Abstract
Background:
Lower levels of circulating lipid fractions and cholesterol are risk factors for impulsivity and depressive disorder. A lower level of serum cholesterol is also associated with patients presenting with history of self-harm.
Materials and Methods:
A total of 30 depressive patients and 30 healthy matched control subjects were recruited from the department of Psychiatry of a tertiary care hospital. We measured serum total cholesterol (TC), low-density lipoprotein (LDL) and high-density lipoprotein cholesterol and triglyceride levels of both patient and control group.
Results:
The serum TC and LDL-cholesterol levels were found to be significantly lower in study group than that of control group.
Conclusion:
Lower levels of serum cholesterol are associated with depressive disorder.
Keywords: Body mass-index, depression, self-harm, serum cholesterol, serum lipid profiles, suicide
INTRODUCTION
Epidemiological and clinical intervention data indicate that low levels of circulating lipids and cholesterol are risk factors for depressive symptoms. An association of low cholesterol and an act of self-harm has also been described.[1,2] Previous studies show that, subjects treated for prevention of coronary artery disease with low levels of serum cholesterol have high mortality due to suicides, accidents and homicidal violence compared with control group.[3,4] However, two large population based study from Finland had findings contrary to that of above studies, i.e., subjects having high cholesterol were having depressive symptoms.[5,6] Low serum cholesterol was associated with low mood and increased risk of hospitalization due to depressive illness.[7,8] Total serum cholesterol has been highly significantly synchronized with the annual rhythms in violent suicide deaths. There were significant inverse time-relationships between the time series of violent suicide rate and L-tryptophan, total cholesterol (TC), CD4+/CD8+ T cell ratio and number of CD20+ B cells.[9] Men whose serum cholesterol concentration decreased by more than 0.13 mmol/l a year had multivariate adjusted relative risk of 2.17 for suicide compared with those whose cholesterol remained stable.[10] Other studies found no significant differences in lipid concentrations of triglyceride (TG), TC, high density lipoprotein (HDL), low density lipoprotein (LDL) among the depressed and non-depressed groups.[11,12] In a study on depressed patients in a psychiatric inpatient unit, no correlation was found between serum cholesterol levels and depression.[13] A 5 year intervention program aimed at reducing cholesterol levels reported improvement in hostility and depression scores in relation to dietary changes and lowering cholesterol.[14] Above findings, show that the relation between cholesterol and depression is complex, which requires further exploration. The above studies also suffered from methodological lacunae such as heterogeneity in sampling and lack of healthy matched (age and sex) control.
There are differences in metabolism between Indian and the Western population as Asian Indians compared with Caucasians have higher body fat, waist to hip ratio, intra-abdominal and subcutaneous fat while lesser average body mass-index (BMI), waist and hip circumference and muscle mass.[15] As there has been a paucity of Indian studies on this area a need was felt for a study to assess the serum cholesterol levels in patients of depression in Indian perspective. So this study was planned to study and compare serum lipid profiles in depressed subjects with that in normal controls.
We hypothesized that the serum cholesterol level is lower in patients with depression than that of healthy controls.
The aim of the present study was to determine serum TG, TC, HDL-cholesterol and LDL-cholesterol levels in Indian patients with depressive episode and healthy controls.
MATERIALS AND METHODS
Subjects
Thirty drug naive patients of age group 18-65 years, diagnosed as having depressive episode (first episode depression) by International classification of diseases, tenth revision, diagnostic criteria for research (ICD-10-DCR)[16] were included in this study from the Department of Psychiatry of a tertiary-care hospital in North-India (All India Institute of Medical Sciences, New Delhi). For this non-randomized and non-stratified sampling was performed. Thirty age and sex matched healthy control subjects were selected from non-blood relatives of patients. Informed consent was obtained prior to inclusion on the study and the subjects were explained in detail about the nature and purpose of the study. Clearance from institute ethics committee was taken.
The controls were of either sex, aged between 18 and 65 years, had no current psychiatric diagnosis, scored less than 2 on General Health Questionnaire (GHQ), receiving no psychotropic medication and had no alcohol or substance dependence disorder, other than nicotine.
The exclusion criteria for both subjects and controls were:
Current history of substance abuse (except nicotine), borderline personality disorder, psychosis or eating disorder.
Persons having known history of dyslipidemia.
Persons who are under any treatment or diet or having illness known to interfere with lipid metabolism.
Assessment
Diagnosis was made clinically by The ICD-10-DCR. Socio-demographic data and clinical details were recorded. The height and weight of the patient was measured. The BMI was calculated using the formula:
BMI = Weight/height2 (kg/m2)
Laboratory investigations
All the subjects and controls underwent estimation of their serum cholesterol, LDL and HDL cholesterol, serum TG levels. A fasting blood sample was taken in plain tube without anticoagulant for measurement of TC, HDL and TG by standard enzymatic method. The samples were stored at −70°C until analysis. Serum cholesterol was estimated by cholesterol oxidase method, TG by enzymatic hydrolysis and HDL cholesterol by phosphotungstate-magnesium chloride precipitation method. LDL cholesterol was calculated using Friedwald formula, i.e., LDL cholesterol = Serum TC − (TG/5 − HDL cholesterol).
Hamilton rating scale for depression (HRSD)
Depression was assessed through HRSD. It was originally published in 1960 by Max Hamilton and is presently one of the most commonly used scales for rating depression in medical research. It is a 21-question multiple choice questionnaire rated on 0-4 Likert scale used to rate the severity of depression.[17]
GHQ-12
The GHQ is a distress and well-being scale to measure psychological morbidity in normal population. The items were rated on a four point Likert Scale (0-3) of less than usual, no more than usual, more than usual and much more than usual. However, while computing the scores, each item is scored as 0 or 1 (0-0-1-1). Thus the total score varies from 0 to 12. A case score above 2 is considered as reflecting recognizable psychological problems. The Hindi version of GHQ-12 was standardized and was found to be quite sensitive, reliable and valid instrument for screening psychiatric patients.[18]
Statistics and ethical aspects
Data analysis was carried out using SPSS 15. Baseline data between two groups were compared with Chi-square test/Fisher's exact test for categorical variables. Serum lipid profiles were compared between two groups after adjusting for BMI. For this general linear model analysis of covariance test was applied. The correlation was calculated using Pearson correlation coefficient. The P values were two tailed and probability level for significant difference was set at P < 0.05.
RESULTS
Socio-demographic characteristics
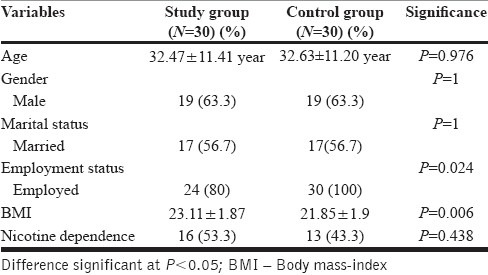
The mean age in study group was 32.47 ± 11.41 years while it was 32.63 ± 11.20 years for the control group. Males constituted 63.3% of the sample both in study as well as control group. There was no difference in age and sex distribution between study group and control group as the controls were selected as age and sex matched. Nearly 56.7% individuals of the sample were married and there was no difference in marital status between study group and control group. Twenty percent of the study sample were unemployed whereas all the controls were employed. There was significant difference in employment status between two groups (P = 0.024). The mean BMI in 30 subjects of patient group was 23.11 ± 1.87 kg/m2, while it was 21.85 ± 1.9 kg/m2 in control group. The difference in BMI between two groups was significant (P = 0.006). The socio-demographic variables have been shown in Table 1.
Table 1.
Socio-demographic and other variables
Clinical variables of patients
The duration of illness in patient group ranged from 20 days to 2 years with a mean of 4.97 ± 4.67 months. The minimum HRSD score was 10 and the maximum score was 27 with a mean of 18.43 ± 3.96. In the study group, there were 6 patients of mild depression, 20 of moderate and 4 patients of severe depression.
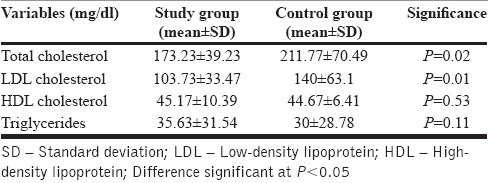
Serum lipid profiles
The mean LDL cholesterol of 30 patients in study group was 103.73 ± 33.47 mg/dl while it was 140 ± 63.1 mg/dl for 30 subjects of group. The mean HDL cholesterol of 30 subjects in study group was 45.17 ± 10.39 mg/dl while it was 44.67 ± 6.41 mg/dl for 30 subjects of control group. The mean TC of 30 subjects in study group was 173.23 ± 39.23 mg/dl while it was 211.77 ± 70.49 mg/dl for 30 subjects of control group. There was no co-relation between serum cholesterol level and severity of depression (P = 0.641).
To eliminate BMI as a confounding factor, serum lipid profiles between cases and controls were compared by adjusting BMI. After that the results are as follows.
The TC and LDL cholesterol levels were significantly low in the study group than the control group. There was no significance difference in HDL cholesterol and TG levels between study group and control group.
The serum lipid profile values of cases and controls have been shown in Table 2.
Table 2.
Comparison of serum lipid profiles between study and control group
DISCUSSION
In our study, when serum TC and LDL cholesterol levels were compared between study group and control group after adjusting for BMI, the levels were found to be significantly lower in study group than control group. This was in keeping with the earlier literature.[7,19,20]
The cholesterol-serotonin hypothesis was initially proposed to explain the link between low cholesterol levels and depression. This hypothesis states that reduction of serum TC may decrease brain cell membrane cholesterol and thereby lowering microviscosity of the cell membrane and subsequently decreasing the exposure of protein serotonin receptor on the membrane surface resulting in poorer uptake of serotonin from blood and less serotonin into brain cells leading to depression.[3] This hypothesis was also testified in Juvenile cynomolgus monkeys. Monkeys that consumed a low-cholesterol diet were more aggressive and had lower cerebrospinal fluid concentrations of 5-hydroxyindoleacetic acid (HIAA) (a measure of brain serotonergic activity) than did their high cholesterol counterparts.[21] However, again studies show contradictory findings. Hibbeln et al., 2000[22] did not find significant co relation between plasma cholesterol levels and 5-HIAA. In view of this finding, they proposed that omega-3 fatty acids may play a role.
An alternative view states that brain serotonin is synthesized from tryptophan in the brain and not sequestered from the blood. It has been hypothesized that the association between low cholesterol levels and violent deaths may be a risk at the initial stage of cholesterol-lowering treatment, which may occur if the treatment is introduced too rapidly or it occurs only in the presence of extremely lowered levels.[23] Maes et al.[24] did not find any significant differences in total or free cholesterol concentrations between depressive patients, their relatives and normal controls. However, depressed subjects and relatives of depressed subjects had a significantly lower esterified cholesterol ratio than normal controls. So they hypothesized that lower esterification in serum cholesterol may constitute a vulnerability factor for depression through alterations in cell membrane microviscosity.
Low serum cholesterol in depression could be a consequence of depression because of their poor health and decreased food intake. And also treating depression has been shown to increase serum cholesterol concentration.[25] Papakostas et al.[26] have proposed that both elevated and low cholesterol levels may be associated with serotonergic dysfunction. The positive correlation between depression and coronary artery disease is well-established. There is evidence of hypothalamo-pituitary-adrenal axis hyperactivity in depression, which can cause hypercortisolemia, which further can induce hypercholesterolemia and hypertension and thereby increasing the risk for coronary heart disease.[27] So as per result of our study, i.e. low cholesterol is associated with depression, it would be difficult to interpret the relation between depression and coronary heart disease. However, studies have also shown that subjects having high cholesterol were having depressive symptoms.[5,6] These two studies were population based studies having large sample size.[5,6]
In our study, there was no significant difference in HDL cholesterol between study group and control group even after adjusting for BMI. This differs from earlier studies, which had shown that serum HDL cholesterol was significantly lower in subjects with major depression than normal controls.[28,29]
The possible explanation could be as follows:
In the study by Maes et al.,[28] out of 36 patients they recruited, 28 were treatment resistant. After admission, the patients were kept drug free for a wash out period of 10 days. In our study, the patients taken were either drug naïve or on same psychotropics for last 6 weeks. In our patient group none of patients were found to be treatment resistant on detailed clinical assessment. In the study by Lehto et al.,[29] the study population had a long history of 7-year of depressive symptoms, which is much more than that of our study population, which had only a brief duration of depressive illness (mean = 4.97 months). In a recent study by Lehto et al.[30] shows that, major depressive disorder (MDD) subjects with a long symptom duration (≥3 years) had lower levels of HDL-C compared with healthy controls or MDD subjects with a symptom duration <3 years. Another study by Zhang et al.[31] had found a lower HDL cholesterol level to be significantly correlated with suicidal attempts. However, in our study sample there was no history of suicidal attempt in any patient. One recent study shows, the dissimilarities in HDL cholesterol level between current MDD versus remitted MDD and controls lost statistical significance when adjusted for possible confounding factors especially BMI.[32]
There were no significant differences in serum TG between cases and control group, which is in line with earlier literature.[11] However, the study by Lindberg et al., 1992[33] found that the serum TG value was lower in those who reported depressive symptoms during the past 6 months in women, but not in men. In this study, they included subjects with self-reported depressive symptoms, not the syndromal diagnosis of MDD. There are some limitations of our study. Tobacco dependency was not excluded. No investigations were carried out to rule out medical illness. Family, history of depression and family history of illness having effect on lipid profiles, which could confound the result, were not assessed.
This work is an attempt to correlate the relation between serum cholesterol and depressive disorder. There are also wide variations in the results of the earlier studies. The above discussion shows that there is a need for more studies on this subject taking representative sample of depressive illness in the community taking care of all the variables and preferably in a totally drug naïve patient group. This has also implications in treatment of hypercholesterolemia and coronary artery diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Olié E, Picot MC, Guillaume S, Abbar M, Courtet P. Measurement of total serum cholesterol in the evaluation of suicidal risk. J Affect Disord. 2011;133:234–8. doi: 10.1016/j.jad.2011.03.028. [DOI] [PubMed] [Google Scholar]
- 2.Garland M, Hickey D, Corvin A, Golden J, Fitzpatrick P, Cunningham S, et al. Total serum cholesterol in relation to psychological correlates in parasuicide. Br J Psychiatry. 2000;177:77–83. doi: 10.1192/bjp.177.1.77. [DOI] [PubMed] [Google Scholar]
- 3.Engelberg H. Low serum cholesterol and suicide. Lancet. 1992;339:727–9. doi: 10.1016/0140-6736(92)90609-7. [DOI] [PubMed] [Google Scholar]
- 4.Muldoon MF, Manuck SB, Matthews KA. Lowering cholesterol concentrations and mortality: A quantitative review of primary prevention trials. BMJ. 1990;301:309–14. doi: 10.1136/bmj.301.6747.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pekkanen J, Nissinen A, Punsar S, Karvonen MJ. Serum cholesterol and risk of accidental or violent death in a 25-year follow-up. The Finnish cohorts of the seven countries study. Arch Intern Med. 1989;149:1589–91. [PubMed] [Google Scholar]
- 6.Tanskanen A, Vartiainen E, Tuomilehto J, Viinamäki H, Lehtonen J, Puska P. High serum cholesterol and risk of suicide. Am J Psychiatry. 2000;157:648–50. doi: 10.1176/appi.ajp.157.4.648. [DOI] [PubMed] [Google Scholar]
- 7.Partonen T, Haukka J, Virtamo J, Taylor PR, Lönnqvist J. Association of low serum total cholesterol with major depression and suicide. Br J Psychiatry. 1999;175:259–62. doi: 10.1192/bjp.175.3.259. [DOI] [PubMed] [Google Scholar]
- 8.Morgan RE, Palinkas LA, Barrett-Connor EL, Wingard DL. Plasma cholesterol and depressive symptoms in older men. Lancet. 1993;341:75–9. doi: 10.1016/0140-6736(93)92556-9. [DOI] [PubMed] [Google Scholar]
- 9.Maes M, Scharpé S, D’Hondt P, Peeters D, Wauters A, Neels H, et al. Biochemical, metabolic and immune correlates of seasonal variation in violent suicide: A chronoepidemiologic study. Eur Psychiatry. 1996;11:21–33. doi: 10.1016/0924-9338(96)80455-X. [DOI] [PubMed] [Google Scholar]
- 10.Zureik M, Courbon D, Ducimetière P. Serum cholesterol concentration and death from suicide in men: Paris prospective study I. BMJ. 1996;313:649–51. doi: 10.1136/bmj.313.7058.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen CC, Huang TL. Association of serum lipid profiles with depressive and anxiety disorders in menopausal women. Chang Gung Med J. 2006;29:325–30. [PubMed] [Google Scholar]
- 12.Huang TL. Serum lipid profiles in major depression with clinical subtypes, suicide attempts and episodes. J Affect Disord. 2005;86:75–9. doi: 10.1016/j.jad.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 13.Apter A, Laufer N, Bar-Sever M, Har-Even D, Ofek H, Weizman A. Serum cholesterol, suicidal tendencies, impulsivity, aggression, and depression in adolescent psychiatric inpatients. Biol Psychiatry. 1999;46:532–41. doi: 10.1016/s0006-3223(98)00345-x. [DOI] [PubMed] [Google Scholar]
- 14.Weidner G, Connor SL, Hollis JF, Connor WE. Improvements in hostility and depression in relation to dietary change and cholesterol lowering. The family heart study. Ann Intern Med. 1992;117:820–3. doi: 10.7326/0003-4819-117-10-820. [DOI] [PubMed] [Google Scholar]
- 15.Banerji MA, Faridi N, Atluri R, Chaiken RL, Lebovitz HE. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84:137–44. doi: 10.1210/jcem.84.1.5371. [DOI] [PubMed] [Google Scholar]
- 16.Geneva: World Health Organisation; 1993. World Health Organisation. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. [Google Scholar]
- 17.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gautam S, Nijhawan M, Kamal P. Standardisation of Hindi version of Goldberg's general health questionnaire. Indian J Psychiatry. 1987;29:63–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Rabe-Jab³on´ska J, Poprawska I. Levels of serum total cholesterol and LDL-cholesterol in patients with major depression in acute period and remission. Med Sci Monit. 2000;6:539–47. [PubMed] [Google Scholar]
- 20.Jow GM, Yang TT, Chen CL. Leptin and cholesterol levels are low in major depressive disorder, but high in schizophrenia. J Affect Disord. 2006;90:21–7. doi: 10.1016/j.jad.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan JR, Shively CA, Fontenot MB, Morgan TM, Howell SM, Manuck SB, et al. Demonstration of an association among dietary cholesterol, central serotonergic activity, and social behavior in monkeys. Psychosom Med. 1994;56:479–84. doi: 10.1097/00006842-199411000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Hibbeln JR, Umhau JC, George DT, Shoaf SE, Linnoila M, Salem N., Jr Plasma total cholesterol concentrations do not predict cerebrospinal fluid neurotransmitter metabolites: Implications for the biophysical role of highly unsaturated fatty acids. Am J Clin Nutr. 2000;71:331S–8. doi: 10.1093/ajcn/71.1.331S. [DOI] [PubMed] [Google Scholar]
- 23.Manfredini R, Caracciolo S, Salmi R, Boari B, Tomelli A, Gallerani M. The association of low serum cholesterol with depression and suicidal behaviours: New hypotheses for the missing link. J Int Med Res. 2000;28:247–57. doi: 10.1177/147323000002800601. [DOI] [PubMed] [Google Scholar]
- 24.Maes M, Delanghe J, Meltzer HY, Scharpé S, D’Hondt P, Cosyns P. Lower degree of esterification of serum cholesterol in depression: Relevance for depression and suicide research. Acta Psychiatr Scand. 1994;90:252–8. doi: 10.1111/j.1600-0447.1994.tb01589.x. [DOI] [PubMed] [Google Scholar]
- 25.Law M. Having too much evidence (depression, suicide, and low serum cholesterol) BMJ. 1996;313:651–2. doi: 10.1136/bmj.313.7058.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Papakostas GI, Ongür D, Iosifescu DV, Mischoulon D, Fava M. Cholesterol in mood and anxiety disorders: Review of the literature and new hypotheses. Eur Neuropsychopharmacol. 2004;14:135–42. doi: 10.1016/S0924-977X(03)00099-3. [DOI] [PubMed] [Google Scholar]
- 27.Raadsheer FC, Hoogendijk WJ, Stam FC, Tilders FJ, Swaab DF. Increased numbers of corticotropin-releasing hormone expressing neurons in the hypothalamic paraventricular nucleus of depressed patients. Neuroendocrinology. 1994;60:436–44. doi: 10.1159/000126778. [DOI] [PubMed] [Google Scholar]
- 28.Maes M, Smith R, Christophe A, Vandoolaeghe E, Van Gastel A, Neels H, et al. Lower serum high-density lipoprotein cholesterol (HDL-C) in major depression and in depressed men with serious suicidal attempts: Relationship with immune-inflammatory markers. Acta Psychiatr Scand. 1997;95:212–21. doi: 10.1111/j.1600-0447.1997.tb09622.x. [DOI] [PubMed] [Google Scholar]
- 29.Lehto SM, Hintikka J, Niskanen L, Tolmunen T, Koivumaa-Honkanen H, Honkalampi K, et al. Low HDL cholesterol associates with major depression in a sample with a 7-year history of depressive symptoms. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1557–61. doi: 10.1016/j.pnpbp.2008.05.021. [DOI] [PubMed] [Google Scholar]
- 30.Lehto SM, Niskanen L, Tolmunen T, Hintikka J, Viinamäki H, Heiskanen T, et al. Low serum HDL-cholesterol levels are associated with long symptom duration in patients with major depressive disorder. Psychiatry Clin Neurosci. 2010;64:279–83. doi: 10.1111/j.1440-1819.2010.02079.x. [DOI] [PubMed] [Google Scholar]
- 31.Zhang J, McKeown RE, Hussey JR, Thompson SJ, Woods JR, Ainsworth BE. Low HDL cholesterol is associated with suicide attempt among young healthy women: The third national health and nutrition examination survey. J Affect Disord. 2005;89:25–33. doi: 10.1016/j.jad.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 32.van Reedt Dortland AK, Giltay EJ, van Veen T, van Pelt J, Zitman FG, Penninx BW. Associations between serum lipids and major depressive disorder: Results from the Netherlands study of depression and anxiety (NESDA) J Clin Psychiatry. 2010;71:729–36. doi: 10.4088/JCP.08m04865blu. [DOI] [PubMed] [Google Scholar]
- 33.Lindberg G, Råstam L, Gullberg B, Eklund GA. Low serum cholesterol concentration and short term mortality from injuries in men and women. BMJ. 1992;305:277–9. doi: 10.1136/bmj.305.6848.277. [DOI] [PMC free article] [PubMed] [Google Scholar]


