Abstract
Objectives:
This study attempted to follow up a cohort of women who presented to a tertiary hospital to investigate the effect of domestic violence on maternal and neonatal outcomes.
Materials and Methods:
Women, between 26-34 weeks of gestation, attending the obstetrics outpatient department, were recruited and followed up until delivery. They were assessed at recruitment and after delivery using the Edinburgh Postnatal Depression Scale, the Abuse Assessment Screen, and a pro forma to assess socio-demographic and clinical characteristics. Bivariate and multivariate statistics were employed to assess statistical significance.
Results:
One hundred and fifty women were recruited, 132 delivered in the hospital and were followed up. Domestic violence was associated with antenatal and postnatal depression, spouse's insistence of a boy baby, medical complications during pregnancy, preterm delivery, and lower birth-weight.
Conclusion:
Domestic violence has a significant impact on maternal and neonatal outcomes. Screening for domestic violence and interventions should be part of all antenatal programs. India should also employ public health approaches to change its patriarchal culture.
Keywords: Cohort design, domestic violence, India, maternal and neonatal outcomes
INTRODUCTION
Domestic violence, a global problem, is also a significant public health concern in India. Studies from India have documented high rates of such violence.[1,2,3,4] Studies analyzing results from the National Family Health Survey -3 have documented a rate of 39.6%.[5] In addition, to being a human rights concern, domestic violence is also been linked to adverse health outcome including termination of pregnancy,[5] sexually transmitted infections, attempted suicide,[6] HIV infection,[7] depression, and anxiety.[8] Violence has also been recorded during pregnancy[9] and is associated with preterm births[10] and low birth weight infants.[11] This study attempted to investigate the effects of domestic violence on maternal and neonatal outcomes during pregnancy and delivery.
MATERIALS AND METHODS
Study design and setting
The study employed a prospective cohort design. Pregnant women attending the obstetrics outpatient department were recruited and followed up until delivery.
Participants
Women, between 26-34 weeks of gestation, who were planning to deliver in the institution, were recruited for the study. The details of the study were explained, and written informed consent was obtained. The study protocol was cleared by the Institutional Review Board.
Data collection
The following instruments were administered:
A pro forma to collect socio-demographic and clinical characteristics,
Edinburgh Postnatal Depression Scale (EPDS):[12] The scale is a commonly employed instrument to assess peri-natal depression. It is a 10-item screen, which is easy to administer and score. It has been employed in many cultures and settings. It has been used in India, and the Tamil version has been employed at Vellore,[13]
Abuse Assessment Screen (AAS):[14,15] This instrument has been commonly employed to assess intimate partner violence in clinical and research settings. It has been used in many countries including India. Privacy and confidentiality was ensured.
Follow-up
The women were followed up until delivery. The following instruments were employed to assess clinical outcome:
A pro forma to collect maternal and neonatal outcomes,
Edinburgh Postnatal Depression Scale,
Abuse Assessment Screen.
Bias
The exposure and outcomes were measured by different physicians. While the exposure was collected by RN, the maternal and neonatal outcomes were documented by the attending physicians and subsequently transcribed from the patient medical records.
Statistics
Descriptive statistics were used to describe continuous variables while frequency distributions were obtained for categorical variables. Mann-Whitney U test was used to assess the significance of continuous variables while the chi-squared test was employed for categorical data. Multivariate analysis, using multiple linear and logistic regressions, was employed to adjust for the effect of maternal age. Subjects lost to follow-up were compared to those who delivery at the hospital in order to assess for participation bias. The sample size was calculated (n = 126) using the computer program Epi-Info version 6 using the value of domestic violence taken as 20%[2] and a precision of 7%.
RESULTS
One hundred and fifty women were recruited for the study. The majority were young women (mean 26.32 years, SD 4.22), literate (100%), housewives (86.7%), primigravidae (59.3%), lived in joint families (73.7%), from middle class backgrounds (mean income Rupees 9000 per month, SD 8252) and were married for a few years (mean 3.11, SD 3.28). Their spouses were a few years older (mean 31.55, SD 3.40) and were literate (100%) and employed (100%). Eleven (7.3%) women reported a history of domestic violence. One hundred and thirty-two (88.0%) were followed up to delivery. There were no statistically significant difference between women who were lost to follow up and those who were followed up till delivery on the following variables: Age, education, occupation, type of family, debt, spouse's age, education, occupation, income, gestation at recruitment, antenatal depression scores, and history of domestic violence.
The proportion of women who had vaginal, instrumental, and cesarean deliveries was 51.5%, 12.9%, and 35.6%, respectively. Sixty-seven babies (50.8%) delivered were boys. The mean APGAR scores at 1 and 5 minutes were 8.86 (SD 0.88) and 9.48 (SD 0.97), respectively. The mean birth weight was 2.886 Kg (SD 0.516).
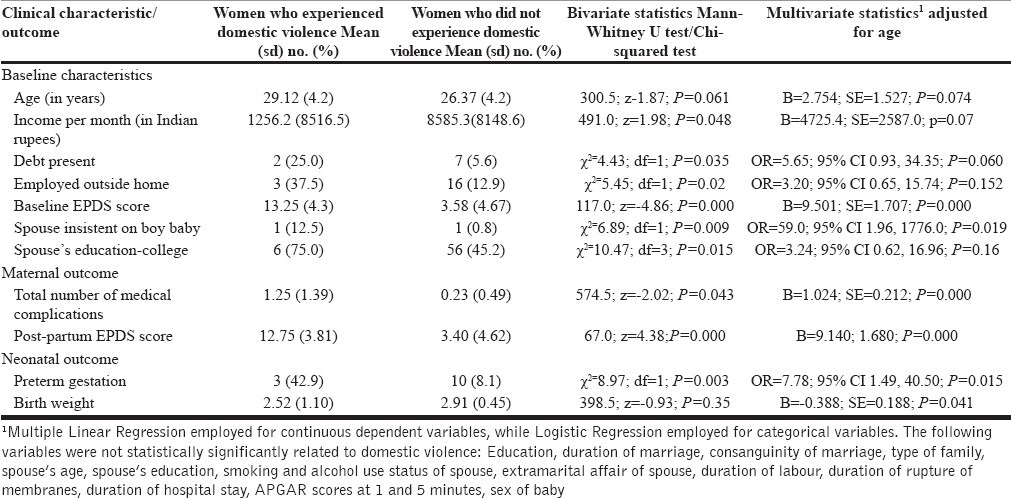
Table 1 documents the characteristics significantly associated with domestic violence. Domestic violence was associated with spouse's desire for a boy baby, complications of pregnancy, maternal antenatal and postnatal depression, preterm delivery, and lower birth weight after adjusting for age using multivariate statistics.
Table 1.
Comparison of clinical outcomes between mothers who did and did not experience domestic violence
DISCUSSION
While there is much data from India on domestic/intimate partner violence and it impact on the mother, there is a dearth of data on its impact on pregnancy, delivery, and neonatal outcomes. The strengths of this study are its prospective cohort design, independent assessments of exposure and clinical outcomes, a good follow up, and the use of multivariate statistics. Its limitations include the fact that its sample and the proportion of women reporting violence was relatively small.
The study confirmed the findings of investigations, which have confirmed a significant association between domestic violence and maternal and pregnancy-related outcomes (e.g. maternal depression).[6,8] It also supported evidence that gender-based violence was associated with the patriarchal preference for boy babies.[13] The findings also argued that such violence impact on neonatal outcomes (e.g. preterm births and lower birth weights).[10,11]
This study adds to the evidence that domestic violence is a significant maternal, child health, and public health issue, which has a significant impact on maternal and neonatal outcomes. It mandates routine screening during the antenatal period and calls for effective clinical interventions for prevention. It also argues for social strategies to change the patriarchal culture and public health approaches to bring about such change in Indian society.
ACKNOWLEDGMENT
The study was funded by a grant from the Christian Medical College, Vellore.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Rocca CH, Rathod S, Falle T, Pande RP, Krishnan S. Challenging assumptions about women's empowerment: Social and economic resources and domestic violence among young married women in urban South India. Int J Epidemiol. 2009;38:577–85. doi: 10.1093/ije/dyn226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stephenson R, Koenig MA, Acharya R, Roy TK. Domestic violence, contraceptive use, and unwanted pregnancy in rural India. Stud Fam Plann. 2008;39:177–86. doi: 10.1111/j.1728-4465.2008.165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koenig MA, Stephenson R, Ahmed S, Jejeebhoy SJ, Campbell J. Individual and contextual determinants of domestic violence in North India. Am J Public Health. 2006;96:132–8. doi: 10.2105/AJPH.2004.050872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeyaseelan L, Kumar S, Neelakantan N, Peedicayil A, Pillai R, Duvvury N. Physical spousal violence against women in India: Some risk factors. J Biosoc Sci. 2007;39:657–70. doi: 10.1017/S0021932007001836. [DOI] [PubMed] [Google Scholar]
- 5.Yoshikawa K, Agrawal NR, Poudel KC, Jimba M. A lifetime experience of violence and adverse reproductive outcomes: Findings from population surveys in India. Biosci Trends. 2012;6:115–21. doi: 10.5582/bst.2012.v6.3.115. [DOI] [PubMed] [Google Scholar]
- 6.Chowdhary N, Patel V. The effect of spousal violence on women's health: Findings from the Stree Arogya Shodh in Goa, India. J Postgrad Med. 2008;54:306–12. doi: 10.4103/0022-3859.43514. [DOI] [PubMed] [Google Scholar]
- 7.Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. JAMA. 2008;300:703–10. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- 8.Patel V, Kirkwood BR, Pednekar S, Pereira B, Barros P, Fernandes J, et al. Gender disadvantage and reproductive health risk factors for common mental disorders in women: A community survey inIndia. Arch Gen Psychiatry. 2006;63:404–13. doi: 10.1001/archpsyc.63.4.404. [DOI] [PubMed] [Google Scholar]
- 9.Peedicayil A, Sadowski LS, Jeyaseelan L, Shankar V, Jain D, Suresh S, et al. India SAFE Group. Spousal physical violence against women during pregnancy. BJOG. 2004;111:682–7. doi: 10.1111/j.1471-0528.2004.00151.x. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues T, Rocha L, Barros H. Physical abuse during pregnancy and preterm delivery. Am J Obstet Gynecol. 2008;198:171.e1–6. doi: 10.1016/j.ajog.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Sharps PW, Laughon K, Giangrande SK. Intimate partner violence and the childbearing year: Maternal and infant health consequences. Trauma Violence Abuse. 2007;8:105–16. doi: 10.1177/1524838007302594. [DOI] [PubMed] [Google Scholar]
- 12.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 13.Chandran M, Tharyan P, Muliyil J, Abraham S. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br J Psychiatry. 2002;181:499–504. doi: 10.1192/bjp.181.6.499. [DOI] [PubMed] [Google Scholar]
- 14.McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA. 1992;267:3176–8. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- 15.Laughon K, Renker P, Glass N, Parker B. Revision of the Abuse Assessment Screen to address nonlethal strangulation. J Obstet Gynecol Neonatal Nurs. 2008;37:502–7. doi: 10.1111/j.1552-6909.2008.00268.x. [DOI] [PubMed] [Google Scholar]


