Abstract
Objectives
Identify patients at risk for intensive care unit readmission, the reasons for and rates of readmission, and mortality after their stay in the intensive care unit; describe the sensitivity and specificity of the Stability and Workload Index for Transfer scale as a criterion for discharge from the intensive care unit.
Methods
Adult, critical patients from intensive care units from two public hospitals in Porto Alegre, Brazil, comprised the sample. The patients' clinical and demographic characteristics were collected within 24 hours of admission. They were monitored until their final outcome on the intensive care unit (death or discharge) to apply the Stability and Workload Index for Transfer. The deaths during the first intensive care unit admission were disregarded, and we continued monitoring the other patients using the hospitals' electronic systems to identify the discharges, deaths, and readmissions.
Results
Readmission rates were 13.7% in intensive care unit 1 (medical-surgical, ICU1) and 9.3% in intensive care unit 2 (trauma and neurosurgery, ICU2). The death rate following discharge was 12.5% from ICU1 and 4.2% from ICU2. There was a statistically significant difference in Stability and Workload Index for Transfer (p<0.05) regarding the ICU1 patients' outcome, which was not found in the ICU2 patients. In ICU1, 46.5% (N=20) of patients were readmitted very early (within 48 hours of discharge). Mortality was high among those readmitted: 69.7% in ICU1 and 48.5% in ICU2.
Conclusions
The Stability and Workload Index for Transfer scale showed greater efficacy in identifying patients more prone to readmission and death following discharge from a medical-surgical intensive care unit. The patients' intensive care unit readmission during the same hospitalization resulted in increased morbidity, mortality, length of stay, and total costs.
Keywords: Intensive care units, Patient readmission, Patient discharge, Mortality rate, Quality of health care, Hospitalization
Abstract
Objetivo
Identificar os pacientes com risco de retornar à unidade de terapia intensiva, os motivos e as taxas de readmissão, e a mortalidade após a estadia na unidade de terapia intensiva; além de descrever a sensibilidade e a especificidade da escala Stability and Workload Index for Transfer como critério de alta da unidade de terapia intensiva.
Métodos
Pacientes adultos críticos de unidades de terapia intensiva de dois hospitais públicos de Porto Alegre (RS) compuseram a amostra. Nas primeiras 24 horas de internação, foram obtidas informações clínicas e demográficas dos pacientes. Eles eram monitorados até seu destino final na unidade de terapia intensiva (óbito ou alta) para a realização do Stability and Workload Index for Transfer. Os óbitos durante a primeira admissão na unidade de terapia intensiva foram desconsiderados, seguindo-se com o acompanhamento dos demais pacientes, pelo sistema eletrônico dos hospitais, para a identificação das altas, óbitos e readmissões.
Resultados
As taxas de readmissão foram 13,7% na unidade de terapia intensiva 1 - clínica cirúrgica (UTI1) e 9,3% na unidade de terapia intensiva 2 - trauma e neurocirurgia (UTI2); as mortes após a alta da unidade de terapia intensiva foram 12,5% na UTI1 1 e 4,2% na UTI2. Houve diferença estatística significativa do Stability and Workload Index for Transfer (p<0,05) nos pacientes da UTI1 em relação ao desfecho, o que não se repetiu nos da UTI2. Na UTI1 46,5% (N=20) dos pacientes foram readmitidos de forma precoce (em menos de 48 horas de alta). A mortalidade entre os readmitidos foi alta, 69,7% (UTI1) e 48,5% (UTI2).
Conclusão
A escala Stability and Workload Index for Transfer apresentou maior eficácia em reconhecer os pacientes mais propensos à readmissão e a óbitos após a alta em uma unidade de terapia intensiva clínica-cirúrgica. A readmissão dos pacientes na unidade de terapia intensiva, durante a mesma hospitalização, resultou em aumento da morbidade e mortalidade, de tempo de permanência e de custos totais.
INTRODUCTION
The introduction of advanced technologies, the increasing number of elderly, and the severity of cases have resulted in increasingly expensive intensive care, making the clinical effectiveness and cost-effectiveness of intensive care units (ICUs) aspects of utmost importance in the care of critically ill patients.(1) In that context, the ICU readmission rates and unexpected deaths following discharge, during the same hospital stay, have been used as indicators of healthcare quality.(1-4)
ICU discharge decision-making is affected by the socioeconomic pressure to grant discharge as soon as possible, towards reducing hospital costs and ensuring bed turnover, with the efforts to reduce the use, expenditure, and length of stay in the ICU.(1) Therefore, patients who still require intensive treatment may have their discharge moved forward to release beds for more severe patients. Furthermore, the criteria used to decide the patients' ICU discharge are extensive and quite subjective, contributing to undue indications and risks for patients.(1-3)
The consequence of these inconsistencies is the early discharge from the ICU to wards, which may expose patients to inappropriate levels of care, resulting in unexpected deaths or ICU readmissions during the same hospitalization.(1-5) The readmission rates reported in the international literature range from 0.9 to 19%,(6,7) with mortality rates among these patients of 26 to 58%.(3,8-10) The readmitted patients show worsening or aggravation of their original condition and increased morbidity, mortality, length of hospital stay, and total costs.(1,2,5)
The main objective of this study was to identify patients at risk for ICU readmission, as well as the reasons and fees associated with readmission and mortality following their stay in the ICU, during the same hospital stay. Our secondary objectives were to describe the sensitivity and specificity of the Stability and Workload Index for Transfer (SWIFT) scale as a criterion for discharge from the ICU and to facilitate the implementation of strategies for quality care.
METHODS
This prospective observational cohort study was conducted at the ICUs of two large and highly complex, non-university, public hospitals located in the city of Porto Alegre, Rio Grande do Sul, Brazil. This study was approved by the institutional Research Ethics Committees, which dismissed the need for informed consent given its observational nature.
The ICU labeled "1" was a medical-surgical (general) ICU, with 40 beds of hospitalization for patients with a serious medical event requiring intensive care, in a general hospital with 801 beds. The ICU labeled "2" was an ICU specialized in caring for trauma victims (car accidents, gunshot wounds, stab wounds, extensive burns, and others) and postoperative neurosurgery patients (tumors and vascular diseases of the central nervous system, brain and spinal cord trauma) and had a capacity of 20 beds in a hospital of 290 beds. Both units belonged to the same hospital group and featured technological characteristics, healthcare structures, and bed numbers compliant with Ordinance GM/MS No. 3,432 of August 12, 1998 and the Brazilian Intensive Care Medicine Association (AMIB) standards.
All critical or potentially critical adult patients, aged 18 years or above, of both genders, who were hospitalized for more than 24 hours in an ICU between May 2008 and March 2009 were included in the study, which was conducted in accordance with the Declaration of Helsinki. Patients referred for palliative care units, following discharge from the ICU, and those who were transferred to other hospitals were excluded from the study. The planned ICU readmissions were also excluded from the analysis, "planned" meaning required for continuation of diagnosis or treatment.
Data were collected by trained evaluators using a specific form, consisting of three parts: (1) ICU admission, (2) ICU outcome, and (3) monitoring following ICU discharge.
The first part was performed within 24 hours of ICU admission and enabled the recording of patients' clinical and demographic characteristics, including identification, gender, age, origin, reason for admission, and comorbidities.
This was followed by the daily monitoring of patients, until their ICU outcome (death or discharge), at which time the second part of the instrument was filled in. Subjects who died during the first ICU admission were disregarded from the final analysis of the study. In cases of ICU discharge, the ward destination, total length of stay, Glasgow Coma Scale (GCS) score, and the last arterial blood gas analysis were surveyed, and the SWIFT, a simple numerical index, developed by Gajic et al.,(11) to predict risk for ICU readmission and unexpected deaths following discharge during the same hospital stay, was assessed.
The final part was filled in after completing all study patients' monitoring using the hospitals' electronic system to identify discharges, deaths, and readmissions. The reason for readmission, length of stay, and ICU or hospital outcome (discharge or death) were surveyed in cases of ICU readmission or new ICU discharge, respectively.
In this study, we use the terms "readmission" to characterize the event of returning to the ICU during the same hospitalization as the first ICU admission; "early readmission" to characterize the events that occurred within 48 hours after ICU discharge; and "unexpected deaths" to characterize deaths that occurred within 7 days after ICU discharge.
All data were collected from the patients' records during their ICU admission, and their monitoring was performed daily using the hospital electronic patient tracking system until their outcome (discharge or death). The readmission data refer to patients who remained hospitalized following ICU discharge during the same hospital stay; hospital readmissions at different hospitals were not analyzed.
The Statistical Package for the Social Sciences (SPSS) software, version 17.0, was used for data tabulation and analysis. Absolute and percentage distributions of univariate and bivariate nonparametric (continuous) variables and parametric (categorical) variables were assessed by descriptive statistics and expressed as the mean ± standard deviation or number (percentage). Correlations were assessed using analysis of variance (ANOVA) for unpaired variables and Pearson's chi-squared test for categorical variables. Significance was defined as p<0.05.
Receiver operating characteristic (ROC) curves were designed to identify the SWIFT's overall accuracy (area under the curve, AUC) according to the patients' outcome, and AUCs were compared using Pearson's chi-squared test. The areas were estimated by points and 95% confidence intervals (95% CIs).
The ICU data were analyzed separately, given the populations' heterogeneity, which could limit and/or allow the extrapolation of the results for each ICU.
RESULTS
Fifty-three of the 1,030 patients evaluated in the study period were excluded because of methodological criteria (transfers to other hospitals, planned readmissions, and ICU hospitalizations less than 24 hours). In total, 61.2% of the 977 patients included in the analysis were men, and the mean age was 53.69±17.63 years. The ICU1 inpatients' mean Acute Physiology and Chronic Health Disease Classification System II (APACHE II) score during the study period was 19.6 points; no ICU severity score was used in ICU2 during the time this study was conducted.
Table 1 shows the patients' outcomes during the first ICU admission and following ICU discharge during the same hospital stay. A high mortality was noted in ICU1 and considerable readmission rates prior to hospital discharge in both units.
Table 1.
Clinical and demographic characteristics of the intensive care units
| ICU | All | Readmitted | Deaths on the ward | Non-readmitted | p value | |
| N | 1 | 546 | 43(13.7) | 39 (12.5) | 231 (73.8) | |
| 2 | 431 | 33 (9.3) | 15 (4.2) | 304 (70.5) | ||
| Male gender | 1 | 317 (58.1) | 23 (53.5) | 23 (59) | 130 (56.3) | 0.882 |
| 2 | 281 (65.2) | 19 (57.5) | 9 (60) | 205 (67.4) | 0.355 | |
| Age (years) | 1 | 57.75±16.3 | 61.91±13.18 | 58.67±15.5 | 56.81±16.24 | 0.319 |
| 2 | 48.56±17.8 | 56.03±17.91 | 61.60±19.84 | 45.55±17.28 | 0.000 | |
| Length of stay in ICU (days) | 1 | 13.7±19.22 | 15.30±17.69 | 16.79±19.3 | 13.91±15.98 | 0.571 |
| 2 | 10.04±8.8 | 8.44±8.43 | 12.40±6.03 | 10.39±9.11 | 0.314 | |
| GCS | 1 | 13.46±2.03 | 12.6±1.86 | 11.67±2.74 | 13.92±1.69 | 0.000 |
| 2 | 12.64±2.28 | 11.35±2.52 | 11.67±1.54 | 12.83±2.23 | 0.000 | |
| PaO2/FiO2 | 1 | 340.44±152.48 | 337.98±152.6 | 368.9±272.8 | 336±121.7 | 0.460 |
| 2 | 361.45±126 | 374.68±124.7 | 389.2±113.5 | 358.61±127.4 | 0.538 | |
| PaCO2 | 1 | 41.31±9.9 | 39.30±9.53 | 40.59±8.43 | 41.81±10.18 | 0.280 |
| 2 | 39.5±6.7 | 39.15±6.8 | 38.60±8.14 | 39.53±6.70 | 0.842 | |
| SWIFT | 1 | 20.34±9.87 | 23.53±9.65 | 26.28±10.5 | 18.74±9.29 | 0.000 |
| 2 | 20.87±10.9 | 22.24±11.5 | 25.27±8.00 | 20.50±10.98 | 0.194 |
ICU - intensive care unit; GCS - Glasgow Coma Scale; SWIFT -Stability and Workload Index for Transfer; PaO2 - arterial oxygen pressure; FiO2 - fraction of inspired oxygen; PaCO2 - partial pressure of carbon dioxide. Results expressed as number (%) or mean ± standard deviation. Mortality at 1st admission to ICUs: ICU1, 233 patients (42%) and ICU2, 78 patients (18%).
Table 1 also shows the clinical and demographic characteristics of the samples. The lack of statistically significant differences between men and women regarding outcome was noted in both ICUs. In ICU2, readmitted patients were older than non-readmitted patients, while in ICU1, age did not significantly correlate with outcome. There was no significant difference between groups regarding the mean length of ICU stay. The readmitted patients in both ICUs showed a more severe lowering of consciousness (lower GCS score) on the day of discharge than non-readmitted patients. There were no differences in the ratio of arterial oxygen pressure/fraction of inspired oxygen (PaO2/FiO2) or partial pressure of carbon dioxide (PaCO2) between ICU-nonreadmitted and ICU-readmitted patients. There was a statistically significant difference in SWIFT between the groups from ICU1 regarding the outcome, while there were no significant differences in that scale between the groups from ICU2.
The main diagnoses reported by ICU1 patients leading to the need for ICU hospitalization were pneumonia (35.7%), renal failure (29.3%), sepsis (18.5%), unspecified shock (16.5%), chronic obstructive pulmonary disease (12.3%), heart failure (11.4%), acute myocardial infarction (10.1%), post-cardiorespiratory arrest (8.1%), stroke (6.6%), and tuberculosis (5.1%). In ICU2, they were traumatic brain injury (28.9%), hemorrhagic stroke (21.6%), central nervous system tumor (18.1%), non-traumatic (17.2%) and traumatic (2.5%) subarachnoid hemorrhage (SAH), and spinal cord injury (2%), with other causes totaling 9.8%.
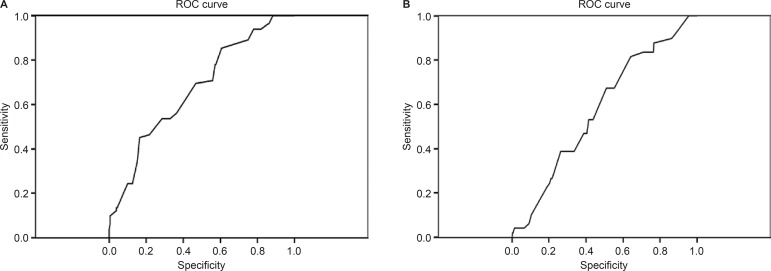
The SWIFT scale had better sensitivity and specificity in ICU1, according to the ROC curves shown in figures 1(A) and (B)
Figure 1.
Stability and Workload Index for Transfer (SWIFT) scale ROC curves. (A) Intensive Care Unit 1. (B) Intensive Care Unit 2. A: Area under the curve = 0.670±0.34; p<0.001 and 95% CI=0.603-0737; B: Area under the curve = 0.577±0.041; p=0.085; 95% CI=0.496-0.658.
Patients readmitted to ICUs are characterized in table 2. A considerable percentage of early readmissions (within 48 hours from ICU discharge) was observed in ICU1, and high mortality was associated with readmission in both units. Finally, table 2 also shows the time between ICU discharge and deaths occurring in wards; the deaths within 7 days of ICU2 discharge stand out (40%).
Table 2.
Characteristics of intensive care unit readmissions and deaths on the wards
| ICU1 - medical-surgical | ICU2 -trauma | ||
| Time between discharge and readmission (days) | 13.14±15.56 | 11.70±11.20 | |
| Readmission less than 48 hours after discharge - N (%) | 20 (46.5) | 5 (15.2) | |
| Reason for readmission | |||
| Pneumonia/bronchopneumonia | 3 (13.6) | 7 (21.2) | |
| Sepsis/septic shock | 5 (22.7) | 8 (24.2) | |
| Post-CRA | 5 (22.7) | 3 (9.1) | |
| Decreased level of consciousness | 0 (0) | 2 (6.1) | |
| Need for intensive care following surgical reoperation | 5 (22.7) | 0 (0) | |
| Neurosurgical PO reoperation | 0 (0) | 9 (27.3) | |
| Others | 4 (18.1) | 3 (9) | |
| Length of stay (days) | 16.33±17 | 10.67±8.90 | |
| ICU outcome | |||
| Death | 18 (41.9) | 14 (42.4) | |
| Discharge | 25 (58.1) | 19 (57.6) | |
| Hospital outcome | |||
| Death | 5 (20.8) | 2 (10.5) | |
| Discharge | 19 (79.2) | 16 (84.2) | |
| Hospital transfer | 0 (0) | 1 (5.3) | |
| Total mortality | 23 (69.7) | 16 (48.48) | |
| Time between discharge from the ICU and death on the ward | 22.13±18.83 | 14.36±15.8 | |
| Death within 1 week of ICU discharge | 11 (28.2) | 6 (40) | |
ICU - intensive care unit; CRA - cardiorespiratory arrest; PO - postoperative. Results expressed as number (%) or mean ± standard deviation.
DISCUSSION
Readmissions and deaths following ICU discharge have been widely discussed in the international literature, but several published studies have been limited by the small sample size, the retrospective nature of the data collection, and heterogeneity of the populations involved.(1,5,11)
In this study, ICU1 showed a predominantly elderly cohort, mostly males, with prolonged hospital stay (13.7 days), mainly due to cardiorespiratory conditions. Mortality rates in the first admission (42%) and after readmission (69.7%) were high in ICU1. The rates of readmission (13.7%) and death within 7 days from ICU1 discharge (28.2%) are within the ranges reported in the international literature, although almost half the patients (46.5%) were readmitted to ICU1 within 48 hours of discharge, suggesting the prevalence of early discharges and confirming the need for and importance of defining the criteria for ICU discharge. The SWIFT index significantly predicted readmission to this ICU, although the patients' origin, length of hospital stay, and respiratory variables (PaO2/FiO2 and PaCO2) showed no significant differences between groups, with significant values only in the neurological item (GCS).
ICU2 attended to relatively younger patients, mostly males, with prolonged mean hospital stay (10.04 days) caused by trauma and neurosurgical postoperative complications. Patients who were readmitted and died following discharge from that ICU were significantly older. The ICU2 rates of readmission (9.3%) and mortality at first admission (18%) are within the ranges reported in the literature, but the mortality rate associated with readmitted patients (48.48%) and deaths within 7 days of ICU2 discharge (40%) were high. The SWIFT index did not significantly predict readmission to that ICU, with significant values only in GCS.
Prevalence studies of ICU readmission conducted in Brazil, Europe, Canada, and Australia have reported values ranging from 0.9 to 19%(6,7), and both ICUs from this study fall within that prevalence range. Rosenberg and Watts(1) reported a 6% mean readmission rate (range 5 to 14%) in a systematic review of studies that included 4,684 patients. In another recent review of 20 studies, Elliot(8) reported 7.8% mean readmission rate (range 0.89 to 19%). The readmission rates reported in the literature for surgical ICU patients range from 0.89 to 9.4%.(1,3,6,12-15) Snow et al.(10) reported a 9.4% mean readmission rate in surgical ICUs but failed to exclude patients who died in the ICU from the analysis. Nishi et al.(6) reported a 0.89% readmission rate, but they only considered those that occurred within 48 hours of discharge (early readmissions).
The ICU1 data regarding the patients' age and gender corroborate previous studies, which indicate a preponderance of elderly men in ICUs, albeit without significant differences between groups regarding outcome. ICU2, however, had relatively younger male patients because it treats trauma emergencies, and patients who were readmitted to ICU2 and died following ICU discharge were significantly older than those non-readmitted.
There was no significant difference between the two ICUs in the length of ICU stay during the first admission, unlike other studies that have reporting readmitted patients' stays to be at least twice as long as that of the non-readmitted patients.(1)
The early readmissions to ICU1 (46.5%) and unexpected deaths following discharge in ICU2 (40%) were high. These rates are considered indicators of care quality by the Critical Care Medical Association and may reflect poor care quality and/or early ICU discharge.(1,5) These patients might require longer periods of hospital stay, more intensive ICU care, or discharge to an intermediate care unit rather than to a standard ward.
The currently used criteria for ICU discharge may also contribute to undue indications and risks for patients. They were suggested and first published in 1988. The research on which those criteria were based was relatively scant, albeit with comparative results regarding the use of those guidelines for ICU discharge decision-making. Well-defined discharge criteria may result in shorter ICU stay, without compromising the quality of care to patients, thereby resulting in lower readmission and mortality rates.(1,4) Furthermore, the pressure to release intensive care beds and to ensure turnover given the high demand of patients requiring intensive care and the number of existing vacancies-a situation where the less serious patients must have their ICU discharge moved forward to give way for the more serious patients-may have contributed to those high rates. Nevertheless, in both ICU1 and ICU2, the ICU-admitted patients considered "less serious" only vacated beds for others who were "more serious" after 24 hours of observation under spontaneous ventilation.
The main reasons for readmissions in both populations studied were post-cardiorespiratory arrest (CRA) (22.7%), need for intensive care following surgical reoperation (22.7%), postoperative neurosurgical reoperation (recurrence of neurovascular condition) (27.2%), sepsis (24.2%), and pneumonia (21.2%). Rosenberg and Watts(1) reported in their systematic review that the most common reasons for ICU readmission are pulmonary complications (hypoxemia, inadequate pulmonary hygiene, pneumonia, and respiratory failure) and cardiac abnormalities (arrhythmias, congestive heart failure, and cardiac arrest), followed by upper-gastrointestinal bleeding and neurological deficit. The proportion of readmissions for CRA in this study suggests that these patients were at high risk of discharge to the ward (hospital rooms) and that they contributed to the high mortality following readmission. In ICU2, readmissions mainly resulted from the need for neurosurgical reoperation due to recurrence of severe conditions (for example, recurrence of brain tumor), which also contributed to the high mortality.
The mortality of readmitted patients was high in both ICUs (69.7% in ICU1 and 48.5% in ICU2). The ICU1 patients' mortality rate was higher than that found in other studies, inside and outside Brazil, which were 12 to 58%.(3,9,10,16) The mortality among readmitted patients was 4.8 times higher in ICU1 and 10.3 times higher in ICU2 than the hospital mortality rates among those without ICU readmission. Previous studies have reported a 4- to 11-fold increase in mortality in readmitted patients (17-20) compared to non-readmitted patients.(3,10,21,22) The high ICU1 mortality rate during the first hospitalization is partly explained by the severity of the patients' conditions, who were often already under mechanical ventilatory support in the hospital emergency room, awaiting intensive care beds. Brazil has a limited number of ICU beds to provide care meeting all patients' demand. Thus, the available beds must be occupied by patients with certain indications and/or high probability of recovery.
The SWIFT scale was better at recommending discharge from ICU1, the clinical-surgical ICU, than from ICU2. In comparisons between groups and SWIFT variables, readmitted patients who died following ICU discharge showed a greater decrease in the level of (sensory) consciousness than non-readmitted patients in both ICUs, according to the GCS, on the day of ICU discharge. Nevertheless, SWIFT was unable to predict ICU2 readmissions, showing that respiratory variables are less sensitive when used for predicting the neurological patients' discharge because the GCS was different between groups, unlike the other variables.
The SWIFT index showed better results in a study conducted in a North American medical ICU than that conducted in a European medical-surgical ICU. SWIFT predicted unplanned ICU readmission with acceptable validation in both cohort derivations; however, the model fit was poor in the European medical-surgical ICU. The observed readmission rate remained high (>5%) in both patient cohorts. The results observed for readmitted patients was worse than that predicted using APACHE III in that study.(11)
Thus, the application of a scale such as SWIFT to calculate the best time of discharge for intensive care patients, given the current status of Brazilian ICUs, is quite complex in the context of high occupancy/load and reduced number of intensive care unit beds in the public health system. The intensive care team often agrees to vacate beds, given the high demand, even before adequate clinical stabilization, resulting in readmissions and deaths due to discontinuation of necessary care in common hospital beds.
Our study has some limitations. We analyzed ICU-hospitalized patient data from electronic and paper medical records because not all required information was recorded in the electronic system. However, paper medical records have several limitations and are inefficient in storing and organizing a large volume of data, with several disadvantages in relation to electronic medical records, including the facts that information from medical records on paper is only available to one professional at a time, has low mobility, may be illegible and ambiguous, is frequently lost, requires multiple folders, complicates collective research, lacks standardization, complicates access, is destructible (paper), and requires large spaces in archive services for safekeeping.
CONCLUSION
The mortality associated with ICU readmission found in our study was higher than that in other studies inside and outside Brazil. The SWIFT scale showed greater effectiveness in identifying the patients most prone to readmission and death following discharge from a medical-surgical ICU than from a trauma and neurosurgery ICU. The importance of the present study lies in the identification and characterization of the population readmitted to ICUs. The present study can serve as an epidemiological reference to review the discharge criteria used and the quality of care offered, representing a basis for future evaluations of the impact of those policies on the care of critically ill patients.
Footnotes
Conflicts of interest: None.
Study conducted at Grupo Hospitalar Conceição -Porto Alegre (RS), Brazil.
REFERENCES
- 1.Rosenberg AL, Watts C. Patients readmitted to ICUs: a systematic review of risk factors and outcomes. Chest. 2000;118(2):492–502. doi: 10.1378/chest.118.2.492. [DOI] [PubMed] [Google Scholar]
- 2.Durbin CG Jr, Kopel R. A case-control study of patients readmitted to the intensive care unit. Crit Care Med. 1993;21(10):1547–1553. doi: 10.1097/00003246-199310000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Franklin C, Jackson D. Discharge decision-making in a medical ICU: characteristics of unexpected readmissions . Crit Care Med. 1983;11(2):61–66. doi: 10.1097/00003246-198302000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg AL, Hofer TP, Hayward RA, Strachan C, Watts CM. Who bounces back? Physiologic and other predictors of intensive care unit readmission. Crit Care Med. 2001;29(3):511–518. doi: 10.1097/00003246-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Kaben A, Corrêa F, Reinhart K, Settmacher U, Gummert J, Kalff R, et al. Readmission to a surgical intensive care unit: incidence, outcome and risk factors. Crit Care. 2008;12(5):R123. doi: 10.1186/cc7023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishi GK, Suh RH, Wilson MT, Cunneen SA, Margulies DR, Shabot MM. Analysis of causes and prevention of early readmission to surgical intensive care. Am Surg. 2003;69(10):913–917. [PubMed] [Google Scholar]
- 7.Levy MF, Greene L, Ramsay MA, Jennings LW, Ramsay KJ, Meng J, et al. Readmission to the intensive care unit after liver transplantation. Crit Care Med. 2001;29(1):18–24. doi: 10.1097/00003246-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Elliott M. Readmission to intensive care: a review of the literature. Aust Crit Care. 2006;19(3):96-8, 100-4. doi: 10.1016/s1036-7314(06)80004-4. [DOI] [PubMed] [Google Scholar]
- 9.Rubins HB, Moskowitz MA. Discharge decision-making in a medical intensive care unit. Identifying patients at high risk of unexpected death or unit readmission. Am J Med. 1988;84(5):863–869. doi: 10.1016/0002-9343(88)90064-2. [DOI] [PubMed] [Google Scholar]
- 10.Snow N, Bergin KT, Horrigan TP. Readmission of patients to the surgical intensive care unit: patient profiles and possibilities for prevention. Crit Care Med. 1985;13(11):961–964. doi: 10.1097/00003246-198511000-00037. [DOI] [PubMed] [Google Scholar]
- 11.Gajic O, Malinchoc M, Comfere TB, Harris MR, Achouiti A, Yilmaz M, et al. The Stability and Workload Index for Transfer score predicts unplanned intensive care unit patient readmission: initial development and validation. Crit Care Med. 2008;36(3):676–682. doi: 10.1097/CCM.0B013E318164E3B0. [DOI] [PubMed] [Google Scholar]
- 12.Chung DA, Sharples LD, Nashef SA. A case-control analysis of readmissions to the cardiac surgical intensive care unit. Eur J Cardiothorac Surg. 2002;22(2):282–286. doi: 10.1016/s1010-7940(02)00303-2. [DOI] [PubMed] [Google Scholar]
- 13.Kogan A, Cohen J, Raanani E, Sahar G, Orlov B, Singer P, et al. Readmission to the intensive care unit after "fast-track" cardiac surgery: risk factors and outcomes. Ann Thorac Surg. 2003;76(2):503–507. doi: 10.1016/s0003-4975(03)00510-1. [DOI] [PubMed] [Google Scholar]
- 14.Metnitz PG, Fieux F, Jordan B, Lang T, Moreno R, Le Gall JR. Critically ill patients readmitted to intensive care units--lessons to learn? Intensive Care Med. 2003;29(2):241–248. doi: 10.1007/s00134-002-1584-z. [DOI] [PubMed] [Google Scholar]
- 15.Moreno R, Morais P. Outcome prediction in intensive care: results of a prospective, multicentre, Portuguese study. Intensive Care Med. 1997;23(2):177–186. doi: 10.1007/s001340050313. [DOI] [PubMed] [Google Scholar]
- 16.Campbell AJ, Cook JA, Adey G, Cuthbertson BH. Predicting death and readmission after intensive care discharge. Br J Anaesth. 2008;100(5):656–662. doi: 10.1093/bja/aen069. [DOI] [PubMed] [Google Scholar]
- 17.Cooper GS, Sirio CA, Rotondi AJ, Shepardson LB, Rosenthal GE. Are readmissions to the intensive care unit a useful measure of hospital performance? Med Care. 1999;37(4):399–408. doi: 10.1097/00005650-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Cohn WE, Sellke FW, Sirois C, Lisbon A, Johnson RG. Surgical ICU recidivism after cardiac operations. Chest. 1999;116(3):688–692. doi: 10.1378/chest.116.3.688. [DOI] [PubMed] [Google Scholar]
- 19.Russell S. Reducing readmissions to the intensive care unit. Heart Lung. 1999;28(5):365–372. doi: 10.1053/hl.1999.v28.a101055. [DOI] [PubMed] [Google Scholar]
- 20.Chen LM, Martin CM, Keenan SP, Sibbald WJ. Patients readmitted to the intensive care unit during the same hospitalization: clinical features and outcomes. Crit Care Med. 1998;26(11):1834–1841. doi: 10.1097/00003246-199811000-00025. [DOI] [PubMed] [Google Scholar]
- 21.Baigelman W, Katz R, Geary G. Patient readmission to critical care units during the same hospitalization at a community teaching hospital. Intensive Care Med. 1983;9(5):253–256. doi: 10.1007/BF01691250. [DOI] [PubMed] [Google Scholar]
- 22.Kirby EG, Durbin CG. Establishment of a respiratory assessment team is associated with decreased mortality in patients re-admitted to the ICU. Respir Care. 1996;41:903–907. [Google Scholar]