Abstract
Objective
The objective of this study was to assess the correlation between the European System for Cardiac Operative Risk Evaluation (EuroSCORE) score and the risk of developing acute kidney injury in cardiac surgery patients.
Methods
This retrospective study was conducted at a tertiary hospital on consecutive cardiac surgery patients (e.g., valvular, ischemic and congenital heart diseases) between October 2010 and July 2011.
Results
One hundred patients were assessed. Among the 100 patients, six were excluded, including five because of prior kidney disease or dialysis therapy and one because of incomplete medical records. The primary surgical indications were myocardial revascularization in 55 patients (58.5% of cases) and valve replacement in 28 patients (29.8%). According to the EuroSCORE, 55 patients were classified as high risk (58.5%), 27 patients as medium risk (28.7%) and 12 patients as low risk (12.8%). In the postoperative period, patients were classified with the Risk, Injury, Failure, Loss and End-stage kidney disease (RIFLE) score. Among the 31 patients (33%) who displayed an increase in serum creatinine, 18 patients (19.1%) were classified as RIFLE "R" (risk), seven patients (7.4%) were classified as RIFLE "I" (injury) and six patients (6.5%) were classified as RIFLE "F" (failure). Among the patients who were considered to be high risk according to the EuroSCORE criteria, 24 patients (43.6%) showed acute kidney injury. Among the patients who were classified as medium or low risk, acute kidney injury occurred in 18.5 and 16.6% of the cases, respectively. The correlations between risk stratification (low, medium and high) and the EuroSCORE and postoperative RIFLE scores were statistically significant (p=0.03).
Conclusion
In the studied population, there was a statistically significant correlation between the EuroSCORE and the risk of developing acute kidney injury in the postoperative period after cardiac surgery.
Keywords: Acute kidney injury, Thoracic surgery, Postoperative complications, Renal dialysis, Severity of illness index, Risk assessment
Abstract
Objetivo
Verificar se há correlação entre valores do EuroSCORE e o risco de desenvolver lesão renal aguda em pacientes submetidos à cirurgia cardíaca.
Métodos
Estudo retrospectivo, realizado em hospital terciário, em pacientes consecutivos com indicação para abordagem cirúrgica cardíaca (valvares, isquêmicas e congênitas) entre outubro de 2010 a julho de 2011.
Resultados
Foram avaliados cem pacientes. Destes, seis foram excluídos (cinco por doença renal ou terapia dialítica prévias e um devido a informações incompletas no prontuário médico). As principais indicações cirúrgicas foram revascularização miocárdica em 55 pacientes (58,5% dos casos) e trocas valvares em 28 pacientes (29,8%). Conforme o EuroSCORE, 55 pacientes foram classificados como risco alto (58,5%), 27 pacientes como risco médio (28,7%) e 12 pacientes como risco baixo (12,8%). No período pós-operatório, 31 pacientes (33%) evoluíram com aumento da creatinina sérica (18 (19,1%) RIFLE "R"; 7 (7,4%) RIFLE "I"; e 6 (6,5%) RIFLE "F"). Na amostra considerada de alto risco pelos critérios do EuroSCORE, 24 pacientes (43,6%) apresentaram comprometimento renal agudo. Nos pacientes classificados como de médio e de baixo risco, ocorreu lesão renal aguda em 18,5 e 16,6% dos casos, respectivamente. A associação entre a estratificação de risco (baixo, médio e alto) do EuroSCORE e o escore do RIFLE pós-operatório foi estatisticamente significante (p=0,03).
Conclusão
Na população estudada, houve correlação estatisticamente significante entre o EuroSCORE e o risco de desenvolvimento de lesão renal aguda no pós-operatório de cirurgia cardíaca.
INTRODUCTION
Acute kidney injury (AKI) in the postoperative period after cardiac surgery has long been known to be a prevalent and severe complication.(1) This disorder persists despite technological advances in extracorporeal circulation, intensive care and intra- and postoperative practices. Research and identification in the preoperative period are inadequate, as they are mostly subclinical. Therefore, research and identification are potential sources of postoperative morbidity and mortality.
The laboratory screening for kidney injury in the general population is performed by measuring plasma creatinine levels and plasma creatinine clearance levels, which reflect the glomerular filtration rate. Compared to more promising biomarkers, serum creatinine offers a relatively late diagnosis of kidney injury in critically ill patients,(2,3) but serum creatinine measurements are essential within the Brazilian public healthcare system, as these tests are affordable and widely available in laboratories.
The use of serum creatinine for AKI classification was standardized with the establishment of the Risk, Injury, Failure, Loss and End-stage kidney disease (RIFLE) score,(4) which assists researchers and clinicians in classifying the severity of renal injury. There are two RIFLE criteria: serum creatinine at hospital admission and variation in the absolute value of serum creatinine. The patient may fulfill one or both of the criteria, and the criterion that leads to the worst classification should always be used.
When a preexisting kidney injury is suspected in the preoperative period of cardiac surgery, patients are commonly subjected to an assessment of renal function. The assessment is necessary because of the high prevalence of AKI (41.3%) that is associated with the surgery.(5) The diseases that cause silent renal alterations (e.g., hypertension and diabetes mellitus) are common comorbidities in cardiac patients with advanced age. Even without a known association with AKI, the postoperative increase in creatinine is associated with a worse prognosis in patients who underwent cardiac surgery for valve replacement.(6)
There is no standard to determine which individuals should be subjected to preoperative screening for previous renal dysfunction, and there is no definition of the level of preoperative renal dysfunction (which is provided by changes in serum creatinine or serum creatinine clearance levels); however, the level of preoperative renal dysfunction may have a negative effect on the postoperative outcome. Therefore, preoperative conditions in cardiac surgery patients who had not been diagnosed with nephropathy were correlated by correlating the European System for Cardiac Operative Risk Evaluation (EuroSCORE) score with the onset of postoperative AKI, which was defined by the RIFLE score.
METHODS
This retrospective study was performed at the Hospital de Base do Distrito Federal (HBDF), which is a tertiary institution of the Distrito Federal public health system. The study relied on pre- and postoperative data from patients who were consecutively admitted to the hospital with surgical indications for heart disease (e.g., valvular, ischemic and congenital types). The following inclusion criteria were used: adult subjects with an indication for cardiac surgery, the absence of previous nephropathy and clinically and laboratory confirmed results (considering serum creatinine levels of more than 1.3mg/dL and/or a creatinine clearance of less than 75mL/min/1.73m2 in women or 80mL/min/1.73m2 in men). The exclusion criteria were the presence of diagnosed kidney disease, the use of any form of renal replacement therapy prior to surgery and missing information in the medical records. The study was approved by the institution Research and Ethics Committee under number 349,630 that waived the need of informed consent due to its observational nature.
The following information was collected from the patient medical records: (1) epidemiological data, including age and gender; (2) clinical history data, including the presence of chronic obstructive pulmonary disease (COPD), extracardiac arteriopathy (a Doppler examination of the cervical vessels), neurological dysfunction, previous cardiac surgery, critical preoperative state, unstable angina, recent acute myocardial infarction (less than 90 days), the need for renal replacement therapy during hospitalization and death during the intensive care unit (ICU) stay; (3) echocardiogram data, including the presence of active endocarditis, left ventricular function and pulmonary hypertension; (4) factors associated with surgery, including the emergency procedure, revascularization surgery associated with valve surgery or corrections of a congenital defect, surgery of the thoracic aorta and the presence of a septal rupture after the myocardial infarction; and (5) laboratory data, including preoperative (the baseline creatinine clearance was calculated using the Cockcroft-Gault equation) and maximum creatinine levels (using the Jaffé method) during the ICU stay.
Based on the obtained data, the logistic and standard EuroSCORE was calculated, and the risk was classified as low, medium or high (scores of 0 to 2, 3 to 5 and 6 or more, respectively).
According to changes in serum creatinine levels during the postoperative period in the ICU, patients were classified as RIFLE "R" (risk: an increase of at least 50% and less than 100% of the baseline creatinine), RIFLE "I" (injury: an increase of at least 100% and less than 200%) and RIFLE "F" (failure: an increase of at least 200%). Patients whose serum creatinine level did not reach 50% of the baseline creatinine level were classified as not having AKI. Only the laboratory data were evaluated to determine the RIFLE score; the measurement of urine output was not considered.
The results were subjected to the following statistical tests: Pearson's chi-squared tests for categorical variables (gender, type of surgery, RIFLE score, progression to hemodialysis and death), one-way ANOVA tests for continuous variables with normal distributions (age, extracorporeal circulation time and serum creatinine levels) and the Kruskal-Wallis H test for continuous variables without a normal distribution (length of ICU stay). The software Statistical Package for the Social Sciences (SPSS) version 19.0 was used.
RESULTS
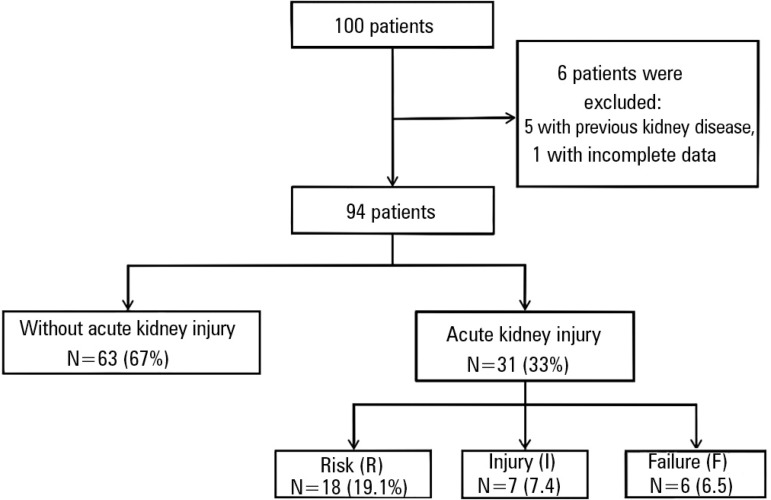
One hundred patients were admitted to the ICU and assessed from October 2010 to July 2011. Six patients were excluded, including five who had previous kidney disease or dialysis therapy and one who had incomplete medical records. A total of 94 patients remained in the study, including 63 patients (67%) who had no change in the baseline serum creatinine (less than 50%) during the ICU stay. The other 31 patients (33%) showed increases in creatinine that could be classifying according to the RIFLE score: 18 were classified as "R" (19.1%), seven were classified as "I" (7.4%) and six were classified as "F" (6.5%). According to the RIFLE score criteria, one-third of the patients (33%) had some form of AKI (Figure 1).
Figure 1.
Distribution of the patient sample according to the presence or absence of acute kidney injury and the RIFLE classification (R, I and F).
There was a prevalence of males in the sample (54 patients, 57.4%). The average age was 55.3±16.5 years, and the average length of ICU stay was 8.2±11.4 days (range, 2 to 89 days). The surgical indications were myocardial revascularization in 55 patients (58.5%), valve replacement in 28 patients (29.8%), congenital heart disease corrections in nine patients (seven atrial septal defect repairs, 7.4%; one ventricular septal defect repair, 1.1%; and one resection of the subaortic membrane, 1.1%) and left ventricular aneurysmectomies in two patients (2.1%). Nine surgeries (9.5%) were emergencies, eight (8.5%) of which were myocardial revascularizations and one (1%) of which was a surgical replacement of a mechanical aortic valve prostheses with acute dysfunction.
The EuroSCORE classified 58.5% of the patients as high risk, 28.7% of the patients as medium risk and 12.8% of the patients as low risk (n=55, 27 and 12 patients, respectively). There were five deaths in the sample population (5.3%). The data are summarized in table 1.
Table 1.
Epidemiological, laboratory and echocardiographic data
| Variables | Results | |
| Gender | ||
| Male | 54 (57.4) | |
| Female | 40 (42.6) | |
| Age (years) | 55.3±16.5 | |
| Type of surgery | ||
| Revascularization | 55 (58.5) | |
| Valve | 28 (29.8) | |
| Congenital | 9 (9.6) | |
| Others | 2 (2.1) | |
| ECC time (minutes) | 106.3±49.6 | |
| EuroSCORE | ||
| Logistic | 11±14 | |
| Standard | 6.4±3.6 | |
| EuroSCORE - Risk | ||
| Low | 12 (12.8) | |
| Medium | 27 (28.7) | |
| High | 55 (58.5) | |
| Baseline creatinine clearance (mL/min/1.73 m2) | 78.7±26.3 | |
| Creatinine | ||
| Baseline | 0.9±0.2 | |
| IPO | 1.0±0.3 | |
| Maximum | 1.5±1.0 | |
| RIFLE score | ||
| Risk | 18 (19.1) | |
| Injury | 7 (7.4) | |
| Failure | 6 (6.5) | |
| Length of ICU stay (days) | 8.2±11.4 | |
| Hemodialysis | 6 (6.5) | |
| Death | 5 (5.3) | |
ECC - extracorporeal circulation; IPO - immediate postoperative creatinine level; ICU - intensive care unit. The results are expressed as number (%) or average±standard deviation.
In the group that was classified as high risk by the EuroSCORE criteria (58.5% of the cases), 24 patients (43.6%) showed some type of acute kidney injury. In the medium- and low-risk groups, AKI was present in 18.5 and 16.6% of the cases, respectively.
Using the EuroSCORE classification, the sample of patients was divided into three groups (Table 2). In the postoperative period after cardiac surgery, a Pearson's chi-squared test showed a statistically significant correlation between the EuroSCORE risk stratification (low, medium and high) and the onset of AKI (p=0.03). There was also a statistically significant correlation between the EuroSCORE classification and the length of ICU stay (p=0.00). No other significant correlations were found in the analysis.
Table 2.
Epidemiological and laboratory data of the studied population: comparison based on the EuroSCORE classification
| Variable | EuroSCORE | p value | |||
| Low | Medium | High | |||
| (N=12) | (N=27) | (N=55) | |||
| Male gender | 10 (83.3) | 17 (63.0) | 27 (49.1) | 0.07 | |
| Age (years) | 42±16 | 54±13 | 59±17 | 0.01 | |
| Type of surgery | |||||
| Revascularization | 7 (58.3) | 16 (59.3) | 32 (58.2) | 1.00 | |
| Valve surgery | 5 (41.7) | 4 (14.8) | 19 (34.5) | 0.12 | |
| Others | 0 | 7 (25.9) | 4 (7.3) | ||
| ECC time (minutes) | 87±37 | 96±45 | 115±52 | 0.10 | |
| Baseline creatinine (mg/dL) | 1.06±0.27 | 0.94±0.16 | 0.99±0.24 | 0.29 | |
| IPO creatinine (mg/dL) | 1.09±0.18 | 1.04±0.34 | 1.09±0.38 | 0.84 | |
| Maximum creatinine (mg/dL) | 1.22±0.36 | 1.38±1.04 | 1.66±1.10 | 0.27 | |
| AKI | 2 (16.7) | 5 (18.5) | 24 (82.8) | 0.03 | |
| RIFLE score | |||||
| Risk | 2 (16.7) | 2 (7.4) | 14 (25.5) | ||
| Injury | 0 | 1 (3.7) | 6 (10.9) | ||
| Failure | 0 | 2 (7.4) | 4 (7.3) | ||
| Length of ICU stay (days) | 3.5±1.7 | 5±3 | 11±14 | 0.00 | |
| Hemodialysis | 0 | 2 (7) | 4 (7) | 0.62 | |
| Death | 0 | 3 (11) | 2 (3.6) | 0.48 | |
ECC - extracorporeal circulation; IPO - immediate postoperative creatinine dosage; AKI - acute kiney injury; ICU - intensive care unit. Pearson's chi-squared test, one-way ANOVA test and Kruskal-Wallis H test. The results are expressed as number (%) or average±standard deviation.
DISCUSSION
The causes of postoperative kidney injury after cardiac surgery can be attributed to the use of extracorporeal circulation that is associated with non-pulsatile blood flow, renal hypoperfusion and hypothermia.(7) In addition to this factor, the nephrotoxic effects of pre-, trans- and postoperative drug use must be considered.
The AKI that was observed in patients who were classified as high risk by the EuroSCORE (43.6%) surpassed the AKI that was identified in the medium- and low-risk patients (18.5% and 16.6%, respectively). None of the patients in this sample were subjected to a detailed evaluation of renal function; that is, their kidney function was considered to be within acceptable parameters. Many kidney injuries are subclinical, as the operative risk underestimates renal changes by only valuing the serum creatinine level without a concomitant functional evaluation. Consistent with this observation, the present creatinine clearance was 78.7±26.3mL/min/1.73m2 in the total sample, and the clearance in the high-risk patients was 71.1±22.7mL/min/1.73m2. In the postoperative period after cardiac surgery, there are possible independent risk factors associated with the onset of AKI, such as blood components and re-surgeries. A lack of this information was identified as a limitation of the present study.
Using the RIFLE score, AKI was detected in 33% of the patients. Antunes et al. obtained a value of 5.6% (which they classified as postoperative renal dysfunction), and they defined renal dysfunction as postoperative serum creatinine levels of more than 2.1mg/dL and an increase of 0.9mg/dL from the baseline level.(7) Using the RIFLE score, Machado et al. identified 48.7% of their patients as having AKI.(8) Various studies have significant variation in the incidence of AKI, which is likely because of conflicting definitions of cardiac surgery-associated acute kidney injury (CSA-AKI).(9) The present study confirms the high prevalence of this complication in this group of patients and highlights the importance of early detection and adequate treatment. Nevertheless, the incidence of patients who require hemodialysis remains low (6.5% in our series), which is consistent with the literature.(10)
The association between preoperative conditions and postoperative outcomes has been the subject of several publications. Roques et al. were the precursors of the EuroSCORE, which is a widely used predictor of hospital mortality that was created by the European Association of Cardiothoracic Surgery.(11-13) Although the EuroSCORE contains information related to renal function,(14,15) there are no studies showing the association between the EuroSCORE's level of preoperative risk and the level of postoperative renal dysfunction.
Among patients who underwent cardiac surgery, D'Onofrio et al.(16) showed a correlation between risky preoperative factors and the development of postoperative AKI. The present study only used the RIFLE criteria for the maximum level of postoperative serum creatinine. When assessing the preoperative risk factors, some of the factors are included in the EuroSCORE classification (e.g., age, peripheral arterial disease, left ventricular ejection fraction and thoracic aorta surgery). Some of the risk factors that were identified by Perez-Valdivieso et al.,(17) such as low left ventricular ejection fraction and emergency surgery, are also found in the EuroSCORE.
For detecting declining renal function, the relevance and sensitivity of progressive changes in serum creatinine are highlighted in the review of studies on CSA-AKI conducted by Shaw et al.(10) With no mention of the minimum urinary output that is achieved in the postoperative period after cardiac surgery, the authors emphasize that the rising serum creatinine levels may be a relevant parameter in the progression to AKI. As highlighted in the work of Prowle et al.,(18) the oliguria (urine output lower than 0.5mL/kg/h) is not a reliable marker of AKI but may serve as a precursor in the use of early biomarkers of kidney injury.
Despite the identification of several early preventive strategies of AKI post-cardiac surgery,(19) many of the strategies have not yet reached statistical power to be validated as guidelines. The risk assessment of AKI onset in these patients should be actively performed with the screening and identification of candidate risk factors. The modifiable risk factors should be optimized,(17) and specific perioperative protocols should be created for these patients, which will minimize the emergence of AKI. Knowledge of the specificities and background of patients should be combined with risk scores to guide surgery, anesthesia and ICU teams in each case.
This study has several limitations, including a small patient sample size and the retrospective analysis of information from medical records. These limitations prevented the acquisition of relevant information, such as the use of blood derivatives. Furthermore, the sample size did not allow the use of a multivariate analysis.
CONCLUSION
In the present population, this study showed that there is a statistically significant association between the values of the EuroSCORE and the risk of developing acute kidney injury in the postoperative period after cardiac surgery. Additionally, this study revealed a significant prevalence of acute kidney injury (according to RIFLE criteria) in the study patients.
Footnotes
Conflicts of interest: None.
This study was conducted at the Hospital de Base do Distrito Federal - HBDF - Brasília (DF), Brazil
REFERENCES
- 1.Abel RM, Buckley MJ, Austen WG, Barnett GO, Beck CH, Jr, Fischer JE. Etiology, incidence, and prognosis of renal failure following cardiac operations. Results of a prospective analysis of 500 consecutive patients. J Thorac Cardiovasc Surg. 1976;71(3):323–333. [PubMed] [Google Scholar]
- 2.Westhuyzen J, Endre ZH, Reece G, Reith DM, Saltissi D, Morgan TJ. Measurement of tubular enzymuria facilitates early detection of acute renal impairment in the intensive care unit. Nephrol Dial Transplant. 2003;18(3):543–551. doi: 10.1093/ndt/18.3.543. [DOI] [PubMed] [Google Scholar]
- 3.Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365(9466):1231–1238. doi: 10.1016/S0140-6736(05)74811-X. Comment in Lancet. 2005;365(9466):1205-6. [DOI] [PubMed] [Google Scholar]
- 4.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup Acute renal failure -definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–R212. doi: 10.1186/cc2872. Comment in Crit Care. 2007;11(2):411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yehia M, Collins JF, Beca J. Acute renal failure in patients with pre-existing renal dysfunction following coronary artery bypass grafting. Nephrology (Carlton) 2005;10(6):541–543. doi: 10.1111/j.1440-1797.2005.00496.x. [DOI] [PubMed] [Google Scholar]
- 6.Anderson RJ, O'Brien M, MaWhinney S, VillaNueva CB, Moritz TE, Sethi GK, et al. Mild renal failure is associated with adverse outcome after cardiac valve surgery. Am J Kidney Dis. 2000;35(6):1127–1134. doi: 10.1016/s0272-6386(00)70050-3. [DOI] [PubMed] [Google Scholar]
- 7.Antunes PE, Prieto D, Ferrão de Oliveira J, Antunes MJ. Renal dysfunction after myocardial revascularization. Eur J Cardiothorac Surg. 2004;25(4):597–604. doi: 10.1016/j.ejcts.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Machado MN, Miranda RC, Takakura IT, Palmegiani E, Santos CA, Oliveira MA, et al. Lesão renal aguda após revascularização do miocárdio com circulação extracorpórea. Arq Bras Cardiol. 2009;93(3):247–252. doi: 10.1590/s0066-782x2009000900008. [DOI] [PubMed] [Google Scholar]
- 9.Hoste EA, Cruz DN, Davenport A, Mehta RL, Piccinni P, Tetta C, et al. The epidemiology of cardiac surgery-associated acute kidney injury. Int J Artif Organs. 2008;31(2):158–165. doi: 10.1177/039139880803100209. [DOI] [PubMed] [Google Scholar]
- 10.Shaw A, Swaminathan M, Stafford-Smith M. Cardiac surgery-associated acute kidney injury: putting together the pieces of the puzzle. Nephron Physiol. 2008;109(4):55–60. doi: 10.1159/000142937. [DOI] [PubMed] [Google Scholar]
- 11.Roques F, Nashef SA, Michel P, Gauducheau E, de Vincentiis C, Baudet E, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15(6):816–822. doi: 10.1016/s1010-7940(99)00106-2. discussion 822-3. [DOI] [PubMed] [Google Scholar]
- 12.Roques F, Nashef SA, Michel P, EuroSCORE study group Risk factors for early mortality after valve surgery in Europe in the 1990s: lessons from the EuroSCORE pilot program. J Heart Valve Dis. 2001;10(5):572–577. discussion 577-8. [PubMed] [Google Scholar]
- 13.Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24(9):882–883. doi: 10.1016/s0195-668x(02)00799-6. [DOI] [PubMed] [Google Scholar]
- 14.Guaragna JC, Bodanese LC, Bueno FL, Goldani MA. Proposta de escore de risco pré-operatório para pacientes candidatos à cirurgia cardíaca valvar. Arq Bras Cardiol. 2010;94(4):541–548. doi: 10.1590/s0066-782x2010005000026. [DOI] [PubMed] [Google Scholar]
- 15.Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, Society of Thoracic Surgeons Quality Measurement Task Force The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 3--valve plus coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88(1) Suppl:S43–S62. doi: 10.1016/j.athoracsur.2009.05.055. [DOI] [PubMed] [Google Scholar]
- 16.D'Onofrio A, Cruz D, Bolgan I, Auriemma S, Cresce GD, Fabbri A, et al. RIFLE criteria for cardiac surgery-associated acute kidney injury: risk factors and outcomes. Congest Heart Fail. 2010;16(Suppl 1):S32–S36. doi: 10.1111/j.1751-7133.2010.00170.x. [DOI] [PubMed] [Google Scholar]
- 17.Perez-Valdivieso JR, Monedero P, Vives M, Garcia-Fernandes N, Bes-Rastrollo M, GEDRCC (Grupo Español de Disfunción Renal en Cirugía Cardiaca) Cardiac-surgery associated acute kidney injury requiring renal replacement therapy. A Spanish retrospective case-cohort study. BMC Nephrol. 2009;10:27–27. doi: 10.1186/1471-2369-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prowle JR, Liu YL, Licari E, Bagshaw SM, Egi M, Haase M, et al. Oliguria as a predictive biomarker of acute kidney injury in critically ill patients. Crit Care. 2011;15(4):R172. doi: 10.1186/cc10318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schetz M, Bove T, Morelli A, Mankad S, Ronco C, Kellum JA. Prevention of cardiac surgery-associated acute kidney injury. Int J Artif Organs. 2008;31(2):179–189. doi: 10.1177/039139880803100211. Comment in Int J Artif Organs. 2008;31(6):561. [DOI] [PubMed] [Google Scholar]