Abstract
Objective
Acute kidney injury is a common complication in critically ill patients, and the RIFLE, AKIN and KDIGO criteria are used to classify these patients. The present study's aim was to compare these criteria as predictors of mortality in critically ill patients.
Methods
Prospective cohort study using medical records as the source of data. All patients admitted to the intensive care unit were included. The exclusion criteria were hospitalization for less than 24 hours and death. Patients were followed until discharge or death. Student's t test, chi-squared analysis, a multivariate logistic regression and ROC curves were used for the data analysis.
Results
The mean patient age was 64 years old, and the majority of patients were women of African descent. According to RIFLE, the mortality rates were 17.74%, 22.58%, 24.19% and 35.48% for patients without acute kidney injury (AKI) in stages of Risk, Injury and Failure, respectively. For AKIN, the mortality rates were 17.74%, 29.03%, 12.90% and 40.32% for patients without AKI and at stage I, stage II and stage III, respectively. For KDIGO 2012, the mortality rates were 17.74%, 29.03%, 11.29% and 41.94% for patients without AKI and at stage I, stage II and stage III, respectively. All three classification systems showed similar ROC curves for mortality.
Conclusion
The RIFLE, AKIN and KDIGO criteria were good tools for predicting mortality in critically ill patients with no significant difference between them.
Keywords: Acute kidney injury, Incidence, Mortality, Prognosis, Intensive care units
Abstract
Objetivo
A lesão renal aguda é uma complicação comum em pacientes gravemente enfermos, sendo os critérios RIFLE, AKIN e KDIGO utilizados para sua classificação. Esse trabalho teve como objetivo a comparação dos critérios citados quanto à capacidade de predição de mortalidade em pacientes gravemente enfermos.
Métodos
Estudo de coorte prospectiva, utilizando como fonte de dados prontuários médicos. Foram incluídos todos os pacientes admitidos na unidade de terapia intensiva. Os critérios de exclusão foram tempo de internamento menor que 24 horas e doença renal crônica dialítica. Os pacientes foram acompanhados até a alta ou óbito Para análise dos dados, foram utilizados os testes t de Student, qui-quadrado, regressão logística multivariada e curva ROC.
Resultados
A média de idade foi de 64 anos, com mulheres e afrodescendentes representando maioria. Segundo o RIFLE, a taxa de mortalidade foi de 17,74%, 22,58%, 24,19% e 35,48% para pacientes sem lesão renal aguda e em estágios Risk, Injury e Failure, respectivamente. Quanto ao AKIN, a taxa de mortalidade foi de 17,74%, 29,03%, 12,90% e 40,32% para pacientes sem lesão renal aguda, estágio I, estágio II e estágio III, respectivamente. Considerando o KDIGO 2012, a taxa de mortalidade foi de 17,74%, 29,03%, 11,29% e 41,94% para pacientes sem lesão renal aguda, estágio I, estágio II e estágio III, respectivamente. As três classificações apresentaram resultados de curvas ROC para mortalidade semelhantes.
Conclusão
Os critérios RIFLE, AKIN e KDIGO apresentaram-se como boas ferramentas para predição de mortalidade em pacientes graves, não havendo diferença relevante entre os mesmos.
INTRODUCTION
Advances in healthcare technologies and greater life expectancy have resulted in more patients with multiple and complex conditions requiring treatment in an intensive care setting. The occurrence of acute kidney injury (AKI) is common in such patients. AKI is a serious complication in the context of severe disease, especially when associated with sepsis and multiple organ dysfunction syndrome. In the literature, AKI is responsible for significant morbidity and mortality, ranging from 20 to 80%.(1-6)
In an attempt to standardize the definition and classification of AKI, the Risk, Injury, Failure, Loss, End-Stage (RIFLE) and Acute Kidney Injury Network (AKIN) criteria were created. Currently, these are the criteria used for classifying AKI based on serum creatinine and urine output.
The RIFLE criteria are based on the definition of three stages of AKI (Risk, Injury and Failure), which are based on changes in serum creatinine values along with urinary output to determine the stage of renal dysfunction. These criteria are also based on two other stages, defined as clinical outcomes, that correspond to more severe disease and a worse prognosis (Loss and End-Stage). The RIFLE criteria have been extensively evaluated for application in the monitoring of critically ill patients. As a result, some studies have shown that these criteria have great relevance for diagnosing, classifying and evaluating the progression of renal disease and for predicting death in this group of patients.(3,7,8)
The AKIN criteria emerged from the joint work of nephrologists and intensivists to make the RIFLE criteria more sensitive and reliable.(7) Several pieces of evidence suggested that even small changes in serum creatinine may be associated with increased mortality.(6) The AKIN criteria proposed a new definition by taking into account these minor changes in serum creatinine values and establishing a period of 48 hours to determine the change in creatinine with no need to first correlate with a baseline value. Additionally, the need for renal replacement therapy (RRT) was taken into account. A major advantage of the AKIN criteria is not using the individual's baseline creatinine. To compare the values of this biomarker according to AKIN, two measurements are needed: an initial (which corresponds to the baseline used by RIFLE) and another obtained after 48 hours. Patients with a primary alteration in serum creatinine >0.3mg/dL or an increase ≥150-199% over the first measurement are classified as having stage 1 injury (which corresponds to the Risk stage of RIFLE). When the increase in serum creatinine is 200-299% compared with the first measurement, the patient is classified as stage 2 (corresponding to the Injury stage of RIFLE). Finally, patients with ≥300% increase over the initial creatinine or a serum creatinine ≥4.0mg/dL with an abrupt rise of at least 0.5mg/dL or the onset of TSR are grouped together (which corresponds to the Failure stage of RIFLE).(7,9) The classification proposed by RIFLE had two major shortcomings. The first was that it depended directly on obtaining the baseline creatinine for each patient, which did not necessarily reflect the state of renal involvement. Secondly, there was no definition of which specific stage indicated patients who required RRT.(10) In this sense, the modifications adopted to generate AKIN were relevant.
Due to the high incidence of AKI in large intensive care units (ICUs) and its significant contribution to high mortality rates in such centers,(4) a comparative study of the RIFLE and AKIN criteria as predictors of mortality in critically ill patients is of great importance. It should be noted that similar studies have been conducted in some regions such as Europe, North America and Australia where the populations analyzed were predominantly Caucasian.(3,4,8) However, those studies were retrospective in design, while the present study had a prospective design and thus higher quality data.
More recently, the Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group(11) proposed changes to the staging for AKI. This new classification was important and novel for medical practice, especially with regard to the criterion of time. KDIGO covers both the AKIN and RIFLE criteria, taking into account changes in creatinine within 48 hours or a decline in the glomerular filtration rate (GFR) over 7 days. Moreover, patients under 18 with a GFR <35mL/min and patients with a serum creatinine >4.0mg/dL (absolute value) were added to AKIN stage 3. Our objective was to prospectively evaluate these three criteria for AKI classification as predictors of death.
METHODS
This was a prospective cohort study using a systematic sample that included cases consecutively admitted to the ICU between January 1 and December 31, 2011. The medical records of patients admitted to the ICU of a general hospital located in northeastern Brazil were used as the data source. This study was approved by the Research Ethics Committee of the Hospital Santo Antônio - Obras Sociais Irmã Dulce, under protocol number 49.342. An informed consent form was signed by all of the patients or their guardians. The study was conducted following the recommendations of Resolution 196/96 of the National Health Council.
All of the included patients were followed from ICU admission until discharge or death. Admitted patients hospitalized <24 hours and patients with dialysis-dependent chronic kidney disease were excluded.
The dependent variables were AKI and death from any cause. The following independent variables were analyzed: age; gender; ethnicity; origin; serum creatinine; serum potassium; need for elective surgery or emergency surgery; APACHE II score; volume of crystalloid administered within 24 hours; urine volume every 6 hours; use of vasoactive drugs; mean arterial pressure (MAP) measured by any method; need for dialysis; and the presence or absence of diabetes mellitus, hypertension, multiple trauma, heart failure/cardiogenic shock, infection and sepsis/septic shock.
The data were analyzed using the statistical program Statistical Package for Social Sciences (SPSS) version 14.0. Descriptive statistics were performed for frequency estimates, measures of central tendency and dispersion. Student's t-test was performed to compare means, and the chi-squared test was used to compare proportions. ROC (receiver operating characteristic) curves were used to evaluate the power of the AKIN, RIFLE and KDIGO criteria to predict death. Finally, a multivariate logistic regression was performed to determine the association between these criteria and mortality.
RESULTS
One hundred ninety patients were studied, and the mean age was 64.00±17.17. The predominant sex was female: 105 patients (55.30%) were women and 85 patients (44.70%) were men. In the present study, African descent was the most prevalent ethnic group, corresponding to 142 (74.70%) patients. Forty-eight patients (25.30%) were not of African descent. Fifty-five patients (28.95%) used vasoactive drugs. The median APACHE score was 15 (9.5). In terms of pathology, of the 190 patients analyzed, 125 patients (65.80%) were hypertensive, 89 patients (46.80%) had heart failure/cardiogenic shock, 79 patients (42.00%) had sepsis/septic shock, and 63 patients (33.2%) had diabetes mellitus. These and other data are displayed in table 1.
Table 1.
Demographic features and clinical-laboratory baselines for critically ill patients (N=190)
| Features | Result |
| Age (years) | 64.00±17.17 |
| Gender | |
| Female | 105 (55.30) |
| Male | 85 (44.70) |
| Ethnicity | |
| African descent | 142 (74.70) |
| Non-African descent | 48 (25.30) |
| Number using vasoactive drugs | 55 (28.95) |
| APACHE II score | 15 (5.5-24.5) |
| Referral | |
| Surgical center | 58 (30.53) |
| Infimary | 58 (30.53) |
| Urgent care | 43 (22.63) |
| Another hospital | 16 (8.42) |
| Hemodynamics | 14 (7.37) |
| Serum creatinine (mg/dL) | 1.22±0.71 |
| Serum K+ (mEq/L) | 4.02±1.35 |
| Volume administered (mL/24 hours) | 2.953.00 (1.018-4.888) |
| Urine output | 1.400.00 (210-2.590) |
| Heart failure/cardiogenic shock | 79 (42.00) |
| Sepsis/septic shock | 89 (46.80) |
| Diabetes mellitus | 63 (33.2) |
| Systemic hypertension | 125 (65.80) |
| Elective surgery | 51 (26.80) |
| Emergency surgery | 21 (11.10) |
| Temperature | 35.73±3.39 |
| MBP (mmHg) | 91.02±22.71 |
| HR | 89.20±23.46 |
| RR | 20.13±6.80 |
| PaO2/FiO2 | 298.03 (123.12-472.94) |
| pH | 7.39±0.09 |
| Serum Na+ (mEq/L) | 139.37±15.23 |
| Hematocrit (%) | 34.11±7.98 |
| White blood cells (/mm3) | 11.600.00 (3.600-19.600) |
| Glasgow | 11.75±3.17 |
Serum K+ - serum potassium; MBP - mean blood pressure; HR - heart rate; RR - respiratory rate; PaO2/FiO2 - arterial oxygen pressure/fraction of inspired oxygen; Serum Na+ - serum sodium. The results are expressed as number (%), mean±standard deviation or median (interquartile interval).
Table 2 shows a cross-tabulation of the agreement between the RIFLE and AKIN criteria at different stages: 34.74% for patients without AKI; 29.47% for AKIN stage I and RIFLE Risk classification; 6.31% for AKIN stage II and RIFLE Injury classification; and 14.21% for AKIN stage III and RIFLE Failure classification.
Table 2.
Cross-tabulation of patients classified by RIFLE versus AKIN criteria
| AKIN | RIFLE | ||||
| Without AKI | Risk | Injury | Failure | Total (AKIN) | |
| Without AKI | 66 (34.74) | 0 | 2 (1.05) | 2 (1.05) | 70(36.84) |
| Stage 1 | 4 (2.10) | 56 (29.47) | 10 (5.26) | 1 (0.53) | 71 (37.37) |
| Stage 2 | 0 | 0 | 12 (6.31) | 3 (1.58) | 15 (7.89) |
| Stage 3 | 1 (0.53) | 2 (1.05) | 4 (2.10) | 27 (14.21) | 34 (17.89) |
| Total (RIFLE) | 71 (37.37) | 58 (30.53) | 28 (17.74) | 33 (17.37) | 190 (100) |
AKI - acute kidney injury. Number of patients classified in the indicated AKI stages by the AKIN or RIFLE criteria are cross-tabulated. The results are expressed as numbers and percentages. Grey cells indicate patients that were assigned to the same AKI degree by both classification systems.
According to the RIFLE criteria, the mortality rates were 11 (17.74%), 14 (22.58%), 15 (24.19%) and 22 (35.48%) for patients without AKI and at the stages of Risk, Injury and Failure, respectively. For the AKIN criteria, the mortality rates were 11 (17.74%), 18 (29.03%), 8 (12.90%) and 25 (40.32%) for patients without AKI and at stages 1, 2, and 3, respectively. Considering the amendments suggested by KDIGO 2012, the mortality rates were 17.74%, 29.03%, 11.29% and 41.94% for patients without AKI and at stage I, stage II and stage III, respectively (Table 3).
Table 3.
Mortality rate stratified according to the RIFLE and AKIN criteria
| Total (N=190) | Death (N=62) | No death(N=128) | |
| RIFLE | |||
| Without AKI | 71 (37.4) | 11 (17.74) | 60 (46.87) |
| Risk | 58 (30.5) | 14 (22.58) | 44 (34.37) |
| Injury | 28 (14.7) | 15 (24.19) | 13 (10.16) |
| Failure | 33 (17.4) | 22 (35.48) | 11 (8.59) |
| AKIN | |||
| Without AKI | 70 (36.8) | 11 (17.74) | 59 (46.09) |
| Stage 1 | 71 (37.4) | 18 (29.03) | 53 (41.40) |
| Stage 2 | 15 (7.9) | 8 (12.90) | 7 (5.47) |
| Stage 3 | 34 (17.9) | 25 (40.32) | 9 (7.03) |
| KDIGO | |||
| Without AKI | 70 (36.8) | 11 (17.74) | 59 (46.09) |
| Stage 1 | 71 (37.4) | 18 (29.03) | 53 (41.40) |
| Stage 2 | 14 (7.36) | 7 (11.29) | 7 (5.47) |
| Stage 3 | 35 (18.42) | 26 (41.94) | 9 (7.03) |
Results expressed as absolute n (valid percent).
We next tested the association between mortality and the RIFLE, AKIN and KDIGO criteria. The results for the RIFLE criteria were as follows: an odds ratio (OR) of 0.56 and a 95% confidence interval (95%CI) of 0.27 to 1.12 for the Risk stage; an OR of 2.82 with a 95%CI of 1.25 to 6.39 for the Injury stage; and an OR of 5.85 with a 95%CI of 2.61 to 13.12 for the Failure stage. The results for the AKIN criteria were and follows: an OR of 0.58 with a 95%CI of 0.30 to 1.11 for stage 1; an OR of 2.56 with a 95%CI of 0.88 to 7.42 for stage 2; and an OR of 8.93 with a 95%CI of 3.83 to 20.83 for stage 3. For the KDIGO criteria, the results were as follows: an OR of 0.58 with a 95%CI of 0.30 to 1.11 for stage 1; an OR of 2.2 with a 95%CI of 0.74 to 6.58 for stage 2; and an OR of 9.55 with a 95%CI of 4.10 to 22.22 for stage 3 (Table 4).
Table 4.
Association between mortality and the RIFLE, AKIN and KDIGO criteria
| Odds ratio (95%CI) | Odds ratio (95%CI) corrected for age and APACHE II score | |
| RIFLE criteria | ||
| Risk | 0.56 (0.27-1.12) | 0.48 (0.19-1.21) |
| Injury | 2.82 (1.25-6.39) | 1.19 (0.40-3.47) |
| Failure | 5.85 (2.61-13.12) | 4.12 (1.45-11.72) |
| AKIN criteria | ||
| Stage 1 | 0.58 (0.30-1.11) | 0.56 (0.24-1.30) |
| Stage 2 | 2.56 (0.88-7.42) | 2.60 (0.64-10.52) |
| Stage 3 | 8.93 (3.83-20.83) | 4.40 (1.47-13.16) |
| KDIGO criteria | ||
| Stage 1 | 0.58 (0.30-1.11) | 0.56 (0.24-1.30) |
| Stage 2 | 2.2 (0.74-6.58) | 2.30 (0.54-9.76) |
| Stage 3 | 9.55 (4.10-22.22) | 4.74(1.60-14.03) |
* Values for odds ratio with 95% confidence interval (95%CI) for the RIFLE and AKIN criteria based on univariate and multivariate logistic regression analyses.
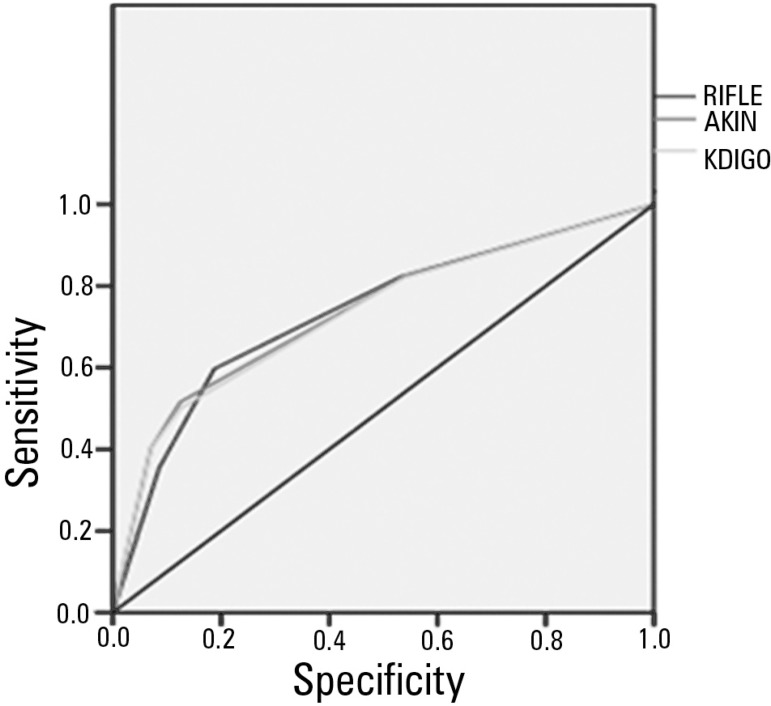
The area under the ROC curve (AUROC) was calculated as 0.735 for the RIFLE criteria, 0.74 for the AKIN criteria and 0.733 for the KDIGO criteria, with p<0.001 for all three criteria (Figure 1).
Figure 1.
ROC curve and the discriminatory power for death in critically ill patients for the RIFLE, AKIN and KDIGO criteria.
DISCUSSION
The present study was developed from a cohort of patients with a high median age. This finding corroborates other studies conducted in the ICU setting that have also evaluated parameters related to the development of kidney disorders.(5,7,8)
An important characteristic of the sample in the present study was that most patients were of African descent, reflecting the reality of the population served by the clinic where this study was conducted.(12) This aspect could lead to an overestimation of the incidence of AKI because such patients have a higher propensity to develop systemic hypertension, which is a disease known to be associated with kidney disorders.(13-16)
It should be noted that the RIFLE, AKIN and KDIGO criteria all operate using the same laboratory parameters and urine output measurements to stratify pre-established renal injury stages. Therefore, any bias that may compromise the accuracy of the values will affect all of the indices, thus reducing any particular influence on the outcome.(7)
A literature review conducted by searching medical-scientific databases analyzed several relevant studies published from January 2000 to June 2011 to arrive at a consensus definition of the parameters for AKI. Among the important conclusions expressed by the review, there was no clear superiority between the RIFLE and AKIN criteria for the establishment of AKI; the results for mortality were similar regardless of the classification used.(6) These findings were consistent with the results of the present study. However, experts prefer the AKIN index because it can detect AKI earlier by taking into account lower biomarker values.(6)
The first study to compare the RIFLE and AKIN criteria and relate them to AKI in an ICU setting was published in 2008 by Bagshaw et al. This large study involved more than 120,000 patients and concluded that the establishment of the AKIN criteria, which were derived from the renowned RIFLE criteria, was not significant in bringing substantial benefits.(7) Although the sample size was large and it was a multicenter study, that study had limitations related to being retrospective and because there were no data on the need for dialysis or urinary output every 6 hours, which may have led to misclassification of the different stages of AKI.
According to the data presented in the results of this work, it was evident that there was essentially no significant difference between the rates of AKI and mortality as determined by the RIFLE and AKIN criteria. This finding was consistent with similar studies in the medical-scientific literature.(5-7,17,18) However, some studies have shown small differences in the ability to diagnose AKI between the RIFLE and AKIN criteria. Some of those studies referred to the RIFLE as a more sensitive predictor,(10,19) while others indicated the AKIN as a better classification tool,(20,21) although both yield very similar results regarding the prediction of death.
As demonstrated in the literature by studies on the same topic using similar methodologies, mortality rates are expected to grow as the AKI progresses from initial to subsequent stages according to the RIFLE and AKIN classifications.(6) However, due to a small sample size, the present study was unable to show a statistically significant relationship between the severity of AKI and progression of mortality rates between the different stages. However, we found higher mortality rates associated with the KDIGO and AKIN stages III and the Failure classification in RIFLE. Moreover, both the KDIGO and AKIN stages III and the Failure classification in RIFLE were significantly associated with a higher likelihood of death in univariate and multivariate analyses corrected for age and APACHE II score (Tables 3 and 4).
Analyzing the layout of the ROC curves corroborated the findings of the present study. As explained in the results above, the AUROCs for the RIFLE, AKIN and KDIGO criteria were 0.735, 0.74 and 0.733, respectively, with p<0.001 for all three criteria. In this context, these values were similar to results found in the literature in studies addressing the same main topic.(5,7,22-24)
Although this study was not original because the topic has already been addressed in other populations, its main strength was the prospective design, which was in contrast to many studies that have been based on queries of large databases, as was the study by Bagshaw et al.(7) This design allowed the classifications based on the RIFLE and AKIN criteria to take into account the urinary output every 6 hours, related elevations in serum creatinine and the need for dialysis, thereby eliminating potential sources of classification bias. In addition, the recent amendments proposed by KDIGO(11) were also compared with the RIFLE and AKIN criteria as predictors of mortality. Additional limitations of the present study were the single center focus and the number of patients included.
CONCLUSION
The RIFLE, AKIN and KDIGO scores were all good predictors of mortality in critically ill patients, and there were no differences among them in terms of predicting death. These scores are good predictors of death.
Footnotes
Conflicts of Interest: None.
REFERENCES
- 1.Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30(9):2051–2058. doi: 10.1097/00003246-200209000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Thadhani R, Pascual M, Bonventre JV. Acute renal failure. N Engl J Med. 1996;334(22):1448–1460. doi: 10.1056/NEJM199605303342207. [DOI] [PubMed] [Google Scholar]
- 3.Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients. Crit Care. 2006;10(3):R73. doi: 10.1186/cc4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta RL, Pascual MT, Soroko S, Savage BR, Himmelfarb J, Ikizler TA, Paganini EP, Chertow GM, Program to Improve Care in Acute Renal Disease Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int. 2004;66(4):1613–1621. doi: 10.1111/j.1523-1755.2004.00927.x. [DOI] [PubMed] [Google Scholar]
- 5.Chang CH, Lin CY, Tian YC, Jenq CC, Chang MY, Chen YC, et al. Acute kidney injury classification: comparison of AKIN and RIFLE criteria. Shock. 2010;33(3):247–252. doi: 10.1097/SHK.0b013e3181b2fe0c. [DOI] [PubMed] [Google Scholar]
- 6.Valette X, du Cheyron D. A critical appraisal of the accuracy of the RIFLE and AKIN classifications in defining "acute kidney insufficiency" in critically ill patients. J CritCare. 2013;28(2):116–125. doi: 10.1016/j.jcrc.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 7.Bagshaw SM, George C, Bellomo R, ANZICS Database Management Committe A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23(5):1569–1574. doi: 10.1093/ndt/gfn009. [DOI] [PubMed] [Google Scholar]
- 8.Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C, Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294(7):813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 9.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, et al. Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med. 2009;35(10):1692–1702. doi: 10.1007/s00134-009-1530-4. [DOI] [PubMed] [Google Scholar]
- 11.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl. 2012;2(Suppl 1):1–138. [Google Scholar]
- 12.Instituto Brasileiro de Geografia e Estatística - IBGE . Cidades. Informações sobre os municípios brasileiros. Bahia. Salvador: [citado 2013 Dec4]. [Internet] Disponível em: http://cidades.ibge.gov.br/xtras/perfil.php?lang=&codmun=292740&search=bahia|salvador. [Google Scholar]
- 13.Rose DE, Farmer MM, Yano EM, Washington DL. Racial/ethnic differences in cardiovascular risk factors among woman veterans. J Gen Intern Med. 2013;Suppl2:S524–S528. doi: 10.1007/s11606-012-2309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarafidis PA, Georgianos P, Bakris GL. Resistant hypertension--its identification and epidemiology. Nat Rev Nephrol. 2013;9(1):51–58. doi: 10.1038/nrneph.2012.260. Review. Erratum in: Nat Rev Nephrol. 2013;9(9):492. [DOI] [PubMed] [Google Scholar]
- 15.Hunte HE, Mentz G, House JS, Schulz AJ, Williams DR, Elliott MR, et al. Variations in hypertension-related outcomes among Blacks, Whites and Hispanics in two large urban areas and in the United States. Ethn Dis. 2012;22(4):391–397. [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang H, Rodriguez-Monguio R. Racial disparities in the risk of developing obesity-related diseases: a cross-sectional study. Ethn Dis. 2012;22(3):308–316. [PubMed] [Google Scholar]
- 17.Tülübas EK, Demir G, Duman E, Altun D, Çetingök H, Hergünsel O, et al. Monitoring of renal function in patients with RIFLE and AKIN scores to compare the effects on mortality and morbidity in ICU. Med J Bakirköy. 2013;9(2):69–72. [Google Scholar]
- 18.Englberger L, Suri RM, Li Z, Casey ET, Daly RC, Dearani JA, et al. Clinical accuracy of RIFLE and Acute Kidney Injury Network (AKIN) criteria for acute kidney injury in patients undergoing cardiac surgery. Crit Care. 2011;15(1):R16. doi: 10.1186/cc9960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kompoti M, Paridou A, Stefanatou E, Koutsodimitropoulos I, Iordanidou O, Markou N, et al. Acute kidney injury predicts mortality in critically ill patients: a comparison of RIFLE and AKIN classifications. Intensive Care Med. 2010;36(2) Suppl:S175. [Google Scholar]
- 20.Ratanarat R, Skulratanasak P, Tangkawattanakul N, Hantaweepant C. Clinical accuracy of RIFLE and Acute Kidney Injury Network (AKIN) criteria for predicting hospital mortality in critically ill patients with multi-organ dysfunction syndrome. J Med Assoc Thai. 2013;96(Suppl 2):S224–S231. [PubMed] [Google Scholar]
- 21.Jiang F, Chen YH, Liang XL, Xu LX, Ma GP, Hu PH, et al. The sensitivity and accuracy of RIFLE and AKIN criteria for acute kidney injury diagnosis in intensive care unit patients. Zhongguo Wei Zhong Bing JiJiu Yi Xue. 2011;23(12):759–762. Chinese. [PubMed] [Google Scholar]
- 22.Yan X, Jia S, Meng X, Dong P, Jia M, Wan J, et al. Acute kidney injury in adult postcardiotomy patients with extracorporeal membrane oxygenation:evaluation of the RIFLE classification and the Acute Kidney Injury Network criteria. Eur J Cardiothorac Surg. 2010;37(2):334–338. doi: 10.1016/j.ejcts.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Robert AM, Kramer RS, Dacey LJ, Charlesworth DC, Leavitt BJ, Helm RE, Hernandez F, Sardella GL, Frumiento C, Likosky DS, Brown JR, Northern New England Cardiovascular Disease Study Group Cardiac surgery-associated acute kidney injury: a comparison of two consensus criteria. Ann Thorac Surg. 2010;90(6):1939–1943. doi: 10.1016/j.athoracsur.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 24.Lopes JA, Fernandes J, Jorge S, Neves J, Antunes F, Prata MM. An assessment of the RIFLE criteria for acute renal failure in critically ill HIV-infected patients. Crit Care. 2007;11(1):401. doi: 10.1186/cc5121. [DOI] [PMC free article] [PubMed] [Google Scholar]