Abstract
Objective
To characterize the profile of effective organ and tissue donors and to understand which organs and tissues were donated for transplantation.
Methods
This was a quantitative, descriptive, exploratory, retrospective study that analyzed clinical data from 305 donors between January 2006 to December 2010. The data were then analyzed using descriptive analyses, generating frequency tables, measures of position (mean, minimum and maximum) and measures of dispersion (standard deviation) for data that was social and clinical in nature.
Results
There was an overall predominance of white (72%) and male (55%) individuals between the ages of 41 and 60 years (44%). The primary cause of brain death was cerebrovascular accident (55%). In the patient history, 31% of the patients were classified as overweight, 27% as hypertensive and only 4.3% as having diabetes mellitus. Vasoactive drugs were used in 92.7% of the donors, and the main drug of choice was noradrenaline (81.6%). Hyperglycemia and hypernatremia were diagnosed in 78% and 71% of the donors, respectively.
Conclusion
Significant hemodynamic changes were found, and the results indicate that the use of vasoactive drugs was the main strategy used to control these changes. Furthermore, most donors presented with hyperglycemia and hypernatremia, which were frequently reported in association with brain death. The persistent nature of these findings suggests that the organ donors were inadequately maintained.
Keywords: Brain death, Organ transplantation, Tissue donors, Intensive care units
INTRODUCTION
In the area of transplantation, Brazil is notable for having one of the largest public organ and tissue transplant programs in the world, currently ranked second in kidney, liver and cornea transplants according to absolute numbers.(1) Thus, despite the advances in transplantation and the fact that Brazil has a systematic and legal protocol for diagnosing brain death (BD),(2) there is still a growing imbalance between the supply and demand for organs.(3,4)
Among potential brain-dead organ donors, there are several reasons for not harvesting the organs for donation,(5) of which cardiac arrest (CA) is the second leading reason for not harvesting organs for donation in 2012, reaching 52% in some regions.(6)
To increase the number of brain-dead organ and tissue donors, it is vital that the occurrence of CA be reduced by employing strategies aimed at maintaining the physiological stability of the patient, thus achieving the maximum vitality of potentially transplantable organs.
Maintaining the potential brain-dead donor requires the dedication and technical expertise of the team responsible for patient care because, during BD, a series of physiological changes occur that contribute to the instability of the patient, which may result in hypotension, diabetes insipidus, hypothermia, hypernatremia, metabolic acidosis, pulmonary edema and disseminated intravascular coagulation,(5,6) in addition to hyperglycemia, which can be explained by the combination of elevated endogenous catecholamines, exogenous inotropic agents and steroids, which are further aggravated by the administration of glycosylated substances.(7)
These physiological changes may occur secondary to patient treatment, neurological damage or as a result of physiological changes resulting from BD.(8) When these changes are present in a potential donor, they can contribute to CA.
Although organ and tissue transplantation is a safe and effective therapeutic alternative in the treatment of various diseases, resulting in improved quality of life and increased likelihood of survival,(6) there is a race against time to turn a potential donor, with all the hemodynamic/physiological instability that BD causes, into an effective donor that can offer recipients the highest quality organs. Thus, there is a need to know the functional status of the organs that are removed for transplantation and to adopt corrective strategies in response to possible changes. This study therefore aimed to characterize the profile of effective organ and tissue donors.
METHODS
This was a quantitative, descriptive, exploratory and retrospective study.(9) The research was conducted at the Organ and Tissue Procurement Service of the Hospital de Clínicas da Universidade Estadual de Campinas (UNICAMP), located in the city of Campinas, São Paulo (SP), Brazil. This service is responsible for the notification and implementation of donations in all the hospitals in the administrative region of Campinas. The study was approved by the Research Ethics Committee of the Faculdade de Ciências Médicas, UNICAMP (Opinion Nº 1163/2011), which granted a waiver for the informed consent requirement.
The study population consisted of patients whose data were contained in the "Information About Multiple Organ Donor" records of the Organ and Tissue Procurement Services (potential deceased donors who were brain dead) and who underwent surgery to remove the organs (effective donor) with the approval of the Organ Notification, Procurement and Distribution Center of the municipality of Ribeirão Preto.
The patient records that were reviewed and analyzed were from the period between January 2006 and December 2010. They contained all the information necessary to meet the inclusion and exclusion criteria of the study protocol. Data collection was performed between December 2011 and January 2012.
The inclusion criteria were that the data contained in the record showed that patients were effective donors, i.e., the extraction surgery was performed. These patients were identified by records showing that the extracted organs were subsequently implanted or discarded for transplantation (when sent for pathological examinations).
The exclusion criteria included prospective donors who were not effective donors, i.e., who did not undergo surgical removal of organs, and living organ donors, understood here as related (relatives up to the fourth degree) or unrelated (no relation) donors.
The principal investigator performed the data collection on the premises of the Organ and Tissue Procurement Services.
The data on the effective donors were recovered using records on Multiple Organ Donors prepared by the State Department of Health/State Transplant System (records available at the Organ and Tissue Procurement Services) and then entered into a spreadsheet prepared especially for this study. The following information was recorded: gender, age range, race, cause of BD, comorbidities (hypertension - HTN, diabetes mellitus - DM in the donor or in first-degree relatives - DFDR), obesity, habits (tobacco use, drug addiction and alcoholism), mean arterial pressure (MAP) levels, amount and type of vasoactive drugs (DVA) used, serum levels of urea, creatinine, sodium, potassium and glucose and the organs and tissues donated.
The data were transferred to the program Excel for Windows/2003 and then to the program Statistical Analysis System (SAS) for Windows, version 8.02, for the descriptive analyses and to calculate frequency tables, measures of position (mean, minimum and maximum) and measures of dispersion (standard deviation) for data that were social and clinical in nature.
The reference values used in adults, which were established by the pathology laboratory at the Hospital de Clínicas of the UNICAMP where the blood samples were processed, were serum urea (<58mg/dL), creatinine (male up to 1.2mg/dL and female up to 0.9mg/dl), sodium (136 to 146mEq/L), potassium (3.1 to 5.4mEq/L) and glucose (60 to 100mg/dL). The discrimination criteria for being overweight (body mass index - BMI≥25) or obese (BMI≥30) were based on the classification defined by the World Health Organization.(10)
RESULTS
The Organ and Tissue Procurement Services of the Hospital de Clínicas of the UNICAMP, from January 2006 to December 2010, provided 305 effective donors for the State Transplantation System of São Paulo.
The majority of the effective donors were male (n=167, 55%) and Caucasian (n=220, 72%), with a mean age of 41.45±14.1 years (ranging from 1.5 years to 81 years), as shown in table 1.
Table 1.
Descriptive, clinical, hemodynamic characterization and renal and electrolyte profiles of effective donors
| Variable | Result (N=305) |
|---|---|
| Age (years) | 41.45±14.1 |
| Race | |
| Caucasian | 220 (72.0) |
| Black | 28 (9.0) |
| Asian | 3 (0.9) |
| Pardo (mixed race) | 54 (17.0) |
| Male | 167 (55) |
| History | |
| Overweight | 95 (31.15) |
| HTN | 82 (27.0) |
| DFDR | 42 (14.0) |
| Obesity | 23 (7.55) |
| DM | 13 (4.3) |
| Habits | |
| Tobacco use | 60 (19.7) |
| Alcoholism | 57 (18.7) |
| Drug addiction | 27 (8.8) |
| Hemodynamics | |
| VAG | 283 (92.7) |
| Noradrenaline | 249 (81.6) |
| Dose (mcg/kg/min) | 0.21 (0.001-3.25) |
| Dopamine | 73 (24.0) |
| Dose (mcg/kg/min) | 7 (0.1-20.0) |
| Dobutamine | 9 (3.0) |
| Dose (mcg/kg/min) | 7.5 (4.0-10.0) |
| Vasopressin | 2 (0.65) |
| Dose (U/min) | 0.44 (0.4-0.48) |
| Renal profile | |
| Creatinine (mg/dL) | 0.93±0.11 |
| Urea (mg/dL) | 47±29.3 |
| Electrolyte profile | |
| Sodium (mEq/L) | 160.42±16.1 |
| Potassium (mEq/L) | 3.33±1.0 |
| Glucose (mg/dL) | 162.5±86.0 |
HTN - hypertension; DFDR - first-degree relatives with diabetes mellitus, DM - diabetes mellitus; VAG - vasoactive drugs. Results are expressed as number (percentage), mean±standard deviation or median (minimum–maximum).
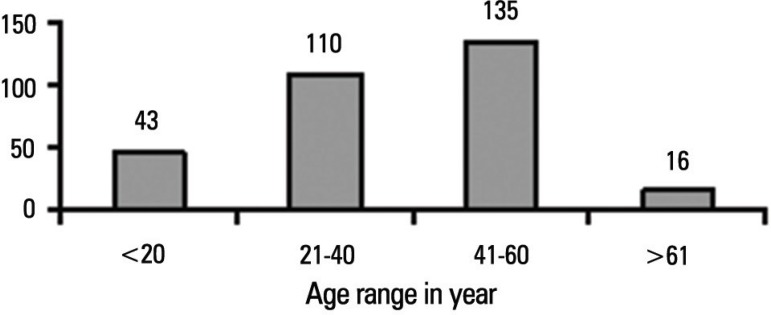
Figure 1 shows that 44% (n=135) of the donors evaluated by the Organ and Tissue Procurement Services of the Hospital de Clínicas of the UNICAMP were in the 41-60 year age group.
Figure 1.
Distribution of organ and tissue donors according to age range.
Among the primary causes of BD in effective donors evaluated, cerebrovascular accident (CVA) was the most predominant, responsible for more than half of all cases of BD (55%), followed by traumatic brain injury (TBI) at 35% and "other", which accounted for a total of 10% of the cases of BD, including central nervous system tumors, hypoxicischaemic encephalopathy, firearm injuries and hydrocephalus.
Of the history and lifestyle habits of the donors (Table 1), being overweight (31.15%) and hypertensive (27.0%) stood out. Among the lifestyle habits, tobacco use or alcohol consumption were found in approximately 20% of the donors.
For hemodynamic maintenance, ventricular assist devices (VADs) were used in 92.7% (n=283) of the donors, of which noradrenaline was the main drug of choice (n=249, 81.6%) and vasopressin the secondary drug of choice (n=2, 0.65%) (Table 1). The mean MAP levels were 88.02±17.02mmHg (ranging from 49 to 136.66mmHg).
According to table 1, the renal function evaluation of potential organ and tissue donors revealed an average creatinine level of 0.93±0.11mg/dL (ranging from 0.05 to 6.7mg/dL). For urea, the mean level was 47.0±29.3mg/dL (ranging from 10 to 221mg/dL). Values that were higher than the accepted reference values for serum creatinine levels were observed in 159 (52.1%) effective donors, 89 (29.2%) of whom had creatinine values >1.5mg/dL, and of these, 77 (25.3%) were kidney donors.
For the electrolyte profile, the mean serum sodium level was 160.42±16.1mEq/L (127 to 203mEq/L), and the mean potassium level was 3.33±1.0mEq/L (1.4 to 7.8mEq/L). In 189 (62%) donors, the serum sodium levels were greater than 155mEq/L, and of these, the liver was harvested from 162 (53.1%) donors.
The average blood glucose level was 162.5±86.0mg/dL (55 to 586mg/dL), and hyperglycemia was observed in 78.4% of the donors evaluated. In 29.2% (n=89) of the donors, the blood glucose value was higher than 180mg/dL. Hypernatremia was observed in 77.7% (n=237) of the donors, and hypokalemia was observed in 15.0% (n=46).
All the donors with expanded criteria had at least one organ harvested. Among the 14 donors more than 60 years of age, 12 were liver donors and 14 were kidney donors. Of the donors between the ages of 50 and 59 years with prior HTN and who had a CVA as the cause of coma (n=36), 29 of them were liver donors and 34 were kidney donors. Among the obese donors (n=23), there were 18 liver donors, 16 kidney donors, three heart donors and three pancreas donors.
In total, 92.7% (n=283) of the donors had their kidney harvested, 87.8% (n=268) their liver, 79.0% (n=241) their corneas, 23.3% (n=71) their pancreas, 11.5% (n=35) their bones, 11.1% (n=34) their hearts and only 6% (n=18) their lungs.
DISCUSSION
In the present study, the major comorbidities observed in organ and tissue donors from the Organ and Tissue Procurement Services of the Hospital de Clínicas of the UNICAMP included being overweight and hypertensive. For pressure stability, noradrenaline was the drug of choice, and vasopressin was used the least often. Hyperglycemia and hypernatremia were the most frequent metabolic disorders, representing, in part, the likely failure to maintain potential donors. The serum creatinine levels were greater than the reference values in more than 50% of the donors, and of those with creatinine levels >1.5mg/dL (89, 29.2%), 77 (25.3%) were kidney donors. At least one organ was harvested in 100% of the donors who were considered "marginal". The kidneys were harvested the most frequently compared to other organs, such as the liver, pancreas, heart and lungs. The corneas were the tissue harvested most frequently for transplantation.
Studies performed in Brazil(11,12) and abroad(13,14) are consistent with the present study, i.e., the age range of approximately 50% of the donors was between 41 and 60 years.
Of the primary causes of BD among organ and tissue donors, CVA was the most prevalent, which is consistent with reports by other researchers.(11-15) In the present study, TBI was the second leading cause, and this finding is confirmed in the literature.(11,13,15) These data indicate a change in the profile of organ donors because traumatic causes are being supplanted by CVA as the cause of death. This change may be related to stricter traffic regulations in Brazil, which have reduced the number of automotive accidents and increased the life expectancy of Brazilians.
Researchers have shown direct correlations between CVA and cardiovascular diseases with obesity, hypertension, diabetes, tobacco use and alcoholism.(16,17) In recent decades, the number of obese donors has been increasing, and complications following renal transplantation have been correlated with being overweight and obese.(13)
As we observed in this study for donors with these comorbidities and potentially health-compromising social habits, the quality of the graft is expected to be worse because of the dysfunctional organic processes that characterize these diseases.
Donors with such risk factors are referred to as "marginal", "borderline" or "expanded criteria" donors, and these donations have been legalized by laws governing transplantation due to the small number of organs available for transplantation in Brazil.(18)
The use of organs from "marginal" donors may increase the chances of transplant failure. One study reported an increase in mortality in liver transplant patients, especially in cases in which the recipients were more seriously ill.(19)
Due to the shortage of organs and the number of people needing a transplant, it is extremely important that potential donors are well cared for by trained professionals, minimizing important endocrine, metabolic and hemodynamic disturbances caused by BD.
Hemodynamic maintenance is the main challenge in treating potential donors because following the adrenergic storm, hypotension is observed, which is a common problem that leads to decreased perfusion of various organs,(20) requiring the pressure parameters to be corrected fairly quickly. Experts recommend that the achievable blood pressure goals should be a MAP between 60 and 80mmHg and a systolic BP ranging from 90 to 100mmHg.(21-24)
To ensure adequate perfusion, vasopressor and inotropic support should be provided if the minimum BP is not reached or maintained after adequate volume expansion. Vasopressor and/or inotropic drugs should then be given with caution because the overuse of these drugs can lead to severe vasoconstriction followed by ischemia of the organs.(23,24) The administration (more restrictive) of fluids for fluid replacement in maintaining the potential donor has resulted in an increased number of successful lung transplants.(5,16)
In the present study, the analysis of the mean blood pressure values (MAP 88.02±17.02 mmHg, ranging from 49 to 136.66mmHg) and VAD use in a large number of donors (92.7%) indicates that the use of vasopressor drugs in potential donors may have been excessive and/or indiscriminate, given that most of the MAP values in this study were higher than those recommended in the literature.
One strategy by which to improve hemodynamic maintenance in potential deceased donors involves hormone replacement therapy, with the administration of vasopressin, thyroid hormones and corticosteroids.(25) In this study, the use of vasopressin was limited (only administered to two donors, 0.65%), which can be explained by the fact that the donor sample consisted of organ and tissue donors from the period between 2006 and 2010, which is well before the "Guidelines for the Handling of Multiple Organs from Potential Adult Deceased Donors" was available to the Brazilian scientific community.
The use of managed treatment protocols for potential deceased donors helps improve the hemodynamic and physiological maintenance of these patients by reducing the incidence of CA before harvesting the organs, which may contribute to an increase in the supply of organs and tissues.(26)
In the analysis of the renal profile, the mean creatinine and urea levels, as shown in table 1, were found to be comparable to those reported by Weissenbacher et al.(13) in a sample of 1,113 deceased kidney donors.
A study indicates that changes in glucose levels, if not corrected, affect the renal function of donors.(27) Olmos et al.(28) reported significant correlations between donors undergoing procedures to correct blood glucose levels and improved renal function.
Blasi-Ibañez et al.(29) evaluated 458 organ donors and showed a strong correlation between blood glucose and serum creatinine levels immediately before nephrectomy, reporting blood glucose levels >200mg/dL in 72% of the donors at the time of organ harvesting. However, these findings are somewhat controversial because there is only a limited number of studies that have performed correlation analyses with these variables in brain-dead patients. In addition, in a study conducted using intensive care patients, there was an increase in mortality reported for patients who were maintained at normoglycemia.(25,30)
In maintaining potential organ donors, experts recommend that hyperglycemia be corrected using intravenous insulin therapy to achieve blood glucose levels of <180mg/dL.(25,26) In an American study that compared blood glucose levels in deceased organ donors and the use of glycemic control protocols during the period from 2005 to 2006 (donors not receiving the glycemic control protocols) and the period from 2009 to 2010 (donors receiving the glycemic control protocols), the reported averages were 212±32 and 162±44mg/dL, respectively.(28) The high blood glucose values observed in the present study (162.5±86.0mg/dL, 55 to 586mg/dL) suggest the lack of or ineffectiveness of the protocols for glycemic control in caring for potential donors.
As for hypernatremia, sodium levels >155mEq/L may contribute to edema, dysfunction, apoptosis and cellular necrosis. These complications contribute to primary graft failure, with the worst results evident in liver transplants.(7,30) The analysis of heart donors showed an increase in the mortality of recipients when the serum sodium levels were <130mEq/L or >170mEq/L.(18) The data collected in this study, in which the mean serum sodium level was 160.42±16.1mEq/L (ranging from 127 to 203mEq/L), showed that disorders of this electrolyte, coupled with other metabolic abnormalities, put at risk the quality of the organs that were extracted from the donors at the Organ and Tissue Procurement Services of the Hospital de Clínicas of the UNICAMP.
Understanding these changes in potential donors, as well as factors that reduce the quality of the graft supplied for transplantation such as age, tobacco use, history of alcoholism, cause of BD, cold ischemia time (time that the organ is outside the donor's body and under refrigeration) >12 hours and warm ischemia time (time between the onset of the anastomosis of the vena cava and portal vein reperfusion in liver recipients) >45 minutes,(31) should help doctors anticipate major complications in transplant patients.
As noted in this study, the primary harvested organ was the kidney (in 92.7% of effective donors). This fact can be explained by certain advantages that the kidneys have over other solid organs that are harvested: a prolonged cold ischemia time of up to 36 hours,(32,33) acceptable donor age of 75 years, provided that renal function is preserved and the presence of two organs (some changes observed by the surgeon at the time of the nephrectomy can lead to discarding only one kidney). Moraes et al.(11) reported similar results to those observed in this study, including that 81% of their patients were kidney donors and only 2% were lung donors. These numbers are typical worldwide.(34) For tissue donations, corneas were the primary tissue harvested (79%), which can also be explained by the advantages that this tissue has over other tissues, including that it is not limited by age or the blood type of the potential donor and that it can be harvest up to 24 hours later if the body of the donor is maintained at the appropriate temperature (4°C).(31)
Therefore, this study detected the harvest of organs and tissues from donors with expanded criteria and identified flaws in the hemodynamic and physiological maintenance of these patients. The limitations of the study included that it was not possible to analyze the function of these organs following explantation (either the transplanted organs or those sent for pathology) or to identify the actions taken by the care teams concerning the observed changes.
We suggest that correlation studies be performed to verify the function of these grafts and the quality of life of the transplant patients and to analyze the primary changes that led to the discarding of the graft.
CONCLUSION
When considering the clinical profile of effective donors, being overweight and hypertensive were the most common comorbidities observed. Notably, most of the patients had altered serum levels of glucose, sodium and creatinine. Hemodynamic instability occurred in the majority of the subjects, and the use of noradrenaline as a vasopressor drug was observed in almost all cases. Finally, among the "marginal" donors, 100% had at least one organ harvested. The kidneys were the organ that was harvested the most often for transplant, followed by the liver, pancreas, heart, lungs and corneas.
Footnotes
Conflicts of interest: None.
REFERÊNCIAS
- 1.Dimensionamento dos transplantes no Brasil e em cada estado (2005-2012) [acesso em 09 Setembro 2013];Registro Brasileiro de Transplantes. 2012 18(4) Disponível em: http://www.abto.org.br/abtov03/Upload/file/RBT/2012/RBTdimensionamento2012.pdf. [Google Scholar]
- 2.Morato EG. Morte encefálica: conceitos essenciais, diagnóstico e atualização. Rev Med Minas Gerais. 2009;19(3):227–236. [Google Scholar]
- 3.Brasil. Secretaria de Estado da Saúde de São Paulo. Sistema Estadual de Transplantes . Lista de espera por órgão e córnea - 2010. Lista de espera para transplante, com doador cadavérico, no Estado de São Paulo. São Paulo: Secretaria de Estado da Saúde de São Paulo; 2010. [citado 2011 Ago 5]. Disponível em: http://www.saude.sp.gov.br/ses/perfil/gestor/informacoes-de-saude_1/transplantesem-dados/lista-de-espera-por-orgao-e-cornea-2012. [Google Scholar]
- 4.United States of America [cited 2014 Jan 21];Organ Procurement and Transplantation Network. Data. Waiting list candidates 2014. Disponível em: http://optn.transplant.hrsa.gov/
- 5.Shah VR. Aggressive management of multiorgan donor. Transplant Proc. 2008;40(4):1087–1090. doi: 10.1016/j.transproceed.2008.03.029. [DOI] [PubMed] [Google Scholar]
- 6.Mascia L, Mastromauro I, Viberti S, Vincenzi M, Zanello M. Management to optimize organ procurement in brain dead donors. Minerva Anestesiol. 2008;74:1–8. [PubMed] [Google Scholar]
- 7.Smith M, Vyas H. Management of the potential organ donor. Paediatr Child Health (Oxford) 2011;21(4):182–186. [Google Scholar]
- 8.Shemie SD, Ross H, Pagliarello J, Baker AJ, Greig PD, Brand T, Cockfield S, Keshavjee S, Nickerson P, Rao V, Guest C, Young K, Doig C, Pediatric Recommendations Group Organ donor management in Canada: recommendations of the forum on Medical Management to Optimize Donor Organ Potential. CMAJ. 2006;174(6):S13–S32. doi: 10.1503/cmaj.045131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gil AC. Como elaborar projeto de pesquisa. 4ª ed. São Paulo: Atlas; 2002. [Google Scholar]
- 10.World Health Organization . Obesity and overweight. WHO; [Updated March 2013]. [cited 2013 Set 3]. http://www.who.int/mediacentre/factsheets/fs311/en/ Fact sheet nº 311; Updated March 2013. [Google Scholar]
- 11.Moraes EL, Silva LB, Moraes TC, Paixão NC, Izumi NM, Guarino AJ. The profile of potential organ and tissue donors. Rev Latinoam Enferm. 2009;17(5):716–720. doi: 10.1590/s0104-11692009000500019. [DOI] [PubMed] [Google Scholar]
- 12.Medina-Pestana JO, Sampaio EM, Santos TH, Aoqui CM, Ammirati AL, Caron D, et al. Deceased organ donation in Brazil: how can we improve? Transplant Proc. 2007;39(2):401–402. doi: 10.1016/j.transproceed.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Weissenbacher A, Jara M, Ulmer H, Biebl M, Bösmüller C, Schneeberger S, et al. Recipient and donor body mass index as important risk factors for delayed kidney graft function. Transplantation. 2012;93(5):524–529. doi: 10.1097/TP.0b013e318243c6e4. [DOI] [PubMed] [Google Scholar]
- 14.Jeong JC, Kim MG, Ro H, Kim YJ, Park HC, Kwon HY, et al. Outcomes of management for potential deceased donors. Transplant Proc. 2012;44(4):843–847. doi: 10.1016/j.transproceed.2012.01.102. [DOI] [PubMed] [Google Scholar]
- 15.Silva V, Formaggio P, Oliveira PC, Schaff C, Formigoni TH, Santos XCM. Profile of organs and tissue donors and their relatives of a Brazilian Organ Procurement Organization. 11th Congress of the International Society for Organ Donation and Procurement; 2nd Congress of the Iberoamerican Society of Transplant Coordinators; 2011 Nov 27-30; Buenos Aires, Argentina. Buenos Aires: ISODP; 2011. pp. 176–176. [Google Scholar]
- 16.World Health Organization (WHO) Cardiovascular diseases (CVDs) - What are the risk factors for cardiovascular disease? Geneva: WHO; [Updated March 2013]. [cited 2013 May 25]. Available from: http://www.who.int/mediacentre/factsheets/fs317/en/ [Google Scholar]
- 17.World Health Organization (WHO) What are the health consequences of being overweight? Geneva: WHO; [Updated December 2011]. [cited 2012 Feb 4]. Available from: http://www.who.int/features/qa/49/en/index.html. [Google Scholar]
- 18.McKeown DW, Bonser RS, Kellum JA. Management of the heart beating brain-dead organ donor. Br J Anaesth. 2012;108(Suppl 1):i96–107. doi: 10.1093/bja/aer351. [DOI] [PubMed] [Google Scholar]
- 19.Bacchella T, Gavão FH, Jesus de Almeida JL, Figueira ER, de Moraes A, César Machado MC. Marginal grafts increase early mortality in liver transplantation. Sao Paulo Med J. 2008;126(3):161–165. doi: 10.1590/S1516-31802008000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dictus C, Vienenkoetter B, Esmaeilzadeh M, Unterberg A, Ahmadi R. Critical care management of potential organ donors: our current standard. Clin Transplant. 2009;23(Suppl 21):2–9. doi: 10.1111/j.1399-0012.2009.01102.x. Review. [DOI] [PubMed] [Google Scholar]
- 21.Murugan R, Venkataraman R, Wahed AS, Elder M, Carter M, Madden NJ, Kellum JA, HIDonOR Study Investigators HIDonOR Study Investigators. Preload responsiveness is associated with increased interleukin-6 and lower organ yield from brain-dead donor. Crit Care Med. 2009;37(8):2387–2393. doi: 10.1097/CCM.0b013e3181a960d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frontera JA, Kalb T. How I manage the adult potential organ donor: donation after neurological death (part 1) Neurocrit Care. 2010;12(1):103–110. doi: 10.1007/s12028-009-9292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mascia LI, Mastromauro I, Viberti S, Vincenzi M, Zanello M. Management to optimize organ procurement in brain death donors. Minerva Anestesiol. 2009;75(3):125–133. [PubMed] [Google Scholar]
- 24.Westphal GA, Caldeira Filho M, Vieira KD, Zaclikevis VR, Bartz MC, Wanzuita R, et al. Diretrizes para manutenção de múltiplos órgãos no potencial doador adulto falecido. Parte I. Aspectos gerais e suporte hemodinâmico. Rev Bras Ter Intensiva. 2011;23(3):255–268. [PubMed] [Google Scholar]
- 25.Westphal GA, Caldeira Filho M, Vieira KD, Zaclikevis VR, Bartz MC, Wanzuita R, et al. Diretrizes para manutenção de múltiplos órgãos no potencial doador adulto falecido. Parte II. Ventilação mecânica, controle endócrino metabólico e aspectos hematológicos e infecciosos. Rev Bras Ter Intensiva. 2011;23(3):269–282. [PubMed] [Google Scholar]
- 26.Westphal GA, Zaclikevis VR, Vieira KD, Cordeiro RB, Horner MB, Oliveira TP, et al. Protocolo gerenciado de tratamento do potencial doador falecido reduz incidência de parada cardíaca antes do explante dos órgãos. Rev Bras Ter Intensiva. 2012;24(4):334–340. doi: 10.1590/S0103-507X2012000400007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marik PE. Techniques for assessment of intravascular volume in critically ill patients. J Intensive Care Med. 2009;24(5):329–337. doi: 10.1177/0885066609340640. [DOI] [PubMed] [Google Scholar]
- 28.Olmos A, Swain S, Blasilbanez A, Cahilkova R, Feiner J, Niemann C. Hyperglycemia and perioperative renal injury in the setting of kidney transplantation: a quality assessment study [abstract]; 11th Congress of the International Society for Organ Donation and Procurement; 2nd Congress of the Iberoamerican Society of Transplant Coordinators; 2011 Nov 27-30; Buenos Aires, Argentina. Buenos Aires: ISODP; 2011. p. 167. [Google Scholar]
- 29.Blasi-Ibañez A, Hirose R, Feiner J, Freise C, Stock PG, Roberts JP, et al. Predictors associated with terminal renal function in deceased organ donors in the intensive care unit. Anesthesiology. 2009;110(2):333–341. doi: 10.1097/ALN.0b013e318194ca8a. [DOI] [PubMed] [Google Scholar]
- 30.Feng S. Donor intervention and organ preservation: where is the science and what are the obstacles? Am J Transplant. 2010;10(5):1155–1162. doi: 10.1111/j.1600-6143.2010.03100.x. [DOI] [PubMed] [Google Scholar]
- 31.Totsuka E, Fung U, Hakamada K, Tanaka M, Takahashi K, Nakai M, et al. Analysis of clinical variable of donors and recipients with respect to short-term graft outcome in human liver transplantation. Transplant Proc. 2004;36(8):2215–2218. doi: 10.1016/j.transproceed.2004.08.052. [DOI] [PubMed] [Google Scholar]
- 32.Associação Brasileira de Transplante de Órgãos (ABTO) Diretrizes básicas para captação e retirada de múltiplos órgãos e tecidos da Associação Brasileira de Transplante de Órgãos. São Paulo: Associação Brasileira de Transplante de Órgãos; 2009. [Google Scholar]
- 33.Moraes EL, Silva LB, Glezer M, Paixão NC, Moraes TC. Trauma e doação de órgãos e tecidos para transplante. J Bras Transpl. 2006;9:561–565. [Google Scholar]
- 34.Thomson EM, McKeown DW. Organ donation and management of the potential organ donor. Anaesth Intensive Care Med. 2012;13(6):252–258. [Google Scholar]