Abstract
Hybrid coronary revascularization combines the benefits of both percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) in the treatment of multivessel coronary artery disease (CAD) by combining the benefits of the LIMA-to-LAD graft and drug eluting stent (DES) to non-LAD regions. Through this approach, a patient receives the long-term benefit of the LIMA graft and avoids the morbidity of a full sternotomy and saphenous vein grafts. Available data related to outcomes following hybrid revascularization is limited to small studies. In this review we seek to provide an overview of hybrid revascularization in the era of modern drug eluting stent technology, discuss appropriate patient selection, and comment on future trial design. Additionally, we review the recent literature pertaining to the hybrid approach.
Keywords: Hybrid coronary revascularization, Coronary artery disease, Coronary artery bypass grafting, Percutaneous coronary intervention, Completion angiography, PCI, CABG
Introduction
Hybrid coronary revascularization is a treatment strategy for coronary artery disease (CAD), which offers an alternative to either traditional coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI) alone. With the goal being to reduce the risk of the procedure and maximize the benefit, hybrid therapy capitalizes on the strengths of each approach. Since first being described by Angelini and colleagues in 1996 [1], advances in both surgical and catheter based techniques have made hybrid therapy a more attractive option for the treatment of multi-vessel CAD. Using one of several minimally invasive techniques, the left anterior descending coronary artery is grafted with the left internal mammary (LIMA), and percutaneous intervention is applied to atherosclerotic disease in the left circumflex and right coronary arteries. In this approach, the well-established survival benefit of the LIMA graft [2] is capitalized upon and, being done with minimally invasive techniques, the increased morbidity of a full sternotomy is avoided. Additionally, the use of the LIMA graft confers benefit related to the relief of angina and long term patency. In addition to the requirement of a sternotomy for traditional CABG, another weakness has been the lower patency rates of saphenous vein grafts. Newer generation drug eluting stents have continued to improve long term patency following PCI, to rates similar to or even surpassing that of saphenous vein grafts [3–6].
CABG vs. PCI and the Role of HCR
Coronary revascularization has been shown to be superior to medical management in the setting of acute coronary syndrome. As an example, the reported median survival for patients with left main disease who undergo surgical revascularization is 13.3 years in comparison to 6.6 years for those managed medically [7]. Additionally, coronary revascularization may provide symptomatic relief in patients with angina, which may be especially important in patients with persistent angina despite medical therapy. To date, two dominant forms of coronary revascularization (i.e., coronary artery bypass grafting [CABG] and percutaneous coronary intervention [PCI]) have been established. Historically, CABG has been the preferential revascularization technique among specific subsets of patients, including those with diabetes, multi-vessel disease, systolic dysfunction, and left main disease. However, innovations in both stent design and minimally invasive operative techniques have the potential to change this balance. Hybrid revascularization combines the mortality benefit and higher rates of patency of the left internal mammary graft with the lower restenosis rates of DES in comparison to saphenous vein grafting for other coronary territories [8, 9••], all with a less invasive procedure than traditional CABG. While hybrid therapy has not been proven to be superior in any way to traditional CABG, multiple studies have suggested that it does not appear inferior [10–12, 13•, 14].
Within high risk subjects including diabetic patients with significant left coronary disease, revascularization via CABG utilizing a left internal mammary artery (LIMA) has been shown to have a substantial mortality benefit over PCI based revascularization strategies or medical management [15–17]. In comparison to the other revascularization approaches, LIMA has been shown to exceed 90 % patency at 10 years [15, 16, 18]. This high rate of success however, is not shared by saphenous vein grafts, which have reported failure rates up to 30 % at one year [19]. This was shown and confirmed in the 10 year outcome data from the Bypass Angioplasty Revascularization Investigation (BARI) trial [15]. Patients with a history of treated diabetes who were randomized to CABG with at least one arterial graft (n= 145) had a 10 year survival of 64.3 % in comparison to 39.4 % for those who underwent CABG with vein grafts only (n=33) and 45.5 % in those who were randomized to PTCA (n=63). Among participants not treated for diabetes, there was no significant difference in 10 year survival for patients who underwent CABG with or without the use of arterial grafts (75.3 % vs. 77.8 %).
CABG vs. PCI: Role of Bare Metal and Drug-Eluting Stents
Initial studies compared revascularization strategies for multivessel disease using a percutaneous transluminal coronary angioplasty (PTCA) based technique in comparison to CABG surgery. Hoffman et al. performed a meta-analysis of 13 randomized trials incorporating a total of 7964 patients with coronary disease who were randomized to strategies of CABG versus PTCA [20]. They found patients randomized to CABG had lower five-year mortality, citing a 1.9 % absolute survival advantage (p<0.02), as well as less angina. As had been noted in the individual studies, patients randomized to PTCA also had significantly more frequent revascularizations (P<0.001). Among patients who underwent placement of stents, however, the rate of revascularization was reduced by about half.
A subsequent meta-analysis of four trials (Arterial Revascularization Therapies Study, Stent or Surgery Trial, Argentine Randomized Trial of Percutaneous Transluminal Coronary Angioplasty Versus Coronary Artery Bypass Surgery in Multivessel Disease 2, and Medicine, Angioplasty, or Surgery Study 2) compared revascularization strategies of PCI with bare metal stents (BMS) (n=1518) versus CABG (n=1533) [21]. The primary combined outcome of death, myocardial infarction, and stroke occurred in 8.7 % of patients randomized to multivessel PCI versus 9.1 % of patients randomized to CABG (hazard ratio 0.95, 95 % CI 0.74 – 1.2). As seen in prior studies, patients who underwent PCI with BMS required repeat revascularization procedures more frequently than those who had CABG (18 % vs 4.4 %, hazard ratio 4.4, 95 % CI 3.3–5.9). Additionally, a higher percentage of patients who had CABG were angina free compared to those who underwent multivessel PCI (82 % vs. 77 %, P=0.002).
There are increasing data supporting the use of drug eluting stents (DES) over bare metal stents in many clinical situations. A recent meta-analysis compared outcomes of patients who underwent revascularization using drug eluting stents (n=18,538) versus CABG (n=15,740) [22]. All-cause mortality at 12 months (4.5 % vs 4.0 %, P=.92) and 24 months (6.2 % vs 8.4 %, P=.27) were not significantly different. The 30-day rate of myocardial infarction was similar for each group as well (DES 1.4 % vs. CABG 2.0 %, P=0.60). Patients who underwent DES placement had significantly lower 30 day rates of stroke (0.4 vs. 1.7 %, P <0.001), major cardiac and cerebrovascular events (3.6 % vs. 5.5 %, P<0.04) and all-cause mortality (0.9 % vs. 2.3 %, P<0.001). In comparison to those who underwent PCI, patients who underwent CABG had a significantly lower incidence of post-procedural myocardial infarction (4.7 % vs. 5.5 %, P=0.03), rate of revascularization (4.1 % vs. 22.2 %, P<0.001), and 12-month major adverse cardiac and cerebrovascular events (10.5 % vs. 16.7 %, P<0.001). Outcomes were similar among the subset of patients with multi-vessel coronary disease. Thus it appears that there are advantages and disadvantages to a “complete” CABG or PCI approach, even when drug-eluting stents are used. Hybrid revascularization, on the other hand, may combine the benefits of both.
Patient Selection for Hybrid Revascularization
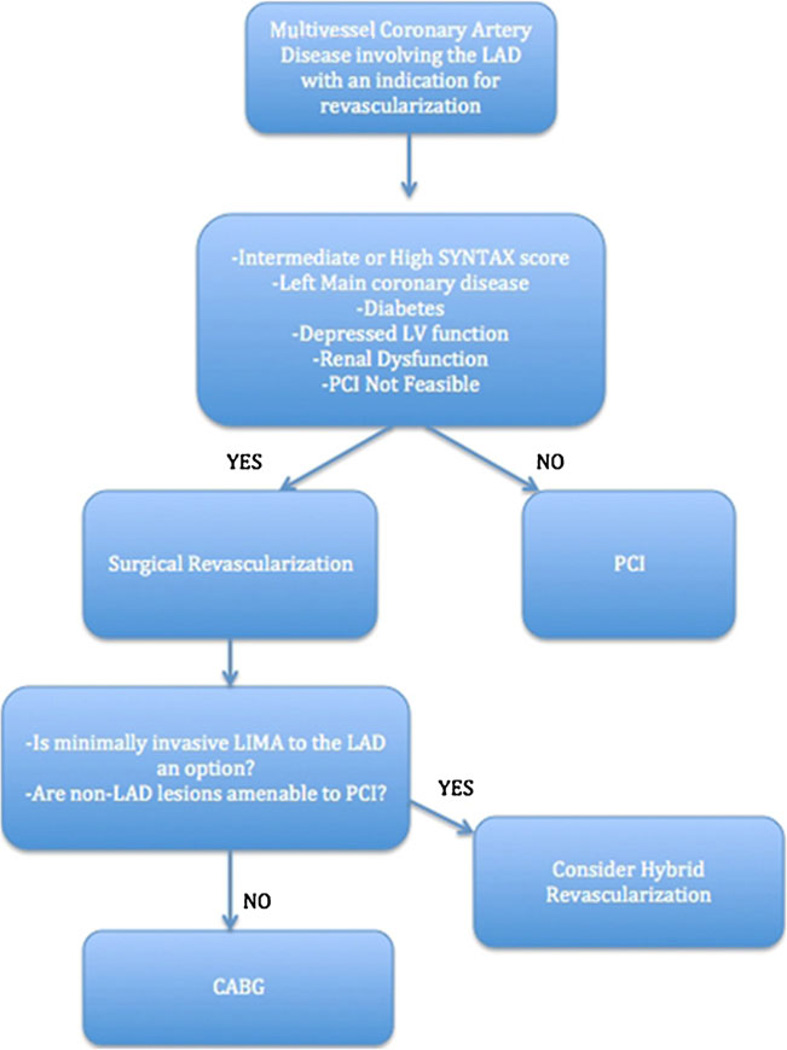
The patient population for whom hybrid therapy is optimal has not been well validated. In many patients for whom CABG is not an option, a hybrid approach offers benefit beyond PCI or medical therapy alone. Specifically, this is a reasonable consideration in treating patients with at least two-vessel disease (both an LAD and a non-LAD target) who are suboptimal surgical candidates, in whom the non-LAD lesions are amenable to PCI (Fig. 1). Such scenarios may occur in patients who have a lack of suitable conduits, a severely calcified aorta, or a non-graftable coronary vessel for which PCI remains an option. Tortuosity of the LAD, or LAD lesion characteristics that may require complex PCI, may also make a LIMA graft a more attractive option than PCI alone [23]. Patients with comorbidities that are known to increase surgical mortality may especially benefit from the minimally invasive techniques of hybrid therapy. Such patients include those with significant non cardiac pathology, recent history of myocardial infarction, prior sternotomy, poor left ventricular function (ejection fraction <0.40) [24], or severe extra-cardiac arteriopathy [25].
Fig. 1.
A proposed algorithm for considering revascularization approaches in patients with multivessel CAD. It should be noted that more evidence is needed prior to advocating hybrid therapy as a routine strategy
To qualify for the hybrid procedure, patients must meet the requirements of both the catheter-based and surgical component of the operation. Ideal candidates have lesions in the right coronary and circumflex arteries amenable to stent implantation. Ideally, to receive maximum benefit from the hybrid approach, it is important that these non-LAD lesions, and the patient in general, qualify for drug eluting stents (DES). The patient should be properly screened for conditions that may interfere with the longer period of dual antiplatelet therapy required after DES placement. These would include high risk of bleeding, a history of medication non-adherence, or upcoming procedures, which may require cessation of antiplatelet agents. Patients with non-LAD disease that is not amenable to successful PCI (i.e., long lesions requiring multiple stents, small diameter vessels, lesions previously treated with PCI, or other more challenging lesions) are also less suitable for hybrid therapy [13•]. When the complexity of a lesion as a potential target for PCI is considered, local expertise may also be a factor in determining the appropriateness of hybrid therapy for a given patient. Relative contraindications for hybrid therapy include a non-graftable LAD, hemodynamic instability, prior thoracic surgery that may complicate access to the LIMA, and a large body mass index (>40). In addition, patients with coronary artery disease characteristics such as chronic total occlusions, bifurcation lesions, etc., generally should receive traditional open CABG [13•].
In an effort to identify which therapy would better address an individual patient’s coronary disease, several investigators have sought to establish a system of stratification to predict clinical outcomes after interventions. In the landmark Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial, the SYNTAX Investigators reported on the predictive utility of a semi-quantitative angiographic scoring system that culminates in a SYNTAX score to characterize the coronary anatomy of patients with multi-vessel or complex CAD. An angiographic assessment is made of each lesion with a total cumulative score being calculated. They found that when patients were separated by SYNTAX score, there were no significant differences between CABG and PCI for those with low scores (0–22). Those with intermediate (23–32) to high (>33) scores who underwent PCI, however, had significantly higher incidences of MACCE at 36 months [26]. Although the SYNTAX score is useful in identifying patients at high risk following PCI, it does not identify patients at risk undergoing CABG, as the risk of bypass is determined by patient comorbidities. These risks are integrated in the European System for Cardiac Operative Risk Evaluation (EuroSCORE), in which clinical variables and a variety of risk factors such as age and renal function are considered in forming an additive score. The EuroSCORE is well validated in predicting event rates in the CABG group and is an independent predictor of MACCE following PCI as well. The EuroSCORE is insufficient for selection of CABG versus PCI, but is effective in identifying patients at high risk for mortality and poor outcome in either revascularization method [26]. We retrospectively analyzed the 30-day outcomes of 381 consecutive patients undergoing coronary bypass grafting (n=301) vs hybrid coronary revascularization (n=80) to identify patients best suited to hybrid therapy [9••]. After stratification of the groups by the SYNTAX score (≤32 vs ≥33) and the EuroSCORE (<5 vs ≥5), the composite endpoint (MACCE) and secondary endpoints (decline in renal function and bleeding) were determined. The 30-day rate of MACCE for hybrid vs CABG was similar in patients with low and intermediate SYNTAX score (≤32). However, patients with high SYNTAX scores (>32) and EuroSCOREs (>5) experienced better outcomes with standard CABG than with hybrid therapy. As in previous studies, outcomes in the CABG group were not influenced by the SYNTAX score, and the EuroSCORE alone did not discern MACCE. Our findings demonstrate the effect of lesion complexity on PCI outcome, whereas the success of CABG is related to the quality of the distal targets and patients' suitability for major surgery, and not to the coronary lesions themselves. While the principal finding of this study was that hybrid revascularization is safe and feasible for many patients with multivessel CAD, these findings suggest that it should be considered only with caution in patients with high (≥33) SYNTAX scores, and even more so in those who also have a high (>5) EuroSCORE.
Even within the hybrid strategy, a patient’s comorbidities or risk factors may indicate certain surgical approaches. Various minimally invasive techniques exist for the surgical portion of the procedure, and patient selection largely depends on the patient’s candidacy for one of these. An example of one of the techniques used for the LIMA to LAD grafting is minimally invasive direct coronary artery bypass (MIDCAB). In this method, LIMA mobilization is performed through a sternal-sparing, limited (typically 5–6 cm) anterior or left thoracotomy incision and the LIMA-to-LAD anastomosis is subsequently completed by hand or by use of robotic manipulation of the beating heart [25, 27]. Patients benefit from the smaller incision and the avoidance of aortic manipulation and cardiopulmonary bypass, thereby reducing morbidity (i.e., adverse neurologic events, bleeding, infection, and pulmonary complications) and possibly improving outcomes (i.e., earlier hospital discharge and recovery) [28]. To demonstrate technique specific contraindications, adequate exposure during a MIDCAB is likely to require single lung ventilation, thereby making patients with severe pulmonary disease less optimal candidates.
Other Technical Issues
Different strategies for hybrid therapy have been described in which revascularization is carried out in one visit to a hybrid operating suite, or the two procedures are conducted in a staged fashion in different locations separated by hours to days. Questions remain to be answered regarding the optimal order in which to conduct the procedures and advantages and disadvantages exist of each. Furthermore, questions remain related to the administration of antiplatelet therapy and its implications on timing of surgery. Small studies have reported reduction in length of hospital stay and more rapid return to work [10, 29], though overall cost advantage may be offset by the utilization of two relatively expensive procedures [30]. Large, randomized controlled trials comparing outcomes following hybrid therapy vs CABG or multi-vessel PCI have not been performed.
The ideal hybrid program has available a hybrid operating suite providing the option for one stop revascularization with completion angiography. Our group has previously described the experience from within Vanderbilt Heart and Vascular Institute related to completion angiography [23]. Reported was a series of 366 consecutive patients who underwent CABG with (n-112) or without (n-254) concomitant PCI, with completion angiography performed in all patients. In this series, 796 grafts were evaluated prior to chest closure. Of these, 97 (12 %) demonstrated defects, which required minor adjustment of the graft (n=22, 2.8 %), intraoperative open-chest PCI (unplanned hybrid, n=48, 6 %) or traditional surgical revision (n=27, 3.4 %). These findings strongly support the argument that completion angiography should be routinely utilized, whether the patient is undergoing planned hybrid revascularization, or as a quality control measure following traditional CABG. In centers with hybrid operating suites, graft defects can be identified immediately and addressed with either surgical revision or percutaneous intervention. We are currently performing follow up of this patient cohort with the intention of providing longer-term data on what advantage may exist to immediate correction of graft defects.
Review of Recent Literature and Future Trial Design
While large, randomized trials comparing hybrid revascularization have not been performed, smaller series continue to be published (Table 1). Halkos et al. recently published what may be the largest series to date, in which 147 patients who underwent hybrid revascularization between 2003 and 2010 were compared in a 4:1 ratio to patients undergoing multi-vessel off-pump CABG [13•]. Over a median follow up of 3.2 years, both survival and observed rates of major adverse events were similar. There was a higher rate of repeated revascularization in the hybrid group (12.2 % vs 3.7 %, p<0.001). The authors concluded that HCR was a safe and effective therapy in appropriately selected patients with multivessel CAD. Bachinsky and colleagues reported a series of 25 patients who underwent one stop hybrid revascularization, specifically by robotic assisted takedown of the LIMA [10]. When compared to well matched, low to moderate risk patients undergoing standard CABG, they reported similar rates of MACE. They did find lower rates of in hospital post-operative blood transfusions, shorter hospital stay, and earlier return to work in the hybrid group. These advantages came at the expense of higher total hospital cost, due to higher procedural cost. Similarly, Rab and colleagues reported on 22 patients with left main lesions who underwent minimally invasive LIMA to LAD grafting [11]. PCI of the LM, as well as other needed vessels was staged an average of 3 days later, following angiographic confirmation of LIMA patency. They reported no 30 day MACCE and at a mean of 38.8 month follow up, 21 of 22 patients were alive. The conclusion was that HCR represented a feasible alternative to CABG or PCI alone of an unprotected LM. In this series, PCI of the LM into the circumflex resulted in “jailing” of the LAD ostium in 18 of 22 patients. Considering that LAD perfusion was assured by the LIMA graft, no adverse effects were observed. This ability to avoid complex stenting techniques was felt to make the overall procedure both simpler and safer. Furthermore, the observation was made that LIMA grafting, as opposed to PCI, protects against future disease progression in the proximal segment of the LAD.
Table 1.
Summary of published hybrid revascularization studies
| Author | Year | Method | N | Mortality (%) |
PTCA/PCI restenosis (%, per patient) |
Mean/median follow-up (month) |
MACCE- free survival (%) |
|---|---|---|---|---|---|---|---|
| Angelini et al. [1] | 1996 | MidCAB/PTCA/PCI | 6 | 0 | n/r | n/r | n/a |
| Lloyd et al. [31] | 1999 | MidCAB/PTCA | 18 | 0 | 6 | 18 | 89 |
| Lewis et al. [32] | 1999 | MidCAB/PTCA/PCI | 14 | 0 | 0 | 1.44 | 93 |
| Zenati et al. [33] | 1999 | MidCAB/PCI | 31 | 0 | 10 | 11 | 90 |
| Wittwer et al. [34] | 1999 | MidCAB/PTCA/PCI | 35 | 0 | 7 | 11 | 87 |
| Isomura et al. [35] | 2000 | MidCAB/PTCA | 37 | 0 | n/r | 24 | 92 |
| De Canniere et al. [29] | 2001 | MidCAB/PTCA | 20 | 0 | 5 | 24 | 95 |
| Presbitero et al. [36] | 2001 | MidCAB/PTCA | 42 | 2 | 14 | 18 | 83 |
| Cisowski et al. [37] | 2002 | MidCAB/PTCA | 50 | 0 | 10 | 12 | 87 |
| Stahl et al. [38] | 2002 | MidCAB/PTCA | 54 | 0 | n/r | 12 | 87 |
| Riess et al. [39] | 2002 | MidCAB/PTCA | 57 | 0 | 24 | 24 | n/r |
| Lee et al. [40] | 2004 | TECAB/PCI | 6 | 0 | 16 | 12 | n/r |
| Davidavicius et al. [41] | 2005 | TECAB/PCI | 20 | 0 | 0 | 19 | 100 |
| Kiaii et al. [42] | 2005 | TECAB/PCI | 1 | 0 | 0 | 6 | 100 |
| Us et al. [43] | 2006 | MidCAB/PCI | 17 | 0 | 18 | 21 | 87 |
| Katz et al. [44] | 2006 | TECAB/PCI | 10 BMS 17 DES |
0 | 30 BMS 24 DES |
3 | 67 |
| Vassiliades et al. [45] | 2006 | TECAB/PCI | 47 DES | 0 | 6.6 | 7 | 90 |
| Gilard et al. [46] | 2007 | MidCAB/PCI | 70 DES | 1.4 | 1.4 | 33 | 97 |
| Kon et al. [47] | 2008 | MidCAB/PCI | 15 DES | 0 | 3 | 12 | 93 |
| Bonatti et al. [48] | 2008 | TECAB/PCI | 5 DES | 0 | 0 | 6 | 100 |
| Reicher et al. [49] | 2008 | MidCAB/PCI | 13 DES | 0 | 8 | 14 | 86 |
| Holzhey et al. [50] | 2008 | TECAB/PCI | 117 | 1.9 | 4.2 | 12 | 86 |
| Zhao et al. [23] | 2009 | Transsternal CABG/PCI | 87 DES 1 BMS 8 Both |
2.6 | 11 BMS 5 DES |
42 | 88 |
| Halkos et al. [13•] | 2011 | EndoACAB | 147 DES | 0.7 | 3.4 | 38.4 | 86 |
| Hu et al. [51] | 2011 | MidCAB/PCI | 104 | 0 | 1.9 (n/r) | 18 | 99 |
| Rab et al. [11] | 2012 | MidCAB/PCI | 22 DES | 4.5 | 0 | 38.8 | 95 |
| Leacche et al. [9••] | 2012 | MidCAB/PCI | 80 | 5 | N/A | 1 | 91 |
| Bachinsky et al. [10] | 2012 | Robotic MidCAB/PCI | 25 (17 DES) | 0 | 0 | 1 | 100 |
| Fedakar et al. [12] | 2012 | OPCABG/PTCA/PCI | 11* | 0 | 0 | 0.5 | 100 |
MACCE: any death, stroke, MI, and/or revascularization/restenosis
Unknown type of stent
According to ClinicalTrials.gov, the Hybrid Revascularization Observational Study, funded by the National Heart Lung and Blood Institute, has recently been completed. The largest observational study to date, with planned enrollment of over 6000 patients, this study was intended to inform the design of a pivotal comparative effectiveness trial and more optimally identify the population for whom hybrid therapy may be the better option. Primary outcomes are a composite of death, stroke, MI, or repeat revascularization with follow up over 18 to 21 months. To date, no data from this study have been published. As noted previously, there are no large randomized controlled trials evaluating hybrid coronary revascularization. The numerous studies that have been published to date vary in the surgical and interventional techniques, as well as patient selection, anti platelet strategies and one-stop vs staged approaches.
The ideal study design will be a multi centered, randomized controlled trial comparing hybrid revascularization to CABG. A design in which hybrid revascularization is compared directly to multi-vessel PCI will essentially be comparing the well-established advantage of the LIMA graft to LAD stenting, which is largely a non-contested issue. The hybrid vs CABG design will allow a true comparison of non LAD PCI to saphenous vein grafting, as well as allow for observations of what decrease in morbidity may be observed by avoiding a sternotomy. Additionally, we submit that the design will incorporate both staged and one stop procedures. Completion angiography should be an integral part as this is one of the advantages offered by the hybrid approach. Centers included in the trial should have surgeons experienced in minimally invasive techniques, as the technical expertise required could directly affect the outcome. As has been discussed extensively, a strong collaboration between the interventional cardiology and cardiovascular surgery departments is imperative to an individual programs success.
Conclusions
Combined surgical and percutaneous coronary revascularization is a valuable option for management of multivessel disease in centers with hybrid capabilities. The optimum approach utilizes a minimally invasive surgical technique for LIMA to LAD anastomosis in conjunction with percutaneous coronary intervention employing newer generation drug eluting stents for suitable lesions in non-LAD vessels. A number of selection factors including: Distal LM or proximal LAD disease, diabetes, systolic dysfunction, surgical risk, and coronary anatomy; may be important in deciding which patients may be candidates for a hybrid approach. Further studies are needed to better define the impact of a hybrid approach on patient outcome and to determine the patient population for whom this strategy may be best suited.
Footnotes
This article is part of the Topical Collection on Interventional Cardiology
Disclosure No potential conflicts of interest relevant to this article were reported.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Angelini GD, Wilde P, Salerno TA, Bosco G, Calafiore AM. Integrated left small thoracotomy and angioplasty for multivessel coronary artery revascularisation. Lancet. 1996;347(9003):757–758. doi: 10.1016/s0140-6736(96)90107-5. [DOI] [PubMed] [Google Scholar]
- 2.Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med. 1986;314(1):1–6. doi: 10.1056/NEJM198601023140101. [DOI] [PubMed] [Google Scholar]
- 3.Yeung AC, Leon MB, Jain A, et al. Clinical evaluation of the resolute zotarolimus-eluting coronary stent system in the treatment of de novo lesions in native coronary arteries. J Am Coll Cardiol. 2011;57(17):1778–1783. doi: 10.1016/j.jacc.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Puskas JD, Williams WH, Mahoney EM, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA. 2004;291(15):1841–1849. doi: 10.1001/jama.291.15.1841. [DOI] [PubMed] [Google Scholar]
- 5.Weisz G, Leon MB, Holmes DR, et al. Five-year follow-up after sirolimus-eluting stent implantation. J Am Coll Cardiol. 2009;53(17):1488–1497. doi: 10.1016/j.jacc.2009.01.050. [DOI] [PubMed] [Google Scholar]
- 6.Alfonso F, Perez-Vizcayno M-J, Hernandez R, et al. Sirolimus-eluting stents versus bare-metal stents in patients with in-stent restenosis: results of a pooled analysis of two randomized studies. Catheter Cardiovasc Interv. 2008;72(4):459–467. doi: 10.1002/ccd.21694. [DOI] [PubMed] [Google Scholar]
- 7.Caracciolo EA, Davis KB, Sopko G, et al. Comparison of surgical and medical group survival in patients with left main equivalent coronary artery disease. Long-term CASS experience. Circulation. 1995;91(9):2335–2344. doi: 10.1161/01.cir.91.9.2335. [DOI] [PubMed] [Google Scholar]
- 8.Mauri L, Orav EJ, Kuntz RE. Late loss in lumen diameter and binary restenosis for drug-eluting stent comparison. Circulation. 2005;111(25):3435–3442. doi: 10.1161/CIRCULATIONAHA.104.513952. [DOI] [PubMed] [Google Scholar]
- 9. Leacche M, Byrne J, Solenkova N, Reagan B, et al. Comparison of 30-day outcomes of coronary artery bypass grafting surgery verus hybrid coronary revascularization stratified by SYNTAX and euroSCORE. J Thorac Cardiovasc Surg. 2012:1–10. doi: 10.1016/j.jtcvs.2012.03.062.. This study identifies patient populations best suited for hybrid therapy using SYNTAX and euroSCORE.
- 10.Bachinsky WB, Abdelsalam M, Boga G, Kiljanek L, Mumtaz M, McCarty C. Comparative study of same sitting hybrid coronary artery revascularization versus off-pump coronary artery bypass in multivessel coronary artery disease. J Interv Cardiol. 2012;25(5):460–468. doi: 10.1111/j.1540-8183.2012.00752.x. [DOI] [PubMed] [Google Scholar]
- 11.Rab ST, Douglas JS, Jr, Lyons E, et al. Hybrid coronary revascularization for the treatment of left main coronary stenosis: a feasibility study. Cathet Cardiovasc Interv. 2011;80(2):238–244. doi: 10.1002/ccd.23312. [DOI] [PubMed] [Google Scholar]
- 12.Fedakar A, Tasar M, Rabus MB, Alsalehi S, Toker ME, Balkanay M. Hybrid coronary revascularization for the treatment of left main coronary artery disease in high-risk patients. Heart Surg Forum. 2012;15(1):E51–E55. doi: 10.1532/HSF98.20111116. [DOI] [PubMed] [Google Scholar]
- 13. Halkos ME, Vassiliades TA, Douglas JS, et al. Hybrid coronary revascularization versus off-pump coronary artery bypass grafting for the treatment of multivessel coronary artery disease. Ann Thorac Surg. 2011;92(5):1695–1702. doi: 10.1016/j.athoracsur.2011.05.090.. This is the largest published series to date, concluding that Hybrid therapy is safe and effective in appropriately selected patients.
- 14.Hu S-S, Xiong H, Zheng Z, et al. Midterm outcomes of simultaneous hybrid coronary artery revascularization for left main coronary artery disease. Heart Surg Forum. 2012;15(1):E18–E22. doi: 10.1532/HSF98.20111004. [DOI] [PubMed] [Google Scholar]
- 15.The BARI Investigators. The final 10-year follow-up results from the BARI randomized trial. J Am Coll Cardiol. 2007;49(15):1600–1606. doi: 10.1016/j.jacc.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 16.Serruys PW, Morice M-C, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 17.Willerson JT. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. Circulation. 1996;94(6):1194. doi: 10.1161/01.cir.94.6.1193. [DOI] [PubMed] [Google Scholar]
- 18.The BARI Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. The Bypass Angioplasty Revascularization Investigation (BARI) investigators. N Engl J Med. 1996;335(4):217–225. doi: 10.1056/NEJM199607253350401. [DOI] [PubMed] [Google Scholar]
- 19.Alexander JH, Hafley G, Harrington RA, et al. Efficacy and safety of edifoligide, an E2F transcription factor decoy, for prevention of vein graft failure following coronary artery bypass graft surgery: PREVENT IV: a randomized controlled trial. JAMA. 2005;294(19):2446–2454. doi: 10.1001/jama.294.19.2446. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman SN, TenBrook JA, Wolf MP, Pauker SG, Salem DN, Wong JB. A meta-analysis of randomized controlled trials comparing coronary artery bypass graft with percutaneous transluminal coronary angioplasty: one- to eight-year outcomes. J Am Coll Cardiol. 2003;41(8):1293–1304. doi: 10.1016/s0735-1097(03)00157-8. [DOI] [PubMed] [Google Scholar]
- 21.Mercado N, Wijns W, Serruys PW, et al. One-year outcomes of coronary artery bypass graft surgery versus percutaneous coronary intervention with multiple stenting for multisystem disease: a meta-analysis of individual patient data from randomized clinical trials. J Thorac Cardiovasc Surg. 2005;130(2):512–519. doi: 10.1016/j.jtcvs.2004.12.049. [DOI] [PubMed] [Google Scholar]
- 22.Yan TD, Padang R, Poh C, et al. Drug-eluting stents versus coronary artery bypass grafting for the treatment of coronary artery disease: a meta-analysis of randomized and nonrandomized studies. J Thorac Cardiovasc Surg. 2011;141(5):1134–1144. doi: 10.1016/j.jtcvs.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Zhao DX, Leacche M, Balaguer JM, et al. Routine intraoperative completion angiography after coronary artery bypass grafting and 1-stop hybrid revascularization. J Am Coll Cardiol. 2009;53(3):232–241. doi: 10.1016/j.jacc.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 24.Us MH, Basaran M, Yilmaz M, et al. Hybrid coronary revascularization in high-risk patients. Tex Heart Inst J. 2006;33(4):458–462. [PMC free article] [PubMed] [Google Scholar]
- 25.Umakanthan R, Leacche M, Zhao DX, Gallion AH, Mishra PC, Byrne JG. Hybrid options for treating cardiac disease. Semin Thorac Cardiovasc Surg. 2011;23(4):274–280. doi: 10.1053/j.semtcvs.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Lee M-S, Faxon DP. Revascularization of left main coronary artery disease. Cardiol Rev. 2011;19(4):177–183. doi: 10.1097/CRD.0b013e318219244d. [DOI] [PubMed] [Google Scholar]
- 27.Balaguer JM, Umakanthan R, Leacche M, Byrne JG. Minimally invasive cardiac surgery. Curr Probl Surg. 2012;49(9):529–549. doi: 10.1067/j.cpsurg.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 28.Narasimhan S, Srinivas VS, DeRose JJ., Jr Hybrid coronary revascularization. Cardiol Rev. 2011;19(3):101–107. doi: 10.1097/CRD.0b013e3182140330. [DOI] [PubMed] [Google Scholar]
- 29.de Canniere D, Jansens JL, Goldschmidt-Clermont P, Barvais L, Decroly P, Stoupel E. Combination of minimally invasive coronary bypass and percutaneous transluminal coronary angioplasty in the treatment of double-vessel coronary disease: two-year follow-up of a new hybrid procedure compared with “on-pump” double bypass grafting. Am Heart J. 2001;142(4):563–570. doi: 10.1067/mhj.2001.118466. [DOI] [PubMed] [Google Scholar]
- 30.Bonatti J, Lehr EJ, Vesely M, et al. Hybrid coronary revascularization – techniques and outcome. Eur Surg. 2011;43(4):198–204. [Google Scholar]
- 31.Lloyd CT, Calafiore AM, Wilde P, et al. Integrated left anterior small thoracotomy and angioplasty for coronary artery revascularization. Ann Thorac Surg. 1999;68(3):908–911. doi: 10.1016/s0003-4975(99)00555-x. discussion 911–2. [DOI] [PubMed] [Google Scholar]
- 32.Lewis BS, Porat E, Halon DA, et al. Same-day combined coronary angioplasty and minimally invasive coronary surgery. Am J Cardiol. 1999;84(10):1246–1247. A8. doi: 10.1016/s0002-9149(99)00538-x. [DOI] [PubMed] [Google Scholar]
- 33.Zenati M, Cohen HA, Griffith BP. Alternative approach to multivessel coronary disease with integrated coronary revascularization. J Thorac Cardiovasc Sur. 1999;117(3):439–444. doi: 10.1016/s0022-5223(99)70322-3. discussion 444–6. [DOI] [PubMed] [Google Scholar]
- 34.Wittwer T, Cremer J, Klima U, Wahlers T, Haverich A. Myocardial “hybrid” revascularization: intermediate results of an alternative approach to multivessel coronary artery disease. J Thorac Cardiovasc Sur. 1999;118(4):766–767. doi: 10.1016/S0022-5223(99)70035-8. [DOI] [PubMed] [Google Scholar]
- 35.Isomura T, Suma H, Horii T, Sato T, Kobashi T, Kanemitsu H. Minimally invasive coronary artery revascularization: off-pump bypass grafting and the hybrid procedure. Ann Thorac Surg. 2000;70(6):2017–2022. doi: 10.1016/s0003-4975(00)01839-7. [DOI] [PubMed] [Google Scholar]
- 36.Presbitero P, Nicolini F, Maiello L, et al. “Hybrid” percutaneous and surgical coronary revascularization: selection criteria from a single-center experience. Ital Heart J. 2001;2(5):363–368. [PubMed] [Google Scholar]
- 37.Cisowski M, Morawski W, Drzewiecki J, et al. Integrated minimally invasive direct coronary artery bypass grafting and angioplasty for coronary artery revascularization. Eur J Cardiothorac Surg. 2002;22(2):261–265. doi: 10.1016/s1010-7940(02)00262-2. [DOI] [PubMed] [Google Scholar]
- 38.Stahl KD, Boyd WD, Vassiliades TA, Karamanoukian HL. Hybrid robotic coronary artery surgery and angioplasty in multivessel coronary artery disease. Ann Thorac Surg. 2002;74(4):S1358–S1362. doi: 10.1016/s0003-4975(02)03889-4. [DOI] [PubMed] [Google Scholar]
- 39.Riess F-C, Bader R, Kremer P, et al. Coronary hybrid revascularization from January 1997 to January 2001: a clinical follow-up. Ann Thorac Surg. 2002;73(6):1849–1855. doi: 10.1016/s0003-4975(02)03519-1. [DOI] [PubMed] [Google Scholar]
- 40.Lee MS, Wilentz JR, Makkar RR, et al. Hybrid revascularization using percutaneous coronary intervention and robotically assisted minimally invasive direct coronary artery bypass surgery. J Invasive Cardiol. 2004;16(8):419–425. [PubMed] [Google Scholar]
- 41.Davidavicius G, Van Praet F, Mansour S, et al. Hybrid revascularization strategy: a pilot study on the association of robotically enhanced minimally invasive direct coronary artery bypass surgery and fractional-flow-reserve-guided percutaneous coronary intervention. Circulation. 2005;112(9 Suppl):I317–I322. doi: 10.1161/CIRCULATIONAHA.104.524264. [DOI] [PubMed] [Google Scholar]
- 42.Kiaii B, McClure RS, Kostuk WJ, et al. Concurrent robotic hybrid revascularization using an enhanced operative suite. Chest. 2005;128(6):4046–4048. doi: 10.1378/chest.128.6.4046. [DOI] [PubMed] [Google Scholar]
- 43.Kappetein AP, Feldman TE, Mack MJ, et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32(17):2125–2134. doi: 10.1093/eurheartj/ehr213. [DOI] [PubMed] [Google Scholar]
- 44.Katz MR, Van Praet F, de Canniere D, et al. Integrated coronary revascularization: percutaneous coronary intervention plus robotic totally endoscopic coronary artery bypass. Circulation. 2006;114(1 Suppl):I473–I476. doi: 10.1161/CIRCULATIONAHA.105.001537. [DOI] [PubMed] [Google Scholar]
- 45.Vassiliades TAJ, Douglas JS, Morris DC, et al. Integrated coronary revascularization with drug-eluting stents: immediate and seven-month outcome. J Thorac Cardiovasc Surg. 2006;131(5):956–962. doi: 10.1016/j.jtcvs.2005.10.058. [DOI] [PubMed] [Google Scholar]
- 46.Gilard M, Bezon E, Cornily JC, et al. Same-day combined percutaneous coronary intervention and coronary artery surgery. Cardiology. 2007;108(4):363–367. doi: 10.1159/000099110. [DOI] [PubMed] [Google Scholar]
- 47.Kon ZN, Brown EN, Tran R, et al. Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg. 2008;135(2):367–375. doi: 10.1016/j.jtcvs.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bonatti J, Schachner T, Bonaros N, et al. Simultaneous hybrid coronary revascularization using totally endoscopic left internal mammary artery bypass grafting and placement of rapamycin eluting stents in the same interventional session. The COMBINATION pilot study. Cardiology. 2008;110(2):92–95. doi: 10.1159/000110486. [DOI] [PubMed] [Google Scholar]
- 49.Reicher B, Poston RS, Mehra MR, et al. Simultaneous “hybrid” percutaneous coronary intervention and minimally invasive surgical bypass grafting: feasibility, safety, and clinical outcomes. Am Heart J. 2008;155(4):661–667. doi: 10.1016/j.ahj.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Holzhey DM, Jacobs S, Mochalski M, et al. Minimally invasive hybrid coronary artery revascularization. Ann Thorac Surg. 2008;86(6):1856–1860. doi: 10.1016/j.athoracsur.2008.08.034. [DOI] [PubMed] [Google Scholar]
- 51.Hu S, Li Q, Gao P, et al. Simultaneous hybrid revascularization versus off-pump coronary artery bypass for multivessel coronary artery disease. Ann Thorac Surg. 2011;91(2):432–438. doi: 10.1016/j.athoracsur.2010.10.020. [DOI] [PubMed] [Google Scholar]