Abstract
Background
Schizophrenia is a serious public health concern and a leading cause of disability. Previous studies have shown this disease is associated with an economic burden of more than $60 billion annually in direct and indirect costs in the United States.
Objective
To analyze the annual and longitudinal costs associated with the treatment of patients with schizophrenia from a payer perspective.
Methods
Two claim-based analyses were conducted using data from the Truven Health MarketScan database of a commercially insured population: (1) an annual snapshot of patients with newly diagnosed and chronic schizophrenia, and (2) a 24-month longitudinal analysis of patients with newly diagnosed schizophrenia. The snapshot analysis included individuals who had ≥2 claims with a diagnosis code for schizophrenia on separate dates during 2011 (with the date of the first claim designated as the index date), and who were enrolled for 12 months before the index date. For the longitudinal analysis, patients were included if they were continuously enrolled for 24 months after the date of schizophrenia diagnosis, which was designated as the index date. The claims were grouped by inpatient, outpatient, professional, and prescription drug categories, and were further segmented by claims for schizophrenia, other psychiatric, and nonschizophrenia/nonpsychiatric conditions.
Results
A total of 8985 patients with schizophrenia met the inclusion criteria for the snapshot analysis. The mean cost per patient per month (PPPM) for a patient with schizophrenia was $1806 versus $419 per member per month for the demographically adjusted nonschizophrenic (ie, matched for age and sex) population. The PPPM cost of $1806 for patients with schizophrenia was 42% for inpatient expenditures, 33% for outpatient, and 25% for prescription drug costs. The annual inpatient admission rates were 636 per 1000 patients with schizophrenia and 48 per 1000 persons for the demographically adjusted population without schizophrenia. The annual emergency department visits for patients with schizophrenia were 2270 per 1000 patients and 158 per 1000 persons without schizophrenia for the demographically adjusted population. For the longitudinal analysis, 1902 patients with newly diagnosed schizophrenia were identified. The total claim costs for patients increased from $800 monthly in the 12 months before the index date to approximately $2000 in the month before the index date. The highest costs occurred in the month of diagnosis (designated as the index month; mean cost, $6601). The total all-cause claim cost after the index date decreased to $1635 monthly for months 2 to 6, $1456 monthly for months 7 to 12, $1324 monthly for months 13 to 18, and $1218 monthly for months 19 to 24.
Conclusion
Although the prevalence of schizophrenia is low in a commercially insured US population, this analysis shows that the average total claim cost per patient with schizophrenia is more than 4 times the average total claim cost for a demographically adjusted population without schizophrenia. Furthermore, for newly diagnosed patients with schizophrenia, the cost, which is largely driven by inpatient charges, is highest in the month of diagnosis.
Schizophrenia is a serious public health problem that affects approximately 1% of the US population.1 Schizophrenia is a leading cause of disability, and is associated with an economic burden of more than $60 billion annually in direct and indirect costs in the United States.2 Schizophrenia is a severe form of mental illness broadly characterized by 3 domains of psychopathology, including negative symptoms (ie, social withdrawal, lack of motivation, and lack of emotional reactivity), positive symptoms (ie, hallucinations and delusions), and cognitive deficits (ie, working memory, attention, and executive function).3–6 In addition, serious medical conditions, such as type 2 diabetes, obesity, hypertension, and dyslipidemia, are more common in patients with schizophrenia than in the general population; in turn, these conditions may increase the risk for cardiovascular disease and lead to increased morbidity and mortality.7 Notably, the estimated prevalence of diabetes in patients with schizophrenia is 13% to 15%; dyslipidemia, 25%; obesity, 42%; and hypertension, 19% to 58%.8
Numerous studies have investigated the cost and resource utilization associated with schizophrenia in commercially insured, self-insured, Medicare, Medicaid, and Veterans Administration populations.2,9–14 Data have consistently shown that schizophrenia represents a substantial economic burden for patients and their families, healthcare providers, and for society in terms of costs associated with the healthcare, social, and justice systems; informal caregivers; and productivity loss as a result of unemployment or premature death.15 Schizophrenia is one of the most expensive disorders in adults,12,16 accounting for an estimated 2.5% of the total healthcare expenditures in the United States.17,18
Although schizophrenia is costly and difficult to treat, it has not received the level of attention from commercial payers that many other chronic diseases (eg, diabetes, asthma, and hypertension) receive. The 2013 addition of several schizophrenia Healthcare Effectiveness Data and Information Set (HEDIS) criteria will bring increased attention to the population of patients with schizophrenia by insurers and represents an opportunity for treatment improvement.19 In particular, the HEDIS criteria include adherence to antipsychotic medications for patients with schizophrenia, diabetes screening for patients with schizophrenia or bipolar disorder who are using antipsychotics, cardiovascular monitoring for patients with cardiovascular disease and schizophrenia, and diabetes monitoring for patients with diabetes and schizophrenia.19
In addition, the Affordable Care Act (ACA) will affect insurance coverage for the uninsured population of patients with schizophrenia in 2014, with Medicaid expansion and insurance subsidies available for qualified individuals purchasing insurance on state exchanges. The 2011 federally mandated extension of commercial coverage to adult children until age 26 years has increased the prevalence of patients with schizophrenia in commercially insured populations, because most patients with schizophrenia are diagnosed in their early 20s.4,20 A recent study estimated that there would be an increase of approximately 2.3 million new users of mental health services in Medicaid and approximately 2 million covered by commercial insurance by the time healthcare reform according to the ACA is fully implemented in 2019.20
With the expected rise in the number of insured patients with schizophrenia and an increased focus on the management of schizophrenia as a result of the new HEDIS criteria, the intent of the current study was to provide an up-to-date descriptive analysis of the schizophrenia population from the payer perspective, including (1) relevant demographic characteristics, (2) a snapshot analysis of resource utilization and healthcare costs, and (3) a longitudinal analysis of resource utilization and healthcare costs over a period of 24 months by patients with newly diagnosed schizophrenia.
KEY POINTS
-
▸
Schizophrenia is a serious medical condition and a leading cause of disability.
-
▸
Although the prevalence of schizophrenia is low in commercially insured populations, the total annual cost burden of the disease is more than $60 billion in the United States.
-
▸
This new study involved 2 claims-based analyses of the annual and longitudinal costs associated with the treatment of schizophrenia in a commercially insured population.
-
▸
Among patients with newly diagnosed schizophrenia, the cost was highest (mean cost, $6601) in the month of diagnosis, and was largely driven by inpatient charges.
-
▸
The annual inpatient admission rate was 636 per 1000 patients with schizophrenia versus 48 per 1000 persons in a demographically adjusted population without schizophrenia, a 13-fold difference.
-
▸
The mean monthly cost for a patient with schizophrenia was $1806, which is more than 4 times the mean monthly cost of $419 for a demographically matched member without schizophrenia.
-
▸
As this analysis shows, the cost of treating schizophrenia is substantial, yet this chronic disease does not receive the same level of payer attention afforded to other chronic diseases.
-
▸
The 2013 addition of HEDIS criteria for schizophrenia will likely draw more attention from insurers to this patient population and represents an opportunity for treatment improvement.
Methods
Data Source
The study population was selected from the Truven Health MarketScan commercial claim data files between 2007 and 2011. These files contain all paid claims generated by more than 40 million commercially insured individuals annually, as well as member identification codes that allow members to be followed longitudinally over time. This administrative claim data set contains standard codes for diagnosis, procedure, diagnosis-related group (DRG), and National Drug Code (NDC); site of service information and amounts paid by commercial insurers; and cost-sharing by members. We performed 2 analyses: (1) an annual snapshot analysis of patients with newly diagnosed and chronic schizophrenia, using 2011 as the index year, and (2) a longitudinal analysis of patients with newly diagnosed schizophrenia using 2008 and 2009 as index years, and 2008 to 2011 for the 24-month postdiagnosis period.
Study Population
The study population for each analysis consisted of individuals aged 13 to 64 years who met the HEDIS claims-based identification criteria of 2 or more inpatient or outpatient claims with International Classification of Diseases, Ninth Revision (ICD-9) code 295.xx for schizophrenia on separate dates during the index year. Patients were included in the study if they had a newly diagnosed schizophrenia and had no claim coded with schizophrenia in the 12 months before the index date (“newly diagnosed” was defined as having no claim with an ICD-9 diagnosis code of schizophrenia in any position in the 12 months before the index date). In both analyses, all patients were required to be continuously enrolled for the 12-month look-back period. For the snapshot analysis, patients were not required to be enrolled continuously during the entire 2011 index year, and each patient's cost contribution was weighted by member months of enrollment during 2011. For the longitudinal analysis, the patients were required to be continuously enrolled for 24 months after the index date (ie, date of schizophrenia diagnosis).
Methodology
All claims for patients meeting the schizophrenia identification and eligibility criteria were grouped into major utilization categories (eg, inpatient or outpatient) using a combination of revenue codes, Healthcare Common Procedure Coding System (HCPCS) codes, DRGs, Current Procedural Terminology (CPT)-4 codes, ICD-9 procedure codes, and NDC codes that included inpatient, outpatient, professional, and prescription drug. The claims were further segmented by claims for schizophrenia and other psychiatric and nonschizophrenia/nonpsychiatric conditions.
Schizophrenia-related inpatient claims were identified via a psychiatric DRG (880–887), as well as an ICD-9 295.xx diagnosis code in any position of the inpatient claim. Schizophrenia-related emergency department visits and professional fee claims were identified if an ICD-9 diagnosis code in the 295.xx range was coded in any position of the claim. Psychiatric inpatient claims were coded with a psychiatric DRG (880–887) and were not coded with ICD-9 295.xx code in any position of the inpatient claim. Psychiatric-related emergency department and professional claims were coded with an ICD-9 code of 291 to 319.xx (excluding 295.xx) in any position of the claim.
All other claims were considered to be related to nonschizophrenia/nonpsychiatric conditions. Outpatient facility claims other than emergency department were not designated as schizophrenia or other psychiatric. The use of electroconvulsive therapy was identified by claims coded with ICD-9 procedure codes 94.23, 94.24, 94.26, or 94.27, or with the CPT-4 code 90870. Drug use by class—including antipsychotics, antidepressants, anticonvulsants, or antianxiety—was identified using NDC code lists from the Medi-Span 2013 drug data.
To compare the costs and medical utilization of the population of patients with schizophrenia and the population of individuals without schizophrenia in the Truven Health MarketScan claims data, we demographically adjusted the nonschizophrenic population to contribute the same weighting by 5-year age and sex bands.
Results
Snapshot Analysis
Prevalence/incidence
A total of 8985 patients in the 2011 MarketScan database met the criteria for schizophrenia (newly diagnosed, N = 2827; chronic, N = 6158), and the average member enrollment in a plan was 11.5 months. Of the 8985 patients with schizophrenia, 3550 (39.5%) were employees, 2599 (28.9%) were spouses, and 2836 (31.6%) were categorized as children/other.
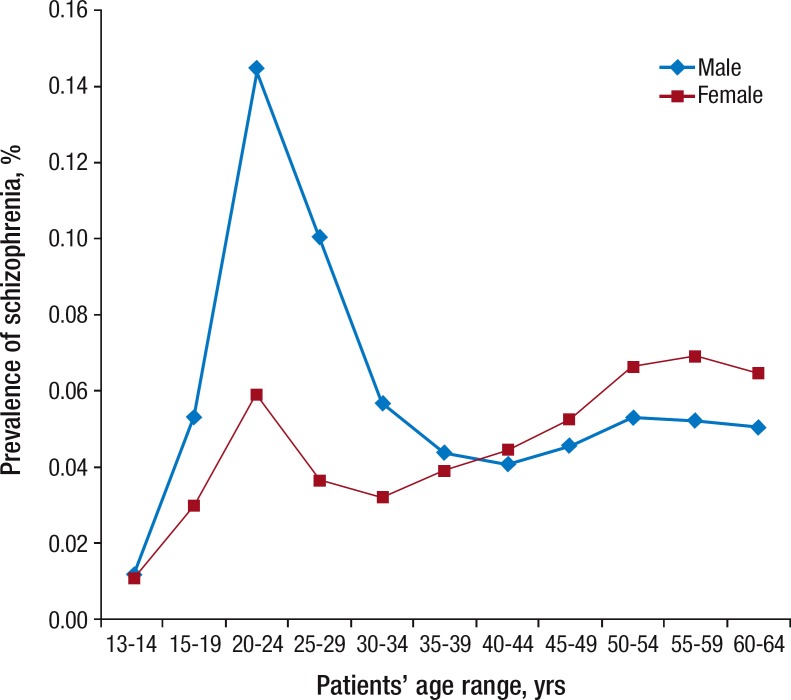
The prevalence of schizophrenia was 0.54 per 1000 persons in the 13- to 64-year-old age range, with the highest prevalence observed in men in the 20- to 24-year-old age cohort (1.45 per 1000 persons) and the prevalence in women ranging from 0.32 per 1000 persons to 0.69 per 1000 persons for the 30- to 34-year-old and 55- to 59-year-old age cohorts, respectively. The incidence of patients with schizophrenia (and with no schizophrenia claims in the 12 months before the index date) was 0.17 per 1000 persons among the 13- to 64-year-old cohort, with the highest incidence in men (0.65 per 1000 persons) and women (0.27 per 1000 persons) in the 20- to 24-year-old age cohorts. Figure 1 and Figure 2 outline the prevalence and incidence of schizophrenia, by age and by sex.
Figure 1. Prevalence Rate of Patients with Schizophrenia, 2011.
Source: Truven Health MarketScan database; 2011.
Figure 2. Incidence Rates of Patients with Schizophrenia, 2011.
Source: Truven Health MarketScan database; 2011.
Costs
For the patients with schizophrenia, the mean cost per patient per month (PPPM), including paid amount by the insurer and patient cost-sharing, was $1806, more than 4 times higher than that of $419 for the population without schizophrenia in the MarketScan database with the same demographic (ie, age and sex) weighting (Table).
Table.
Snapshot Analysis: Mean PPPM and PMPM Costs and Resource Utilization for Patients with Schizophrenia Compared with Demographically Adjusted Total Commercially Insured Population
| Variable | Patients with schizophrenia | Matched population with similar demographics, without schizophrenia |
|---|---|---|
| Total PPPM/PMPM cost, $ | 1806 | 419 |
| Inpatient PPPM/PMPM cost, $ | 762 | 97 |
| Outpatient PPPM/PMPM cost, $ | 592 | 239 |
| Prescription drug PPPM/PMPM cost, $ | 452 | 83 |
| Annual inpatient admissions per 1000 patients, N | 636 | 48 |
| Schizophrenia-related inpatient cases, N | 322 | — |
| Psychiatric/nonschizophrenia-related inpatient cases, N | 155 | — |
| Nonschizophrenia/nonpsychiatric-related inpatient cases, N | 158 | — |
| Annual emergency department visits per 1000 patients, N | 2270 | 158 |
| Schizophrenia-related emergency department visits, N | 242 | — |
| Psychiatric/nonschizophrenia-related emergency department visits, N | 513 | — |
| Nonschizophrenia/nonpsychiatric-related emergency department visits, N | 1516 | — |
PMPM indicates per member per month; PPPM, per patient per month.
Source: Truven Health MarketScan database; 2011.
The cost for patients with schizophrenia included $762 (42%) PPPM for inpatient costs (facility and professional), $592 (33%) PPPM for outpatient costs (facility and professional), and $452 (25%) PPPM for prescription drug costs. The most common prescription drug claims for patients with schizophrenia were antipsychotics (84% of patients with schizophrenia), followed by antidepressants (56% of patients with schizophrenia), anticonvulsants (43% of patients with schizophrenia), and antianxiety drugs (32% of patients with schizophrenia), with allowed PPPM costs of $302.20, $24.32, $16.65, and $2.60, respectively.
Hospitalization
The annual inpatient admission rate during the study period was 13 times higher in the population with schizophrenia than in the general population, with an annual rate of 636 admissions per 1000 patients with schizophrenia compared with an annual rate of 48 admissions per 1000 persons in the general demographically adjusted commercial population (Table). Of the inpatient admissions (N = 636) in patients with schizophrenia, 51% (N = 322) were schizophrenia-related, 24% (N = 155) were psychiatric-related (nonschizophrenia), and 25% (N = 158) were neither schizophrenia-related nor psychiatric-related.
Similarly, the annual emergency department utilization rate for patients with schizophrenia was 14 times higher than in the general population—2270 visits per 1000 patients with schizophrenia compared with 158 visits per 1000 persons in the demographically adjusted commercial population (Table). Of the emergency department visits (N = 2270) by patients with schizophrenia, 11% (N = 242) were schizophrenia-related, 23% (N = 513) were psychiatric-related, and 67% (N = 1516) were neither schizophrenia-related nor psychiatric-related.
Longitudinal Analysis
The longitudinal analysis required patients with schizophrenia to be continuously enrolled for 3 years, which allowed for a 12-month look back from the index date and a 24-month follow-up from the index date. Two index years were used to increase the sample size: index year 2008 required eligibility in 2007 to 2010 and index year 2009 required eligibility in 2008 to 2011. A total of 1902 patients were identified with newly diagnosed schizophrenia.
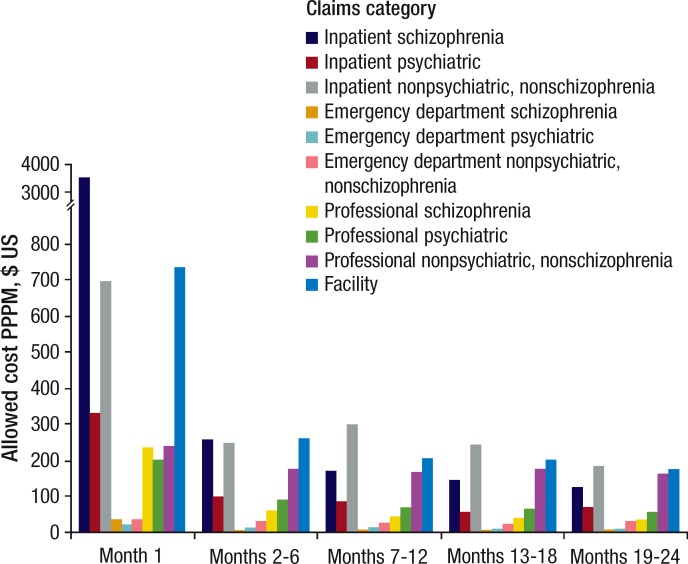
The cost for patients with schizophrenia gradually increased from approximately $800 in the 12 months before the index date to approximately $2000 in the month before the index date. The highest costs were incurred in the index month (ie, month of diagnosis), with an average cost of $6601 for the index month. Inpatient costs accounted for $4597 (70%) of the costs in the index month; 413 (22%) of the patients with schizophrenia were admitted to the hospital at some point during the index month. In addition to the patients who were admitted to the hospital in the index month, 307 (16%) patients had visited the emergency department at some point during the index month.
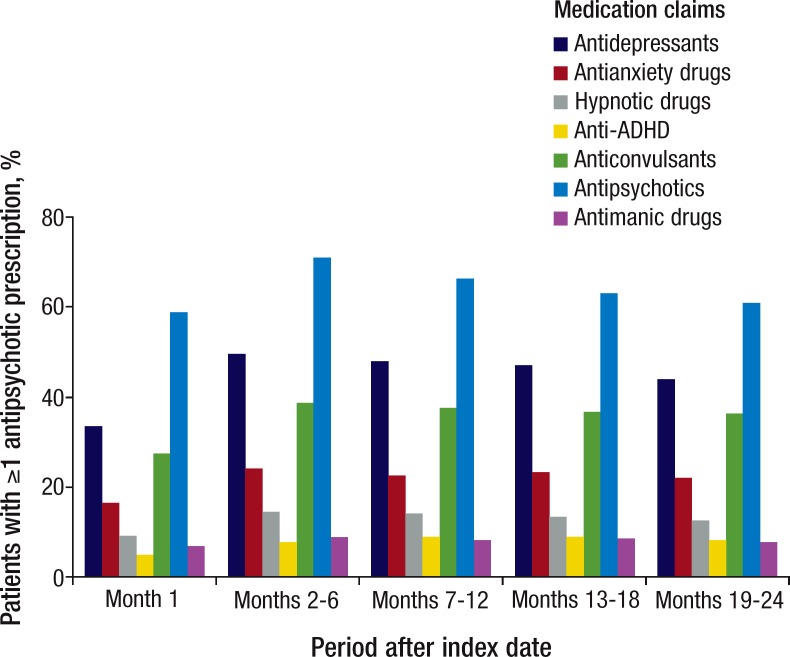
The cost in the months after the index date decreased to an average of $1635 monthly for months 2 to 6, $1456 monthly for months 7 to 12, $1324 monthly for months 13 to 18, and $1218 monthly for months 19 to 24. The percentage of patients with schizophrenia who had an antipsychotic claim was 58% in the index month, 71% during months 2 to 6, 66% during months 7 to 12, 63% during months 13 to 18, and 61% during months 19 to 24. The use of antidepressants and anticonvulsants were also high: 34% and 27% of patients with schizophrenia, respectively, had a prescription claim in the index month; 49% and 39% during months 2 to 6 after the index month; 48% and 37% during months 7 to 12; 47% and 36% during months 13 to 18; and 44% and 36% during months 19 to 24. Figure 3, Figure 4, and Figure 5 provide details of the cost and the use of key services in the months after the index date.
Figure 3. Longitudinal Analysis: Mean PPPM Monthly Cost Allowed after Index Date for Patients with Newly Diagnosed Schizophrenia.
PPPM indicates per patient per month.
Source: Truven Health MarketScan database; 2011.
Figure 4. Longitudinal Analysis: Monthly Inpatient Admissions and Emergency Department Visits after Index Date for Patients with Newly Diagnosed Schizophrenia.
Source: Truven Health MarketScan database; 2011.
Figure 5. Longitudinal Analysis of Patients with Newly Diagnosed Schizophrenia and ≥1 Claim for Antipsychotics during Months after Index Date.
ADHD indicates attention-deficit/hyperactivity disorder.
Source: Truven Health MarketScan database; 2011.
Discussion
Our findings corroborate the findings of previous studies in terms of schizophrenia cost and resource utilization for a commercially insured population. Data regarding the prevalence of schizophrenia in commercially insured populations are limited. One study based on 1999 to 2002 claims data from 17 self-insured US employers representing 3 million commercially insured individuals aged <65 years reported a prevalence rate of 1.3 per 1000 persons, but it used criteria that only required 1 claim with a schizophrenia code during a 3-year period.10
Our analysis identified a lower prevalence rate of 0.54 per 1000 persons, which would be expected, because our criteria required 2 or more claims with a schizophrenia code in a 12-month period. The prevalence of schizophrenia in Medicaid populations has been more frequently reported, with the rate of 17 per 1000 persons in the Medicaid population aged <65 years.10
Nicholl and colleagues used medical and pharmacy claims data from the PharMetrics Integrated Database (1998–2007) to explore the effect of duration of illness on the cost of inpatient care and the overall economic burden of treatment in patients with recently diagnosed (N = 970) and with chronic (N = 2996) schizophrenia.9 A greater proportion of patients with recently diagnosed schizophrenia compared with patients with chronic schizophrenia were hospitalized (22.3% vs 12.4%, respectively; P <.001), and the former group spent a greater number of days in the hospital than the latter group (mean, 5.1 vs 3 days, respectively; P = .065). The average annual healthcare costs in recently diagnosed patients and in patients with chronic disease were $20,654 and $15,489, respectively, and inpatient costs constituted a higher proportion of total costs in the former group than in the latter group (62.9% vs 38.5%, respectively),9 which was similar to our findings.
Wilson and colleagues conducted a retrospective claims analysis using a large, privately insured claims-based database in California to determine the direct costs of treating schizophrenia in a privately insured setting (June 2001-May 2004) and compared the costs in newly diagnosed patients versus the costs of previously diagnosed patients.11 The overall direct annual treatment costs and schizophrenia-specific costs were $12,885 and $6220, respectively; inpatient services and medications comprised most of the schizophrenia-specific costs ($2762 and $2479, respectively). Patients with newly diagnosed schizophrenia had significantly higher inpatient costs than previously diagnosed patients ($4222 vs $2240, respectively; P <.05), and had significantly lower schizophrenia-specific medication costs ($1593 vs $2438, respectively; P <.05).11
Crown and colleagues used the MarketScan (now Truven Health) database, the same database that was used in our study, but with older data (1991–1993) to compare the expenditures of privately insured patients with schizophrenia who were hospitalized (N = 185) with data for patients who were not hospitalized (N = 480) in the 1-year period after the initial diagnosis.21 The unadjusted mean total healthcare costs were $20,161 in the hospitalized patients and $2966 in the nonhospitalized group; after adjusting for differences in the characteristics of the 2 groups, the incremental cost of hospitalization was $15,805.21
Our study shows that the reduction in costs after the index date is largely driven by a reduction in hospitalization and emergency department admission in subsequent months. This is expected, because the diagnosis itself can be triggered by a psychotic episode, resulting in an inpatient stay. In the months after the index date, patients may receive various interventions, including medications, psychosocial therapy, family therapy, and support groups, which may contribute to the stabilization of their disease.
As a result of the very high costs associated with inpatient services, the interventions that are most effective at lowering the probability of hospital admission or readmission for patients with schizophrenia have the potential to realize the greatest cost-savings. For example, a consistent cost driver for patients with schizophrenia is suboptimal adherence to antipsychotic therapy through its association with an increased risk for relapse and rehospitalization, as well as increased hospitalization costs.14,16,22
Sun and colleagues used data from 7 published articles on the economic impact of antipsychotic nonadherence among Medicaid patients with schizophrenia to estimate the costs of rehospitalization.16 The estimated total national rehospitalization cost associated with antipsychotic nonadherence in patients with schizophrenia in 2005 was $1.479 billion.16
dosReis and colleagues used retrospective Maryland Medicaid administrative data of 1727 patients with schizophrenia to study the relationship between antipsychotic treatment patterns and acute hospitalizations.14 The average duration of antipsychotic use was 6 months in any 1-year period and 4.5 years across the 7-year study period. The likelihood of hospitalization in patients with moderate adherence (50%-75% of eligible days) and light adherence (<50% of eligible days) to antipsychotic medication was 52% and 72% greater, respectively, than in patients with greater adherence (75%-100% of eligible days) to antipsychotic medication; furthermore, the average length of hospital stay was approximately 20% longer in light than in continuous users of antipsychotic medications.14
Marcus and Olfson analyzed the correlation between gaps in antipsychotic medication and hospital admission in patients with schizophrenia based on Medicaid data (2001–2003).22 The total number of annual acute care inpatient admissions of Medicaid patients with schizophrenia was approximately 87,000 (approximately 930,000 hospital days), at a total annual cost of $806 million. The investigators determined that improving adherence to antipsychotic medication could reduce the number of acute care admissions by approximately 12.3%, and the number of inpatient treatment days by approximately 13.1%, thereby saving an estimated $106 million in inpatient costs.22
Our analysis provides data regarding the prevalence of schizophrenia in a commercially insured population using recent data, as well as new HEDIS claims-based identification criteria, which has not been presented previously. In addition, more recent estimates of annual costs incurred by commercial payers across the populations of patients with newly diagnosed and chronic schizophrenia are provided, as well as a longitudinal view of resource utilization and costs during the first 2 years after diagnosis, showing that patients with schizophrenia represent a high-cost population for commercial payers.
Limitations
Our analysis was based on Truven Health MarketScan data, which we are unable to audit; however, we assumed that the data were accurate and comprehensive. Claims data limitations include the potential for provider coding inaccuracies, as well as the inability to identify clinical or psychosocial factors that may impact the mix of individual patient severity levels. We recognize that individuals conducting a similar analysis using other data sets or alternative coding logic would potentially produce results that are different from ours.
Our definition of “newly diagnosed” (ie, no claim with an ICD-9 diagnosis code of schizophrenia in any position in the 12 months before the index date) could have included some patients with schizophrenia who had infrequent contact with a healthcare provider in the 12 months before our assigned index date, although we expect that this would be a small portion of the population with schizophrenia.
Because we limited the longitudinal analysis to patients with 3 years of continuous eligibility and enrollment, we excluded individuals for whom the primary insurer changes insurers (MarketScan has consistent member identification numbers for individuals enrolled in the same plan annually), and we excluded patients with schizophrenia who lost insurance, such as those who were covered by their parents and reached the age of 26 years. These patients might have purchased a separate insurance policy or might have qualified for Medicaid, which we could not distinguish and, as such, the resource utilization patterns and costs for these patients are not reflected in this study.
Conclusions
Schizophrenia is a debilitating disease associated with substantial medical, social, and economic burdens. The 2013 addition of several schizophrenia HEDIS criteria will most likely bring increased attention from insurers to the population of patients with schizophrenia.19 The present study highlights the high cost of schizophrenia to commercial payers, with a total cost PPPM that is more than 4 times higher than for an average commercially insured person with similar demographics but without schizophrenia. Although the costs peak in the month of diagnosis, the average monthly costs remain disproportionately high throughout the 24-month follow-up period. Further claims data analyses that investigate patterns of care, drug therapy adherence patterns, and barriers to medication adherence among patients with schizophrenia are necessary to improve the quality of care for patients with schizophrenia and to more efficiently manage the cost of the care.
Stakeholder Perspective
Schizophrenia: “The Forgotten Illness”?
By Atheer A. Kaddis, PharmD
Senior Vice President, Sales and Business Development, Diplomat Specialty Pharmacy, Flint, MI
PAYERS: Schizophrenia, the forgotten illness? That may be too dramatic a description of the disease, but it nevertheless brings to light the lack of focus on schizophrenia as a disease that is rapidly growing in treatment costs, and the impact that it will have on commercial payers in the United States over the next decade. Schizophrenia is an important disease state that will become even more important to commercial insurers as a result of the healthcare coverage expansion beginning in 2014. The cost burden of the disease state is underestimated: more attention should be focused on this disease, and how to cost-effectively manage it in the future.
The article by Fitch and colleagues provides an excellent overview of the costs resulting from a diagnosis of schizophrenia, and it details how costs change over time after the index diagnosis. Of particular interest is that the mean per-patient per-month (PPPM) cost for a patient with schizophrenia was more than 4 times greater than the PPPM cost for a demographically adjusted population without schizophrenia. In addition, the highest cost was associated with the month of diagnosis (designated as the index month), which was a mean cost of $6601.
PROVIDERS/PATIENTS: What can we do about the costs of treating patients with schizophrenia? We do not have to look far to find meaningful ways to address schizophrenia costs, while also improving patient care. The answer can be found with appropriate medication therapy, focusing on medications with improved effectiveness and a lower incidence of side effects, and on improving medication adherence. In the current analysis, medications accounted for 25% of the overall costs of managing patients with schizophrenia compared with 42% for inpatient expenditures, and 33% for outpatient expenditures, respectively. Although medication costs would increase by choosing newer therapies and improving adherence, studies have shown that improving medication adherence can result in lower medical expenditures overall.1,2
The latest therapies to be approved for use in the United States include oral medications with significantly less impact on exacerbating negative symptoms (eg, social withdrawal, lack of motivation, etc). Newer therapies have also been introduced in depot formulations, which provide longer periods of controlling schizophrenia with only once-monthly dosing.3 Overall, this can result in improved medication adherence, which should reduce emergency department visits and hospitalizations resulting from symptoms of the disease.
PHARMACISTS: Although the newer medications are more expensive overall for payers, the impact on medical expenditure reductions should not be overlooked. Pharmacists can play a significant role in improving medication adherence, and this has been proven within the specialty pharmacy industry where medication possession ratios regularly exceed 80% as a result of adherence calls, compliance packaging, financial assistance, side-effect management, etc.4
POLICYMAKERS: If you believe that schizophrenia is the forgotten illness, you need not wait any longer, because the changes occurring in healthcare today, as they relate to schizophrenia, will bring this illness to the forefront for all payers. Understanding the costs and utilization associated with schizophrenia is the first step, but we need to focus next on providing cost-effective care for patients in need.
- 1.dosReis S, Johnson E, Steinwachs D, et al. Antipsychotic treatment patterns and hospitalizations among adults with schizophrenia. Schizophr Res. 2008; 101: 304–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marcus SC, Olfson M. Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull. 2008; 34: 173–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abilify Maintena (aripiprazole) extended-release injectable suspension, for intramuscular use [prescribing information]. Tokyo, Japan: Otsuka America Pharmaceutical, Inc; February 2013. [Google Scholar]
- 4.Tschida S, Aslam S, Khan TT. Managing specialty medication services through a specialty pharmacy program: the case of oral renal transplant immunosuppressant medications. J Manag Care Pharm. 2013; 19: 26–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
Biography

Kathryn Fitch
Source of Funding
This research was funded by Genentech, Inc.
Author Disclosure Statement
Ms Fitch provides consulting services to Genentech; Mr Iwasaki is an employee of Milliman, which provides consulting services to Genentech; and Ms Villa was an employee of and had stocks in Genentech at the time of writing.
Contributor Information
Kathryn Fitch, Ms Fitch is Principal and Healthcare Consultant, Milliman, Inc, New York, NY.
Kosuke Iwasaki, Mr Iwasaki is Director, Japan Healthcare Practice and Data Analytics, Milliman, Inc, New York, NY.
Kathleen F. Villa, Ms Villa was Senior Health Economist, Genentech, Inc, South San Francisco, CA, at the time of writing..
References
- 1.Regier DA, Narrow WE, Rae DS, et al. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993; 50: 85–94 [DOI] [PubMed] [Google Scholar]
- 2.Wu EQ, Birnbaum HG, Shi L, et al. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005; 66: 1122–1129 [DOI] [PubMed] [Google Scholar]
- 3.Chumakov I, Blumenfeld M, Guerassimenko O, et al. Genetic and physiological data implicating the new human gene G72 and the gene for D-amino acid oxidase in schizophrenia. Proc Natl Acad Sci U S A. 2002; 99: 13675–13680 Erratum in: Proc Natl Acad Sci U S A. 2002; 99: 17221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Schizophrenia. www.who.int/mental_health/management/schizophrenia/en/ Accessed September 26, 2013.
- 5.Switaj P, Anczewska M, Chrostek A, et al. Disability and schizophrenia: a systematic review of experienced psychosocial difficulties. BMC Psychiatry. 2012; 12: 193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tandon R, Nasrallah HA, Keshavan MS. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res. 2009; 110: 1–23 [DOI] [PubMed] [Google Scholar]
- 7.Jacob R, Chowdhury AN. Metabolic comorbidity in schizophrenia. Indian J Med Sci. 2008; 62: 23–31 [PubMed] [Google Scholar]
- 8.Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2006; 67 (suppl 9): 25–30 [PubMed] [Google Scholar]
- 9.Nicholl D, Akhras KS, Diels J, Schadrack J. Burden of schizophrenia in recently diagnosed patients: healthcare utilisation and cost perspective. Curr Med Res Opin. 2010; 26: 943–955 [DOI] [PubMed] [Google Scholar]
- 10.Wu EQ, Shi L, Birnbaum H, et al. Annual prevalence of diagnosed schizophrenia in the USA: a claims data analysis approach. Psychol Med. 2006; 36: 1535–1540 [DOI] [PubMed] [Google Scholar]
- 11.Wilson LS, Gitlin M, Lightwood J. Schizophrenia costs for newly diagnosed versus previously diagnosed patients. Am J Pharm Benefits. 2011; 3: 107–115 [Google Scholar]
- 12.Bartels SJ, Clark RE, Peacock WJ, et al. Medicare and Medicaid costs for schizophrenia patients by age cohort compared with costs for depression, dementia, and medically ill patients. Am J Geriatr Psychiatry. 2003; 11: 648–657 [DOI] [PubMed] [Google Scholar]
- 13.McDonald M, Hertz RP, Lustik MB, Unger AN. Healthcare spending among community-dwelling adults with schizophrenia. Am J Manag Care. 2005; 11 (8 suppl): S242–S247 [PubMed] [Google Scholar]
- 14.dosReis S, Johnson E, Steinwachs D, et al. Antipsychotic treatment patterns and hospitalizations among adults with schizophrenia. Schizophr Res. 2008; 101: 304–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charrier N, Chevreul K, Durand-Zaleski I. The cost of schizophrenia: a literature review. Encephale. 2013; 39 (suppl 1): S49–S56 [DOI] [PubMed] [Google Scholar]
- 16.Sun SX, Liu GG, Christensen DB, Fu AZ. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Curr Med Res Opin. 2007; 23: 2305–2312 [DOI] [PubMed] [Google Scholar]
- 17.Albers LJ, Musenga A, Raggi MA. Iloperidone: a new benzisoxazole atypical antipsychotic drug. Is it novel enough to impact the crowded atypical antipsychotic market? Expert Opin Investig Drugs. 2008; 17: 61–75 [DOI] [PubMed] [Google Scholar]
- 18.Bernardo M, Ramón Azanza J, Rubio-Terrés C, Rejas J. Cost-effectiveness analysis of schizophrenia relapse prevention: an economic evaluation of the ZEUS (Ziprasidone-Extended-Use-In-Schizophrenia) study in Spain. Clin Drug Investig. 2006; 26: 447–457 [DOI] [PubMed] [Google Scholar]
- 19.National Committee for Quality Assurance. HEDIS 2013. www.ncqa.org/Portals/0/HEDISQM/HEDIS2013/List_of_HEDIS_2013_Measures_7.2.12.pdf Accessed September 26, 2013.
- 20.Garfield RL, Zuvekas SH, Lave JR, Donohue JM. The impact of national health care reform on adults with severe mental disorders. Am J Psychiatry. 2011; 168: 486–494 [DOI] [PubMed] [Google Scholar]
- 21.Crown WH, Neslusan C, Russo PA, et al. Hospitalization and total medical costs for privately insured persons with schizophrenia. Adm Policy Ment Health. 2001; 28: 335–351 [DOI] [PubMed] [Google Scholar]
- 22.Marcus SC, Olfson M. Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull. 2008; 34: 173–180 [DOI] [PMC free article] [PubMed] [Google Scholar]