Synopsis
Substance use among adolescents increases the risk of unplanned pregnancies, which then increases the risk of fetal exposure to addictive, teratogenic substances. Specific interventions are necessary to target pregnancy planning and contraception among reproductive age substance users. Screening for substance use using the CRAFFT is recommended in all health care settings treating adolescent patients. Screening for tobacco and nicotine use is also recommended along with provision of smoking cessation interventions. Using motivational interviewing style and strategies is recommended to engage adolescents in discussions related to reducing substance use, risky sexual behavior, and probability of unplanned pregnancy or late-detection pregnancy. Earlier interventions that strengthen autonomy and resourcefulness in recognizing and caring for an unplanned conception is a form of advanced directive that may well reduce fetal exposure to tobacco, alcohol, and drugs and simultaneously empower girls and women in self-care.
Keywords: Adolescents, Substance Use, Unintended Pregnancy, Contraception, Motivational Interviewing
INTRODUCTION
Most United States teen pregnancies are unplanned; preconception substance use is a significant risk factor for unintended pregnancy (Finer and Zolna, 2013) and both teenage pregnancy and teenage substance use are national public health concerns targeted for improved outcomes (USHHS, Healthy People 2020). Unplanned pregnancies are associated with higher rates of maternal infections, obstetric complications, low birth weight, childhood growth stunting, poor child development, and subsequent child abuse or neglect (Institute of Medicine, 1995; Baydar, 1995; Naimi et al., 2003; Shapiro-Mendoza et al., 2005). Teen pregnancy and childbearing also has substantial economic and social costs: U.S. taxpayers paid $10.9 billion in 2008 for costs associated with teen pregnancy including increased health care, foster care, lost tax revenue, and higher incarceration rates among children of teen parents (National Campaign to Prevent Teen and Unplanned Pregnancy, 2011).
This article presents recent data relevant to adolescent sexuality and substance use with the aim of defining strategies to reduce the risk of unplanned pregnancy in substance using teens and to thereby protect healthy adolescent development and prevent fetal exposure to substances.
ADOLESCENT SUBSTANCE USE AND SEXUAL ACTIVITY
Teen substance use is an enduring problem in the United States. In 2011, 75% of high school students reported having used addictive substances including tobacco, alcohol, marijuana and other illicit drugs; 46% reported current use of addictive substances; and one in three substance-using students met the medical criteria for addiction (Adolescent substance use, 2011).
According to the Monitoring the Future database survey results for 2012 (Johnston et al., 2013), high school seniors self-report the following past-year substance use rates:
24% are binge drinkers (drank 5 or more drinks in a row at least once in the past 2 weeks)
17% are current tobacco cigarette smokers
8% misuse prescription opioids
6.5% are daily or near-daily marijuana users
These national data are consistent with other 2012 data showing one in five high school girls binge drink (defined as 4 or more drinks over 3 hours; Substance Abuse and Mental Health Administration/NSDUH, 2013).
Almost half (47.4%) of high school students have had sexual intercourse and 22% of sexually active high school students reported having used alcohol or other drugs before their last sexual experience (26% of boys and 18% of girls) (CDC, 2012). Risk reduction efforts targeting safer sexual behavior is most relevant in teens 15 and older since rates of sexual activity in the youngest adolescents (age 10-14) are much lower than in age 15 and older, and in those age 12 and younger sexual activity is mostly non-consensual, representing a different public health concern beyond the scope of this paper, i.e., preventing the sexual abuse of minors (Finer and Philbin, 2013).
UNPLANNED PREGNANCY AND SUBSTANCE USE
Defined by Finer and Zolna (2013) as mistimed (pregnancy occurring sooner than desired) or unwanted pregnancies, unintended pregnancies are associated with potential health risks to the fetus due to delayed pregnancy recognition with 58% of unplanned pregnancies being confirmed after five weeks gestation (Naimi, 2003). More than half (51%) of all pregnancies in the United States in 2008 were unintended (rate of 54 unintended pregnancies per 1000 women aged 15-44 years), with 91% of all pregnancies in 15-17 year olds being unintended. Between 2001-2008 the rate rose for both unintended pregnancy and for those continuing an unplanned pregnancy to childbirth (Finer and Zolna, 2013). Therefore, delayed pregnancy recognition is more likely to result in inadequate prenatal care and unintentional fetal exposure to substances.
Rates of unintended pregnancies are higher among substance using women, especially opioid users. Among treatment-seeking pregnant women with opioid use disorders, 86% of pregnancies were reported to be unplanned (Heil et al., 2011). Prospective self-report surveys of outpatient women in an Australian opioid treatment program revealed that nearly half (47%) had a teenage pregnancy and 84% of these were unplanned; nearly one third of the sample were pregnant in the year prior to entry with 75% of these pregnancies unplanned (Black et al., 2012). Risk factors associated with unplanned pregnancy included substance intoxication during sexual activity and lack of contraceptive use.
Among white women participating in a large national community sample study using case control methods (N= 72,907; Pregnancy Risk Assessment Monitoring System), preconception binge drinking was significantly associated with unplanned pregnancy and was also predictive of alcohol and tobacco use during pregnancy (Naimi, 2003).
The relationships among age, substance use, and risky sexual behavior for unplanned pregnancy are complex and frequently confounded by other high-risk demographic factors such as race/ethnicity, poverty, lower education, being a victim of abuse, being the child of a teenage mother, co-occurring mental illness, and lack of access to health care (e.g., Kotchik et al., 2001; Meade and Ickovics, 2005; Martinez et al., 2011). Adolescents who are sexually active and use substances have high rates of unintended pregnancy and of repeat unplanned pregnancy for multiple reasons. Teens that use tobacco, alcohol, marijuana or other drugs are more likely to be sexually active, to engage in risky sexual behavior and to experience the consequences of risky sex, including unintended pregnancy, compared with peers who do not use substances (Adolescent substance use, 2011). Moreover, a sexually active teen has high fertility: for teens age 16 -19, the probability of becoming pregnant is 2-5 times more likely for teens not using contraception at first sexual intercourse compared to those who did use contraception at first sex (Martinez et al., 2011). The more forms of addictive substances a teen uses in his or her lifetime, the less likely that teen is to report condom use at last intercourse (Santelli et al., 2001; Adolescent substance use, 2011). Absence of any teen contraceptive use is high: half of pregnant teens age 15-18 were not using contraception when they became pregnant and 31% of these believed they could not get pregnant at the time (CDC, 2012).
PREGNANT TEEN SUBSTANCE USE
The most recent national estimates of substance use among pregnant teenagers are known from self-report data in the large National Survey on Drug Use and Health (Substance Abuse and Mental Health Administration/NSDUH, 2013). In 2011-2012 pooled data for pregnant teens age 15 to 17, 18.3% reported past-month illicit drug use, a significant increase from 2009-2010 (15.7%). Young pregnant teens reported greater drug use compared to same-age non-pregnant peers (13.8%), double the rate of pregnant youth age 18-25 (9%), and 6 times the rate of pregnant women age 26 to 44 (3.4%). Specific drugs used remains stable, with marijuana, cocaine, and prescription medications (mainly opioid analgesics) being the top three reported in order of greatest frequency of use among all pregnant women age 15 to 44.
Past-month alcohol use is significantly less among pregnant youth age 18-25 compared to age-matched non-pregnant peers (7% vs. 60%), but pregnant teens age 15-17 are drinking at half the rate of age-matched non-pregnant peers (13.4% vs. 21.6%) and double the rate of pregnant youth. These rates are unchanged since 2009-2010.
Past-month cigarette use is unknown for age 15-17 but nearly 21% for age 18-25. Although data for all pregnant women age 15-44 indicate that rates of second and third trimester use of alcohol and drugs fall below 5%, tobacco use persists at rates of 13.6% and 11.1% in second and third trimester, respectively. These data are alarming given the teratogenic effects of prenatal exposure to addictive substances reviewed by Rayburn in this issue and previously by Behnke and Smith (2013). Furthermore, these estimates may under-represent true rates of fetal exposure due to reluctance to disclose substance use, especially among underage users and pregnant women.
SCREENING ADOLESCENTS FOR SUBSTANCE USE
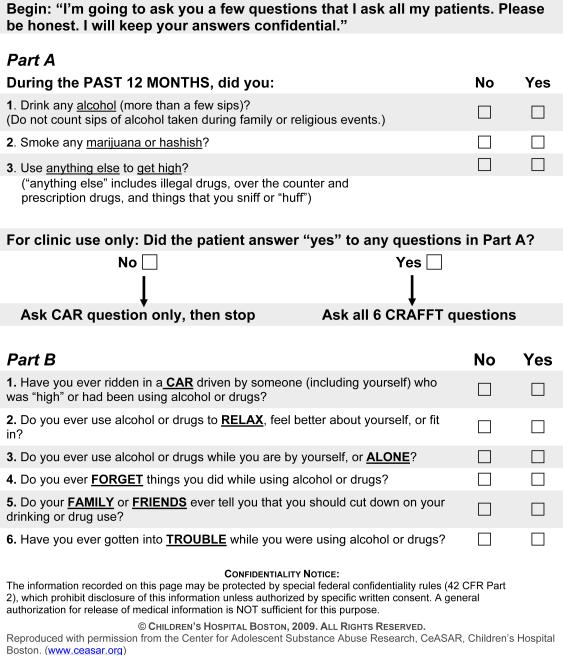
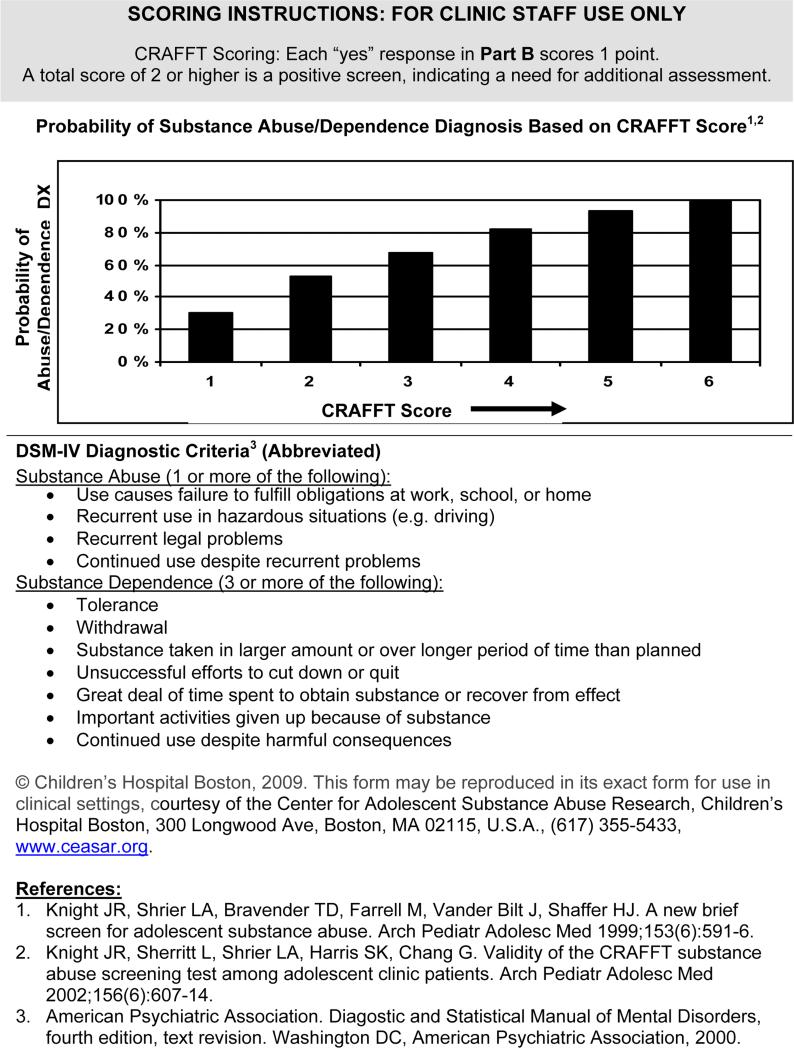
While many evidence-based office tools exist to assist clinicians in screening for substance use (reviewed in Burns et al., 2010 and Goodman and Wolff, 2013), including brief screens such as the T-ACE (Sokol et al., 1989) and TWEAK (Russell and Bigler, 1979) for use in pregnant women, among assessments we recommend use of the CRAFFT screening tool which was designed specifically for use in adolescents and has been validated in multiple community and hospital-based clinical contexts (Knight et al. 1999, 2002, 2003; Dhalla et al., 2011). It has also been effectively used to detect preconception substance use in a small cohort of pregnant women age 17 to 25 (Chang et al., 2011). Figure 1 outlines instructions, question item content, and scoring for the CRAFFT.
The CRAFFT Screening Interview
Advantages of the CRAFFT
The CRAFFT has several advantages:
Free public access
No training required
2-3 minutes to complete
Screens both alcohol and drug use simultaneously, with good positive and negative predictive probability for problem use, abuse, and dependence
74% sensitivity, 96% specificity
Computerized version validated and can be incorporated into other screening programs (Knight et al., 2007)
Available in many languages
Limitations of the CRAFFT
Limitations of the CRAFFT include:
Not a comprehensive assessment of substance use
Needs a separate screen for tobacco products, e-cigarettes, and “hookah” vaping; typically these are single-item questions about ever-use followed by quantification for positive screens (Chang et al., 2005; Stanton and Grimshaw, 2013; Palazzolo 2013; Barnett et al., 2013)
Requires knowledgeable interpretation for risk assessment
Not intended to measure treatment outcomes
Positive screens on the CRAFFT provide an opportunity for follow up conversations regarding substance use health risks, including risky sexual behavior and unplanned pregnancy. Separate screening for nicotine use is also recommended, especially as teenage cigarette smoking is associated with higher rates of co-occurring mental illness and substance abuse (Chang et al., 2005). While brief educational follow up may be helpful, educational content delivered within the context of a motivational enhancement session is likely to have more impact.
MOTIVATIONAL INTERVIEWING IN ADOLESCENTS
What is motivational interviewing (MI)?
Motivational interviewing (MI) is a client-centered, collaborative approach to eliciting and strengthening motivation for change, and evoking ideas and plans for changing behavior (Miller and Rollnick, 2012). MI is well-suited to working with clients who are difficult to engage in treatment (e.g., adolescents, substance users, and those with high-risk lifestyles) because it always engages the client from their position of autonomy and resourcefulness. The interventionist's primary tasks are twofold. First, to recognize and verbally reinforce “change talk” – statements oriented toward desire, ability, reason or need to change behavior – using empathic reflections that highlight “change talk” while ignoring other verbalizations associated with barriers to change, or “sustain talk” (commonly called “resistance” to change). Second, to assist the client in formulating plans, actions, and commitments to change drawing on the client's inherent resourcefulness and adding collaborative expertise and strategy when this is sought by the client. MI has a very strong evidence base for promoting change and is popular with clinicians because its spirit is compassionate and its emphasis on client responsibility reduces frustration and burn-out. MI does require training and practice to learn, and many opportunities for clinician training are provided through the MI Network of Trainers (MINT; www.motivationalinterviewing.org).
Does MI reduce substance use in adolescents?
There is ample evidence of MI's efficacy in reducing teen substance use. Barnett and colleagues (2012) reviewed the literature and cite 26 clinical trials of good quality with participants younger than 18 years showing at least modest effects on improving substance use outcomes, including alcohol, tobacco, and marijuana, the three most commonly used substances among preconception and pregnant teens. The number of MI sessions delivered ranged from one to more than three, and studies that included personalized feedback were no more effective than studies that did not include a feedback component. Individual MI sessions composed the majority of studies and the efficacy of MI in a group treatment setting remains uncertain. Where feedback was provided, in-person feedback was superior to computerized feedback, but in-person sessions did not appear to always be superior to telephone sessions. Involving parents as part of the delivered interventions (for instance, adding a component of addiction education for the parent) appears to support improved outcomes. More suggestive evidence is provided by a Cochrane review of 28 clinical trials targeting adolescent smoking cessation (Stanton and Grimshaw, 2013). The authors conclude that although current evidence does not yet support clear recommendations, the most promising studies, i.e., those demonstrating post-intervention abstinence at 30 days or 6 months continuous abstinence, incorporated a motivational interviewing or motivational enhancement intervention.
MI is a natural match for engaging adolescents because they are focused on developing autonomy and discovering their own capacities. When clinicians are adherent to the spirit of MI, adolescents are more welcoming of conversations related to risk reduction, self-efficacy development, and collaborative goal-setting. Practical applications and adaptations for adolescent treatment, including chapters on substance use and risky sexual behavior, is well-outlined in Naar-King and Suarez's textbook (2011).
Can MI reduce risk of unplanned teen pregnancy?
Only one randomized controlled clinical trial using computer-assisted MI as part of a home- and community-delivered intervention to prevent repeat pregnancy, conducted in a population of at-risk African-American adolescents, informs us about the potential benefit of MI in teens at high risk for unplanned pregnancy (Barnet et al., 2009). Paraprofessionals selected for their empathy and knowledge of participant culture and norms received 2.5 days of training and certification as MI interventionists followed by 4 months fidelity monitoring and feedback using audiotaped sessions. The MI intervention consisted of computer self-report on sexual behaviors and contraceptive use, and data resulted in assessment of contraceptive use stage of change and feedback on risk for pregnancy. The MI interventionists then conducted a 20-minute stage-matched MI session to enhance motivation for contraceptive use and avoiding pregnancy. At least 7 sessions had to be delivered, the first within 6 weeks postpartum, in order to count as a completed intervention. Results showed MI alone non-significantly reduced 24-month repeat pregnancy while MI + parent training/case management intervention significantly reduced pregnancy rates compared to office-based treatment as usual (p < .05). It is noted that the MI+ group was more adherent than the MI alone group, with sooner transition of phone contact to in-home visits; this may have affected outcomes.
Among adult women at risk for unplanned pregnancy due to risky drinking and high-risk for ineffective contraceptive use, two brief counseling interventions using MI plus personalized feedback, CHOICES (delivered as four 30-75 minute sessions) and BALANCE (an adaptation of CHOICES for a college sample of youth age 18-25, delivered as one 60 minute session), coupled with a medical contraception counseling appointment (in BALANCE, this was strongly encouraged but not delivered with the intervention) have been tested in randomized controlled trials (Ingersoll et al., 2003, 2005; Floyd et al., 2007; Ceperich and Ingersoll, 2011). Interventions in both studies were compared to an informational brochure to reduce risk of unplanned pregnancy by reviewing topics of fetal alcohol spectrum disorder, women's health and contraception, and mental health and substance use. Both of these MI-based interventions were superior to control for reducing risky drinking, improving contraception rates, and decreasing absolute risk of alcohol-exposed pregnancies (absolute risk reduction in CHOICES was 18% and BALANCE was 15%).
As a follow up, in an effort to adapt these treatments to better serve real-world practice and community samples, the authors examined the effect of one 60 minute MI session plus assessment feedback (EARLY) in a community sample of women at risk for unplanned pregnancy due to risky drinking and ineffective contraceptive behavior (Ingersoll et al., 2013). Informational videos (45 mins.) or brochure on relevant topic content were the two control comparisons. All interventions showed statistically significant, modest reductions in drinks per drinking day, ineffective contraception rates and alcohol-exposed pregnancies over a three month period, and EARLY was superior to the informational controls in reducing alcohol-exposed pregnancies at 3 months (absolute risk reduction 6.3% vs. video and 8.3% vs. brochure). Although the effects were smaller in magnitude when compared with multi-session CHOICES, this intervention provides an effective alternative when a more intensive intervention is not feasible. It should be noted that MI interventionists in this study had either Master's or Doctoral level training, completed extensive pre-study MI training and certification, and participated in weekly MI supervision including review of audiotaped sessions to insure protocol adherence and fidelity to MI intervention. This aspect of the study as it pertains to successful outcomes must not be overlooked when clinical settings are considering applications of this type of intervention; the need for high-quality training and longitudinal supervision in motivational interventions is a well-documented determinant of intervention efficacy (Martino et al., 2008|).
SUBSTANCE ABUSE TREATMENT PROGRAMS: ROLE IN REDUCING RISK FOR UNPLANNED PREGNANCY
Need for family planning services in substance abuse treatment programs
Women account for approximately 30–40% of patients attending substance use treatment programs, yet these programs do not routinely address women's’ reproductive health (Sherman et al., 2008). By integrating reproductive services into substance abuse treatment, patients have improved maternal health through facilitated access in a less threatening environment (Niccols et al., 2010).
Specific guidelines and policies are lacking in substance abuse treatment centers for family planning. Perhaps this is because of the fact that family planning implies intentional consideration of becoming (or not becoming) a mother, and women presenting to general substance use treatment centers are often in crisis and commonly suffering the acute symptoms of co-occurring mental illness, such as suicidal ideation, psychosis, severe anxiety and trauma-related disorders. Quality treatment typically includes screening for risky sexual behaviors and strategies to reduce such exposures in order to avoid STDs, becoming a victim of physical or sexual abuse, and unintended pregnancy. While health care referral options are made available if a woman discovers she is pregnant while in treatment, specific contraceptive counseling and family planning interventions are often absent or inadequately addressed, being deferred to the next referral point of care. Routine brief interventions focus on the health of the woman in treatment and may avoid discussion of the unintended effects of drugs and alcohol on her baby should she become pregnant and the impact of this on her own psychological health in the future. Since data suggest that substance-using pregnant teens and women effectively reduce alcohol and drug use in second and third trimesters, it may be that current treatment practice underestimates this valued incentive to change among the majority of substance-using women entering treatment programs. Additionally, the lack of equivalent reduction rates of tobacco use in later pregnancy may well reflect another problem needing to be addressed in substance abuse treatment: the need to correct clinician and client perceptions about tobacco use as a lethal drug use disorder and to provide relevant access to care and reimbursement schedules for evidence-based tobacco cessation treatments (Williams et al., 2013).
Pregnancy diagnosed in the context of substance abuse treatment
Women and teens with active substance use diagnosed with an unplanned pregnancy should be referred to an obstetrician for prenatal care and more intensive substance abuse counseling if the patient elects to continue her pregnancy. Comprehensive referrals are needed to adequately address the mental health risks of pregnant and parenting teen mothers, particularly high rates of depression (16-44%), stress and trauma-related disorders, and substance use (Hodgkinson et al., 2014).
Approximately half of unintended pregnancies in the United States are terminated by elective abortion (Finer and Henshaw, 2006), and studies report that resolution of an unintended pregnancy by induced abortion is associated with higher maternal rates of alcohol consumption, nicotine dependence, and illegal drug use (Reardon et al., 2004; Pedersen, 2007). Elective abortion among adolescents appears to be medically safe (Renner et al., 2013) but there is little data to guide clinicians on appropriate mental health monitoring post-abortion. Aftercare planning is therefore typically determined by client history and presenting risk factors. Conservative decision-making on monitoring frequency and anticipation of possible delayed mental health symptoms is warranted.
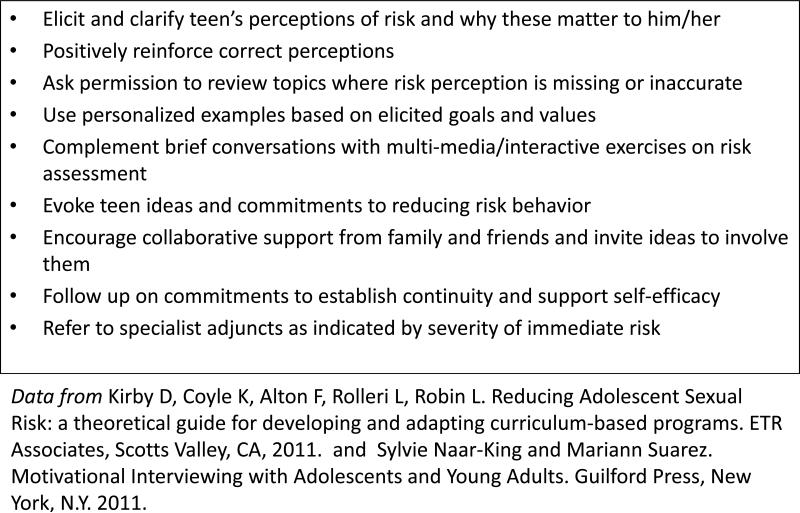
COMMON OPPORTUNITES TO REDUCE UNPLANNED TEEN PREGNANCY
According to 2011 CDC surveys, only 65% of teenage girls and 53% of teenage boys received formal sex education about both abstinence and birth control, and only 44% of teenage girls and 27% of teenage boys report having talked with their parents about abstinence and birth control. Clinicians may use motivational interviewing styles and strategies to effectively engage teens in conversation about sensitive topical content in order to optimally educate clients and to promote and support self-efficacy for behavioral risk reduction. These topics also provide opportunistic targets, with teen permission, for engaging family and friends in active support of healthy choices and behaviors. Figure 2 outlines recommended brief interventions consistent with motivational interviewing principles and practices that, based on the current evidence, we would consider “best practices” for reducing risk related to teen substance use, sexual behavior, and unintended pregnancy.
Figure 2.
Strategies to increase perceived risks of unplanned pregnancy and substance use
The CDC recommends that healthcare providers increase the availability of birth control to sexually active teens and offer teens long-acting reversible birth control such as IUDs or long-acting implants (CDC Vital Signs, 2011). Communities are asked to increase access to reproductive services and sex education that has been proven efficacious in preventing unintended pregnancy.
These recommendations are controversial with regard to religious and cultural freedoms and respect for family of origin preferences/beliefs; thus clinicians and communities experience important challenges in implementing interventions that would protect teens from unplanned pregnancy while remaining neutral and respectful of family and individual choices. Motivational interviewing, with its emphasis on autonomy, empathy, and clear comprehension of client goals and values, provides an evidence-supported tool for discussing sensitive public health recommendations while maintaining respect and professional neutrality.
For sexually active teens, barriers to optimal contraceptive use include access to healthcare providers, cost of contraception, concerns about confidentiality, negative attitudes about contraception, concerns about side effects, low self-efficacy, poor communication with partner, and partner resistance to contraception (Coles et al., 2011). The most commonly used and least expensive forms of contraception, oral contraceptives and condoms, have high failure rates due in large part to problems with adherence (Trussell et al., 2008; Blumenthal et al., 2010). Substance use further impairs proper adherence due to intoxication at time of use, forgetfulness, and lack of structure in lifestyle. Reduction of substance use is here considered an important target for contraceptive adherence, or for those not using contraceptives, for supporting self-efficacy in abstinence or limiting sexual activity to safe, committed partners with whom family planning has been fully addressed.
Increased use of long-acting methods that minimize risk of human error such as the intrauterine device (IUD) and hormone implants could play an important role in preventing pregnancy among substance users (Winner et al., 2012). The American Congress of Obstetricians and Gynecologists indicated that such methods should be “first-line” choices for young women, and coupling IUDs with condoms for additional protection may have the potential to reduce unintended pregnancy even further (ACOG, 2005; Finer and Zolna, 2011). One major barrier to using these longer term methods is the upfront out-of-pocket cost for uninsured or underinsured women despite the fact that they are significantly cost-effective over time. Economic modeling of the costs of unintended pregnancy using a third-party payer database demonstrated that 53% of unintended pregnancies were due to imperfect adherence with reversible contraceptive methods and that savings in the millions would be possible if even 10% of women in their twenties switched from oral contraceptives to longer-acting contraception (Trussell et al., 2013). As lower-income women have higher rates of unintended pregnancy resulting in childbirth (Finer and Zolna, 2013), providing financial access to health care options including family planning and pregnancy prevention, substance use treatment when indicated, and prenatal care are especially important in a population that is more difficult to engage in comprehensive health care.
KEY POINTS.
Unplanned pregnancy is a significant public health issue with rates being highest among adolescents. A main risk factor for unplanned pregnancy is alcohol and drug use.
Adolescents are poorly trained to anticipate and recognize unplanned pregnancy. Fetal exposure to substances and late prenatal care may occur for many continuing to childbirth.
It is recommended that primary care clinicians, including pediatricians and obstetrician-gynecologists, routinely screen adolescent patients for substance use.
It is recommended that substance abuse treatment centers incorporate contraception and family planning education into their comprehensive treatment programs.
Motivational interviewing effectively engages substance using adolescents in treatments to reduce substance use, and may also enhance pregnancy prevention in high-risk youth.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Finer LB, Zolna MR. Shifts in Intended and Unintended Pregnancies in the United States, 2001–2008. American Journal of Public Health. 2013 doi: 10.2105/AJPH.2013.301416. (e-View Ahead of Print. doi: 10.2105/AJPH.2013.301416) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. [1/18/2014];USHHS Healthy People. 2020 Topics: adolescent health http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=2.
- 3.Institute of Medicine . The Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. In: Brown Sarah S., Eisenberg Leon., editors. Committee on Unintended Pregnancy, Division of Health Promotion and Disease Prevention. National Academy Press; Washington, D.C.: 1995. [PubMed] [Google Scholar]
- 4.Baydar N. Consequences for children of their birth planning status. Fam Plann Perspect. 1995;27:228–245. [PubMed] [Google Scholar]
- 5.Naimi TS, Lipscomb LE, Brewer RD, Colley Gilbert B. Binge drinking in the preconception period and the risk of unintended pregnancy: Implications for women and their children. Pediatrics. 2003;111:1136. [PubMed] [Google Scholar]
- 6.Shapiro-Mendoza C, Selwyn BJ, Smith DP, Sanderson M. Parental pregnancy intention and early childhood stunting: Findings from Bolivia. Int. J. Epidemiol. 2005;34(2):387–396. doi: 10.1093/ije/dyh354. [DOI] [PubMed] [Google Scholar]
- 7.National Campaign to Prevent Teen and Unplanned Pregnancy [December 22, 2013];Counting It Up: The Public Costs of Teen Childbearing. 2011 from http://www.thenationalcampaign.org/costs/default.aspx.
- 8.Adolescent substance use: America's #1 public health problem. The National Center on Addiction and Substance Abuse at Columbia University; 2011. http://www.casacolumbia.org/upload/2011/20110629adolescentsubstanceuse.pdf. [Google Scholar]
- 9.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future: national results on drug use: 2012 Overview, Key Findings on Adolescent Drug Use. Institute for Social Research, The University of Michigan; Ann Arbor: 2013. [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration . Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. [Google Scholar]
- 11.CDC Youth risk behavior surveillance—United States, 2011. MMWR. 2012;61(SS-4) [PubMed] [Google Scholar]
- 12.Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013 May;131(5):886–91. doi: 10.1542/peds.2012-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heil SH, Jones HE, Arria A, Kaltenbach K, Coyle M, Fischer G, Stine S, Selby P, Martin PR. Unintended pregnancy in opioid-abusing women. J Subst Abuse Treat. 2011 Mar;40(2):199–202. doi: 10.1016/j.jsat.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Black KI, Stephens C, Haber PS, Lintzeris N. Unplanned pregnancy and contraceptive use in women attending drug treatment services. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2012;52:146–150. doi: 10.1111/j.1479-828X.2012.01413.x. [DOI] [PubMed] [Google Scholar]
- 15.Kotchick BA, Shaffer A, Miller KS, Forehand R. Adolescent sexual risk behavior: a multi-system perspective. Clinical Psychology Review. 2001;21(4):493–519. doi: 10.1016/s0272-7358(99)00070-7. [DOI] [PubMed] [Google Scholar]
- 16.Meade CS, Ickovics JR. Systematic review of sexual risk among pregnant and mothering teens in the USA: pregnancy as an opportunity for integrated prevention of STD and repeat pregnancy. Soc Sci Med. 2005 Feb;60(4):661–78. doi: 10.1016/j.socscimed.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 17.Martinez G, Copen CE, Abma JC. Vital Health Stat. 31. Vol. 23. National Center for Health Statistics; 2011. Teenagers in the United States: Sexual activity, contraceptive use, and childbearing, 2006–2010 National Survey of Family Growth. [PubMed] [Google Scholar]
- 18.Santelli JS, Robin L, Brener ND, Lowry R. Timing of alcohol and other drug use and sexual risk behaviors among unmarried adolescents and young adults. Family Planning Perspectives. 2001;33(5):200–205. [PubMed] [Google Scholar]
- 19.Behnke M, Smith VC. Committee on Substance Abuse; Committee on Fetus and Newborn. Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics. 2013 Mar;131(3):e1009–24. doi: 10.1542/peds.2012-3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burns E, Gray R, Smith LA. Brief screening questionnaires to identify problem drinking during pregnancy: a systematic review. Addiction. 2010 Apr;105(4):601–14. doi: 10.1111/j.1360-0443.2009.02842.x. [DOI] [PubMed] [Google Scholar]
- 21.Goodman DJ, Wolff KB. Screening for Substance Abuse in Women's Health: A Public Health Imperative. J Midwifery Womens Health. 2013;58:278–287. doi: 10.1111/jmwh.12035. [DOI] [PubMed] [Google Scholar]
- 22.Sokol RJ, Martier SS, Ager JW. The T-ACE questions: practical prenatal detection of risk-drinking. Am J Obstet Gynecol. 1989;160:863–8. doi: 10.1016/0002-9378(89)90302-5. discussion 868–70. [DOI] [PubMed] [Google Scholar]
- 23.Russell M, Bigler L. Screening for alcohol-related problems in an outpatient obstetric– gynecologic clinic. Am J Obstet Gynecol. 1979;134:4–12. doi: 10.1016/0002-9378(79)90787-7. [DOI] [PubMed] [Google Scholar]
- 24.Knight JR, et al. A new brief screen for adolescent substance abuse. Arch Pediatr Adolesc Med. 1999 Jun;153(6):591–6. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- 25.Knight JR, Sherritt L, Shrier LA, et al. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156:607–614. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 26.Knight JR, Sherritt L, Harris SK, et al. Validity of the brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcohol Clin Exp Res. 2003;27:67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- 27.Dhalla S, Zumbo BD, Poole G. A review of the psychometric properties of the CRAFFT instrument: 1999-2010. Curr Drug Abuse Rev. 2011 Mar 1;4(1):57–64. doi: 10.2174/1874473711104010057. [DOI] [PubMed] [Google Scholar]
- 28.Chang G, Orav EJ, Jones JA, Buynitsky T, Gonzalez S, Wilkins-Haug L. Self-reported alcohol and drug use in pregnant young women: a pilot study of associated factors and identification. J Addict Med. 2011 Sep;5(3):221–6. doi: 10.1097/ADM.0b013e318214360b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knight JR, Harris SK, Sherritt L, Van Hook S, Lawrence N, Brooks T, Carey P, Kossack R, Kulig J. Adolescents’ preference for substance abuse screening in primary care practice. Subst Abus. 2007;28(4):107–17. doi: 10.1300/J465v28n04_03. [DOI] [PubMed] [Google Scholar]
- 30.Chang G, Sherritt L, Knight JR. Adolescent cigarette smoking and mental health symptoms. J Adolesc Health. 2005 Jun;36(6):517–22. doi: 10.1016/j.jadohealth.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Stanton A, Grimshaw G. Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews. 2013 doi: 10.1002/14651858.CD003289.pub5. Issue 8. Art. No.: CD003289. [DOI] [PubMed] [Google Scholar]
- 32.Palazzolo DL. Electronic Cigarettes and Vaping: A New Challenge in Clinical Medicine and Public Health. A Literature Review. Front Public Health. 2013 Nov 18;1:56. doi: 10.3389/fpubh.2013.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barnett TE, Forrest JR, Porter L, Curbow BA. A Multiyear Assessment of Hookah Use Prevalence Among Florida High School Students. Nicotine Tob Res. 2013 Dec 17; doi: 10.1093/ntr/ntt188. [DOI] [PubMed] [Google Scholar]
- 34.Miller William R., Rollnick Stephen. Helping People Change. 3rd ed. Guilford Press; New York, N.Y.: 2012. Motivational Interviewing. [Google Scholar]
- 35.Barnett E, Sussman S, Smith C, Rohrbach LA, Spruijt-Metz D. Motivational Interviewing for adolescent substance use: A review of the literature. Addict Behav. 2012 Dec;37(12):1325–34. doi: 10.1016/j.addbeh.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naar-King Sylvie, Suarez Mariann. Motivational Interviewing with Adolescents and Young Adults. Guilford Press; New York, N.Y.: 2011. [Google Scholar]
- 37.Barnet B, Liu J, DeVoe M, Duggan AK, Gold MA, Pecukonis E. Motivational Intervention to Reduce Rapid Subsequent Births to Adolescent Mothers: Community-Based Randomized Trial. Ann Fam Med. 2009 Sep-Oct;7(5):436–45. doi: 10.1370/afm.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ingersoll K, Floyd L, Sobell M, Velasquez MM. Project CHOICES Intervention Research Group. Reducing the risk of alcohol-exposed pregnancies: A study of a motivational intervention in community settings. Pediatrics. 2003;111:1131–1135. [PubMed] [Google Scholar]
- 39.Ingersoll KS, Ceperich SD, Nettleman MD, Karanda K, Brocksen S, Johnson BA. Reducing alcohol-exposed pregnancy risk in college women: Initial outcomes of a clinical trial of a motivational intervention. Journal of Substance Abuse Treatment. 2005;29:173–180. doi: 10.1016/j.jsat.2005.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Floyd RL, Sobell M, Velasquez MM, Ingersoll K, Nettleman M, Sobell L, et al. Preventing alcohol-exposed pregnancies: A randomized controlled trial. American Journal of Preventive Medicine. 2007;32:1–10. doi: 10.1016/j.amepre.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ceperich SD, Ingersoll KS. Motivational interviewing + feedback intervention to reduce alcohol-exposed pregnancy risk among college binge drinkers: Determinants and patterns of response. Journal of Behavioral Medicine. 2011;34:381–395. doi: 10.1007/s10865-010-9308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ingersoll KS, Ceperich SD, Hettema JE, Farrell-Carnahan L, Penberthy JK. Preconception motivational interviewing interventions to reduce alcohol-exposed pregnancy risk. J Subst Abuse Treat. 2013 Apr;44(4):407–416. doi: 10.1016/j.jsat.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Community program therapist adherence and competence in motivational enhancement therapy. Drug Alcohol Depend. 2008 Jul 1;96(1-2):37–48. doi: 10.1016/j.drugalcdep.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sherman SG, Kamarulzaman A, Spittal P. Women and drugs across the globe: a call to action. Int J Drug Policy. 2008;19(2):97–98. doi: 10.1016/j.drugpo.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 45.Niccols A, Milligan K, Sword W, Thabane L, Henderson J, Smith A, Liu J, Jack S. Maternal mental health and integrated programs for mothers with substance abuse issues. Psychol Addict Behav. 2010;24:466–474. doi: 10.1037/a0020139. [DOI] [PubMed] [Google Scholar]
- 46.Williams JM, Willett JG, Miller G. Partnership between tobacco control programs and offices of mental health needed to reduce smoking rates in the United States. JAMA Psychiatry. 2013 Dec 1;70(12):1261–2. doi: 10.1001/jamapsychiatry.2013.2182. [DOI] [PubMed] [Google Scholar]
- 47.Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the Mental Health Needs of Pregnant and Parenting Adolescents. Pediatrics. 2014 Jan;133(1):114–22. doi: 10.1542/peds.2013-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on Sexual and Reproductive Health. 200638(2):90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 49.Reardon DC, Coleman PK, Cougle JR. Substance use associated with unintended pregnancy outcomes in the nationa longitudinal survey of youth. Amer Jour Drug Alc Abuse. 2004;30(2):369–383. doi: 10.1081/ada-120037383. [DOI] [PubMed] [Google Scholar]
- 50.Pedersen W. Childbirth, abortion and subsequent substance use in young women: a population-based longitudinal study. Addiction. 2007;102(12):1971–1978. doi: 10.1111/j.1360-0443.2007.02040.x. [DOI] [PubMed] [Google Scholar]
- 51.Renner RM, de Guzman A, Brahmi D. Abortion care for adolescent and young women. Int J Gynaecol Obstet. 2013 Oct 31; doi: 10.1016/j.ijgo.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 52.Kirby D, Coyle K, Alton F, Rolleri L, Robin L. Reducing Adolescent Sexual Risk: a theoretical guide for developing and adapting curriculum-based programs. ETR Associates; Scotts Valley, CA: 2011. Free access at http://pub.etr.org/upfiles/Reducing_Adolescent_Sexual_Risk.pdf. [Google Scholar]
- 53.CDC Vital Signs . Preventing teen pregnancy in the US. Centers for Disease Control; 2011. [October 5, 2013]. from http://www.cdc.gov/VitalSigns/pdf/2011-04-vitalsigns.pdf. [Google Scholar]
- 54.Coles MS, Makino KK, Stanwood NL. Contraceptive experiences among adolescents who experience unintended birth. Contraception. 2011;84(6):578–584. doi: 10.1016/j.contraception.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Trussell J, Wynn LL. Reducing unintended pregnancy in the United States. Contraception. 2008;77:1–5. doi: 10.1016/j.contraception.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 56.Blumenthal PD, Voedisch A, Gemzell-Danielsson K. Strategies to prevent unintended pregnancy: Increasing use of long-acting reversible contraception. Hum. Reprod. Update. 2011;17:121–137. doi: 10.1093/humupd/dmq026. [DOI] [PubMed] [Google Scholar]
- 57.Winner B, Peipert JF, Zhao Q, Buckel C, Madden T, Allsworth JE, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 58.ACOG Committee on Practice Bulletins Clinical management guidelines for obstetrician-gynecologists: intrauterine device. Obstet Gynecol. 2005;105:223–32. doi: 10.1097/00006250-200501000-00060. [DOI] [PubMed] [Google Scholar]
- 59.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478–485. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–161. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]