Abstract
Background
Harmful medication errors, or preventable adverse drug events (ADEs), are a prominent quality and cost issue in healthcare. Injectable medications are important therapeutic agents, but they are associated with a greater potential for serious harm than oral medications. The national burden of preventable ADEs associated with inpatient injectable medications and the associated medical professional liability (MPL) costs have not been previously described in the literature.
Objective
To quantify the economic burden of preventable ADEs related to inpatient injectable medications in the United States.
Methods
Medical error data (MedMarx 2009–2011) were utilized to derive the distribution of errors by injectable medication types. Hospital data (Premier 2010–2011) identified the numbers and the types of injections per hospitalization. US payer claims (2009–2010 MarketScan Commercial and Medicare 5% Sample) were used to calculate the incremental cost of ADEs by payer and by diagnosis-related group (DRG). The incremental cost of ADEs was defined as inclusive of the time of inpatient admission and the following 4 months. Actuarial calculations, assumptions based on published literature, and DRG proportions from 17 state discharge databases were used to derive the probability of preventable ADEs per hospitalization and their annual costs. MPL costs were assessed from state- and national-level industry reports, premium rates, and from closed claims databases between 1990 and 2011. The 2010 American Hospital Association database was used for hospital-level statistics. All costs were adjusted to 2013 dollars.
Results
Based on this medication-level analysis of reported harmful errors and the frequency of inpatient administrations with actuarial projections, we estimate that preventable ADEs associated with injectable medications impact 1.2 million hospitalizations annually. Using a matched cohort analysis of healthcare claims as a basis for evaluating incremental costs, we estimate that inpatient preventable ADEs associated with injectable medications increase the annual US payer costs by $2.7 billion to $5.1 billion, averaging $600,000 in extra costs per hospital. Across categories of injectable drugs, insulin had the highest risk per administration for a preventable ADE, although errors in the higher-volume categories of anti-infective, narcotic/analgesic, anticoagulant/thrombolytic and anxiolytic/sedative injectable medications harmed more patients. Our analysis of liability claims estimates that MPL associated with injectable medications totals $300 million to $610 million annually, with an average cost of $72,000 per US hospital.
Conclusion
The incremental healthcare and MPL costs of preventable ADEs resulting from inpatient injectable medications are substantial. The data in this study strongly support the clinical and business cases of investing in efforts to prevent errors related to injectable medications.
Preventable medication errors have emerged as a prominent cost and quality issue in the United States, and are estimated to impact more than 7 million patients, contribute to 7000 deaths, and cost almost $21 billion in direct medical costs across all care settings annually.1,2 Adverse drug events (ADEs) are harms that result from medication use; when these harms result from a medication error, they are known as “preventable ADEs.”3 The inpatient hospital setting is particularly resource-intensive in terms of care delivered and exposure to potential harms and errors.4,5 In 2007, the Institute of Medicine (IOM) estimated that 1 medication error occurred per patient per day in hospital care.4 In 2008, the US Department of Health and Human Services (HHS) estimated that approximately 1 of every 7 (13.5%) hospitalized Medicare patients experienced permanent harm from a medical error, and that 37% of these inpatient injuries were associated with medications.5 In addition, the study investigators estimated that 50% of these ADEs were preventable.5
The majority of hospitalized patients receive medications, which means that a high volume of doses are prescribed and are administered daily in the inpatient setting. A study in a 735-bed academic medical center estimated that approximately 16,000 medication doses were administered daily.6 This study and others report that up to 1 of 5 medication doses are associated with an error, and that between 3% and 7% of these errors are potentially harmful to patients.6,7
Furthermore, many of the medications used in the inpatient setting are delivered by injectable routes; these injectable medications have among the highest risk for error and the most severe harms.8 In a study of inpatient ADEs, including life-threatening ADEs, 50% of the medications that were implicated were injectable, including antihypertensives, insulin, and anticoagulants.9 Similarly, studies in the inpatient intensive care unit setting, where medications delivered by infusion are common, have reported that a patient's risk for a medication error is approximately 10%, with 1 in 100 errors causing harm that requires life-saving treatment.8,10
In addition to the clinical harms caused by preventable ADEs, healthcare stakeholders incur the economic consequences as well. When a patient experiences a preventable ADE, there may be direct medical costs to payers, such as an extended inpatient stay, use of additional medications, and physician visits in an outpatient setting to restore the patient's health. There are also indirect costs, which may include missed work, reduced quality of life, and disability for the patient, as well as possible uncompensated expenses for the healthcare provider. In a 1997 study, preventable ADEs were estimated to add $4685 in adjusted, postevent costs to an inpatient hospitalization, amounting to an additional $2.8 million in annual costs per hospital.11 Citing articles by Bates and colleagues and Classen and colleagues, the IOM estimates that preventable ADEs affect up to 450,000 hospitalized patients and add $3.5 billion in extra costs to hospitals annually.4,11,12
KEY POINTS
-
▸
Half of all adverse drug events (ADEs) are a result of medication errors and are therefore preventable.
-
▸
Injectable medications are among those at highest risk for error and can be associated with life-threatening events.
-
▸
This is the first analysis of the national burden of medication errors associated with inpatient injectable medications.
-
▸
The results show that preventable ADEs associated with injectable medications impact more than 1 million patients in the inpatient setting.
-
▸
Injectable-related preventable ADEs cause an increase of $2.7 billion to $5.1 billion in annual costs to US healthcare payers, with an average of $600,000 in extra annual cost per hospital.
-
▸
Furthermore, the analysis of liability claims shows a cost burden of $300 million to $610 million annually in medical professional liability, with an average cost of $72,000 per hospital.
-
▸
Reducing injectable medication errors and the associated preventable ADEs can improve quality of care for patients and reduce unnecessary cost for payers, hospitals, and physicians.
-
▸
The study's broad approach to costs, including the 4 months after discharge and medical professional liability costs, is aligned with healthcare reform initiatives in the United States, where payers are introducing new payment structures that consider patient outcomes beyond the inpatient stay.
Lawsuits and administrative actions related to preventable ADEs also increase costs for healthcare stakeholders. Provider costs related to medical professional liability (MPL), once called “medical malpractice,” are substantial. A previous study of MPL claims estimated that 73% of ADE-related cases were preventable; although legal defense costs were similar for inpatient and outpatient ADEs, the legal settlement costs were greatest for inpatient ADEs, which averaged $376,500 per MPL case.13
We conducted a comprehensive analysis of US payer and MPL costs for preventable ADEs related to injectable medications in the inpatient setting. We chose to focus this study on preventable ADEs resulting from injectable medications for several reasons, including their frequent use, their high risk for error, and their potential for targeted prevention strategies in the inpatient setting.14
Methods
In this study we used a healthcare payer perspective to analyze the probability of preventable ADEs and associated medical costs related to inpatient injectable medications and projected the national number of ADEs and their costs. In addition, this analysis took an MPL insurer perspective in analyzing medication-related facility and professional insurance claims to generate national-level MPL costs related to preventable ADEs.
Definitions
The definitions of the terms that are used in this study are listed in Table 1.
Table 1.
Adverse Drug Events Definitions Used in This Study
| Term | Definition |
|---|---|
| ADE | An injury due to medication; not all are due to errors or are preventable. For example, there may be no warning that a patient will have an allergic reaction to a medication |
| Medication error | Any error that occurs during the medication use process |
| Preventable ADE | When an ADE coexists with a medication error, it is considered a preventable ADE |
| Medical professional liability | Formerly called medical malpractice, medical professional liability costs include claims, administrative costs, insurer profit, and legal fees. The MPL of hospitals and professionals (eg, physicians) are often administered separately |
ADE indicates adverse drug event.
Data Sources and Methodology
The formulas for each calculation and further information on each source that was used are detailed in the Appendix, which is available at www.AHDBonline.com.
A medication error reporting system database with records noting each type of medication, standardized categories of error and clinical consequences, and setting of care was used to determine the distribution of ADEs for each injectable medication (Quantros MedMarx 2009–2011). The Premier National Database 2010–2011, which contains discharge data from 160 hospitals with detailed medication orders per patient record, was used to examine the frequency of each type of injection per discharge, by diagnosis-related group (DRG).
Payer administrative claims databases (Medicare 5% Analytic Sample 2009–2010 and Thomson Reuters MarketScan, 2009–2010), which include all sites of service, were used to select ADE cases and controls to calculate the incremental healthcare costs for preventable ADEs. The distribution of hospitalizations by payer and by DRG was derived from 2010 data, which were comprised of 17 state-level inpatient claims sets (from Arizona, California, Florida, Illinois, Iowa, Maryland, Massachusetts, New Jersey, New York, Oklahoma, Rhode Island, Texas, Utah, Vermont, Virginia, Washington, and Wisconsin), and were extrapolated to match the US total number of annual hospitalizations of approximately 37 million.
Five sources were used to estimate relevant MPL costs for inpatient preventable ADEs, including (1) a national database of closed MPL claims for 1990–2011 (National Practitioner Data Bank, HHS); (2) 2007–2011 premium rate filings for publicly available MPL state-level insurance (8 states, including California, Florida, Louisiana, Massachusetts, North Carolina, Ohio, Pennsylvania, and Vermont); (3) the 2010 American Hospital Association hospital-level survey on operational and financial statistics; (4) an industry survey of rate relativities for 201015; and (5) a detailed hospital and professional MPL closed claims database for 1994–2009 (Florida's Closed Claim Database).
The Florida Closed Claim Database is the only publicly available database that allows separation of hospital and physician liabilities for inpatient cases associated with medications.
Cost Analysis: Injectable Medication ADEs and Matched Controls
Matched cohorts of inpatient cases and controls were analyzed to calculate the incremental costs resulting from an injectable ADE. For the cases, patients with International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes identifying likely inpatient medication errors—such as a wrong dose or improper administration (ICD-9 codes E850.xx-E853.xx) and poisoning from an overdose or a wrong substance that was given or taken in error (ICD-9 codes 960.xx-979.xx)—were selected from the 2 sets of payer administrative claims. To ensure that our cases included only patients with a preventable ADE occurring during the admission, we selected surgical DRG cases with error codes, because surgical admissions would unlikely be caused by an outpatient preventable ADE. The detailed claims for each ADE case, including the full list of patient-level diagnoses and procedures coded during the admission, were independently reviewed by 2 physicians to confirm the reasonability of the ADE assignment.
The same databases were used to identify the controls, who were matched by discharge DRG and by preadmission patient costs that were within 3% of ADE case costs. The incremental cost of a preventable ADE was calculated as the cost difference between cases and matched controls within 4 months of the index hospitalization, inclusive of physician services during the hospitalization and any postdischarge care. This matched cohort analysis was applied for Medicare and for commercial patients separately; per-patient Medicaid costs were estimated as 80% of Medicare costs. All costs were inflated to 2013 dollars using the annual trend rate of 5% for commercial insurers or 4% for other insurers.
Medical Professional Liability Analysis
The portion of MPL attributable to inpatient medication errors was developed from the National Practitioner Data Bank data, using cases associated with nurses as a proxy for hospital inpatient site of service, which were not available. We applied this same attributable portion to estimate the per-bed inpatient medication MPL costs, using premium rate documentation that was filed by state-level MPL insurers. Regional MPL estimates were summed to calculate the national figure. The estimated MPL cost includes the facility inpatient (ie, the hospital's liability) as well as professional (ie, physician and other clinician liability) costs.
Statistical Considerations
Our analysis applied findings from the HHS study that the probability of a preventable medication error during an inpatient stay was 10.07% and that 50% of ADEs were preventable. The preventable ADEs associated with injectable medications were modeled as 87% (from injectable proportions of ADEs reported in the medication errors database) of the estimated preventable ADE total admissions, payer costs, and MPL costs. The means and the 95% confidence intervals were calculated on each result. A sensitivity analysis was conducted by varying the probability of an inpatient medication error per admission and the portion of such errors that were preventable to illustrate the variability of results. The year-to-year statistical variation in the national closed claim cost during the period between 2004 and 2011 was used to generate an estimated range of national MPL costs resulting from preventable ADEs.
Results
The mean probability for a preventable ADE per administration of an injectable medication was 0.25% (Table 2). Of the injectable medications, insulin had the highest probability for a preventable ADE (1.16%), followed by cardiovascular medications (0.5%), narcotic/analgesic medications (0.33%), and anticoagulant/thrombolytic medications (0.26%).
Table 2.
Probability of Preventable Adverse Drug Events per Injectable Drug Administered and Administrations of Injectable Drug per Admission
| Injectable drug group | Probability of preventable ADE per administration of injectable medicationa, % (95% CI) | Injectable drugs administered per admissionb, N (95% CI) | Total admissions receiving injectable medication, in millions, N (95% CI) |
|---|---|---|---|
| Insulin | 1.16 (0.43–1.89) | 0.74 (0.74–0.74) | 6.7 (6.7–6.7) |
| Cardiovascular | 0.50 (0.19–0.82) | 0.51 (0.51–0.51) | 5.3 (5.3–5.3) |
| Narcotic/analgesic | 0.33 (0.12–0.53) | 2.29 (2.28–2.29) | 15.4 (15.4–15.5) |
| Anticoagulant/thrombolytic | 0.26 (0.10–0.43) | 1.92 (1.92–1.92) | 14.2 (14.2–14.2) |
| Electrolytes/minerals | 0.25 (0.09–0.40) | 0.85 (0.84–0.85) | 5.9 (5.9–5.9) |
| Anxiolytic/sedative | 0.22 (0.08–0.35) | 0.63 (0.63–0.63) | 12.0 (12.0–12.0) |
| Anti-infective | 0.15 (0.06–0.25) | 2.93 (2.93–2.93) | 18.5 (18.5–18.5) |
| Other | 0.11 (0.04–0.19) | 5.53 (5.52–5.53) | 25.7 (25.7–25.7) |
| Mean | 0.25 (0.09–0.40) | 15.39 (15.38–15.40) | 31.4 (31.4–31.4) |
Estimated from Premier Database and Quantros MedMarx.
Weighted average of all hospitalizations, by Medicare severity diagnosis-related group in the United States.
ADEs indicates adverse drug events; CI, confidence interval.
The mean number of administrations of injectable medications per inpatient hospitalization was 15.39, with anti-infectives (2.93) and narcotic/analgesics (2.29) as the leading classes of administered doses.
The probability of a preventable ADE from an injectable medication per patient varied by the type of hospitalization, with surgical DRGs carrying a 6.4% probability and medical DRGs carrying a 3.3% probability, whereas patients with other hospitalization types (eg, obstetrics, psychiatry) were significantly less likely to have a preventable ADE from an injectable medication. The 20 DRG families with the highest probability of preventable ADEs from injectable medications per hospitalization are listed in Table 3.
Table 3.
Diagnosis-Related Group Families with Greatest Contributions to Preventable Adverse Drug Events
| Description (MS DRGs included in each family) | Proportion of preventable ADEs resulting from injectable medication, % | Proportion of hospitalizations, % | Probability of a preventable ADE resulting from injectable medication administered at the hospital, % |
|---|---|---|---|
| Septicemia or severe sepsis without mechanical ventilation 96+ hrs (871–872) | 3.75 | 1.94 | 6.3 |
| Major small and large bowel procedures (329–331) | 2.71 | 0.86 | 10.4 |
| Extracorporeal membrane oxygenation or tracheostomy with mechanical ventilation 96+ hrs (003) | 2.57 | 0.14 | 59.8 |
| Heart failure and shock (291–293) | 2.56 | 2.18 | 3.9 |
| Respiratory system diagnosis with ventilator support (207–208) | 2.44 | 0.60 | 13.3 |
| Major joint replacement or reattachment of lower extremity (469–470) | 2.42 | 2.40 | 3.3 |
| Cesarean section (765–766) | 2.27 | 3.57 | 2.1 |
| Coronary bypass (231–236) | 2.15 | 0.41 | 17.2 |
| Simple pneumonia and pleurisy (193–195) | 2.04 | 2.25 | 3.0 |
| Esophagitis, gastroenteritis, and miscellaneous digestive disorders (391–392) | 1.84 | 2.52 | 2.4 |
| Chronic obstructive pulmonary disease (190–192) | 1.73 | 1.85 | 3.1 |
| Cardiac valve and other major cardiothoracic procedure (216–221) | 1.63 | 0.28 | 18.9 |
| Infectious and parasitic diseases with operating room procedure (853–855) | 1.59 | 0.29 | 18.1 |
| Percutaneous cardiovascular procedure with stent (246–249) | 1.51 | 1.26 | 3.9 |
| Rehabilitation (945–946) | 1.48 | 1.32 | 3.7 |
| Diabetes (637–639) | 1.48 | 0.91 | 5.3 |
| Cellulitis (602–603) | 1.47 | 1.47 | 3.3 |
| Tracheostomy with mechanical ventilation 96+ hrs (004) | 1.46 | 0.12 | 38.8 |
| Vaginal delivery (774–775) | 1.45 | 6.75 | 0.7 |
| Renal failure (682–684) | 1.41 | 1.15 | 4.0 |
ADEs indicates adverse drug events; MS DRGs, Medicare severity diagnosis-related groups.
A total of 303 preventable ADE cases and 37,513 control matches were identified for the incremental cost analysis. The national incidence and incremental cost of preventable ADEs from injectable medications is shown in Table 4. Preventable ADEs from the administration of injectable medications were estimated to occur in 1.2 million (95% confidence interval, 1.0 million-1.4 million) inpatient hospitalizations annually in the United States. The incremental cost of the preventable ADEs from injectable medications averaged $3100 per admission. The incremental annual cost for preventable ADEs resulting from injectable medications was estimated to be between $2.7 billion and $5.1 billion, which averages $600,000 of payer costs per hospital (Table 4).
Table 4.
Estimated National Incidence and Incremental Cost of Preventable Adverse Drug Events Related to Injectable Medications
| Annual number of inpatient hospitalizations in the United Statesa | 37 million |
| Probability of avoidable ADE from injectable medications per hospitalization | 3.3% (95% CI, 2.7%-3.9%) |
| Annual number of hospitalizations with preventable ADEs resulting from injectable medications in the United States | 1.2 million (95% CI, 1.0 million-1.4 million) |
| Incremental cost of preventable ADE from injectable medications per hospitalizationb | $3100 (95% CI, $2700-$3600) |
| Annual incremental cost of preventable ADEs resulting from injectable medicationsb | $3.8 billion (95% CI, $2.7 billion-$5.1 billion) |
| Average annual inpatient preventable ADE cost resulting from injectable medication per hospital (6268 hospitals)b | $600,000 |
American Hospital Association. AHA Hospital Statistics, 2012 edition. 2012. www.aha.org/research/rc/stat-studies/fast-facts.shtml. Accessed September 17, 2012.
Costs are expressed in projected 2013 dollars.
ADEs indicates adverse drug events; CI, confidence interval.
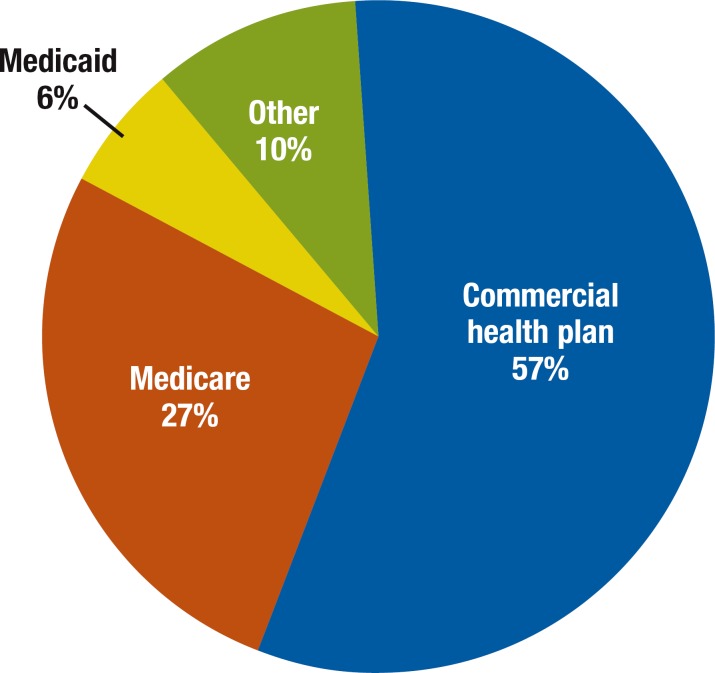
The annual payer cost burdens are illustrated in the Figure, which shows that the majority (57%) of costs for preventable ADEs is paid by commercial health plans.
Figure. Costs of Preventable ADEs from Inpatient Injectable Medications, by Payer.
ADEs indicates adverse drug events.
We estimate the 2013 MPL costs that are associated with inpatient injectable ADEs to be between $300 million and $610 million (Table 5). Although costs vary by region, type, and size of hospital, the total medication-related MPL costs average an annual $72,000 per US hospital.
Table 5.
Estimated Medical Professional Liability Costs Associated with Inpatient Adverse Drug Events
| Number of inpatient hospital licensed bedsa | 931,000 |
| Inpatient hospital annual MPL cost per licensed bedb | $3700 |
| Total annual inpatient hospital MPL cost | $3.48 billion |
| Estimated percentage of hospital MPL cost attributable to ADEs resulting from injectable medicationsc | 6.5% |
| Ratio of physician plus facility MPL cost to facility MPL costd | 2 |
| Annual inpatient ADE MPL cost resulting from injectable medication | $450 million (95% CI, $300 million-$610 million) |
| Average annual inpatient ADE MPL cost associated with injectable medication per hospital (total of 6268 hospitals)b | $72,000 |
American Hospital Association. AHA Hospital Statistics, 2012 edition. 2012. www.aha.org/research/rc/stat-studies/fast-facts.shtml. Accessed September 17, 2012. Adjusted to remove nonacute beds.
Authors' analysis of hospital MPL premium rates.
Authors' analysis of National Practitioner Data Bank.
Authors' analysis of the Florida Department of Insurance Closed Claim Database.
ADEs indicates adverse drug events; CI, confidence interval; MPL, medical professional liability.
Discussion
Our study of inpatient injectable medications estimated that there are 1.2 million hospitalizations with preventable ADEs annually, contributing incremental direct medical costs of between $2.7 billion and $5.1 billion annually to US payers. This study is among the first to include the postdischarge costs in estimating the impact of inpatient preventable harms. In addition, we estimated that $300 million to $610 million is spent annually in medical liability for inpatient ADEs resulting from injectable medications (Table 5).
Previous studies on medication errors have estimated a 0.06% risk for a preventable ADE per dose and have concluded that a hospital with 6 million annual doses could attribute 4000 preventable ADEs annually to medication administration errors.9 Our study showed that the average hospitalized patient is receiving more than 15 injections, with a probability of a preventable ADE of approximately 1 of every 400 injections (0.25%). A hospital with 10,000 injectable doses daily could expect 25 daily preventable ADEs, or more than 9000 preventable ADEs annually resulting from injectable medications.
Research Implications
Our study builds on the 2010 HHS study that reported estimates of numbers and costs of inpatient preventable ADEs in Medicare beneficiaries.5 We expanded to a national estimate but narrowed the focus to injectable medications that may be targeted for prevention strategies. The current study is unique in its inclusion of all-payer national cost estimates encompassing nonfacility inpatient costs, such as physician costs, costs to payers other than traditional Medicare (ie, Medicare Advantage, commercial, and Medicaid), and postdischarge costs for 4 months. This broader vantage is aligned with healthcare reform initiatives in the United States, where payers are introducing new payment structures that consider patient outcomes beyond the inpatient stay.
With preventable ADEs related to injectable medication errors adding $2.7 billion to $5.1 billion in extra costs, this issue is similar in magnitude to other foci for healthcare reform, such as reducing bedsore pressure ulcers and hospital-acquired infections. In a study on adverse event costs related to medical errors, Van Den Bos and colleagues documented that pressure ulcers and postoperative infections were the most common preventable events, accounting for approximately $3.27 billion each in annual costs.16 With increased awareness of the healthcare waste related to preventable medical errors, a number of initiatives have been introduced to address this issue, including streamlined provider communication initiatives, payment reform (eg, Medicare's “never event”) initiative, and reduced payments for hospital-acquired infections.16
Injectable medication errors may be similarly targeted with prevention strategies. The inpatient medication use process includes several steps—prescribing, transcribing/documentation, dispensing (including medication preparation), administering, and monitoring. Errors in the early steps of the medication system can be prevented by verifications done by pharmacists and nurses.
Some interventions developed through systematic approaches to error prevention that dramatically reduce the frequency of medication errors and that also impact injectable medications include computerized physician order entry with decision support,17 automated medication dispensing systems,18 and bar-coded medication administration.6 However, a large proportion of medication errors (56%-62%) occur during the administration step of the medication use process.3,19
Errors in administration are the most difficult to detect, because they occur in the last step of the medication use process, usually by the bedside nurse, and often without additional oversight.20
Several technologies specifically targeting the administration of injectable medications include smart infusion pumps,21 prefilled syringes,8 and in-line sensors to ensure the correct medication and the correct concentration.22
Our data analysis covers both high-risk clinical conditions and medications. For example, although 2% of national hospitalizations are for septicemia/sepsis, these DRGs make up almost 4% of the preventable ADE cases; 6% of septicemia/sepsis hospitalizations are predicted to experience a harmful medication error (Table 3). The recognition that the DRG families in Table 3 are associated with hospitalizations that are not only intense utilizers of clinical resources but are also at increased risk for medication errors may sharpen hospitals' focus on improvement opportunities.
Our results are consistent with other estimates, and our intermediate results for particular types of patients or injectable medications could be validated through intensive studies, such as direct observations or patient chart audits. Sensitivity analyses confirm our linear projections, with each 1% increase or decrease in either the probability of an inpatient medication error per admission or the portion of such errors that were preventable resulting in an increase or a decrease in the estimated costs by 1%. For example, based on the HHS study,5 we assumed that 50% of ADEs were preventable. If this assumption were reduced to 40%, then the average annual incremental cost for preventable ADEs resulting from injectable medication would be reduced by 20%; our midpoint estimate of $3.8 billion would thereby be reduced to $3.0 billion.
Limitations
In this study we relied on multiple administrative claims data with known inherent limitations, such as coding inaccuracies and lack of clinical detail.23
In addition, although it is possible that patients could appear in multiple databases that we used, this would not cause double counting, because each source was used to develop distinct assumptions.
Our analysis also relied on several assumptions from previous work on preventable ADEs.5 We focused on ADEs from injectable medications, and we mapped reported errors for injectable medications to Medicare severity DRG, but we estimated costs from ADEs caused by all medications and modeled the attribution to injectable medications. We did not include in our calculation patients in observation beds or patients in the emergency department who were not admitted to the hospital.
A potential limitation related to our use of a medication error reporting database is whether there is bias in the reporting of adverse events, as would be the case if reported events tended to be more serious. However, in healthcare settings, there is strong evidence that event severity has little relationship to whether the event is reported.24 This assumption invokes the “causal continuum hypothesis” used in other industries, such as in aviation, which suggests that the characteristics and circumstances of reported errors are similar to those of unreported errors.25
Finally, our MPL estimate relied on historical financial information sources and sources that were not assembled for the purpose of quantifying costs associated with MPL. We assumed that all MPL costs were associated with preventable ADEs, which ignores the possibility that some MPL awards may not be associated with preventable errors (or even unpreventable errors). Certainly, for both healthcare and MPL costs, other methodologies and additional data sources could produce different estimates.
Conclusions
The approach taken in this study may serve as a basis for further studies of medication errors for injectables. The results of this study highlight potential areas for future prospective research on high-frequency and high-risk medications, such as insulin, narcotics, and anxiolytics.
Inpatient preventable ADEs are often caused by injectable medications, potentially affecting more than 1 million US patient hospitalizations and adding $2.7 billion to $5.1 billion of extra direct medical costs to payers and hundreds of millions of dollars in extra liability costs to hospitals and physicians, annually. Reducing the risk for injectable medication errors is a clear target area for improving acute patient quality of care and for reducing unnecessary costs in the US healthcare system.
Study Funding
Funding for this study was provided by Becton, Dickinson and Company.
Author Disclosure Statement
Ms Lahue is an employee of and Mr Pyenson, Mr Iwasaki, Dr Blumen, Ms Forray, and Dr Rothschild are consultants to Becton, Dickinson and Company.
Contributor Information
Betsy J. Lahue, Vice President, Health Economics and Outcomes Research, Becton, Dickinson and Company, Franklin Lakes, NJ.
Bruce Pyenson, Principal, Consulting Actuary, Milliman Inc, New York, NY.
Kosuke Iwasaki, Consulting Actuary, Milliman Inc, New York, NY.
Helen E. Blumen, Principal, Senior Health Consultant, Milliman Inc, New York, NY.
Susan Forray, Consulting Actuary at Milliman Inc, New York, NY.
Jeffrey M. Rothschild, Associate Professor of Medicine, Division of General Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA.
References
- 1.New England Health Institute. Preventing medication errors: a $21 billion opportunity. www.nehi.net/bendthecurve/sup/documents/Medication_Errors_%20Brief.pdf Accessed September 17, 2012.
- 2.Committee on Quality of Health Care in America, Institute of Medicine. Errors in health care: a leading cause of death and injury. In: Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 3.Leape LL, Bates DW, Cullen DJ, et al. Systems analysis of adverse drug events. ADE Prevention Study Group. JAMA. 1995; 274: 35–43 [PubMed] [Google Scholar]
- 4.Committee on Identifying and Preventing Medication Errors, Institute of Medicine. Medication errors: incidence and cost. In: Preventing Medication Errors: Quality Chasm Series. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 5.Levinson DR. Adverse events in hospitals: national incidence among Medicare beneficiaries. US Dept of Health and Human Services, Office of Inspector General. November 2010. OEI-06-09-00090. https://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf Accessed November 15, 2012.
- 6.Poon EG, Keohane CA, Yoon CS, et al. Effect of bar-code technology on the safety of medication administration. N Engl J Med. 2010; 362: 1698–1707 [DOI] [PubMed] [Google Scholar]
- 7.Barker KN, Flynn EA, Pepper GA, et al. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002; 162: 1897–1903 [DOI] [PubMed] [Google Scholar]
- 8.Adapa RM, Mani V, Murray LJ, et al. Errors during the preparation of drug infusions: a randomized controlled trial. Br J Anaesth. 2012; 109: 729–734 [DOI] [PubMed] [Google Scholar]
- 9.Kale A, Keohane CA, Maviglia S, et al. Adverse drug events caused by serious medication administration errors. BMJ Qual Saf. 2012; 21: 933–938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osmon S, Harris CB, Dunagan WC, et al. Reporting of medical errors: an intensive care unit experience. Crit Care Med. 2004; 32: 727–733 [DOI] [PubMed] [Google Scholar]
- 11.Bates DW, Spell N, Cullen DJ, et al. The costs of adverse drug events in hospitalized patients. Adverse Drug Events Prevention Study Group. JAMA. 1997; 277: 307–311 [PubMed] [Google Scholar]
- 12.Classen DC, Pestotnik SL, Evans RS, Burke JP. Computerized surveillance of adverse drug events in hospital patients. JAMA. 1991; 266: 2847–2851 [PubMed] [Google Scholar]
- 13.Rothschild JM, Federico FA, Gandhi TK, et al. Analysis of medication-related malpractice claims: causes, preventability, and costs. Arch Intern Med. 2002; 162: 2414–2420 [DOI] [PubMed] [Google Scholar]
- 14.Sanborn MD, Moody ML, Harder KA, et al. Second Consensus Development Conference on the Safety of Intravenous Drug Delivery Systems—2008. Am J Health Syst Pharm. 2009; 66: 185–192 [DOI] [PubMed] [Google Scholar]
- 15.Medical Liability Monitor annual rate survey. Medical Liability Monitor. 2011; 36: 7–43 [Google Scholar]
- 16.Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Aff (Millwood). 2011; 30: 596–603 [DOI] [PubMed] [Google Scholar]
- 17.Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999; 6: 313–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chapuis C, Roustit M, Bal G, et al. Automated drug dispensing system reduces medication errors in an intensive care setting. Crit Care Med. 2010; 38: 2275–2281 [DOI] [PubMed] [Google Scholar]
- 19.Beyea SC, Hicks RW, Becker SC. Medication errors in the OR—a secondary analysis of Medmarx. AORN J. 2003; 77:122, 125–129,132–134. [DOI] [PubMed] [Google Scholar]
- 20.Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA. 1995; 274: 29–34 [PubMed] [Google Scholar]
- 21.Rothschild JM, Keohane CA, Cook EF, et al. A controlled trial of smart infusion pumps to improve medication safety in critically ill patients. Crit Care Med. 2005; 33: 533–540 [DOI] [PubMed] [Google Scholar]
- 22.SEA Medical Systems. Technology. www.seamedical.com/?pg=products Accessed September 17, 2012.
- 23.Meddings JA, Reichert H, Rogers MA, et al. Effect of nonpayment for hospital-acquired, catheter-associated urinary tract infection: a statewide analysis. Ann Intern Med. 2012; 157: 305–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levinson DR. Hospital incident reporting systems do not capture most patient harm. US Dept of Health and Human Services, Office of Inspector General. January 2012. Report No OEI-06-09-00091. http://psnet.ahrq.gov/resource.aspx?resourceID=23842 Accessed November 24, 2012.
- 25.Cure L, Zayas-Castro J, Fabri P. Clustering-based methodology for analyzing near-miss reports and identifying risks in healthcare delivery. J Biomed Inform. 2011; 44: 738–748 [DOI] [PubMed] [Google Scholar]