Abstract
Objective
To identify scales that can establish a quantitative assessment of delirium symptoms in critically ill patients through a systematic review.
Methods
Studies that evaluated delirium stratification scales in patients hospitalized in intensive care units were selected in a search performed in the MedLine database. Validation studies of these scales and their target patient populations were analyzed, and we identified the examiner and the signs and symptoms evaluated. In addition, the duration of the application and the sensitivity and specificity of each scale were assessed.
Results
Six scales were identified: the Delirium Detection Score, the Cognitive Test of Delirium, the Memorial Delirium Assessment Scale, the Intensive Care Delirium Screening Checklist, The Neelon and Champagne Confusion Scale and the Delirium Rating Scale-Revised-98.
Conclusion
The scales identified allow the stratification and monitoring of critically ill patients with delirium. Among the six scales, the most studied and best suited for use in the intensive care units was the Intensive Care Delirium Screening Checklist.
Keywords: Delirium, Evaluation/methods, Scales, Sensitivity and specificity, Intensive Care Units
Abstract
Objetivo
Identificar escalas capazes de estabelecer uma avaliação quantitativa dos sintomas do delirium em pacientes graves por meio de uma revisão sistemática.
Métodos
Foram selecionados estudos que avaliaram escalas de estratificação de delirium em pacientes internados em unidades de terapia intensiva a partir de busca na base de dados MedLine. Os estudos de validação dessas escalas foram analisados, e foram identificados os pacientes alvos para aplicação, o avaliador, os sinais e sintomas avaliados, a duração da aplicação, além da sensibilidade e da especificidade de cada escala.
Resultados
Seis escalas foram identificadas: o Delirium Detection Score, o Cognitive Test of Delirium, a Memorial Delirium Assessment Scale, o Intensive Care Delirium Screening Checklist, a The Neelon and Champagne Confusion Scale e a Delirium Rating Scale-Revised-98.
Conclusão
As escalas identificadas permitem estratificação e acompanhamento do paciente grave com delirium. Dentre as seis escalas, a mais estudada e que melhor se adequa ao uso em unidade de terapia intensiva foi o Intensive Care Delirium Screening Checklist.
INTRODUCTION
Delirium is a common neurological dysfunction observed in intensive care units (ICU). Its incidence ranges from 5 to 92% according to the population studied,(1-4) and delirium is associated with high mortality, longer ICU hospitalizations, extended periods of mechanical ventilation, and long-term cognitive and functional deficits.(1-3,5-7)
Despite being a major neurological syndrome, delirium is underdiagnosed,(1,3) particularly in patients on mechanical ventilation.(3,6,8) Based on this observation, several tools have been developed to facilitate the diagnosis of delirium in critically ill patients.
The criteria recommended by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV), and the International Classification of Disease, 10th revision (ICD-10), are the most frequently used tools in individuals who are able to communicate verbally and are typically used by professionals specialized in the neuroscience field. In critically ill patients, the diagnostic scales most commonly used due to their simplicity and adequate accuracy are the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and the Intensive Care Delirium Screening Checklist (ICDSC).(9-11) However, both the DSM-IV and the ICD-10 as well as the CAM-ICU tools are dichotomous and do not permit stratification according to the severity of the condition. The DSM-IV and ICD-10 are based on the signs and symptoms necessary to diagnose or exclude a certain pathology (including delirium). In turn, the CAM-ICU was created based on the DSM-IV criteria to facilitate the diagnosis of delirium in the ICU and to allow the assessment of patients on mechanical ventilation (who are unable to communicate verbally). The CAM-ICU only permits diagnosis and does not establish a correlation with the severity of the condition.
The present study aimed to systematically review the scales that are able to establish a quantitative assessment of delirium symptoms in critically ill patients.
METHODS
An extensive search was performed in the MedLine database to identify studies that addressed delirium assessment and stratification scales in ICU patients. A search was performed for the keywords "delirium", "acute confusion", "confusion state", "confusional state", "acute confusion state" and "acute confusional state", the associated terms "scales", "scores", "state", "measures", "measurement", "questionnaires", "evaluation", "levels", "indices", "assessment", and "instrument" and the terms "ICU", "critical care", "ICU patients", "sensitivity", "specificity", and "accuracy".
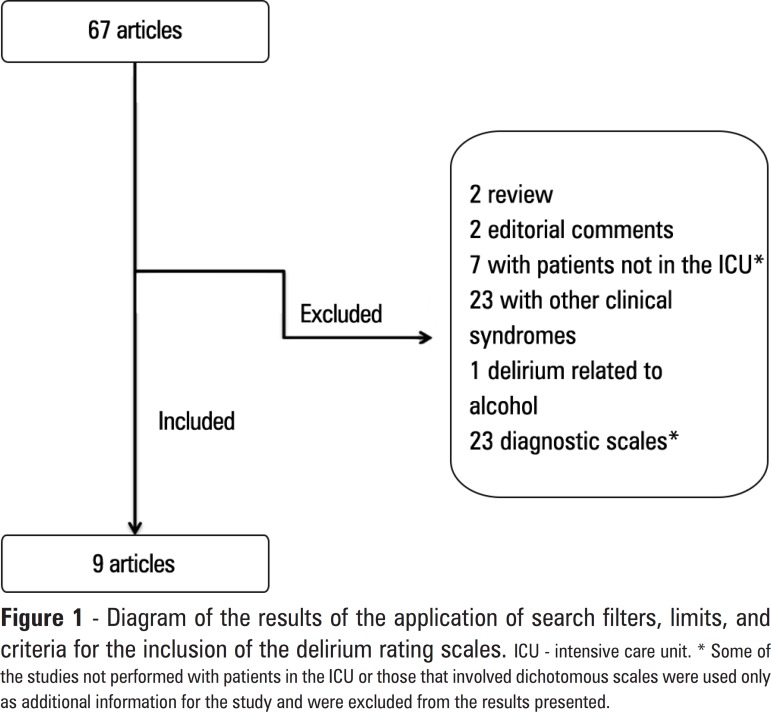
Subsequently, limits and inclusion criteria were established. Studies that addressed scales for a quantitative assessment of delirium were the main inclusion criterion. Only studies published in English and performed in adults (over 18 years) were analyzed. The results of the application of search filters, limits, and the inclusion criteria are described in figure 1.
Figure 1.
Diagram of the results of the application of search filters, limits, and criteria for the inclusion of the delirium rating scales.
ICU - intensive care unit. * Some of the studies not performed with patients in the ICU or those that involved dichotomous scales were used only as additional information for the study and were excluded from the results presented.
The final search strategy was as follows: ((((ICU) OR critical care) OR ICU patients)) AND ((((((((((delirium) OR confusional state) OR confusion state) OR acute confusion) OR acute confusion state) OR acute confusional state)) AND (((((((((((scales) OR scores) OR state) OR measurement) OR questionnaires) OR evaluation) OR indices) OR levels) OR measures) OR assessment) OR instruments))) AND (((sensitivity) OR specificity) OR accuracy)) AND (Humans[Mesh] AND (English[lang]) AND adult[MeSH]). Two authors independently performed the search for the studies. Possible divergences regarding the studies selection were resolved with a discussion between all of the authors.
After the selected studies were analyzed and the scales that would be used were identified, a new search for the specific name of each scale was performed to obtain further information.
RESULTS
After applying the search filter and considering the limits and inclusion criteria defined for the present study, six scales were selected that were able to quantitatively identify the symptoms of delirium (each one is briefly described and analyzed below). Table 1 describes the studies included in the review. Table 2 presents a comparative summary of all of the scales included in the study. The description of the variables present in each scale is shown in table 3.
Table 1.
Articles included in the review results
| Author | Journal | Year | Type of study | Scales addressed in the study |
| Included by the search criteria (N=9) | ||||
| Hart et al.(12) | Psychosomatics | 1996 | Validation | CTD |
| Hart et al.(13) | J Psychosom Res | 1997 | Primary | CTD (abbreviated form) |
| Bergeron et al.(10) | Intensive Care Med | 2001 | Primary | ICDSC |
| Otter et al.(14) | Neurocrit Care | 2005 | Validation | DDS |
| Van Rompaey et al.(15) | Crit Care | 2008 | Validation | NEECHAM |
| Osse et al.(16) | Interact Cardiovasc Thorac Surg | 2009 | Comparative | DRS-R-98 |
| Shyamsundar et al.(17) | J Crit Care | 2009 | Validation | MDAS |
| Gusmao-Flores et al.(11) | Clinics (São Paulo) | 2011 | Validation | ICDSC |
| Neufeld et al.(18) | Psychosomatics | 2011 | Validation | ICDSC |
| Included after a second search, specific for each scale (N=7) | ||||
| Breitbart et al.(19) | J Pain Symptom Manage | 1997 | Validation | MDAS |
| Immers et al.(20) | BMC Nurs | 2005 | Validation | NEECHAM |
| Fadul et al.(21) | Support Care Cancer | 2007 | Validation | MDAS |
| de Negreiros et al.(22) | Int J Geriatr Psychiatry | 2008 | Validation | DRS-R-98 |
| Radtke et al.(23) | Br J Anaesth | 2008 | Comparative | DDS |
| Radtke et al.(24) | World J Surg | 2010 | Comparative | DDS |
| Tomasi et al.(25) | J Crit Care | 2012 | Comparative | ICDSC |
Table 2.
Results and characteristics of the analyzed scales
| Scale | Author | Type of study | Target population | Examiner | Stratification | Sensitivity/specificity | Application time | Comments |
| Intensive Care Delirium Screening Checklist (ICDSC) | Gusmao-Flores et al.(11) | Validation for use in Brazil (translation to Portuguese) | ICU | Physician on duty and nurses | Score of 0 or 1 for each item, and a higher final score is correlated with greater severity. | 96%/72.4% for a suggested cut-off value of 4 points | 1-2 minutes | Scale adapted to Portuguese and validated for Brazil. Scale used more for diagnosis than for evaluation. |
| Cognitive Test of Delirium (CTD) | Hart et al.(12) | Validation | ICU | Physician on duty | The lower the score, the more severe the delirium. | 100%/95% for a suggested cut-off value ≤ 18 points | 10-15 minutes | Able to differentiate delirium from dementia. Use of non-verbal language. |
| Delirium Detection Score (DDS) | Otter et al.(14) | Evaluation and validation | ICU | Physician on duty | 7-10 = Mild 10-19 = Moderate >19 = Severe | 69%/75% for a suggested cut-off value >7 points | 3-4 minutes | Can only be applied to patients under light sedation (Ramsay ≤ 3). |
| Memorial Delirium Assessment Scale (MDAS) | Shyamsundar et al.(17) | Validation for use in developing countries | ICU and advanced stage cancer Patients not intubated | Residents or physicians on duty | Score for each item: 0 = absent, 1 = mild, 2 = moderate and 3 = severe. The higher the final score, the greater the severity. | 100%/95.5% for a suggested cut-off value of 10 points | 10-15 minutes | Validated in studies in developing countries without ideal ICU structures and staff. |
| The Neelon and Champagne Confusion Scale (NEECHAM) | Immers et al.(20) | Validation | ICU, not intubated | Nurses | 27 to 30 - normal patients 25 to 26 - group at risk of developing delirium 20 to 24 - mild delirium ≤ 19 - moderate to severe delirium | 97.2%/82.8% for a cut-off value ≤ 24 points | 3-4 minutes | Easy to apply. Should be used only as a tool for monitoring because it establishes a comparison with the previous 24 hours. |
| Delirium Rating Scale-Revised-98 (DRS-98-R) | de Negreiros et al.(22) | Validation | General UTI | Psychiatrists | Of the 16 items, 13 are used for severity assessment The higher the final score, the greater the severity. | 92.6%/94.6% for a suggested cut-off value of 20 | Old scale, validated for Portuguese and for use in Brazil. The validation was performed in the general patient population by psychiatrists. |
ICU – intensive care unit.
Table 3.
Variables present in each scale
| Scale | Number of variables | Signs and symptoms evaluated |
| Delirium Detection Score (DDS) | 8 items | Orientation Agitation Anxiety Hallucinations Seizures Paroxysmal sweating Sleep-wake cycle Tremors |
| Cognitive Test of Delirium (CTD) | 5 items | Attention/Orientation Vigilance Comprehension Memory |
| Memorial Delirium Assessment Scale (MDAS) | 10 items, divided in 2 groups (1st with 4 items and the 2nd with 6 items) | Attention/Orientation Immediate memory Behavior Perception Sleep-wake cycle Hallucinations Delusions Thinking alterations |
| Intensive Care Delirium Screening Checklist (ICDSC) | 8 items | Attention/Orientation Hallucinations Consciousness level Psychomotor agitation Alterations of language and behavior Sleep-wake cycle Fluctuating pattern of symptoms |
| The Neelon and Champagne Confusion Scale (NEECHAM) | 9 items, divided in 3 sub-scales | Attention/Orientation Obedience to commands Behavior (motor and verbal pattern and appearance) Physiological condition (vital signs, oxygen saturation and urinary incontinence) |
| Delirium Rating Scale-Revised-98 (DRS-98-R) | 16 items, 3 of them used only for diagnosis and the other 13 for stratification | Attention/Orientation Onset of symptoms Fluctuating nature Associated factors Sleep-wake cycle Immediate and delayed memory Illusions and hallucinations Delusions Emotional liability Language Disorders of thought Agitation or degradation Visual and special ability |
Delirium Detection Score
The Delirium Detection Score (DDS) is a validated scale that considers eight of the symptoms of delirium. Each one of these symptoms receives a score of 0, 1, 4, or 7 points.(14) The scale was created by modifying an instrument for the evaluation of alcohol withdrawal syndrome (Clinical Withdrawal Assessment for Alcohol - CIWA-Ar).(23,24) Therefore, it is a useful scale to assess the degree of delirium and guide treatment, and the tool may also serve as a diagnostic scale. The scale exhibited good correlation between examiners, as long as the examiners were previously trained in the scale's application.(24)
Cognitive Test of Delirium
The Cognitive Test of Delirium (CTD) evaluates five items, each of which receives a score of 0, 2, 4, or 6 points. Thus, the scale has a total of 30 points possible. There is no subdivision described in the literature that correlates the severity levels with the respective CTD values. However, the lower the CTD value, the worse the clinical outcome.(12) The scale is able to differentiate delirium from other psychiatric illnesses such as dementia.(12) Due to the long application time, an abbreviated form of the CTD was created, requiring only a few minutes of application time, but it has not yet been validated for routine use in the ICU.(13)
Memorial Delirium Assessment Scale
The Memorial Delirium Assessment Scale (MDAS) was initially created to diagnose delirium in patients with advanced cancer, but it has already been tested and validated for use in the general ICU.(17,21) The scale assesses variables of two major groups: cognition and behavior.(17,21) Based on the score obtained, the MDAS allows the stratification of delirium by severity.(19,21)
Intensive Care Delirium Screening Checklist
The Intensive Care Delirium Screening Checklist (ICDSC) is a scale for delirium stratification, but it can also be used as a diagnostic scale,(10) and the scale's application is easy and quick.(18) The ICDSC consists of eight observed variables that are compared with the assessment of the previous day, and increasing values on the ICDSC are compatible with severity stratification.(11) In addition, the ICDSC is useful in the diagnosis of subsyndromal delirium.(25) The ICDSC has the advantage of being adapted to Portuguese and validated for routine use in Brazil by Gusmao-Flores et al.(11) The ICDSC have been demonstrated to be a good scale to assess and monitor delirium.(10,11)
The Neelon and Champagne Confusion Scale
The Neelon and Champagne Confusion Scale (NEECHAM) was created as an instrument for nurses to assess delirium daily and has been validated for patients in the ICU(15) and those on mechanical ventilation.(20)
Delirium Rating Scale-Revised-98
The Delirium Rating Scale-Revised-98 (DRS-R-98) is the oldest and most traditional scale, created to measure the degree of delirium in patients. Among the scales that allow delirium stratification, the DRS-R-98 is one of the most well-known and frequently used in intensive care.(12,16,18) The DRS-R-98 consists of a scale with 16 items (3 of them used only at the moment of diagnosis and 13 used for stratification in successive evaluations). Each item receives 0 to 2 or 0 to 3 points, and the higher the final score, the higher the severity of the condition.(22) One of the difficulties of this scale is its complexity, as it requires training of qualified professionals, which sometimes generates divergent results.(16) The DRS-R-8 has already been studied and validated for Portuguese by Negreiros et al.(22)
DISCUSSION
Many scales are used to detect and evaluate patients with delirium. The present review identified six stratification scales used in ICU patients. The six scales have already been adequately validated in their original language. However, only the ICDSC and DRS-R-68(11,22) have been translated and validated for the Portuguese language. Other scales need to be validated specifically for use in sedated critically ill patients (DDS), as they should only be applied in patients with Ramsay scale <3.(14) The CTD and ICDSC have the advantage of having dichotomous variables (ICDSC) and using non-verbal language (CTD), allowing simpler and affordable evaluations for intubated patients. However, the level of sedation may influence the accuracy of the scale.(10)
Regarding the time of application of each instrument, the CTD and MDAS have a long application time for each patient, hindering the adherence for effective use in the ICU. The ideal tool would be one with an application time that would allow a periodic assessment during each shift in the ICU (due to the fluctuating nature of delirium), such as the ICDSC, NEECHAM or DDS.
Most of the variables assessed in each scale were chosen based on the diagnosis by the DSM-IV criteria. However, some variables incorporated other symptoms that are less common in delirium, which decreases the sensitivity of the tool.(23) One such example is the DDS, which evaluates signals such as tremors and paroxysmal sweating, findings that are not frequent in the course of delirium.(23) Another important aspect is that most scales have variables that assess hyperactive delirium, such as agitation, anxiety, and hallucinations, but few are able to assess hypoactive delirium, which is the most common subtype of the disease, with specificity.(18,23) The hypoactive nature of the disease (drowsiness, passivity, and inactivity), in most cases, is an intrinsic difficulty of disease, which makes it virtually unrecognizable without the use of a suitable tool.(18) The evaluation of behavior (and not just the agitation), attention, sleep-wake cycle, and the level of consciousness, such as the evaluation permitted by the ICDSC, allows for the evaluation of patients with hypoactive delirium. However, changes in the sleep-wake cycle, present in DDS, MDAS, and ICDSC, hinder precise evaluation, requiring longitudinal information, which can limit its use.
Scales such as the NEECHAM and ICDSC have the advantage of being previously validated, allowing the application both by nurses and nursing home residents, as long as they are properly trained.(11,20) With respect to the DRS-R-98, its validation study for use in Brazil was applied only by psychiatrists, although these physicians would not be responsible for its application in the ICU.(22) The other tools (DDS, MDAS, and CTD) were tested with the physician-on-duty as the evaluator. The MDAS was also validated when applied by residents.(17) However, training and qualification must be applied prior to the use of the various instruments. With previous training of the professionals, most scales exhibited good correlations between evaluators.(21,26) The subgroups of patients to be evaluated are another important factor to be considered when choosing the scale. The choice of the tool, based on the admission type and the severity of the patient, influences its accuracy and correlation with other scales.(27) The ICDSC was more sensitive than the CAM-ICU in the subgroup of surgical patients, for example.(27) Therefore, the choice of the scale that will be used is at the discretion of each intensive care unit, as long as it is correctly used with the most suitable professionals.
Currently, there are several consolidated diagnostic methods,(28) but those that use quantitative evaluation remain underused by the medical staff. The combination of diagnostic scales with validated instruments for stratification should always be considered to better understanding and monitoring patients with delirium. The DDS, for example, should only be used after the diagnosis is confirmed.(10) ICDSC, despite having been studied as a diagnostic tool, exhibits varied specificity.(10,29,30) Thus, the ICDSC can generate false-positive results.(25,27) However, meta-analyses and recent guidelines suggest that the CAM-ICU and ICDSC are the best-studied instruments for the diagnosis of delirium; therefore, they are suggested as the tools of choice for this purpose.(28,30,31)
The ICDSC was the most thoroughly studied tool among the studies identified,(10,11,25,28-30) suggesting that although there is not an ideal tool, the ICDSC is the best suited to evaluate the stratification of delirium. Another important characteristic of this tool is the possibility of diagnosing subsyndromal delirium,(25) which is a clinical condition with intermediate outcomes among patients with and without delirium.(32)
The diagnosis of delirium is already well established in the literature; however, its stratification is remains insufficiently described, which hindered the present review. The studies identified here are heterogeneous with respect to the target population, professional examiner, degree of sedation of the patients included, and the signs and symptoms evaluated, thus making impossible a comparison between the different scales. Therefore, only a descriptive analysis was possible. However, the present review identified the characteristics and the positive and negative aspects of each scale available in the literature for the stratification of ICU patients with delirium.
CONCLUSION
Six validated scales (only two validated for Portuguese) for the diagnosis of delirium in intensive care unit patients under different degrees of sedation (intubated or not) were identified. All of the scales exhibited good accuracy for the stratification of delirium. The most studied scale and the one best suited for use in the intensive care unit was the ICDSC because of its practicality, accuracy, and validation for the portuguese language.
Footnotes
Conflicts of interest: None.
REFERENCES
- 1.Spronk PE, Riekerk B, Hofhuis J, Rommes JH. Occurrence of delirium is severely underestimated in the ICU during daily care. Intensive Care Med. 2009;35(7):1276–1280. doi: 10.1007/s00134-009-1466-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kishi Y, Iwasaki Y, Takezawa K, Kurosawa H, Endo S. Delirium in critical care unit patients admitted through an emergency room. Gen Hosp Psychiatry. 1995;17(5):371–379. doi: 10.1016/0163-8343(95)00056-w. [DOI] [PubMed] [Google Scholar]
- 3.Lin SM, Liu CY, Wang CH, Lin HC, Huang CD, Huang PY, et al. The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med. 2004;32(11):2254–2259. doi: 10.1097/01.ccm.0000145587.16421.bb. [DOI] [PubMed] [Google Scholar]
- 4.Guenther U, Popp J, Koecher L, Muders T, Wrigge H, Ely EW, et al. Validity and reliability of the CAM-ICU Flowsheet to diagnose delirium in surgical ICU patients. J Crit Care. 2010;25(1):144–151. doi: 10.1016/j.jcrc.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 5.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 6.Mistarz R, Eliott S, Whitfield A, Ernest D. Bedside nurse-patient interactions do not reliably detect delirium: an observational study. Aust Crit Care. 2011;24(2):126–132. doi: 10.1016/j.aucc.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 7.van den Boogaard M, Pickkers P, Slooter AJ, Kuiper MA, Spronk PE, van der Voort PH, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ. 2012;344:e420. doi: 10.1136/bmj.e420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han JH, Zimmerman EE, Cutler N, Schnelle J, Morandi A, Dittus RS, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193–200. doi: 10.1111/j.1553-2712.2008.00339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29(7):1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27(5):859–864. doi: 10.1007/s001340100909. [DOI] [PubMed] [Google Scholar]
- 11.Gusmao-Flores D, Salluh JI, Dal-Pizzol F, Ritter C, Tomasi CD, Lima MA, et al. The validity and reliability of the Portuguese versions of three tools used to diagnose delirium in critically ill patients. Clinics (Sao Paulo) 2011;66(11):1917–1922. doi: 10.1590/S1807-59322011001100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hart RP, Levenson JL, Sessler CN, Best AM, Schwartz SM, Rutherford LE. Validation of a cognitive test for delirium in medical ICU patients. Psychosomatics. 1996;37(6):533–546. doi: 10.1016/S0033-3182(96)71517-7. [DOI] [PubMed] [Google Scholar]
- 13.Hart RP, Best AM, Sessler CN, Levenson JL. Abbreviated cognitive test for delirium. J Psychosom Res. 1997;43(4):417–423. doi: 10.1016/s0022-3999(97)00140-2. [DOI] [PubMed] [Google Scholar]
- 14.Otter H, Martin J, Bäsell K, von Heymann C, Hein OV, Böllert P, et al. Validity and reliability of the DDS for severity of delirium in the ICU. Neurocrit Care. 2005;2(2):150–158. doi: 10.1385/NCC:2:2:150. [DOI] [PubMed] [Google Scholar]
- 15.Van Rompaey B, Schuurmans MJ, Shortridge-Baggett LM, Truijen S, Elseviers M, Bossaert L. A comparison of the CAM-ICU and the NEECHAM Confusion Scale in intensive care delirium assessment: an observational study in non-intubated patients. Crit Care. 2008;12(1):R16. doi: 10.1186/cc6790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osse RJ, Tulen JH, Hengeveld MW, Bogers AJ. Screening methods for delirium: early diagnosis by means of objective quantification of motor activity patterns using wrist-actigraphy. Interact Cardiovasc Thorac Surg. 2009;8(3):344–348. doi: 10.1510/icvts.2008.192278. discussion 348. [DOI] [PubMed] [Google Scholar]
- 17.Shyamsundar G, Raghuthaman G, Rajkumar AP, Jacob KS. Validation of memorial delirium assessment scale. J Crit Care. 2009;24(4):530–534. doi: 10.1016/j.jcrc.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Neufeld KJ, Hayat MJ, Coughlin JM, Huberman AL, Leistikow NA, Krumm SK, et al. Evaluation of two intensive care delirium screening tools for non-critically ill hospitalized patients. Psychosomatics. 2011;52(2):133–140. doi: 10.1016/j.psym.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 19.Breitbart W, Rosenfeld B, Roth A, Smith MJ, Cohen K, Passik S. The Memorial Delirium Assessment Scale. J Pain Symptom Manage. 1997;13(3):128–137. doi: 10.1016/s0885-3924(96)00316-8. [DOI] [PubMed] [Google Scholar]
- 20.Immers HE, Schuurmans MJ, van de Bijl JJ. Recognition of delirium in ICU patients: a diagnostic study of the NEECHAM confusion scale in ICU patients. BMC Nurs. 2005;4:7. doi: 10.1186/1472-6955-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fadul N, Kaur G, Zhang T, Palmer JL, Bruera E. Evaluation of the memorial delirium assessment scale (MDAS) for the screening of delirium by means of simulated cases by palliative care health professionals. Support Care Cancer. 2007;15(11):1271–1276. doi: 10.1007/s00520-007-0247-6. [DOI] [PubMed] [Google Scholar]
- 22.de Negreiros DP, da Silva Meleiro AM, Furlanetto LM, Trzepacz PT. Portuguese version of the Delirium Rating Scale-Revised-98: reliability and validity. Int J Geriatr Psychiatry. 2008;23(5):472–477. doi: 10.1002/gps.1906. [DOI] [PubMed] [Google Scholar]
- 23.Radtke FM, Franck M, Schneider M, Luetz A, Seeling M, Heinz A, et al. Comparison of three scores to screen for delirium in the recovery room. Br J Anaesth. 2008;101(3):338–343. doi: 10.1093/bja/aen193. [DOI] [PubMed] [Google Scholar]
- 24.Radtke FM, Franck M, Schust S, Boehme L, Pascher A, Bail HJ, et al. A comparison of three scores to screen for delirium on the surgical ward. World J Surg. 2010;34(3):487–494. doi: 10.1007/s00268-009-0376-9. [DOI] [PubMed] [Google Scholar]
- 25.Tomasi CD, Grandi C, Salluh J, Soares M, Giombelli VR, Cascaes S, et al. Comparison of CAM-ICU and ICDSC for the detection of delirium in critically ill patients focusing on relevant clinical outcomes. J Crit Care. 2012;27(2):212–217. doi: 10.1016/j.jcrc.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 26.Devlin JW, Fong JJ, Fraser GL, Riker RR. Delirium assessment in the critically ill. Intensive Care Med. 2007;33(6):929–940. doi: 10.1007/s00134-007-0603-5. Review. [DOI] [PubMed] [Google Scholar]
- 27.Fagundes JA, Tomasi CD, Giombelli VR, Alves SC, de Macedo RC, Topanotti MF, et al. CAM-ICU and ICDSC agreement in medical and surgical ICU patients is influenced by disease severity. PloS One. 2012;7(11):e51010. doi: 10.1371/journal.pone.0051010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neto AS, Nassar AP Jr, Cardoso SO, Manetta JA, Pereira VG, Espósito DC, et al. Delirium screening in critically ill patients: a systematic review and meta-analysis. Crit Care Med. 2012;40(6):1946–1951. doi: 10.1097/CCM.0b013e31824e16c9. Review. [DOI] [PubMed] [Google Scholar]
- 29.George C, Nair JS, Ebenezer JA, Gangadharan A, Christudas A, Gnanaseelan LK, et al. Validation of the Intensive Care Delirium Screening Checklist in nonintubated intensive care unit patients in a resource-poor medical intensive care setting in South India. J Crit Care. 2011;26(2):138–143. doi: 10.1016/j.jcrc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Gusmao-Flores D, Figueira Salluh JI, Chalhub RA, Quarantini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of deliriuma systematic review and meta-analysis of clinical studies. Crit Care. 2012;16(4):R115. doi: 10.1186/cc11407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM, Coursin DB, Herr DL, Tung A, Robinson BR, Fontaine DK, Ramsay MA, Riker RR, Sessler CN, Pun B, Skrobik Y, Jaeschke R, American College of Critical Care Medicine Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. Review. [DOI] [PubMed] [Google Scholar]
- 32.Cole M, McCusker J, Dendukuri N, Han L. The prognostic significance of subsyndromal delirium in elderly medical inpatients. J Am Geriatr Soc. 2003;51(6):754–760. doi: 10.1046/j.1365-2389.2003.51255.x. [DOI] [PubMed] [Google Scholar]