Abstract
Objective
To analyze the outcomes of increased or decreased intracranial pressure and/or the decrease in cerebral perfusion pressure resulting from respiratory physiotherapy on critically ill patients admitted to the intensive care unit.
Methods
Through a systematic review of the literature, clinical trials published between 2002 and 2012 were selected. The search involved the LILACS, SciELO, MedLine and PEDro databases using the keywords "physical therapy", "physiotherapy", "respiratory therapy" and "randomized controlled trials" combined with the keyword "intracranial pressure".
Results
In total, five studies, including a total of 164 patients between 25 and 65 years of age, reporting that respiratory physiotherapy maneuvers significantly increased intracranial pressure without changing the cerebral perfusion pressure were included. The articles addressed several techniques including vibration, vibrocompression, tapping, postural drainage, and the endotracheal aspiration maneuver. All patients required invasive mechanical ventilation.
Conclusion
Respiratory physiotherapy leads to increased intracranial pressure. Studies suggest that there are no short-term hemodynamic or respiratory repercussions or changes in the cerebral perfusion pressure. However, none of the studies evaluated the clinical outcomes or ensured the safety of the maneuvers.
Keywords: Physical therapy modalities, Intracranial pressure, Critical care, Respiratory physiotherapy
Abstract
Objetivo
Analisar os desfechos aumento/diminuição da pressão intracraniana e/ou queda da pressão de perfusão cerebral, proporcionados pela fisioterapia respiratória em pacientes graves assistidos em unidade de terapia intensiva.
Métodos
Por meio de uma revisão sistemática da literatura, foram selecionados ensaios clínicos publicados entre 2002 e 2012. A busca envolveu as bases de dados LILACS, SciELO, MedLine e PEDro, usando os descritores "physical therapy", "physiotherapy", "respiratory therapy" e "randomized controlled trials" em cruzamento com o descritor "intracranial pressure".
Resultados
Foram incluídos 5 estudos, que somaram 164 pacientes, com média de idade entre 25 e 65 anos, e que indicaram que as manobras de fisioterapia respiratória aumentaram significativamente a pressão intracraniana, sem alterar a pressão de perfusão cerebral. Os artigos abordaram as técnicas de vibração, vibrocompressão, tapotagem, drenagem postural, além da manobra de aspiração intratraqueal. Todos os pacientes estavam sob ventilação mecânica invasiva.
Conclusão
A fisioterapia respiratória promove aumento da pressão intracraniana. Os estudos sugerem que não há repercussões hemodinâmicas e respiratórias a curto prazo ou alteração da pressão de perfusão cerebral. Entretanto, não há estudos que avaliem desfechos clínicos e que assegurem a segurança das manobras.
INTRODUCTION
Patients with neurological pathologies, whether traumatic or not, with a Glasgow coma scale ≤8 usually undergo intracranial pressure (ICP), mean arterial pressure (MAP) and cerebral perfusion pressure (CPP) monitoring and are treated with a strict patient-care protocol, including sedation, head-of-bed elevation, invasive mechanical ventilation (IMV) and motor and respiratory physiotherapy.(1,2)
In the intensive care unit (ICU), the main objective of critical patient care is to prevent secondary injury by maintaining hemodynamic, metabolic and respiratory stability.(3,4) One way to assess brain injury severity is ICP monitoring. This variable reflects the relationship between the cranial contents and the cranial volume, and a change in this parameter may cause intracranial hypertension (ICH).(5,6) In addition, ICP elevations can lead to a decrease in the CPP and result in circulatory impairment with cerebral hypoxia and increased cerebral edema, which may then evolve to brain death in severe cases.(7,8)
In critical cases, respiratory physiotherapy (RP) plays an important role in maintaining the airway and preventing complications through maneuvers and specific positions, which are based on the patient's clinical condition.(9-11) However, the techniques applied by physiotherapists lead to transient hemodynamic changes, which may cause changes in parameters including the ICP.
Previous studies have shown that RP maneuvers can lead to momentary increases in the intrathoracic pressure (ITP), decreasing the cerebral venous return and possibly elevating the ICP.(12,13) However, there are still disagreements in the scientific literature regarding the effects of RP maneuvers on ICP in critical ICU patients, as some authors have reported elevations in the ICP during and/or after the RP techniques and others have reported no significant changes at any of the time points evaluated.
In the technical literature, there are currently no meta-analyses or systematic reviews addressing the effects of RP on ICP in critical patients. Thus, the present study aimed to conduct a systematic review of the literature to clarify the outcomes of an increase/decrease in ICP and/or a decrease in CPP, resulting from RP on critically ill adult patients admitted to the ICU.
METHODS
This review was conducted according to the PRISMA guidelines for conducting systematic reviews.(14)
Identification and selection criteria
The search for articles involving the desired clinical outcome was performed with the following databases: Latin American and Caribbean Health Sciences Literature (Literatura Latino-Americana e do Caribe em Ciências da Saúde - LILACS), Scientific Electronic Library Online (SciELO), Medical Literature Analysis and Retrieval System Online (MedLine/PubMed) and Physiotherapy Evidence Database (PEDro). Articles were obtained by combining the keyword "intracranial pressure" with the keywords "physical therapy" OR "physiotherapy" OR "respiratory therapy" OR "randomized controlled trials" using the Boolean operator "and".
The reference search was limited to articles published between 2002 and 2012 that were written in Portuguese, English or Spanish.
Based on the desired outcomes, RP interventions were analyzed just prior to, during or after the maneuvers. RP interventions were defined as airway clearance procedures, such as vibration, vibrocompression, tapping, postural drainage, increased expiratory flow rate (IEF) and endotracheal aspiration (ETA) techniques.
The articles included in this study were classified according to their levels of evidence and their degrees of recommendation, as classified by the Oxford Centre for Evidence-Based Medicine.(15)
Inclusion and exclusion criteria
At the end of the analysis, only clinical trials that addressed performing RP on critically ill adult patients with continuous ICP monitoring were included. Letters, abstracts, dissertations, theses, literature reviews and case reports were excluded, as were studies that used children and/or animal models.
Selection strategy
For the selection of articles, an evaluation of the titles related to the topic in question was initially performed. This selection was based on titles whose main subject was the application of RP maneuvers and the ETA technique in critically ill ICU patients under continuous monitoring and with elevated ICP levels. Titles that had the terms "physiotherapy" and "ICP" or information related to these terms were also included. At the end of the search, similar titles were excluded because the search was conducted in several databases. Detailed readings of the article abstracts were then performed to select those articles that exclusively addressed the application of RP on the ICP of critically ill patients. Abstracts that did not address the topic in question were excluded. The full text of the remaining articles was then evaluated, and those that met the inclusion criteria were included.
Assessment of the validity of the study
The titles and abstracts of the articles identified in the search strategy were independently and "blindly" reviewed by two researchers, and in case of disagreement, a third senior researcher decided to include or exclude the article. Studies that addressed the inclusion criteria were assessed using the PEDro scale.(16) This scale was developed by the Australian Physiotherapy Association and attempts to assess the quality of published randomized clinical trials to inform users about the meritorious aspects of each publication and facilitate the rapid identification of studies that contain sufficient information for professional practice.
The PEDro scale assesses the trials using 11 pre-established items. The first item is an additional criterion and represents the external validity (or "potential for generalization" or "applicability" of the trial), but it is not included in the total score. The remaining items assess two aspects of the article's quality: internal validity (items 2-9) and whether the article contains sufficient statistical information to allow the results to be interpreted (items 10 and 11). These items are designated as "applicable" or "not applicable", generating a total score ranging from 0 to 10 points.(17)
The selected articles were analyzed and classified as "high quality" if they received a score ≥4 points on the PEDro scale or as "low quality" if they received a score <4 on the same scale.(18) It should be noted that the PEDro scale score was not used as an inclusion or exclusion criterion for the articles, but it was used as an indicator of the study's scientific quality.
RESULTS
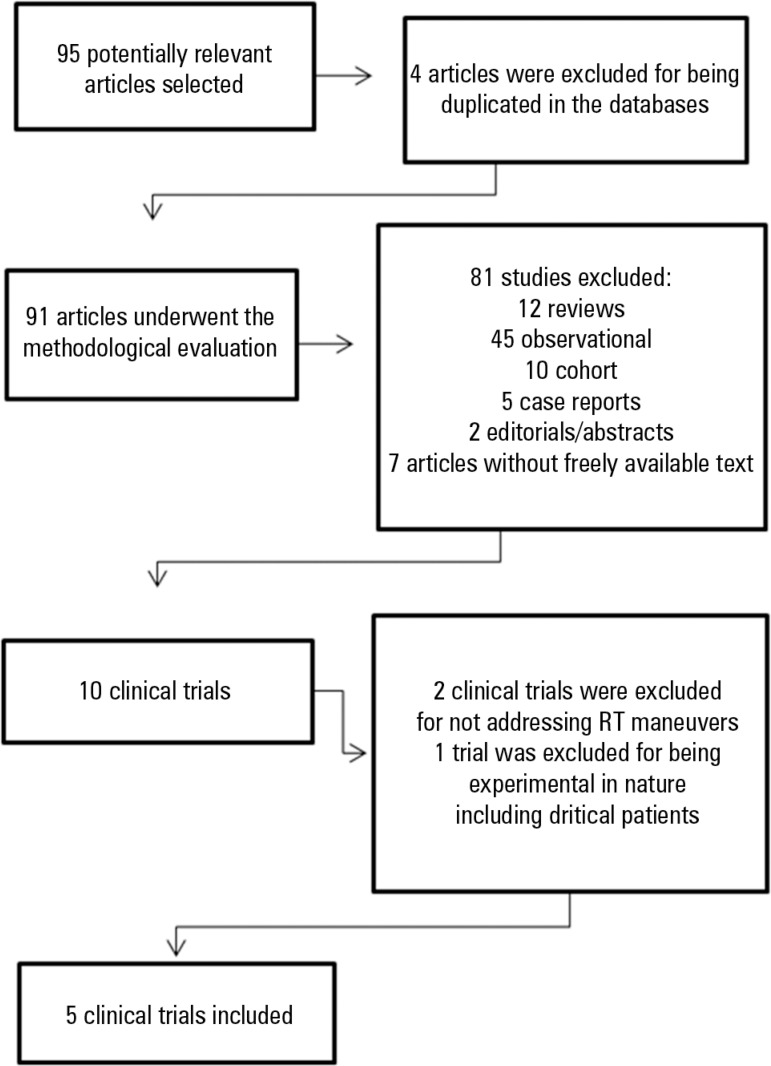
The database search resulted in 95 articles, 90 of which were excluded after the analysis conducted by the two researchers for being duplicates in databases or because they lacked the predefined methodological criteria for the desired outcome (Figure 1).
Figure 1.
Flowchart of the article search strategy. RP - respiratory physiotherapy
Table 1 contains the information on the PEDro scale scores for the randomized clinical trials. Four of the included studies met the eligibility criteria, as they performed intergroup comparisons. All studies had an initial similarity between groups, performed adequate follow-up, provided intention-to-treat analyses and used measures of accuracy and variability. However, due to the small patient sample sizes, there is a high risk of bias, so all the included studies received a score of 0 for this last item. None of the studies conducted "blinding" of the subjects, therapists or evaluators. Regarding the PEDro scale classification, 80% of the studies achieved a score ≥4 points and were classified as "high quality" according to the criteria proposed by Van Peppen et al.(18)
Table 1.
Classification of the randomized clinical trials according to the PEDro scale
| Studies | Thiesen et al.(19) | Nemer et al.(20) | Toledo et al.(21) | Olson et al.(22) | Cerqueira-Neto et al.(23) | |
| PEDro Scale | ||||||
| 1. Eligibility criteria | Yes | Yes | Yes | Yes | Yes | |
| 2. Randomization | 0 | 0 | 0 | 1 | 1 | |
| 3. Blind subject allocation | 0 | 0 | 0 | 0 | 0 | |
| 4. Initial similarity between groups | 1 | 1 | 1 | 1 | 1 | |
| 5. "Blinding" of subjects | 0 | 0 | 0 | 0 | 0 | |
| 6. "Blinding" of therapists | 0 | 0 | 0 | 0 | 0 | |
| 7. "Blinding" of evaluators | 0 | 0 | 0 | 0 | 0 | |
| 8. Adequate follow-up | 1 | 1 | 1 | 1 | 1 | |
| 9. Intention-to-treat analysis | 1 | 1 | 1 | 1 | 1 | |
| 10. Intergroup comparisons | 1 | 1 | 0 | 1 | 1 | |
| 11. Measures of accuracy and variability | 0 | 0 | 0 | 0 | 0 | |
| Total score | 4/10 | 4/10 | 3/10 | 5/10 | 5/10 | |
1 for applicable items and 0 for non-applicable items. Data source: http://www.pedro.org.au.
The studies analyzed in this systematic review were also classified based on their level of evidence according to the Oxford Centre for Evidence-Based Medicine classification.(15) All studies received a recommendation grade of C, and most had a 2B level of evidence (Table 2).
Table 2.
Classification of the level of evidence of the clinical trials according to the Oxford Centre for Evidence-Based Medicine classification(15)
All the included studies involved patients with neurological or neurosurgical diagnoses, and traumatic brain injury (TBI) was the most prevalent injury (80%). All the included studies(19-23) also involved the use of conventional RP maneuvers, such as vibration, vibrocompression, tapping, postural drainage and ETA maneuvers to remove secretions (Table 3).
Table 3.
Characteristics of selected clinical trials published between 2002 and 2012 analyzing the effects of respiratory physiotherapy on the intracranial pressure of critically ill patients
| Author | Sample (N) | Sample characteristics | Intervention | Intervention time | Key variables | Significant outcomes |
| Thiesen et al.(19) | 35 | Severe TBI, undergoing IMV, GCS ≤8, mean age of 24.9 years | Manual expiratory pressure with manual rib vibration; manual expiratory pressure with manual diaphragmatic vibration, postural drainage + tapping; expiratory manual pressure with rib decompression, manual expiratory pressure with diaphragmatic decompression, ETA (30 minutes) | 1 single session | ICP, MAP, CPP | Increase in ICP during manual epressure maneuvers with manual dvibration, postural drainage with tapETA |
| Nemer et al.(20) | 70 | 53 severe TBI and 17 strokes undergoing IMV; GCS ≤8, mean age 45.9±20.2 years | Chest compression, vibration in combination with chest compression; unilateral continuous chest compression; open circuit and closed circuit ETA (16 minutes) | 1 single session | ICP | Three procedures significantly chanICP: unilateral continuous chest comopen circuit and closed circuit ETA |
| Toledo et al.(21) | 11 | Severe TBI, undergoing IMV, age ≥18 years, less than 24 hours in the ICU | Bilateral manual vibrocompression maneuvers; ETA (20 minutes) | 2 times a day for 3 days | ICP, MAP, CPP | Increase in ICP after the ETA maneuve |
| Olson et al.(22) | 28 | Neurological or neurosurgical diagnosis, age ≥18 years | 1 single session | ICP, BP, HR, RR, SpO2 | There were no statistically sdifferences between the ICP of compared to the CG | |
| CG (n = 15) - no intervention | ||||||
| Cerqueira-Neto et al.(23) | 20 | Severe TBI, undergoing IMV, GCS ≤8, mean age 33.5±11.94 years | Unilateral manual vibrocompression maneuvers and increased expiratory flow (5 minutes) in each hemithorax; ETA (10-15 seconds) | 1 single session | ICP, MAP, CPP | Increased ICP and MAP, with consduring the ETA maneuvers |
TBI - traumatic brain injury; IMV - invasive mechanical ventilation, GCS - Glasgow coma scale; ETA - endotracheal aspiration; ICP - intracranial pressure, MAP - mean arterial pressure; CPP - cerebral perfusion pressure; ICU - intensive care unit, IG - intervention group, CG - control group, BP - blood pressure, HR - heart rate, RR - respiratory rate, SpO2 - oxygen saturation.
The patient sample size ranged from 11 to 70 individuals undergoing IMV and included people of both genders between the ages of 25 and 65 years. Only one study(22) had a control group without intervention for comparison of the results; the remaining studies provided comparisons between periods (prior to, during and after the intervention). Four of the included studies only used a single intervention session.(19,20,22,23)
In addition to ICP and CPP, hemodynamic variables, blood pressure (BP), MAP, heart rate (HR), respiratory rate (RR) and oxygen saturation (SpO2) were also considered as outcomes in the studies analyzed.
Two of the five studies showed significant increases in ICP in critically ill patients after RP maneuvers.(19,20) Four studies showed significant increases in this pressure during or after the ETA maneuvers.(19,20,21,23) In addition, another included study did not report any significant differences after comparing the group of patients receiving the RP maneuvers with the control group without intervention.(22) None of the studies analyzed reported significant changes in CPP before, during and/or after the RP interventions.
DISCUSSION
Most studies analyzed in the present study showed that the RP procedures and ETA maneuvers significantly changed the ICP without significantly changing the CPP of ICU patients, as evidenced by methodological and statistical data from the published clinical trials.(16) RP procedures that resulted in this change included manual expiratory pressure combined with manual diaphragmatic vibration, postural drainage with tapping and unilateral continuous chest compression.
The studies included in this review indicated that performing RP and ETA maneuvers on critically ill patients significantly increased the ICP.(19,20,21,23) Theoretically, the RP maneuvers applied to the chest would increase the ITP, which is directly related to the alveolar pressure;(19) decrease the rate of venous return to the heart; and decrease cardiac output (CO) and MAP, which could also compromise the cerebral venous return, thus leading to increased ICP.(12,19) It has been reported that the usual RP interventions in critically ill patients may influence cerebral oxygen transport via adverse effects on CO.(21,24,25) However, several studies have shown that the increase in ICP caused by increases in ITP does not significantly compromise CPP.(11,12,19,21,26)
This review verified the lack of studies in the literature evaluating the effects of RP maneuvers on the ICP of critically ill patients. The few studies included here show that RP led to small and transient increases in ICP without significantly altering the CPP before, during or after the analyzed maneuvers.
Almost all the studies showed that ICP transiently increased during the ETA maneuvers.(19,20,21,23) This increase may be caused by two main factors: tracheal stimulation and an increase in the arterial carbon dioxide partial pressure (PaCO2).(27) Such an increase is offset by a protective response characterized by increases in MAP, jugular venous oxygen tension and middle cerebral artery blood flow velocity, which together maintain the brain oxygen supply during and after ETA.(21,25) Other authors have suggested that ETA can generate increases in ICP in response to the cough reflex, hypercapnia and the Valsalva maneuver, with consequent cerebral vasodilation.(20,26)
The ETA maneuver should be performed with extreme caution over a short period of time, only when absolutely necessary and by professionals who have an understanding of continuous ICP monitoring and its effects on the human body.
The patients included in the analyzed studies had some type of brain injury and required IMV; this procedure predisposed them to pulmonary involvement, which might also have led to reduced arterial oxygen pressure (PaO2) and PaCO2 retention. Therefore, IMV can have hemodynamic repercussions, leading to increases in ICP and reductions in CPP because compression of the alveolar capillaries, which is caused by distention of the alveoli, can lead to increased right ventricle afterload, thus reducing venous return.(28)
The present study has some important limitations in regards to the inadequate identification of the impact of RP maneuvers on important clinical outcomes such as MV time, duration of ICU stay, modified Glasgow score at discharge, mortality and levels of neurological sequelae. These studies only assessed short-term changes in basic ventilation and hemodynamic parameters. In other words, it was not possible to determine whether the application of RP maneuvers neurologically compromised the patients. There are no adequate randomized studies comparing patients with and without RP. Thus, it is evident that the data in the current literature do not allow an assessment of the safety of RP in critically ill patients requiring continuous ICP monitoring. Moreover, the use of the PEDro classification may overestimate the quality of studies because a score of 4 is used as the quality cut-off point. Another limitation is that seven studies were excluded due to difficulties in obtaining them.
CONCLUSION
In conclusion, the methodological analysis performed in this study confirmed the lack of studies that address the effects of respiratory physiotherapy on intracranial pressure and cerebral perfusion pressure in critically ill patients. The currently available evidence indicates that the maneuvers involving airway clearance and endotracheal aspiration techniques lead to increases in intracranial pressure with no clinical repercussions and without changing the cerebral perfusion pressure (level of evidence 2B). However, none of the studies assessed clinical outcomes, so it is not possible to analyze the safety of such maneuvers. Further studies using specific methodological designs are therefore needed.
Footnotes
Conflicts of Interest: None.
REFERENCES
- 1.Schimpf MM. Diagnosing increased intracranial pressure. J Trauma Nurs. 2012;19(3):160–167. doi: 10.1097/JTN.0b013e318261cfb4. [DOI] [PubMed] [Google Scholar]
- 2.Zanier ER, Ortolano F, Ghisoni L, Colombo A, Losappio S, Stocchetti N. Intracranial pressure monitoring in intensive care: clinical advantages of a computerized system over manual recording. Crit Care. 2007;11(1):R7. doi: 10.1186/cc5155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferreira LL, Marino LH, Cavenaghi S. Atuação fisioterapêutica na lesão medular em unidade de terapia intensiva: atualização de literatura. Rev Neurocienc. 2012;20(4):612–617. [Google Scholar]
- 4.Helmy A, Vizcaychipi M, Gupta AK. Traumatic brain injury: intensive care management. Review. Br J Anaesth. 2007;99(1):32–42. doi: 10.1093/bja/aem139. [DOI] [PubMed] [Google Scholar]
- 5.Jantzen JP. Prevention and treatment of intracranial hypertension. Best Pract Res Clin Anaesthesiol. 2007;21(4):517–538. doi: 10.1016/j.bpa.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Pillai S, Praharaj SS, Rao GS, Kolluri VR. Cerebral perfusion pressure management of severe diffuse head injury: effect on brain compliance and intracranial pressure. Neurol India. 2004;52(1):67–71. [PubMed] [Google Scholar]
- 7.Perel P, Edwards P, Wentz R, Roberts I. Systematic review of prognostic models in traumatic brain injury. BMC Med Inform Decis Mak. 2006;6:38. doi: 10.1186/1472-6947-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enrione MA. Current concepts in the acute management of severe pediatric head trauma. Clin Pediatr Emerg Med. 2001;2(1):28–40. [Google Scholar]
- 9.França EE, Ferrari F, Fernandes P, Cavalcanti R, Duarte A, Martinez BP, et al. Fisioterapia em pacientes críticos adultos: recomendações do Departamento de Fisioterapia da Associação de Medicina Intensiva Brasileira. Rev Bras Ter Intensiva. 2012;24(1):6–22. [PubMed] [Google Scholar]
- 10.Jerre G, Silva TJ, Beraldo MA, Gastaldi A, Kondo C, Leme F, et al. Fisioterapia no paciente sob ventilação mecânica. J Bras Pneumol. 2007;33(Supl 2):S142–S150. doi: 10.1590/s1806-37132007000800010. [DOI] [PubMed] [Google Scholar]
- 11.Stiller K. Physiotherapy in intensive care: towards an evidence-based practice. Chest. 2000;118(6):1801–1813. doi: 10.1378/chest.118.6.1801. [DOI] [PubMed] [Google Scholar]
- 12.Georgiadis D, Schwart S, Baumgartner RW, Veltkamp R, Schwab S. Influence of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure in patients with acute stroke. Stroke. 2001;32(9):2088–2092. doi: 10.1161/hs0901.095406. [DOI] [PubMed] [Google Scholar]
- 13.Imle PC, Mars MP, Ciesla ND, Anderson PA, Delaney PA. The effect of chest physical therapy on intracranial pressure and cerebral perfusion pressure. Physiotherapy. 1997;49(1):48–55. [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Reprint--preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89(9):873–880. [PubMed] [Google Scholar]
- 15.Centre for Evidence-based Medicine - Levels of evidence (March 2009). Produced by Bob Phillips, Chris Ball, Dave Sackett, Doug Badenoch, Sharon Straus, Brian Haynes, Martin Dawes since November 1998. [Updated by Jeremy Howick March 2009]. [cited 2013 Nov 22]. Available from: http://www.cebm.net/?O=1025.
- 16.Physiotherapy Evidence Database (PEDro) [Internet] [cited 2011 Sept 7]. Available from: http://www.pedro.org.au.
- 17.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 18.Van Peppen RP, Kwakkel G, Wood-Dauphinee S, Hendriks HJ, Van der Wees PJ, Dekker J. The impact of physical therapy on functional outcomes after stroke: what's the evidence? Clin Rehabil. 2004;18(8):833–862. doi: 10.1191/0269215504cr843oa. [DOI] [PubMed] [Google Scholar]
- 19.Thiesen RA, Dragosavac D, Roquejani AC, Falcão AL, Araújo S, Dantas VP, Filho, et al. Influência da fisioterapia respiratória na pressão intracraniana em pacientes com traumatismo cranioencefálico grave. Arq Neuropsiquiatr. 2005;63(1):110–113. doi: 10.1590/s0004-282x2005000100020. [DOI] [PubMed] [Google Scholar]
- 20.Nemer SN, Machado ST, Caldeira JB, Azeredo LM, Clipes T, Gago R, et al. Efeitos da fisioterapia respiratória e da mobilização passiva sobre a pressão intracraniana. Fisioter Bras. 2005;6(6):437–443. [Google Scholar]
- 21.Toledo C, Garrido C, Troncoso E, Lobo SM. Effects of respiratory physiotherapy on intracranial pressure and cerebral perfusion pressure in severe traumatic brain injury patients. Rev Bras Ter Intensiva. 2008;20(4):339–343. [PubMed] [Google Scholar]
- 22.Olson DM, Thoyre SM, Bennett SN, Stoner JB, Graffagnino C. Effect of mechanical chest percussion on intracranial pressure: a pilot study. Am J Crit Care. 2009;18(4):330–335. doi: 10.4037/ajcc2009523. [DOI] [PubMed] [Google Scholar]
- 23.Cerqueira-Neto ML, Moura AV, Scola RH, Aquim EE, Rea-Neto A, Oliveira MC, et al. The effect of breath physiotherapeutic maneuvers on cerebral hemodynamics: a clinical trial. Arq Neuropsiquiatr. 2010;68(4):567–572. doi: 10.1590/s0004-282x2010000400017. [DOI] [PubMed] [Google Scholar]
- 24.Pinheiro AR, Christofoletti G. Fisioterapia motora em pacientes internados na unidade de terapia intensiva: uma revisão sistemática. Rev Bras Ter Intensiva. 2012;24(2):188–196. [PubMed] [Google Scholar]
- 25.Gemma M, Tommasino C, Cerri M, Giannotti A, Piazzi B, Borghi T. Intracranial effects of endotracheal suctioning in the acute phase of head injury. J Neurosurg Anesthesiol. 2002;14(1):50–54. doi: 10.1097/00008506-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Celik SA, Kanan N. A current conflict: use of isotonic sodium chloride solution on endotracheal suctioning in critically ill patients. Dimens Crit Care Nurs. 2006;25(1):11–14. doi: 10.1097/00003465-200601000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Fisher DM, Frewen T, Swedlow DB. Increase in intracranial pressure during suctioning--stimulation vs. rise in PaCO2 . Anesthesiology. 1982;57(5):416–417. doi: 10.1097/00000542-198211000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Lima WA, Campelo AR, Gomes RL, Brandão DC. Repercussão da pressão positiva expiratória final na pressão de perfusão cerebral em pacientes adultos com acidente vascular hemorrágico. Rev Bras Ter Intensiva. 2011;23(3):291–296. [PubMed] [Google Scholar]