5664/jcsm.2934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wiggs LD. Paediatric sleep disorders: the need for multidisciplinary sleep clinics. Int J Pediatr Otorhinolaryngol. 2003;67(Suppl 1):S115–118. doi: 10.1016/j.ijporl.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130:576–84. doi: 10.1542/peds.2012-1671. [DOI] [PubMed] [Google Scholar]
- 25.Baugh RF, Archer SM, Mitchell RB, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144:S1–30. doi: 10.1177/0194599810389949. [DOI] [PubMed] [Google Scholar]
- 26.Ishman SL. Evidence-based practice pediatric obstructive sleep apnea. Otolaryng Clin N Am. 2012;45:1055–69. doi: 10.1016/j.otc.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 27.Ong JC, Crisostomo MI. The more the merrier? working towards multidisciplinary management of obstructive sleep apnea and comorbid insomnia. J Clin Psychol. 2013;69:1066–77. doi: 10.1002/jclp.21958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ducharme A, Doyon O, White M, Rouleau JL, Brophy JM. Impact of care at a multidisciplinary congestive heart failure clinic: a randomized trial. Can Med Assoc J. 2005;173:40–45. doi: 10.1503/cmaj.1041137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Traynor BJ, Alexander M, Corr B, Frost E, Hardiman O. Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996-2000. J Neurol Neurosurg Psychiatry. 2003;74:1258–61. doi: 10.1136/jnnp.74.9.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yopp AC, Mansour JC, Beg MS, et al. Establishment of a multidisciplinary hepatocellular carcinoma clinic is associated with improved clinical outcome. Ann Surg Oncol. 2014;21:1287–95. doi: 10.1245/s10434-013-3413-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vilaplana J, Solsona F, Abella, Filgueira R, Rius J. The cloud paradigm applied to e-Health. BMC Med Inform Decis Mak. 2013;13:35. doi: 10.1186/1472-6947-13-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forkan A, Khalil I, Tari Z. A cloud-oriented context-aware middleware in ambient assisted living. Future Generation Computer Systems. 2013 [Google Scholar]
- 33.McGregor C, Heath J, Ming W. A Web services based framework for the transmission of physiological data for local and remote neonatal intensive care. The 2005 IEEE International Conference Proceedings on e-Technology, e-Commerce and e-Service 2005; pp. 496–501. [Google Scholar]
- 34.Xia H, Asif I, Zhao X. Cloud-ECG for real time ECG monitoring and analysis. Comput Methods Programs Biomed. 2013;110:253–9. doi: 10.1016/j.cmpb.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Piette JD, Mendoza-Avelares MO, Ganser M, Mohamed M, Marinec N, Krishnan S. A preliminary study of a cloud-computing model for chronic illness self-care support in an underdeveloped country. Am J Prev Med. 2011;40:629–632. doi: 10.1016/j.amepre.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control a cluster randomized clinical trial. JAMA. 2013;310:46–56. doi: 10.1001/jama.2013.6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Med. 2013;7:e1–8. [PMC free article] [PubMed] [Google Scholar]
- 38.Padhy RP, Patra MR, Satapathy SC. Design and implementation of a cloud based rural healthcare information system model. Univers J Appl Comput Sci Technol. 2012;2:149–57. [Google Scholar]
- 39.McGregor C. A cloud computing framework for real-time rural and remote service of critical care. In: Olive M, Solomonides T, editors. Proceedings of CBMS 2011 the 24th International Symposium on Computer-Based Medical Systems; Institute of Electrical and Electronics Engineers, Inc.; 2011. [Google Scholar]
- 40.Armbrust M, Fox A, Griffith R, et al. A view of cloud computing. Commun ACM. 2010;53:50–8. [Google Scholar]
- 41.U.S. Department of Health & Human Services. Health Infomation Privacy. [Accessed February 11, 2014]. Available at: http://www.hhs.gov/ocr/privacy/
- 42.U.S. Department of Health & Human Services. HITECH Act Enforcement Final Rule. Federal Register. 2013.
- 43.U.S. Department of Health & Human Services. Business Associates. [Accessed February 14, 2014]. Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/businessassociates.html.
- 44.EJ S. Reconciliation of the cloud computing model with US federal electronic health record regulations. J Am Med Inform Assoc. 2011;19:161–5. doi: 10.1136/amiajnl-2011-000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Affordable Care Act. 2010. Mar 22, H.R. 3590.
- 46.Maddux FW, McMurray S, Nissenson AR. Toward population management in an integrated care model. Clin J Am Soc Nephrol. 2013;8:694–700. doi: 10.2215/CJN.09050912. [DOI] [PubMed] [Google Scholar]
- 47.RTI International T. Waltham: West Des Moines; 2010. Accountable Care Organization 2012 Program Analysis: Final Report. [Google Scholar]
- 48.Centers for Medicare & Medicaid Services. 2012 Physician Quality Reporting System (Physician Quality Reporting) Measures List. 2012 [Google Scholar]
- 49.Centers for Medicare & Medicaid Services. Proposed Rules. Federal Register. 2013:43282–43532. [Google Scholar]
- 50.Snyder CF, Jensen RE, Segal JB, Wu AW. Patient-reported outcomes (PROs): putting the patient perspective in patient-centered outcomes research. Med Care. 2013;51:S73–S79. doi: 10.1097/MLR.0b013e31829b1d84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu AW, Kharrazi H, Boulware LE, Snyder CF. Measure once, cut twice--adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. J Clin Epidemiol. 2013;66:S12–20. doi: 10.1016/j.jclinepi.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.American Academy of Sleep Medicine. Innovation Care Delivery and Management Program for Patients with OSA. Available at: http://www.aasmnet.org/resources/pdf/SleepInnovationProposal.pdf.
- 53.AlGhanim N, Comondore VR, Fleetham J, Marra CA, Ayas NT. The economic impact of obstructive sleep apnea. Lung. 2008;186:7–12. doi: 10.1007/s00408-007-9055-5. [DOI] [PubMed] [Google Scholar]
- 54.Ubel PA, Hirth RA, Chernew ME, Fendrick AM. What is the price of life and why doesn't it increase at the rate of inflation? Arch Intern Med. 2003;163:1637–41. doi: 10.1001/archinte.163.14.1637. [DOI] [PubMed] [Google Scholar]
- 55.Pietzsch JB, Garner A, Cipriano LE, Linehan JH. An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to-severe obstructive sleep apnea. Sleep. 2011;34:695–709. doi: 10.5665/SLEEP.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reinhold T, Muller-Riemenschneider F, Willich SN, Bruggenjurgen B. Economic and human costs of restless legs syndrome. PharmacoEconomics. 2009;27:267–79. doi: 10.2165/00019053-200927040-00001. [DOI] [PubMed] [Google Scholar]
- 57.McCrae CS, Bramoweth AD, Williams J, Roth A, Mosti C. Impact of brief cognitive behavioral treatment for insomnia on health care utilization and costs. J Clin Sleep Med. 2014;10:127–35. doi: 10.5664/jcsm.3436. [DOI] [PMC free article] [PubMed] [Google Scholar]


